The Relationship between Obesity and Physical Activity of Children in the Spotlight of Their Parents’ Excessive Body Weight
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethics
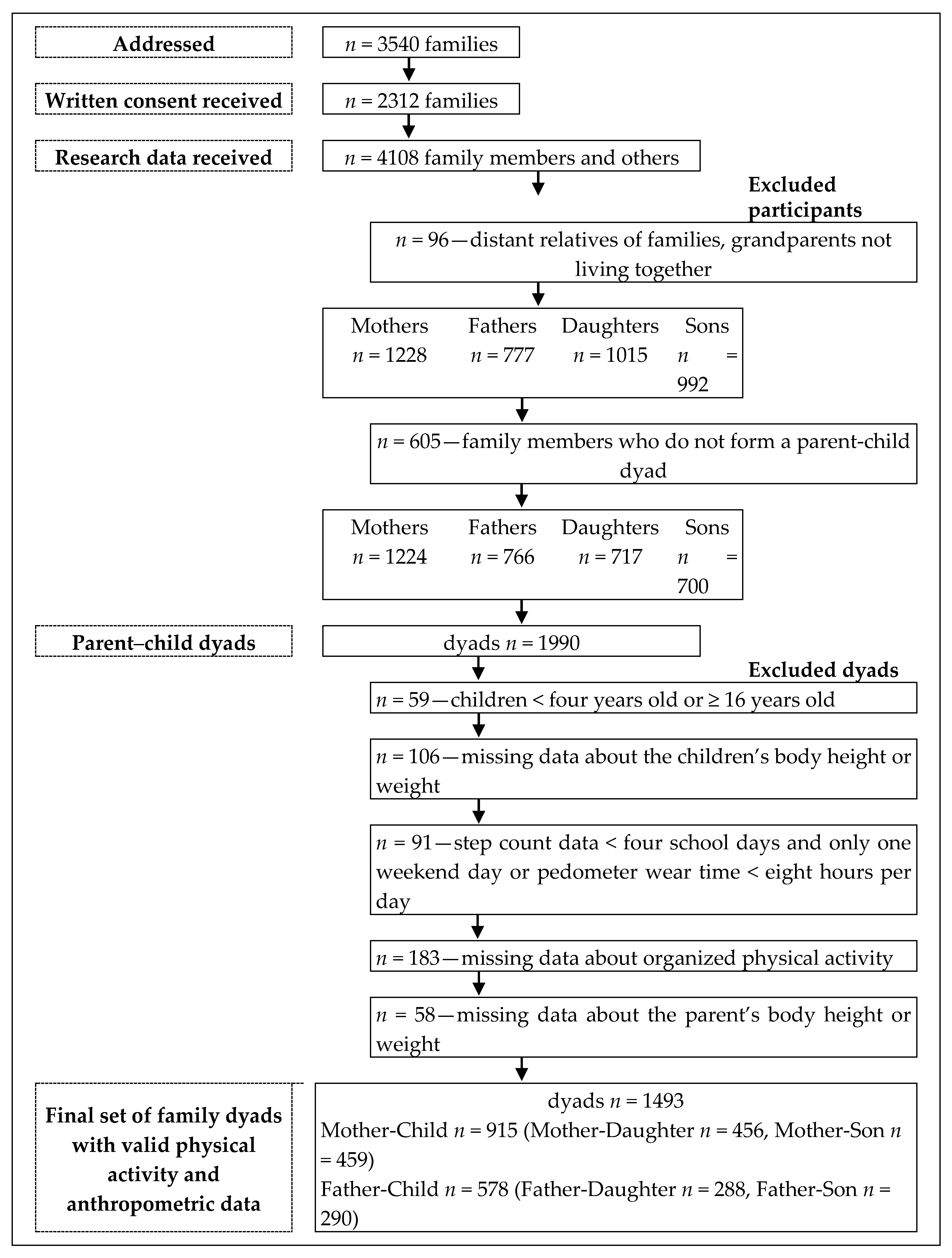
2.2. Participants and Inclusion/Exclusion Criteria
2.3. Procedures and Measurement
2.4. Data Processing and Statistical Analysis
3. Results
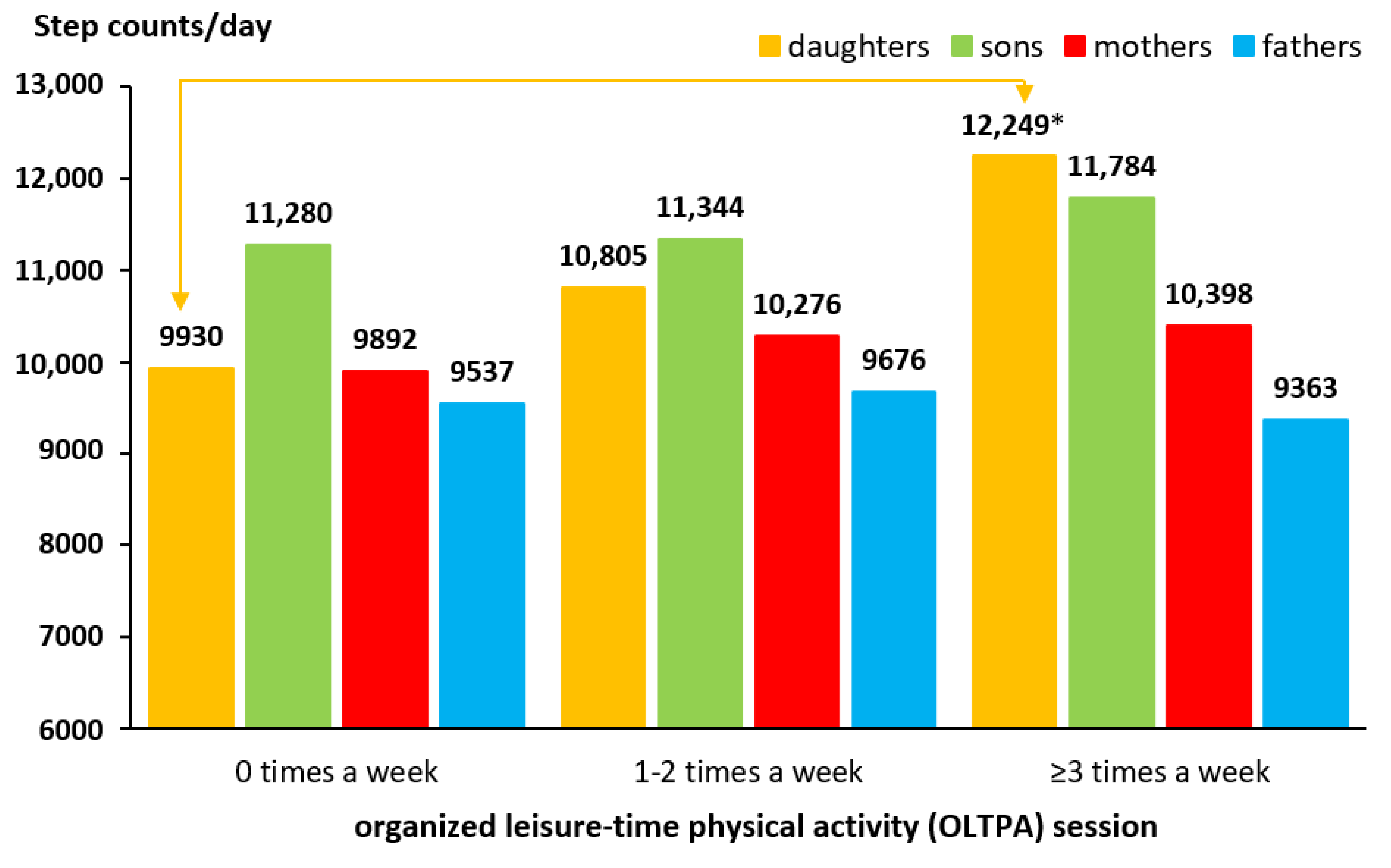
3.1. Daily SC of Family Members Separated by the Participation in OLTPA of Offspring
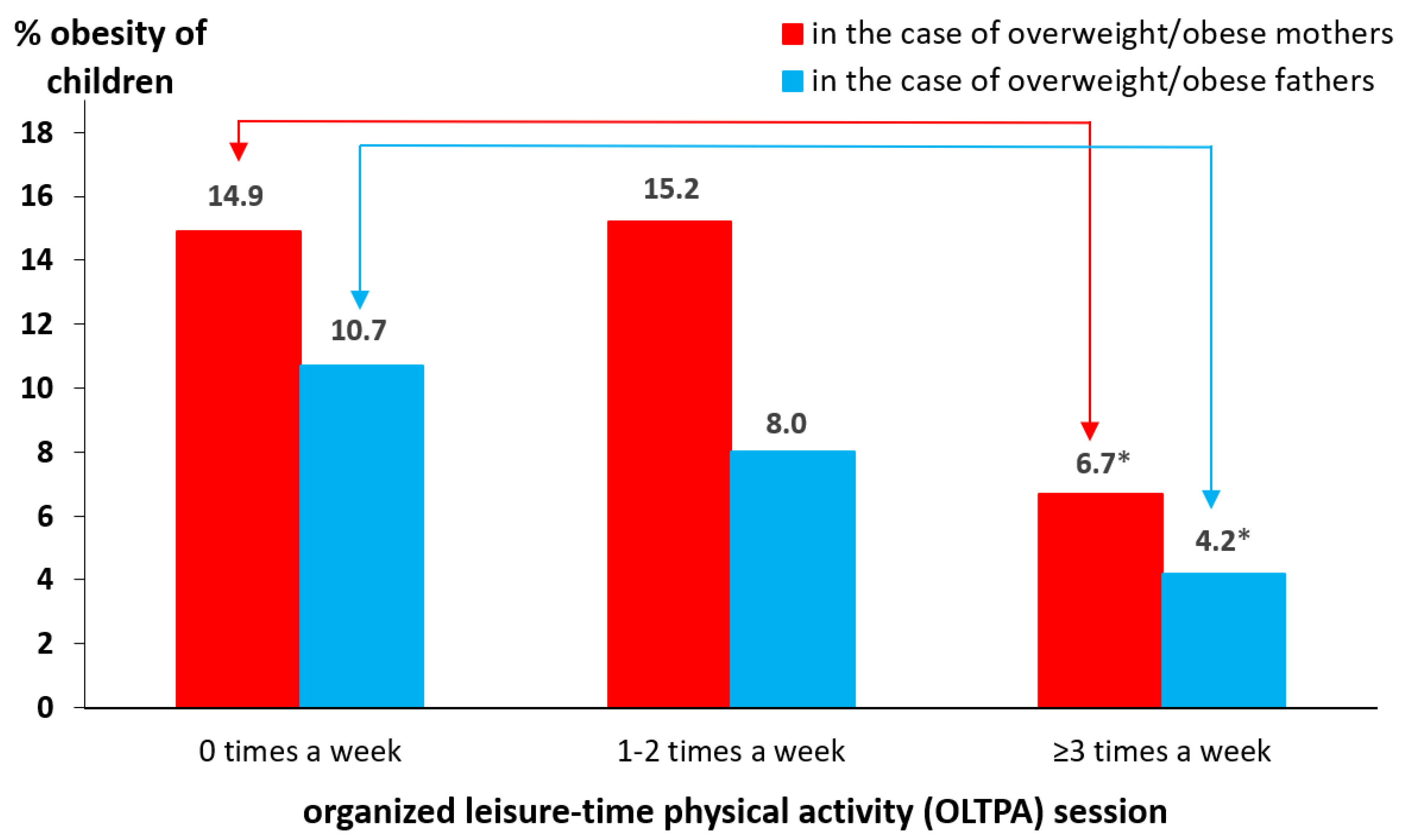
3.2. Prevalence of Obesity of Family Members Separated by the Participation in OLTPA of Offspring
3.3. Association between Child/Parent lifestyle indicators and Obesity of Offspring
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Logan, K.; Cuff, S.; Council on Sports Medicine and Fitness. Organized Sports for Children, Preadolescents, and Adolescents. Pediatrics 2019, 143, e20190997. [Google Scholar] [CrossRef] [PubMed]
- Brière, F.N.; Yale-Soulière, G.; Gonzalez-Sicilia, D.; Harbec, M.-J.; Morizot, J.; Janosz, M.; Pagani, L.S. Prospective associations between sport participation and psychological adjustment in adolescents. J. Epidemiol. Community Health 2018, 72, 575–581. [Google Scholar] [CrossRef] [PubMed]
- Vella, S.A.; Swann, C.; Allen, M.S.; Schweickle, M.J.; Magee, C.A. Bidirectional associations between sport involvement and mental health in adolescence. Med. Sci. Sports Exerc. 2017, 72, 687–694. [Google Scholar] [CrossRef] [PubMed]
- Wichstrøm, L.; von Soest, T.; Kvalem, I.L. Predictors of growth and decline in leisure time physical activity from adolescence to adulthood. Health Psychol. 2013, 32, 775–784. [Google Scholar] [CrossRef] [PubMed]
