Antiviral Agents for the Prevention and Treatment of Herpes Simplex Virus Type-1 Infection in Clinical Oncology: A Network Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
- Participants: Patients undergoing cancer treatment. Adults, children, or both were included in the search.
- Intervention: Any antiviral agent used for the prevention or treatment of oral herpes simplex virus infection were included.
- Comparisons: Active intervention, placebo, or no treatment.
- Outcomes: The primary outcome analyzed for prevention was the occurrence or absence of herpes simplex virus infections, clinically or as a positive culture. The primary outcome analyzed for treatment was the time required for complete healing of the lesions. Secondary outcomes were recurrence of lesions, the time required for pain relief, duration of viral shedding, and adverse effects.
2.2. Data Extraction and Management
2.3. Quality of Assessment
2.4. Strategy for Data Synthesis
3. Results
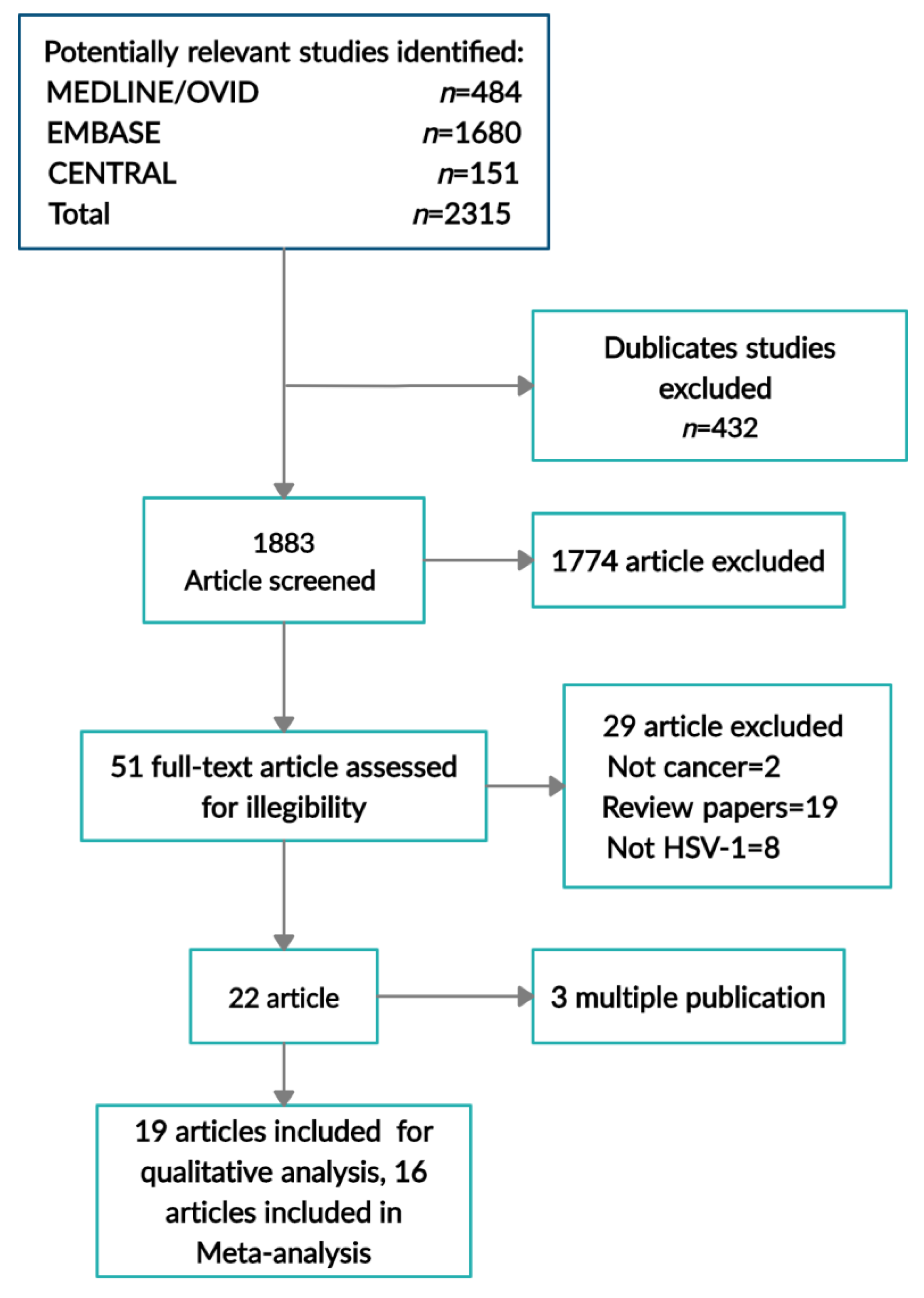
3.1. Study Selection
3.2. Study Characteristics
Quality of RCTs
3.3. Quality of Evidence
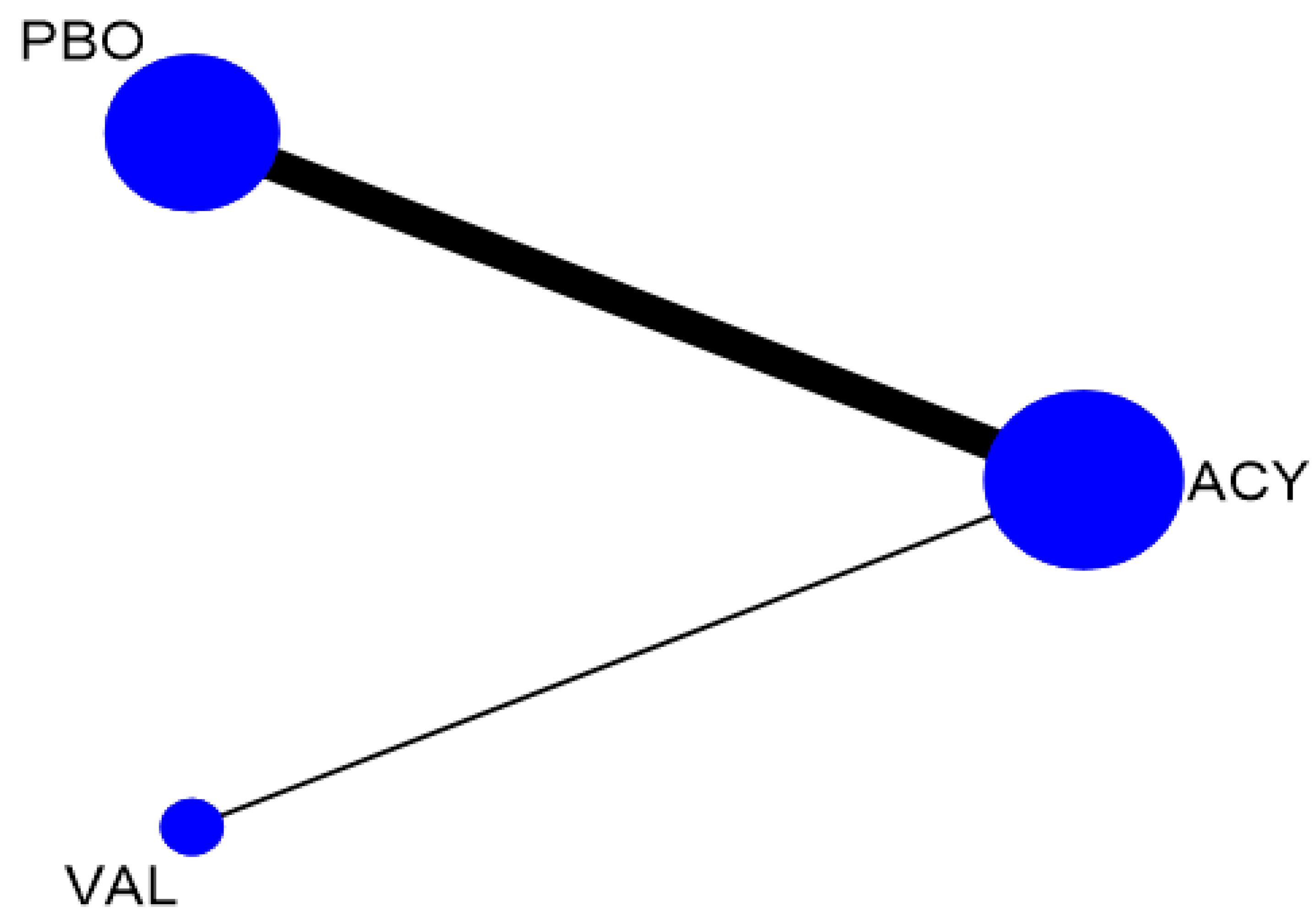
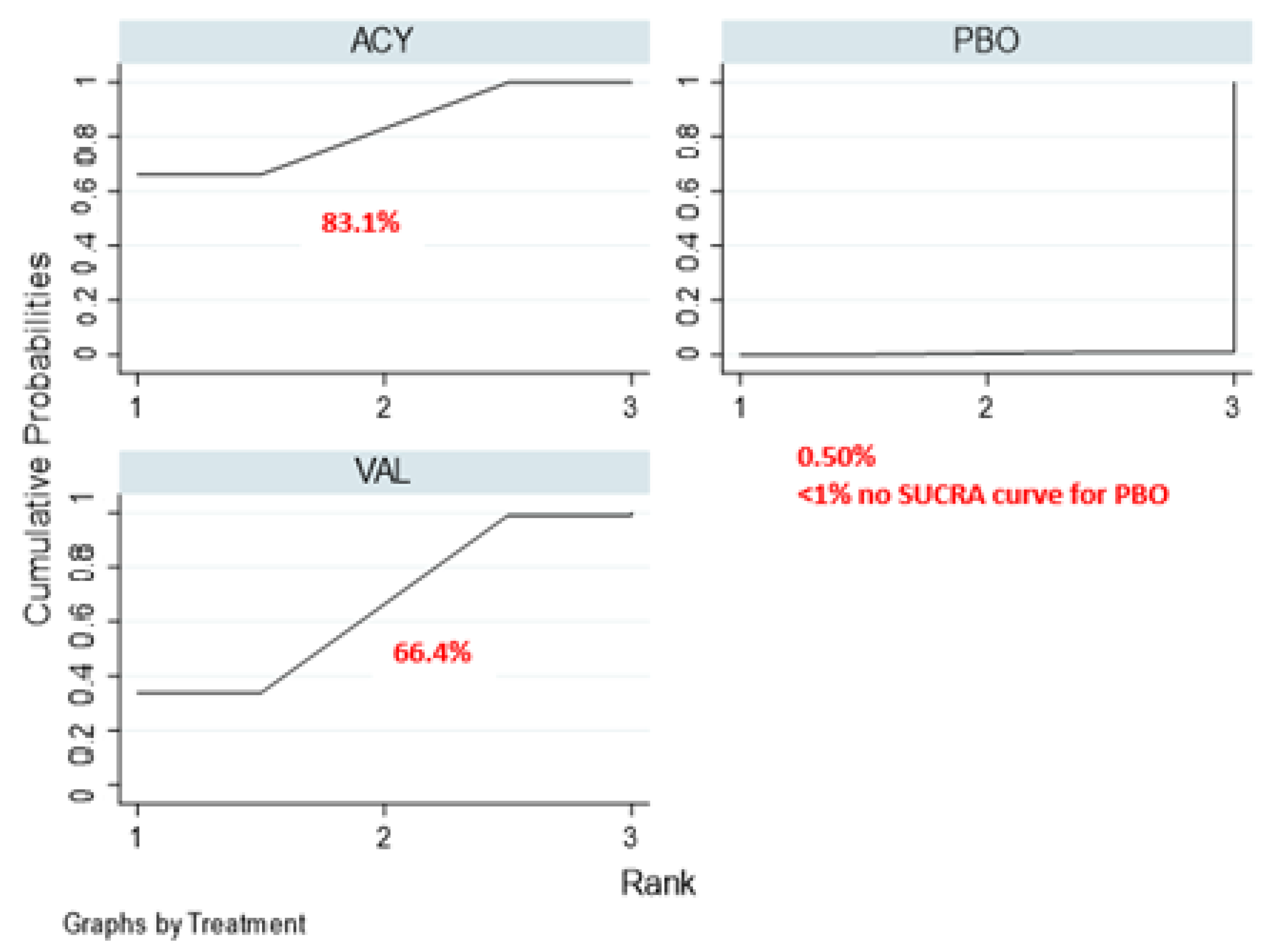
3.4. Prevention of Oral HSV Infection Using Valacyclovir
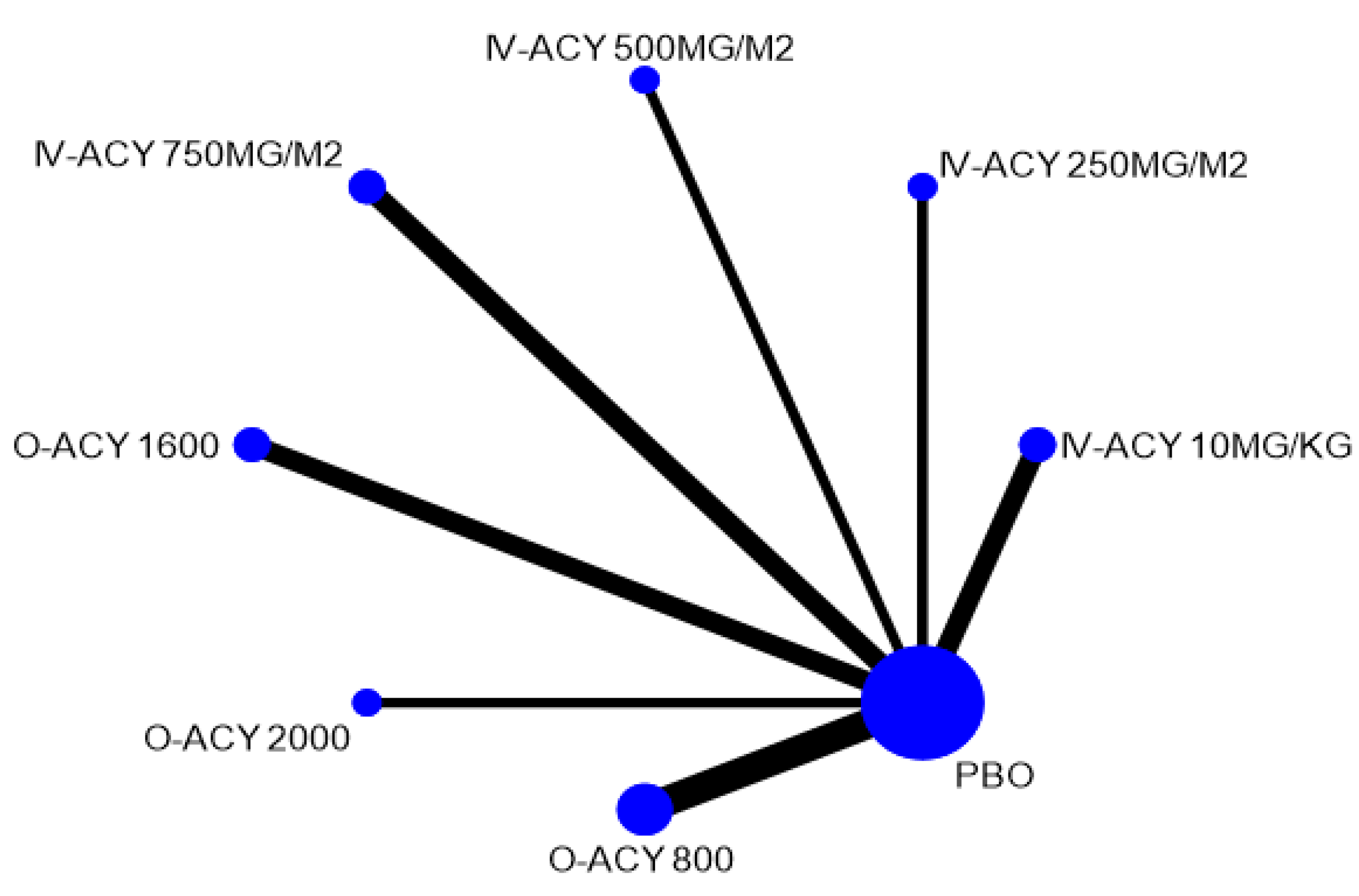
3.5. Treatment of Oral HSV Infection
3.6. Secondary Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A
| # | Keyword | Medline (Ovid) | Embase | Cochrane Central |
|---|---|---|---|---|
| 1 | exp NEOPLASMS/ | 3,327,198 | 4,250,169 | 77,595 |
| 2 | exp LEUKEMIA/ | 231,072 | 281,659 | 4644 |
| 3 | exp LYMPHOMA/ | 170,934 | 278,418 | 3173 |
| 4 | exp RADIOTHERAPY/ | 184,530 | 502,025 | 5856 |
| 5 | Chemotherapy.mp. | 434,962 | 782,593 | 78,184 |
| 6 | Bone Marrow Transplantation/ | 44,512 | 48,482 | 1368 |
| 7 | neoplasm$.mp. | 2,803,199 | 756,571 | 79,397 |
| 8 | cancer$.mp. | 1,769,905 | 3,491,963 | 169,046 |
| 9 | (leukaemi$ or leukemi$).mp. | 326,549 | 437,588 | 15,026 |
| 10 | (tumour$ or tumor$).mp. | 2,085,918 | 2,992,357 | 78,405 |
| 11 | malignan$.mp. | 569,105 | 861,406 | 27,680 |
| 12 | neutropeni$.mp. | 44,306 | 128,428 | 14,301 |
| 13 | carcino$.mp. | 1,021,355 | 1,423,938 | 45,899 |
| 14 | adenocarcinoma$.mp. | 238,058 | 269,624 | 11,190 |
| 15 | lymphoma$.mp. | 242,728 | 314,058 | 12,414 |
| 16 | (radioth$ or radiat$ or irradiat$ or radiochemo$).mp. | 893,029 | 1,226,258 | 51,508 |
| 17 | (bone adj marrow adj5 transplant$).mp | 5,8628 | 85,127 | 4001 |
| 18 | chemo$.mp. | 753,479 | 1,307,643 | 92,912 |
| 19 | or/1–18 | 5,244,394 | 6,656,084 | 271,167 |
| 20 | herpes simplex/or herpes labialis/or stomatitis, herpetic/ | 15,890 | 19,232 | 462 |
| 21 | (herpes or herpetic or “cold sore$”or cold-sore$).mp. | 72,420 | 116,809 | 4872 |
| 22 | simplexvirus/or herpesvirus 1, human/ | 27,442 | 3361 | 195 |
| 23 | HSV$.mp. | 25,977 | 32,427 | 862 |
| 24 | fever blister$.mp. | 39 | 53 | 5 |
| 25 | (oral adj3 infection).ti,ab. | 4631 | 5331 | 430 |
| 26 | (oral and vir$).ti,ab. | 27,253 | 36,737 | 4175 |
| 27 | or/20–26 | 106,267 | 157,655 | 9211 |
| 28 | exp Randomized Controlled Trial/ | 508,037 | 603,738 | 131 |
| 29 | exp Clinical Trial/ | 861,035 | 1,486,491 | 163 |
| 30 | randomized controlled trial.pt. | 507,205 | 0 | 495,880 |
| 31 | random$.tw. | 1,113,139 | 1,526,873 | 956,392 |
| 32 | blind$.ti,ab. | 291,995 | 408,397 | 319,311 |
| 33 | placebo$.ti,ab. | 212,210 | 302,942 | 298,344 |
| 34 | trial$.ti,ab. | 1,005,908 | 1,432,033 | 652,484 |
| 35 | or/28–34 | 2,163,766 | 3,165,315 | 1,236,237 |
| 36 | exp Acyclovir/ | 14,207 | 38,744 | 1205 |
| 37 | exp Zovirax/ | 14,207 | 38,744 | 1205 |
| 38 | antiviral$.ti,ab. | 85,534 | 115,959 | 5684 |
| 39 | exp Valacyclovir/ | 1060 | 7794 | - |
| 40 | exp Valtrex/ | 1060 | 7794 | - |
| 41 | exp Famciclovir/ | 529 | 3865 | - |
| 42 | exp Famvir/ | 529 | 3865 | - |
| 43 | anti viral$.ti,ab. | 6856 | 11,216 | 448 |
| 44 | antiherpetic.mp. | 519 | 638 | 16 |
| 45 | exp Acycloguanosine/ | 14,207 | 38,744 | 1205 |
| 46 | or/36–45 | 102,879 | 161,355 | or/36–41 7036 |
| 47 | 19 AND 27 AND 35 AND 46 | 599 | 1863 | 197 |
| 48 | limit 47 to humans limit 47 to (english language and humans) | 484 | 1680 | 151 |
References
- Naghavi, M.; Abajobir, A.A.; Abbafati, C.; Abbas, K.M.; Abd-Allah, F.; Abera, S.F.; Aboyans, V.; Adetokunboh, O.; Afshin, A.; Agrawal, A.; et al. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390, 1151–1210. [Google Scholar] [CrossRef]
- Epstein, J.B.; Gorsky, M.; Hancock, P.; Peters, N.; Sherlock, C.H. The prevalence of herpes simplex virus shedding and infection in the oral cavity of seropositive patients undergoing head and neck radiation therapy. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2002, 94, 712–716. [Google Scholar] [CrossRef] [PubMed]