- Badura, P.; Sigmundova, D.; Sigmund, E.; Geckova, A.M.; van Dijk, J.P.; Reijneveld, S.A. Participation in organized leisure-time activities and risk behaviors in Czech adolescents. Int. J. Public Health 2016, 62, 387–396. [Google Scholar] [CrossRef]
- Lee, J.; Pope, Z.; Gao, Z. The role of youth sports in promoting children’s physical activity and preventing pediatric obesity: A systematic review. Behav. Med. 2018, 44, 62–76. [Google Scholar] [CrossRef]
- Dunton, G.; McConnell, R.; Jerrett, M.; Wolch, J.; Lam, C.; Gilliland, F.; Berhane, K. Organized physical activity in young school children predicts subsequent 4-year change in body mass index. Arch. Pediatrics Adolesc. Med. 2012, 166, 713–718. [Google Scholar] [CrossRef]
- Herbert, J.J.; Klakk, H.; Møller, N.C.; Grøntved, A.; Andersen, L.B.; Wedderkopp, N. The prospective association of organized sports participation with cardiovascular disease risk in children (the CHAMPS Study-DK). Mayo Clin. Proc. 2017, 92, 57–65. [Google Scholar] [CrossRef]
- Drenowatz, C.; Steiner, R.P.; Brandstetter, S.; Klenk, J.; Wabitsch, M.; Steinacker, J.M. Organized sports, overweight, and physical fitness in primary school children in Germany. J. Obes. 2013, 2013, 935245. [Google Scholar] [CrossRef]
- Basterfield, L.; Reilly, J.K.; Pearce, M.S.; Parkinson, K.N. Longitudinal associations between sports participation, body composition and physical activity from childhood to adolescence. J. Sci. Med. Sport. 2015, 18, 178–182. [Google Scholar] [CrossRef]
- Ara, I.; Vicente-Rodriguez, G.; Perez-Gomez, J.; Jimenez-Ramirez, J.; Serrano-Sanchez, J.A.; Dorado, C.; Calbet, J.A.L. Influence of extracurricular sport activities on body composition and physical fitness in boys: A 3-year longitudinal study. Int. J. Obes. 2006, 30, 1062–1071. [Google Scholar] [CrossRef] [PubMed]
- Matarma, T.; Tammelin, T.; Kulmala, J.; Koski, P.; Hurme, S.; Langström, H. Factors associated with objectively measured physical activity and sedentary time of 5–6-year-old children in the STEPS Study. Early Child Dev. Care 2017, 187, 1863–1873. [Google Scholar] [CrossRef]
- Erkelenz, N.; Kobel, S.; Kettner, S.; Drenowatz, C.; Steinacker, J.M.; The Research Group “Joint the Healthy Boat—Primary School”. Parental activity as influence on children’s BMI percentiles and physical activity. J. Sports Sci. Med. 2014, 13, 645–650. [Google Scholar] [PubMed]
- Rodrigues, D.; Padez, C.; Machado-Rodrigues, A.M. Active parents, active children: The importance of parental organized physical activity in children’s extracurricular sport participation. J. Child Health Care 2018, 22, 159–170. [Google Scholar] [CrossRef]
- Welk, G.; Wood, K.; Morss, G. Parental influences on physical activity in children: An exploration of potential mechanisms. Pediatrics Exerc. Sci. 2003, 15, 19–33. [Google Scholar] [CrossRef]
- Beets, M.W.; Cardinal, B.J.; Alderman, B.L. Parental social support and the physical activity-related behaviors of youth: A review. Health Educ. Behav. 2003, 37, 621–644. [Google Scholar] [CrossRef]
- Pyper, E.; Harrington, D.; Manson, H. The impact of different types of parental support behaviours on child physical activity, healthy eating, and screen time: A cross-sectional study. BMC Public Health 2016, 16, 568. [Google Scholar] [CrossRef]