- Shu, Z.; Li, P.; Yu, B.; Huang, S.; Chen, Y. The effectiveness of probiotics in prevention and treatment of cancer therapy-induced oral mucositis: A systematic review and meta-analysis. Oral Oncol. 2020, 102, 104559. [Google Scholar] [CrossRef] [PubMed]
- Whitley, R.J.; Kimberlin, D.W.; Roizman, B. Herpes simplex viruses. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 1998, 26, 541–553; quiz 554–555. [Google Scholar] [CrossRef]
- Nahmias, A.J.; Lee, F.K.; Beckman-Nahmias, S. Sero-epidemiological and -sociological patterns of herpes simplex virus infection in the world. Scand. J. Infect. Dis. Suppl. 1990, 69, 19–36. [Google Scholar]
- Wald, A.; Corey, L. Persistence in the population: Epidemiology, transmission. In Human Herpesviruses: Biology, Therapy, and Immunoprophylaxis; Arvin, A., Campadelli-Fiume, G., Mocarski, E., Moore, P.S., Roizman, B., Whitley, R., Yamanishi, K., Eds.; Cambridge University Press: Cambridge, UK, 2007; ISBN 978-0-521-82714-0. [Google Scholar]
- Ramchandani, M.; Kong, M.; Tronstein, E.; Selke, S.; Mikhaylova, A.; Magaret, A.; Huang, M.-L.; Johnston, C.; Corey, L.; Wald, A. Herpes Simplex Virus Type 1 Shedding in Tears, and Nasal and Oral Mucosa of Healthy Adults. Sex. Transm. Dis. 2016, 43, 756–760. [Google Scholar] [CrossRef]
- Corey, L.; Spear, P.G. Infections with Herpes Simplex Viruses. N. Engl. J. Med. 1986, 314, 686–691. [Google Scholar] [CrossRef]
- Embil, J.A.; Stephens, R.G.; Manuel, F.R. Prevalence of recurrent herpes labialis and aphthous ulcers among young adults on six continents. Can. Med. Assoc. J. 1975, 113, 627–630. [Google Scholar]
- Young, S.K.; Rowe, N.H.; Buchanan, R.A. A clinical study for the control of facial mucocutaneous herpes virus infections: I. Characterization of natural history in a professional school population. Oral Surg. Oral Med. Oral Pathol. 1976, 41, 498–507. [Google Scholar] [CrossRef]
- Bader, C.; Crumpacker, C.S.; Schnipper, L.E.; Ransil, B.; Clark, J.E.; Arndt, K.; Freedberg, I.M. The Natural History of Recurrent Facial-Oral Infection with Herpes Simplex Virus. J. Infect. Dis. 1978, 138, 897–965. [Google Scholar] [CrossRef]
- Spruance, S.L. Pathogenesis of herpes simplex labialis: Excretion of virus in the oral cavity. J. Clin. Microbiol. 1984, 19, 675–679. [Google Scholar] [CrossRef] [PubMed]
- Kriesel, J.D.; Pisani, P.L.; McKeough, M.B.; Baringer, J.R.; Spruance, S.L. Correlation between detection of herpes simplex virus in oral secretions by PCR and susceptibility to experimental UV radiation-induced herpes labialis. J. Clin. Microbiol. 1994, 32, 3088–3090. [Google Scholar] [CrossRef] [PubMed]
- Joseph, R.; Rose, F.C. Cluster headache and herpes simplex: An association? Br. Med. J. Clin. Res. Ed. 1985, 290, 1625–1626. [Google Scholar] [CrossRef][Green Version]
- Dreizen, S.; Bodey, G.P.; Valdivieso, M. Chemotherapy-associated oral infections in adults with solid tumors. Oral Surg. Oral Med. Oral Pathol. 1983, 55, 113–120. [Google Scholar] [CrossRef]
- Barrett, A.P. A long-term prospective clinical study of orofacial herpes simplex virus infection in acute leukemia. Oral Surg. Oral Med. Oral Pathol. 1986, 61, 149–152. [Google Scholar] [CrossRef]
- Montgomery, M.T.; Redding, S.W.; LeMaistre, C.F. The incidence of oral herpes simplex virus infection in patients undergoing cancer chemotherapy. Oral Surg. Oral Med. Oral Pathol. 1986, 61, 238–242. [Google Scholar] [CrossRef]
- Shepherd, J.P. The management of the oral complications of leukemia. Oral Surg. Oral Med. Oral Pathol. 1978, 45, 543–548. [Google Scholar] [CrossRef]
- Flowers, C.R.; Seidenfeld, J.; Bow, E.J.; Karten, C.; Gleason, C.; Hawley, D.K.; Kuderer, N.M.; Langston, A.A.; Marr, K.A.; Rolston, K.V.I.; et al. Antimicrobial Prophylaxis and Outpatient Management of Fever and Neutropenia in Adults Treated for Malignancy: American Society of Clinical Oncology Clinical Practice Guideline. J. Clin. Oncol. 2013, 31, 794–810. [Google Scholar] [CrossRef]
- Saral, R.; Ambinder, R.F.; Burns, W.H.; Angelopulos, C.M.; Griffin, D.E.; Burke, P.J.; Lietman, P.S. Acyclovir Prophylaxis Against Herpes Simplex Virus Infection in Patients with Leukemia. Ann. Intern. Med. 1983, 99, 773–776. [Google Scholar] [CrossRef]
- Ci, B.; Jc, W. Herpes simplex virus infection in the immunocompromised cancer patient. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 1991, 9, 1903–1915. [Google Scholar] [CrossRef]
- Saral, R.; Burns, W.H.; Prentice, H.G. Herpes virus infections: Clinical manifestations and therapeutic strategies in immunocompromised patients. Clin. Haematol. 1984, 13, 645–660. [Google Scholar] [PubMed]
- Lam, M.T.; Pazin, G.J.; Armstrong, J.A.; Ho, M. Herpes simplex infection in acute myelogenous leukemia and other hematologic malignancies: A prospective study. Cancer 1981, 48, 2168–2171. [Google Scholar] [CrossRef]