- Sigmundová, D.; Sigmund, E.; Badura, P.; Hollein, T. Parent-child physical activity association in families with 4- to 16-year-old children. Int. J. Environ. Res. Public Health 2020, 17, 4015. [Google Scholar] [CrossRef]
- Bushnik, T.; Garriguet, D.; Colley, R. Parent-child association in body weight status. Health Rep. 2017, 28, 12–19. [Google Scholar]
- Notara, V.; Magriplis, E.; Prapas, C.; Antonogeorgos, G.; Rojas-Gil, A.P.; Kornilaki, E.N.; Lagiou, A.; Panagiotakos, D.B. Parental weight status and early adolescence body weight in association with socioeconomic factors. J. Educ. Health Promot. 2019, 8, 77. [Google Scholar]
- Parikka, S.; Mäki, P.; Levälahti, E.; Lehtinen-Jacks, S.; Martelin, T.; Laatikanen, T. Associations between parental BMI, socioeconomic factors, family structure and overweight in Finnish children: A path model approach. BMC Public Health 2015, 15, 271. [Google Scholar] [CrossRef] [PubMed]
- Manios, Y.; Androutsos, O.; Katsarou, C.; Vampouli, E.A.; Kulaga, Z.; Gurzkowska, B.; Iotova, V.; Usheva, N.; Cardon, G.; Koletzko, B.; et al. Prevalence and sociodemographic correlates of overweight and obesity in a large Pan-European cohort of preschool children and their families. The ToyBox study. Nutrition 2018, 55–56, 192–198. [Google Scholar] [CrossRef] [PubMed]
- Sigmund, E.; Sigmundová, D.; Badura, P. Excessive body weight of children and adolescent in the spotlight of their parents’ overweight and obesity, physical activity, and screen time. Int. J. Public Health 2020. [Google Scholar] [CrossRef] [PubMed]