- Styczynski, J.; Reusser, P.; Einsele, H.; de la Camara, R.; Cordonnier, C.; Ward, K.N.; Ljungman, P.; Engelhard, D. Management of HSV, VZV and EBV infections in patients with hematological malignancies and after SCT: Guidelines from the Second European Conference on Infections in Leukemia. Bone Marrow Transplant. 2009, 43, 757–770. [Google Scholar] [CrossRef] [PubMed]
- Sandherr, M.; Einsele, H.; Hebart, H.; Kahl, C.; Kern, W.; Kiehl, M.; Massenkeil, G.; Penack, O.; Schiel, X.; Schuettrumpf, S.; et al. Antiviral prophylaxis in patients with haematological malignancies and solid tumours: Guidelines of the Infectious Diseases Working Party (AGIHO) of the German Society for Hematology and Oncology (DGHO). Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 2006, 17, 1051–1059. [Google Scholar] [CrossRef]
- Ljungman, P. Risk assessment in haematopoietic stem cell transplantation: Viral status. Best Pract. Res. Clin. Haematol. 2007, 20, 209–217. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention; Infectious Disease Society of America; American Society of Blood and Marrow Transplantation. Guidelines for preventing opportunistic infections among hematopoietic stem cell transplant recipients. MMWR Recomm. Rep. 2000, 49, 1–125. [Google Scholar]
- Opstelten, W.; Neven, A.K.; Eekhof, J. Treatment and prevention of herpes labialis. Can. Fam. Physician 2008, 54, 1683–1687. [Google Scholar]
- Kimberlin, D.W.; Whitley, R.J. Antiviral therapy of HSV-1 and -2. In Human Herpesviruses: Biology, Therapy, and Immunoprophylaxis; Arvin, A., Campadelli-Fiume, G., Mocarski, E., Moore, P.S., Roizman, B., Whitley, R., Yamanishi, K., Eds.; Cambridge University Press: Cambridge, UK, 2007; ISBN 978-0-521-82714-0. [Google Scholar]
- Laskin, O.L. Clinical Pharmacokinetics of Acyclovir. Clin. Pharmacokinet. 1983, 8, 187–201. [Google Scholar] [CrossRef] [PubMed]
- Cernik, C.; Gallina, K.; Brodell, R.T. The treatment of herpes simplex infections: An evidence-based review. Arch. Intern. Med. 2008, 168, 1137–1144. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions: Cochrane Book Series; John and Wiley and Sons: Hoboken, NJ, USA, 2008; p. 674. [Google Scholar]
- Hutton, B.; Salanti, G.; Caldwell, D.M.; Chaimani, A.; Schmid, C.H.; Cameron, C.; Ioannidis, J.P.A.; Straus, S.; Thorlund, K.; Jansen, J.P.; et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: Checklist and explanations. Ann. Intern. Med. 2015, 162, 777–784. [Google Scholar] [CrossRef] [PubMed]
- McCoy, C.E. Understanding the Intention-to-treat Principle in Randomized Controlled Trials. West. J. Emerg. Med. 2017, 18, 1075–1078. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366. [Google Scholar] [CrossRef] [PubMed]
- Simultaneous Comparison of Multiple Treatments: Combining Direct and Indirect Evidence—PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/16223826/ (accessed on 27 July 2020).
- Hoaglin, D.C.; Hawkins, N.; Jansen, J.P.; Scott, D.A.; Itzler, R.; Cappelleri, J.C.; Boersma, C.; Thompson, D.; Larholt, K.M.; Diaz, M.; et al. Conducting indirect-treatment-comparison and network-meta-analysis studies: Report of the ISPOR Task Force on Indirect Treatment Comparisons Good Research Practices: Part 2. Value Health J. Int. Soc. Pharm. Outcomes Res. 2011, 14, 429–437. [Google Scholar] [CrossRef] [PubMed]
- Gluckman, E.; Lotsberg, J.; Devergie, A.; Zhao, X.M.; Melo, R.; Gomez-Morales, M.; Mazeron, M.C.; Perol, Y. Oral acyclovir prophylactic treatment of herpes simplex infection after bone marrow transplantation. J. Antimicrob. Chemother. 1983, 12, 161–167. [Google Scholar] [CrossRef] [PubMed]
- Bergmann, O.J.; Ellermann-Eriksen, S.; Mogensen, S.C.; Ellegaard, J. Acyclovir given as prophylaxis against oral ulcers in acute myeloid leukaemia: Randomised, double blind, placebo controlled trial. BMJ 1995, 310, 1169–1172. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Prentice, H.G.; Hann, I.M. Prophylactic studies against herpes infections in severely immunocompromised patients with acyclovir. J. Infect. 1983, 6, 17–21. [Google Scholar] [CrossRef]
- Laskin, O.L.; Saral, R.; Burns, W.H.; Angelopulos, C.M.; Lietman, P.S. Acyclovir concentrations and tolerance during repetitive administration for 18 days. Am. J. Med. 1982, 73, 221–224. [Google Scholar] [CrossRef]
- Gluckman, E.; Devergie, A.; Melo, R.; Nebout, T.; Lotsberg, J.; Zhao, X.M.; Gomez-Morales, M.; Mazeron, M.C.; Perol, Y. Prophylaxis of herpes infections after bone-marrow transplantation by oral acyclovir. Lancet 1983, 322, 706–708. [Google Scholar] [CrossRef]
- Hann, I.M.; Prentice, H.G.; Blacklock, H.A.; Ross, M.G.; Brigden, D.; Rosling, A.E.; Burke, C.; Crawford, D.H.; Brumfitt, W.; Hoffbrand, A.V. Acyclovir prophylaxis against herpes virus infections in severely immunocompromised patients: Randomised double blind trial. Br. Med. J. Clin. Res. Ed. 1983, 287, 384–388. [Google Scholar] [CrossRef] [PubMed]
- Prentice, H.G. Use of acyclovir for prophylaxis of herpes infections in severely immunocompromised patients. J. Antimicrob. Chemother. 1983, 12, 153–159. [Google Scholar] [CrossRef] [PubMed]
- Anderson, H.; Scarffe, J.H.; Sutton, R.N.; Hickmott, E.; Brigden, D.; Burke, C. Oral acyclovir prophylaxis against herpes simplex virus in non-Hodgkin lymphoma and acute lymphoblastic leukaemia patients receiving remission induction chemotherapy. A randomised double blind, placebo controlled trial. Br. J. Cancer 1984, 50, 45–49. [Google Scholar] [CrossRef] [PubMed]
- Wade, J.C.; Newton, B.; Flournoy, N.; Meyers, J.D. Oral Acyclovir for Prevention of Herpes Simplex Virus Reactivation after Marrow Transplantation. Ann. Intern. Med. 1984, 100, 823–828. [Google Scholar] [CrossRef] [PubMed]
- Lundgren, G.; Wilczek, H.; Lönnqvist, B.; Lindholm, A.; Wahren, B.; Ringdén, O. Acyclovir prophylaxis in bone marrow transplant recipients. Scand. J. Infect. Dis. Suppl. 1985, 47, 137–144. [Google Scholar] [PubMed]
- Shepp, D.H.; Dandliker, P.S.; Flournoy, N.; Meyers, J.D. Once-daily intravenous acyclovir for prophylaxis of herpes simplex virus reactivation after marrow transplantation. J. Antimicrob. Chemother. 1985, 16, 389–395. [Google Scholar] [CrossRef] [PubMed]
- Shepp, D.H.; Dandliker, P.S.; Flournoy, N.; Meyers, J.D. Sequential intravenous and twice-daily oral acyclovir for extended prophylaxis of herpes simplex virus infection in marrow transplant patients. Transplantation 1987, 43, 654–658. [Google Scholar] [CrossRef] [PubMed]
- Bubley, G.J.; Chapman, B.; Chapman, S.K.; Crumpacker, C.S.; Schnipper, L.E. Effect of acyclovir on radiation- and chemotherapy-induced mouth lesions. Antimicrob. Agents Chemother. 1989, 33, 862–865. [Google Scholar] [CrossRef] [PubMed]
- Selby, P.J.; Powles, R.L.; Easton, D.; Perren, T.J.; Stolle, K.; Jameson, B.; Fiddian, A.P.; Tryhorn, Y.; Stern, H. The prophylactic role of intravenous and long-term oral acyclovir after allogeneic bone marrow transplantation. Br. J. Cancer 1989, 59, 434–438. [Google Scholar] [CrossRef]
- Lönnqvist, B.; Palmblad, J.; Ljungman, P.; Grimfors, G.; Järnmark, M.; Lerner, R.; Nyström-Rosander, C.; Öberg, G. The Leukemia Group of Middle Sweden Oral acyclovir as prophylaxis for bacterial infections during induction therapy for acute leukaemia in adults. Support. Care Cancer 1993, 1, 139–144. [Google Scholar] [CrossRef]
- Bergmann, O.J.; Mogensen, S.C.; Ellermann-Eriksen, S.; Ellegaard, J. Acyclovir prophylaxis and fever during remission-induction therapy of patients with acute myeloid leukemia: A randomized, double-blind, placebo-controlled trial. J. Clin. Oncol. 1997, 15, 2269–2274. [Google Scholar] [CrossRef]
- Liesveld, J.L.; Abboud, C.N.; Ifthikharuddin, J.J.; Lancet, J.E.; Wedow, L.A.; Oliva, J.; Stamm, C.G.; Nichols, D. Oral valacyclovir versus intravenous acyclovir in preventing herpes simplex virus infections in autologous stem cell transplant recipients. Biol. Blood Marrow Transplant. 2002, 8, 662–665. [Google Scholar] [CrossRef][Green Version]
- Warkentin, D.I.; Epstein, J.B.; Campbell, L.M.; Yip, J.G.; Cox, V.C.; Ransier, A.; Barnett, M.J.; Marra, F. Valacyclovir versus acyclovir for HSV prophylaxisin neutropenic patients. Ann. Pharmacother. 2002, 36, 1525–1531. [Google Scholar] [CrossRef] [PubMed]
- Orlowski, R.; Mills, S.; Hartley, E.; Ye, X.; Piantadosi, S.; Ambinder, R.; Gore, S.; Miller, C. Oral Valacyclovir as Prophylaxis against Herpes Simplex Virus Reactivation During High Dose Chemotherapy for Leukemia. Leuk. Lymphoma 2004, 45, 2215–2219. [Google Scholar] [CrossRef] [PubMed]
- Wade, J.C.; Newton, B.; McLAREN, C.; Flournoy, N.; Keeney, R.E.; Meyers, J.D. Intravenous Acyclovir to Treat Mucocutaneous Herpes Simplex Virus Infection After Marrow Transplantation. Ann. Intern. Med. 1982, 96, 265–269. [Google Scholar] [CrossRef] [PubMed]
- Shepp, D.H.; Newton, B.A.; Dandliker, P.S.; Flournoy, N.; Meyers, J.D. Oral acyclovir therapy for mucocutaneous herpes simplex virus infections in immunocompromised marrow transplant recipients. Ann. Intern. Med. 1985, 102, 783–785. [Google Scholar] [CrossRef] [PubMed]
- Izzedine, H.; Perazella, M.A. Anticancer Drug-Induced Acute Kidney Injury. Kidney Int. Rep. 2017, 2, 504–514. [Google Scholar] [CrossRef] [PubMed]
- Zeng, L.; Nath, C.E.; Blair, E.Y.L.; Shaw, P.J.; Stephen, K.; Earl, J.W.; Coakley, J.C.; McLachlan, A.J. Population Pharmacokinetics of Acyclovir in Children and Young People with Malignancy after Administration of Intravenous Acyclovir or Oral Valacyclovir. Antimicrob. Agents Chemother. 2009, 53, 2918–2927. [Google Scholar] [CrossRef] [PubMed]
- Höglund, M.; Ljungman, P.; Weller, S. Comparable aciclovir exposures produced by oral valaciclovir and intravenous aciclovir in immunocompromised cancer patients. J. Antimicrob. Chemother. 2001, 47, 855–861. [Google Scholar] [CrossRef]