- Abarca-Gómez, L.; Abdeen, Z.A.; Hamid, Z.A.; Abu-Rmeileh, M.; Acosta-Cazares, B.; Acuin, C.; Adams, R.J.; Aekplakorn, W.; Afsana, K.; Aguilar-Salinas, C.A.; et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet 2017, 390, 2627–2642. [Google Scholar] [CrossRef]
- Tran, B.X.; Dang, K.A.; Le, H.T.; Ha, G.H.; Nguyen, L.H.; Nguyen, T.H.; Tran, T.H.; Latkin, C.A.; Ho, C.S.H.; Ho, R.C.M. Global evolution of obesity research in children and youths: Setting priorities for interventions and policies. Obes. Facts 2019, 12, 137–149. [Google Scholar] [CrossRef]
- Baranowski, T.; Motil, K.J.; Moreno, J.P. Multi-etiological perspective on child obesity prevention. Curr. Nutr. Rep. 2019, 8, 1–10. [Google Scholar] [CrossRef]
- Valerio, G.; Bernasconi, S. A multi-etiological model of childhood obesity: A new biobehavioral perspective for prevention? Ital. J. Pediatrics 2019, 45, 169. [Google Scholar] [CrossRef]
- McCrabb, S.; Lane, C.; Hall, A.; Milat, A.; Bauman, A.; Sutherland, R.; Yoong, S.; Wolfenden, L. Scaling-up evidence-based obesity interventions: A systematic review assessing intervention adaptations and effectiveness and quantifying the scale-up penalty. Obes. Rev. 2019, 20, 964–982. [Google Scholar] [CrossRef]
- Beets, M.W.; Brazendale, K.; Weaver, R.G.; Armstrong, B. Rethinking behavioral approaches to compliment biological advances to understand the etiology, prevention, and treatment of childhood obesity. Child. Obes. 2019, 15, 353–358. [Google Scholar] [CrossRef]
- Beets, M.W.; Weaver, R.G.; Ioannidis, J.P.A.; Geraci, M.; Brazendale, K.; Decker, L.; Okely, A.D.; Lubans, D.; van Sluijs, E.; Jago, R.; et al. Identification and evaluation of risk of generalizability biases in pilot versus efficacy/effectiveness trials: A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 19. [Google Scholar] [CrossRef]