- Eisen, D.; Essell, J.; Broun, E.; Sigmund, D.; DeVoe, M. Clinical Utility of Oral Valacyclovir Compared with Oral Acyclovir for the Prevention of Herpes Simplex Virus Mucositis Following Autologous Bone Marrow Transplantation or Stem Cell Rescue Therapy. Available online: https://pubmed.ncbi.nlm.nih.gov/12621507/ (accessed on 28 July 2020).
- Talwani, R.; Gilliam, B.L.; Howell, C. Infectious Diseases and the Liver. Clin. Liver Dis. 2011, 15, 111–130. [Google Scholar] [CrossRef]
- Acyclovir. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury; National Institute of Diabetes and Digestive and Kidney Diseases: Bethesda, MD, USA, 2012. [Google Scholar]
- Yildiz, C.; Ozsurekci, Y.; Gucer, S.; Cengiz, A.B.; Topaloglu, R. Acute kidney injury due to acyclovir. CEN Case Rep. 2012, 2, 38–40. [Google Scholar] [CrossRef]
- Fleischer, R.; Johnson, M. Acyclovir Nephrotoxicity: A Case Report Highlighting the Importance of Prevention, Detection, and Treatment of Acyclovir-Induced Nephropathy. Case Rep. Med. 2010, 2010. [Google Scholar] [CrossRef]
- Adair, J.C.; Gold, M.; Bond, R.E. Acyclovir neurotoxicity: Clinical experience and review of the literature. South Med. J. 1994, 87, 1227–1231. [Google Scholar] [CrossRef] [PubMed]
- Dubrofsky, L.; Kerzner, R.S.; Delaunay, C.; Kolenda, C.; Pepin, J.; Schwartz, B.C. Interdisciplinary Systems-Based Intervention to Improve IV Hydration during Parenteral Administration of Acyclovir. Can. J. Hosp. Pharm. 2016, 69, 7–13. [Google Scholar] [CrossRef]
- Baden, L.R.; Swaminathan, S.; Angarone, M.; Blouin, G.; Camins, B.C.; Casper, C.; Cooper, B.; Dubberke, E.R.; Engemann, A.M.; Freifeld, A.G.; et al. Prevention and Treatment of Cancer-Related Infections, Version 2.2016, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Cancer Netw. JNCCN 2016, 14, 882–913. [Google Scholar] [CrossRef] [PubMed]
- Hadorn, D.C.; Baker, D.; Hodges, J.S.; Hicks, N. Rating the quality of evidence for clinical practice guidelines. J. Clin. Epidemiol. 1996, 49, 749–754. [Google Scholar] [CrossRef]
- Lalla, R.V.; Bowen, J.; Barasch, A.; Elting, L.; Epstein, J.; Keefe, D.M.; McGuire, D.B.; Migliorati, C.; Nicolatou-Galitis, O.; Peterson, D.E.; et al. MASCC/ISOO clinical practice guidelines for the management of mucositis secondary to cancer therapy: MASCC/ISOO Mucositis Guidelines. Cancer 2014, 120, 1453–1461. [Google Scholar] [CrossRef]
- Glenny, A.-M.; Fernandez Mauleffinch, L.M.; Pavitt, S.; Walsh, T. Interventions for the prevention and treatment of herpes simplex virus in patients being treated for cancer. Cochrane Database Syst. Rev. 2009, CD006706. [Google Scholar] [CrossRef] [PubMed]
- Yahav, D.; Gafter-Gvili, A.; Muchtar, E.; Skalsky, K.; Kariv, G.; Yeshurun, M.; Leibovici, L.; Paul, M. Antiviral prophylaxis in haematological patients: Systematic review and meta-analysis. Eur. J. Cancer Oxf. Engl. 1990 2009, 45, 3131–3148. [Google Scholar] [CrossRef]
- Djuric, M.; Jankovic, L.; Jovanovic, T.; Pavlica, D.; Brkic, S.; Knezevic, A.; Markovic, D.; Milasin, J. Prevalence of oral herpes simplex virus reactivation in cancer patients: A comparison of different techniques of viral detection. J. Oral Pathol. Med. Off. Publ. Int. Assoc. Oral Pathol. Am. Acad. Oral Pathol. 2009, 38, 167–173. [Google Scholar] [CrossRef]
- Gopalakrishnan, S.; Ganeshkumar, P. Systematic Reviews and Meta-analysis: Understanding the Best Evidence in Primary Healthcare. J. Fam. Med. Prim. Care 2013, 2, 9–14. [Google Scholar] [CrossRef]
- Zafari, Z.; Thorlund, K.; FitzGerald, J.M.; Marra, C.A.; Sadatsafavi, M. Network vs. pairwise meta-analyses: A case study of the impact of an evidence-synthesis paradigm on value of information outcomes. Pharmacoeconomics 2014, 32, 995–1004. [Google Scholar] [CrossRef]
- Puhan, M.A.; Schünemann, H.J.; Murad, M.H.; Li, T.; Brignardello-Petersen, R.; Singh, J.A.; Kessels, A.G.; Guyatt, G.H. GRADE Working Group A GRADE Working Group approach for rating the quality of treatment effect estimates from network meta-analysis. BMJ 2014, 349, g5630. [Google Scholar] [CrossRef] [PubMed]
- Dignani, M.C.; Mykietiuk, A.; Michelet, M.; Intile, D.; Mammana, L.; Desmery, P.; Milone, G.; Pavlovsky, S. Valacyclovir prophylaxis for the prevention of Herpes simplex virus reactivation in recipients of progenitor cells transplantation. Bone Marrow Transplant. 2002, 29, 263–267. [Google Scholar] [CrossRef] [PubMed]
- Hong, J.; Park, H.-K.; Park, S.; Lee, A.; Lee, Y.-H.; Shin, D.-Y.; Koh, Y.; Choi, J.-Y.; Yoon, S.-S.; Choi, Y.; et al. Strong association between herpes simplex virus-1 and chemotherapy-induced oral mucositis in patients with hematologic malignancies. Korean J. Intern. Med. 2020, 35, 1188–1198. [Google Scholar] [CrossRef] [PubMed]


| Author (Year) | Country | Study Design | Study Comparison | Antiviral: Dose and Duration | Sample Size | Dropout Rate | Outcome: Oral HSV Infection | Duration of Treatment |
|---|---|---|---|---|---|---|---|---|
| Prevention of oral HSV infection | ||||||||
| SARAL et al., 1983 [20] | US, Maryland | randomized, double-blind, placebo controlled | ACY vs. PBO | IV ACY 250 mg/m2 body surface area, three times daily | 30 | 3% | ACY: 0/15 PBO:11/15 | 32 days or until discharged from the hospital or until a culture-positive herpes simplex virus infection was found |
| Hann et al., 1983 [43] | London | randomized, double-blind | ACY vs. PBO | IV ACY, 5 mg/kg, twice daily | 60 | 1.6% | ACY: 2/29 PBO:15/30 | 14 months |
| Bergmann et al.,1997 [53] | Denmark | randomized, double-blind, placebo controlled | ACY vs. PBO | O-ACY 400 mg, twice daily | 90 | 0% | ACY: 1/45 PBO: 8/45 | 28 days |
| G Lundgren et al., 1985 [47] | Sweden | randomized, double-blind and placebo controlled | ACY vs. PBO | IV ACY at a dose of 250 mg/m2, twice daily | 42 | 0% | ACY: 1/20 PBO: 6/22 | 6 months |
| Saral et al., 1981 [41] | US | double-blind | ACY vs. PBO | IV 250 mg/m2 acyclovir, every eight hours | 20 | 0% | ACY: 0/10 PBO: 7/10 | 18 days |
| Bubley et al., 1989 [50] | US | randomized, double-blind, placebo controlled | ACY vs. PBO | O-ACY as four 200-mg capsules, twice daily | 57 | 17.5% | ACY: 0/27 PBO: 5/30 | 7 weeks |
| Shepp et al., 1985 [48] | US | randomized, double-blind | ACY vs. PBO | IV ACY 250 mg/m2, once daily | 30 | 10% | ACY: 6/14 PBO: 9/13 | 4 weeks |
| Lonnqvis et al., 1993 [52] | Sweden | double-blind | ACY vs. PBO | O-ACY 200 mg, four times daily | 116 | 7.7% | ACY: 0/52 PBO:15/55 | Duration varied |
| WADE et al., 1984 [46] | US | double-blind | ACY vs. PBO | O-ACY 400 mg, every four hours | 49 | 0% | ACY: 5/24 PBO:17/25 | 35 days |
| Gluckman et al., 1983 [42] | France | double-blind | ACY vs. PBO | O-ACY 200 mg, every six hours | 40 | 2.5% | ACY: 0/20 PBO:13/20 | from day 8 to day 35 after transplant |
| Anderson et al., 1984 [45] | UK | double-blind | ACY vs. PBO | O-ACY 200 mg four times daily | 41 | 2.5% | ACY: 1/20 PBO: 12/20 | 6 weeks |
| Liesveld et al., 2002 [54] | US | randomized open label | VAL vs. ACY | O-VAL 1 g, twice daily; IV-ACY 250 mg/m2, twice daily | 30 | 3.3% | VAL: 0/14 ACY: 0/16 | until the day of engraftment |
| Prentice et al., 1983 [44] | London | randomized placebo-controlled | ACY vs. PBO | IV-ACY 5 mg/kg infused over one hour, once daily | 60 | 1.6% | ACY: 2/29 PBO:15/30 | during the period of neutropenia |
| Shepp et al., 1987 [49] | US | double-blind | ACY vs. PBO | O-ACY 800 mg, twice daily | 51 | 31% | ACY: 7/25 PBO:12/26 | from day 31 till 75 days |
| Selby et al., 1989 [51] | UK | double-blind | ACY VS. PBO | IV acyclovir 5 mg kg three times daily. Children less than 12 years received 250 mg/m2, followed by 400 mg orally 6-hourly. | 82 | 0% | ACY: 9/42 PBO:17/40 | Over one year |
| Warkentin et al., 2002 [55] | Canada | single-blind, randomized, 3-group clinical trial | VAL 500 VS. VAL 250 VS. ACY 400 | O-VAL (500 mg twice daily); O-VAL (250 mg twice daily); O-ACY (400 mg thrice daily) | 151 | 0% | VAL 500 mg: 8/48 VAL 250 mg:2/52 ACY: 2/52 | Duration varied |
| Orlowski et al. [56] | Sidney | randomized open label | VAL 500 vs. VAL 1000 | Every 8 h | 81 | 14.8% | VAL 500 mg: 0/40 VAL 1000 mg: 0/41 | 1979 days |
| Treatment of oral HSV infection | ||||||||
| Wade et al., 1982 [57] | US | randomized, double-blind | ACY vs. PBO | IV-ACY 750 mg/m2 body surface area once daily | 31 | 0% | ACY:15/17 PBO:16/17 | 7 days |
| Shepp et al., 1985 [58] | - | randomized, double-blinded, placebo-controlled | ACY vs. PBO | O-ACY 400 mg five times daily | 21 | 0% | - | 10 days |
| Author | Year | Random Sequence Generation | Allocation Concealment | Blinding of Participants and Personnel | Blinding of Outcome Assessment | Incomplete Outcome Data | Selective Reporting | Overall Bias |
|---|---|---|---|---|---|---|---|---|
| Saral | 1983 | + | ? | + | + | + | + | ? |
| Hann | 1983 | + | ? | + | + | + | ? | - |
| Bergmann | 1997 | + | ? | + | + | + | + | ? |
| G Lundgren | 1985 | ? | + | + | + | + | + | ? |
| Bubley | 1989 | + | + | + | + | ? | - | - |
| Wade | 1984 | ? | ? | + | + | + | + | - |
| Anderson | 1984 | ? | ? | + | + | + | - | - |
| Shepp | 1987 | ? | ? | + | + | - | ? | - |
| Liesveld | 2002 | + | + | - | - | + | + | - |
| Selby | 1989 | + | ? | + | + | ? | ? | - |
| Warkentin | 2002 | ? | ? | ? | + | + | + | - |
| Saral | 1981 | + | ? | + | + | + | + | ? |
| Shepp | 1985 | + | ? | + | + | - | ? | - |
| Lonnqvis | 1993 | + | + | + | + | + | ? | ? |
| Prentice | 1983 | ? | ? | ? | ? | + | ? | ? |
| Gluckman | 1983 | ? | ? | + | + | + | - | - |
 Low risk,
Low risk,  High risk,
High risk,  unclear.