- Badura, P.; Geckova, A.M.; Sigmundova, D.; van Dijk, J.P.; Reijneveld, S.A. When children play, they feel better: Organized activity participation and health in adolescents. BMC Public Health 2015, 15, 1090. [Google Scholar] [CrossRef] [PubMed]
- Sigmund, E.; Sigmundová, D.; Badura, P.; Voráčová, J.; Hobza, V., Jr.; Hollein, T.; Pavelka, J.; Půžová, Z.; Kalman, M. Time-trends and correlates of obesity in Czech adolescents in relation to family socioeconomic status over a 16-year study period (2002–2018). BMC Public Health 2020, 20, 229. [Google Scholar] [CrossRef] [PubMed]
- Rojíček, M.; Boušková, M.; Elischer, D.; Ernest, J.; Holý, D.; Hrbek, J.; Hronza, M.; Kermiet, V.; Král, K.; Krumpová, E.; et al. Statistical Yearbook of the Czech Republic 2019, 1st ed.; Czech Statistical Office: Prague, Czech Republic, 2019; pp. 119–145. [Google Scholar]
- WHO. Growth Reference 5–19 Years: BMI-For-Age (5–19 Years). Available online: https://www.who.int/growthref/who2007_bmi_for_age/en/?fbclid = IwAR2LzjfL5hjAhI09I-k48x7wSRvkXWnO-Uh0rY-uEMlstb6xArh2HKAiiMA (accessed on 17 September 2020).
- de Onis, M.; Onyango, A.W.; Borghi, E.; Siyam, A.; Nishida, C.; Siekmann, J. Development of a WHO growth reference for school-aged children and adolescents. Bull. World Health Organ. 2007, 85, 660–667. [Google Scholar] [CrossRef] [PubMed]
- WHO. Obesity and Overweight. WHO Fact Sheet No°311. Available online: http://www.who.int/mediacentre/factsheets/fs311/en/ (accessed on 17 September 2020).