unclear.| ACY | 0.79 (0.27, 2.27) | 0.18 (0.12, 0.27) |
| 0.79 (0.25, 2.48) | VAL | NA |
| 0.17 (0.10, 0.30) | 0.22 (0.06, 0.78) | PBO |
| Intervention | Incidence of Herpes Simplex Virus | |
|---|---|---|
| RR (95% CI) | SUCRA Rank (Score) | |
| ACY | 0.17 (0.10, 0.30) | 1 (0.83) |
| VAL | 0.22 (0.06, 0.77) | 2 (0.66) |
| PBO | Reference | 3 (0.005) |
| Overall inconsistency Chi-square (p value) | 1.87 (0.60) | |
| Number of studies | 16 | |
| IV-ACY10MG/KG | NA | NA | NA | NA | NA | NA | 0.14 (0.05, 0.37) |
| 0.33 (0.09, 1.27) | IV-ACY250MG/M2 | NA | NA | NA | NA | NA | 0.41 (0.17, 1.02) |
| 0.63 (0.06, 6.13) | 1.88 (0.20, 17.79) | IV-ACY500MG/M2 | NA | NA | NA | NA | 0.22 (0.03, 1.73) |
| 2.48 (0.28, 21.74) | 7.42 (0.87, 62.95) | 3.96 (0.23, 66.89) | IV-ACY750MG/M2 | NA | NA | NA | 0.06 (0.01, 0.39) |
| 2.25 (0.25, 20.58) | 6.72 (0.76, 59.63) | 3.58 (0.20, 62.69) | 0.91 (0.06, 14.53) | O-ACY1600 | NA | NA | 0.06 (0.01, 0.45) |
| 0.75 (0.17, 3.25) | 2.25 (0.54, 9.27) | 1.20 (0.12, 12.32) | 0.30 (0.03, 2.80) | 0.33 (0.03, 3.22) | O-ACY2000 | NA | 0.18 (0.06, 0.55) |
| 1.95 (0.43, 8.76) | 5.82 (1.36, 25.00) | 3.10 (0.29, 32.72) | 0.78 (0.08, 7.44) | 0.87 (0.09, 8.57) | 2.59 (0.53, 12.60) | O-ACY800 | 0.07 (0.02, 0.22) |
| 0.14 (0.05, 0.37) | 0.41 (0.17, 1.02) | 0.22 (0.03, 1.73) | 0.06 (0.01, 0.39) | 0.06 (0.01, 0.45) | 0.18 (0.06, 0.55) | 0.07 (0.02, 0.22) | PBO |
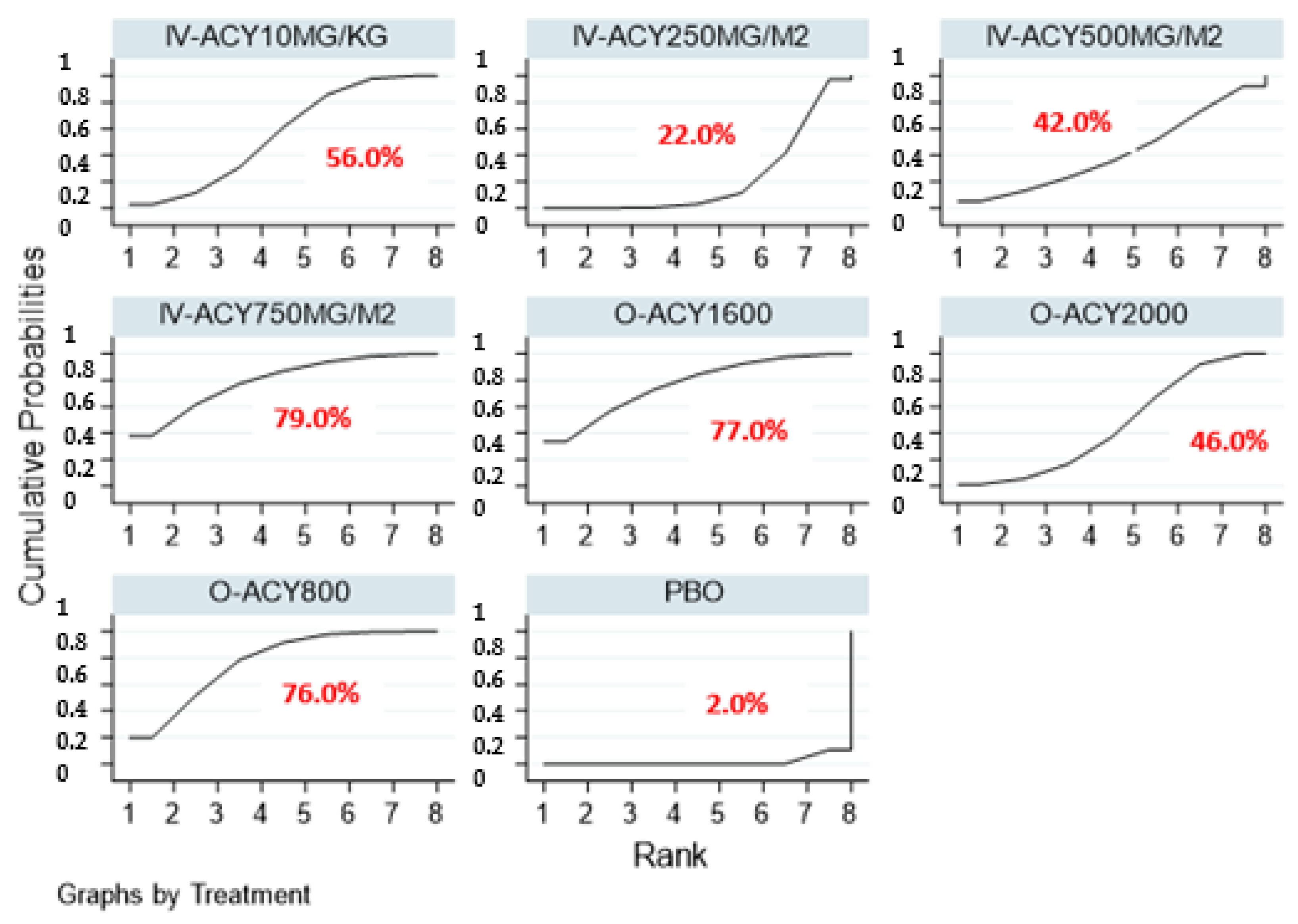
| Intervention | Incidence of Herpes Simplex Virus | |
|---|---|---|
| RR (95% CI) | SUCRA Rank (Score) | |
| IV-ACY 750MG/M2 | 0.06 (0.01, 0.39) | 1 (0.79) |
| O-ACY 1600 | 0.06 (0.01, 0.45) | 2 (0.77) |
| O-ACY 800 | 0.07 (0.02, 0.22) | 3 (0.76) |
| IV-ACY 10MG/KG | 0.14 (0.05, 0.37) | 4 (0.56) |
| O-ACY 2000 | 0.18 (0.06, 0.55) | 5 (0.46) |
| IV-ACY 500MG/M2 | 0.22 (0.03, 1.73) | 6 (0.42) |
| IV-ACY 250MG/M2 | 0.41 (0.17, 1.02) | 7 (0.22) |
| PBO | reference | 8 (0.02) |
| Overall inconsistency Chi-square (p value) | Inconsistency model requested, but there is no source of inconsistency. No tests were performed. | |
| Number of studies | 13 | |
| Network Outcome | Chi Square | p Value for Test of Global Inconsistency |
|---|---|---|
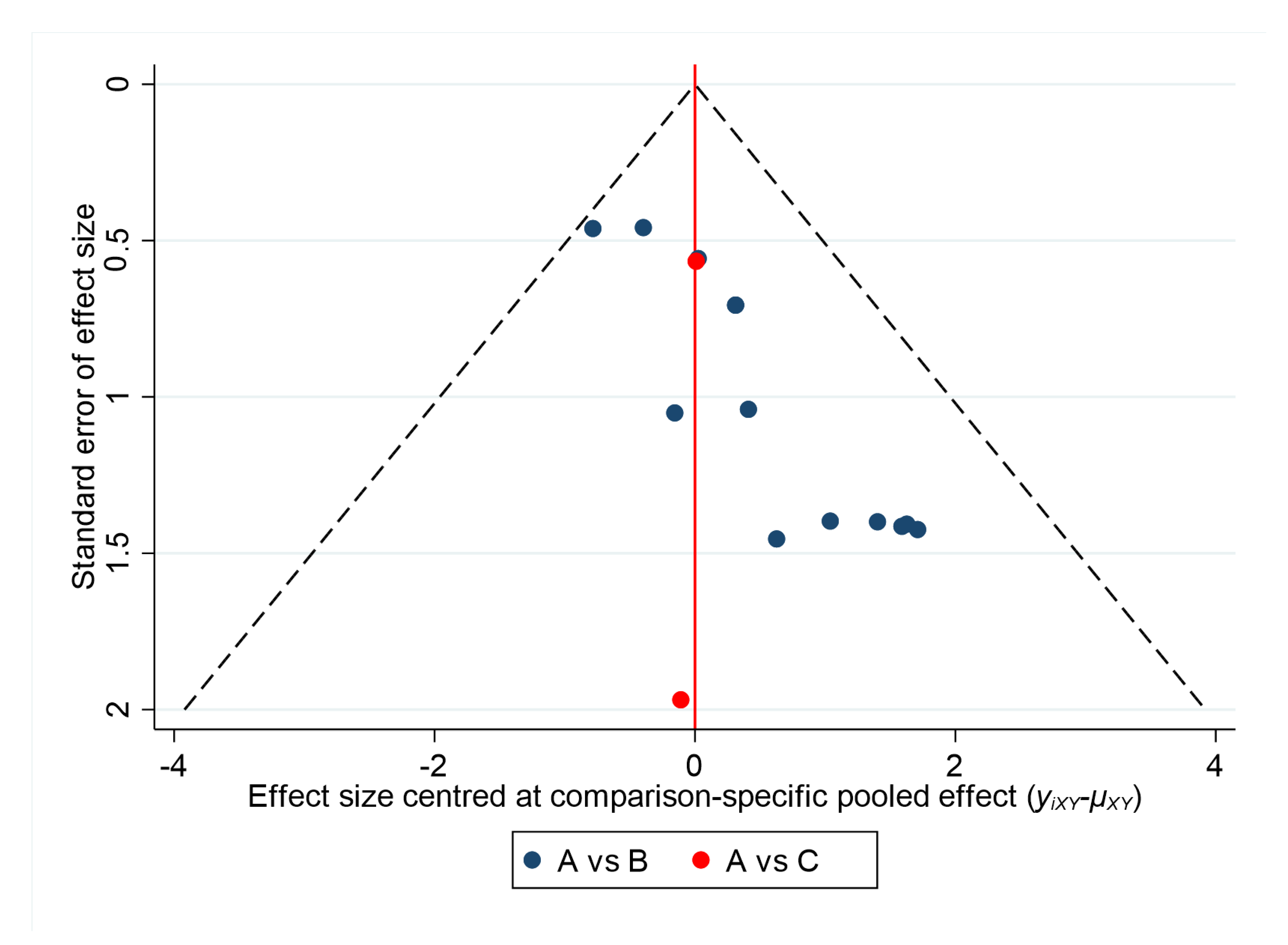
| Incidence of oral HSV by drug class | 1.87 | 0.60 |
| Incidence of oral HSV by dosage form and total daily dose | - | - |
| Comparison | Direct Evidence | Indirect Evidence | Network Meta-Analysis | |||
|---|---|---|---|---|---|---|
| Odds Ratio (95% Confidence Interval) | Quality of Evidence | Odds Ratio (95% Confidence Interval) | Quality of Evidence | Odds Ratio (95% Confidence Interval) | Quality of Evidence | |
| ACY vs. PBO | 0.18 (0.12, 0.28) | Moderate *,‡‡ | 0.17 (0.13, 0.24) | Moderate ¶,‡‡ | 0.17 (0.10, 0.30) | Moderate |
| ACY vs. VAL | 0.79 (0.27, 2.27) | Moderate * | 0.79 (0.01, 608.3) | Low ¶,‡‡,§ | 0.79 (0.25, 2.48) | Moderate |
| Comparison | Direct Evidence | Indirect Evidence | Network Meta-Analysis | |||
|---|---|---|---|---|---|---|
| Odds Ratio (95% Confidence Interval) | Quality of Evidence | Odds Ratio (95% Confidence Interval) | Quality of Evidence | Odds Ratio (95% Confidence Interval) | Quality of Evidence | |
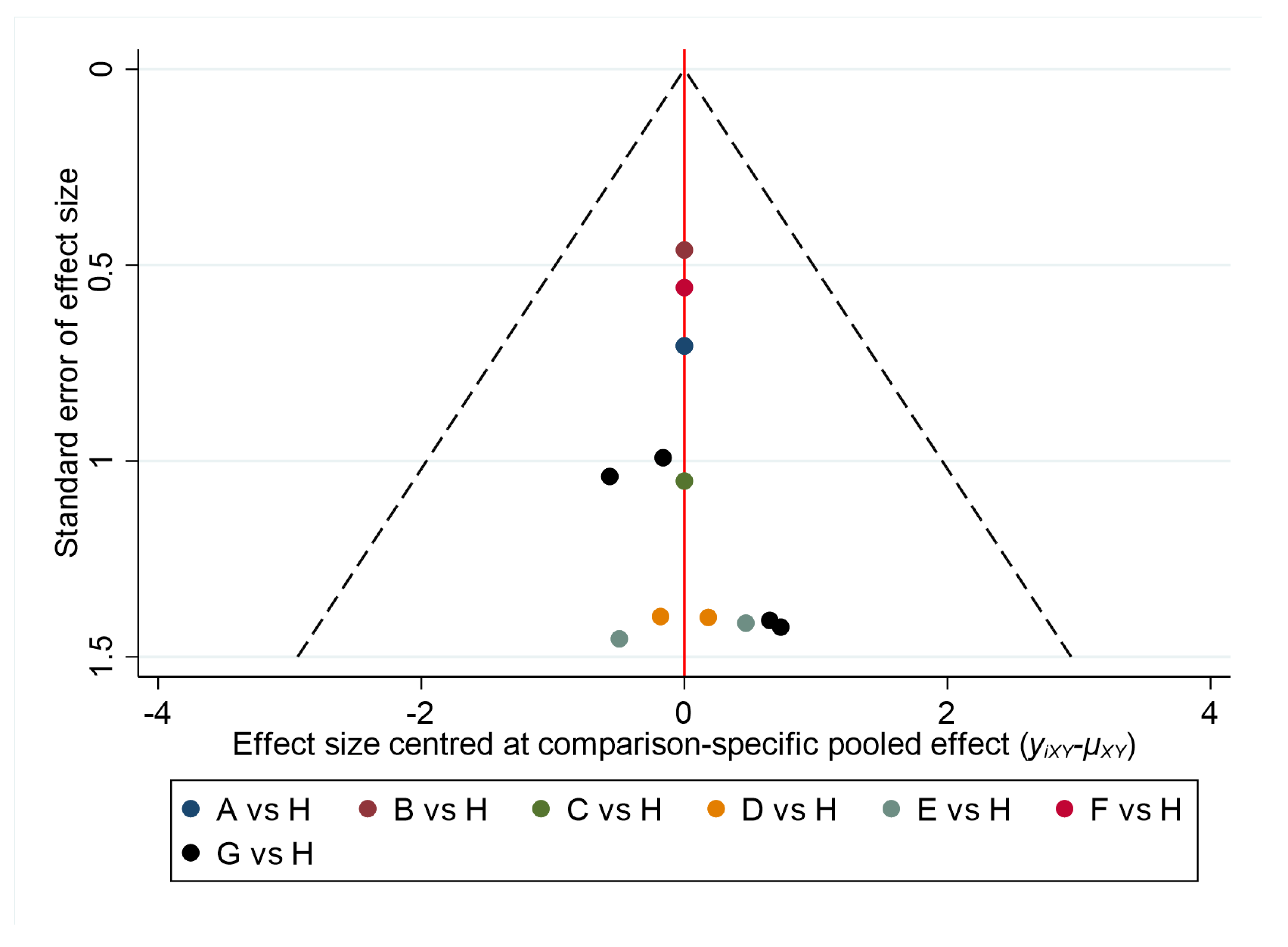
| IV-ACY 10MG/KG vs. PBO | 0.14 (0.05, 0.37) | High * | Not estimable †† | Not estimable †† | 0.14 (0.05, 0.37) | High |
| IV-ACY 250MG/M2 vs. PBO | 0.41 (0.17, 1.02) | Moderate *,‡ | Not estimable †† | Not estimable †† | 0.41 (0.17, 1.02) | Moderate |
| IV-ACY 500MG/M2 vs. PBO | 0.22 (0.03, 1.73) | Moderate *,‡ | Not estimable †† | Not estimable †† | 0.22 (0.03, 1.73) | Moderate |
| IV-ACY 750MG/M2 vs. PBO | 0.06 (0.01, 0.39) | High | Not estimable †† | Not estimable †† | 0.06 (0.01, 0.39) | High |
| O-ACY 1600 vs. PBO | 0.06 (0.01, 0.45) | Moderate *,‡‡ | Not estimable †† | Not estimable †† | 0.06 (0.01, 0.45) | Moderate |
| O-ACY 2000 vs. PBO | 0.18 (0.06, 0.55) | High * | Not estimable †† | Not estimable †† | 0.18 (0.06, 0.55) | High |
| O-ACY 800 vs. PBO | 0.05 (0.01, 0.22) | Moderate *,‡‡ | Not estimable †† | Not estimable†† | 0.07 (0.02, 0.22) | Moderate |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aribi Al-Zoobaee, F.W.; Yee Shen, L.; Veettil, S.K.; Gopinath, D.; Maharajan, M.K.; Kunnath Menon, R. Antiviral Agents for the Prevention and Treatment of Herpes Simplex Virus Type-1 Infection in Clinical Oncology: A Network Meta-Analysis. Int. J. Environ. Res. Public Health 2020, 17, 8891. https://doi.org/10.3390/ijerph17238891
Aribi Al-Zoobaee FW, Yee Shen L, Veettil SK, Gopinath D, Maharajan MK, Kunnath Menon R. Antiviral Agents for the Prevention and Treatment of Herpes Simplex Virus Type-1 Infection in Clinical Oncology: A Network Meta-Analysis. International Journal of Environmental Research and Public Health. 2020; 17(23):8891. https://doi.org/10.3390/ijerph17238891
Chicago/Turabian StyleAribi Al-Zoobaee, Farah Wasim, Loo Yee Shen, Sajesh K. Veettil, Divya Gopinath, Mari Kannan Maharajan, and Rohit Kunnath Menon. 2020. "Antiviral Agents for the Prevention and Treatment of Herpes Simplex Virus Type-1 Infection in Clinical Oncology: A Network Meta-Analysis" International Journal of Environmental Research and Public Health 17, no. 23: 8891. https://doi.org/10.3390/ijerph17238891
APA StyleAribi Al-Zoobaee, F. W., Yee Shen, L., Veettil, S. K., Gopinath, D., Maharajan, M. K., & Kunnath Menon, R. (2020). Antiviral Agents for the Prevention and Treatment of Herpes Simplex Virus Type-1 Infection in Clinical Oncology: A Network Meta-Analysis. International Journal of Environmental Research and Public Health, 17(23), 8891. https://doi.org/10.3390/ijerph17238891