- Chai, L.K.; Collins, C.E.; May, C.; Holder, C.; Burrows, T.L. Accuracy of parent-reported child height and weight and calculated body mass index compared with objectively measured anthropometrics: Secondary analysis of a randomized controlled trial. J. Med. Internet Res. 2019, 21, e12532. [Google Scholar] [CrossRef]
- Huybrechts, I.; Beirlaen, C.; De Vriendt, T.; Slimani, N.; Pisa, T.P.; Schouppe, E.; De Coene, A.; De Bacquer, D.; De Henauw, S.; Himes, J.H. Validity of instruction leaflets for parents to measure their child’s weight and height at home: Results obtained from a randomised controlled trial. BMJ Open 2014, 4, e003768. [Google Scholar] [CrossRef]
- Bowring, A.L.; Peeters, A.; Freak-Poli, R.; Lim, M.S.C.; Gouillou, M.; Hellard, M. Measuring the accuracy of self-reported height and weight in a community-based sample of young people. BMC Med. Res. Methodol. 2012, 12, 175. [Google Scholar] [CrossRef]
- Sigmund, E.; Sigmundová, D. Parent-Child Physical Activity, Sedentary Behaviour, and Obesity, 1st ed.; Palacký University Olomouc: Olomouc, Czech Republic, 2017; pp. 1–85. [Google Scholar]
- Clemes, S.A.; Biddle, S.J.H. The use of pedometers for monitoring physical activity in children and adolescents: Measurement considerations. J. Phys. Act. Health 2013, 10, 249–262. [Google Scholar] [CrossRef]
- Rowe, D.A.; Mahar, M.T.; Raedeke, T.D.; Lore, J. Measuring physical activity in children with pedometers: Reliability, reactivity, and replacement of missing data. Pediatrics Exerc. Sci. 2004, 6, 343–354. [Google Scholar] [CrossRef]
- Rowlands, A.V.; Eston, R.G. The measurement and interpretation of children’s physical activity. J. Sports Sci. Med. 2007, 6, 270–276. [Google Scholar]
- Kooiman, T.J.M.; Dontje, M.; Sprenger, S.R.; Krijnen, W.P.; van der Schans, C.P.; de Groot, M. Reliability and validity of ten consumer activity trackers. BMC Sports Sci. Med. Rehabil. 2015, 7, 24. [Google Scholar] [CrossRef]
- Basett, D.R., Jr.; Toth, L.P.; LaMunion, S.R.; Crouter, S.E. Step counting: A review of measurement considerations and health-related applications. Sports Med. 2017, 47, 1303–1315. [Google Scholar] [CrossRef] [PubMed]
- Sigmundová, D.; Sigmund, E.; Badura, P.; Vokáčová, J.; Trhlíková, L.; Bucksch, J. Weekday-weekend patterns of physical activity and screen time in parents and their pre-schoolers. BMC Public Health 2016, 16, 898. [Google Scholar] [CrossRef] [PubMed]
- Craig, C.L.; Cameron, C.; Tudor-Locke, C. CANPLAY pedometer normative reference data for 21,271 children and 12,956 adolescents. Med. Sci. Sports Exerc. 2013, 45, 123–129. [Google Scholar] [CrossRef] [PubMed]
- Tudor-Locke, C.; Craig, C.; Beets, M.; Belton, S.; Cardon, G.; Duncan, S.; Hatano, Y.; Lubans, D.R.; Olds, T.S.; Raustorp, A.; et al. How many steps/day are enough? For children and adolescents. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 78. [Google Scholar] [CrossRef] [PubMed]
- Tudor-Locke, C.; Craig, C.; Brown, W.; Clemes, S.; De Cocker, K.; Giles-Corti, B.; Hatano, Y.; Inoue, S.; Matsudo, S.M.; Mutrie, N.; et al. How many steps/day are enough? For adults. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 79. [Google Scholar] [CrossRef]
- WHO. Adolescent Obesity and Related Behaviours: Trends and Inequalities in the WHO European Region, 2002–2014. Available online: https://apps.who.int/iris/handle/10665/329417 (accessed on 18 September 2020).
- Craig, C.L.; Cameron, C.; Tudor-Locke, C. Relationship between parent and child pedometer-determined physical activity: A sub-study of the CANPLAY surveillance study. Int. J. Behav. Nutr. Phys. Act. 2013, 10, 8. [Google Scholar] [CrossRef]
- Garriguet, D.; Colley, R.; Bushnik, T. Parent-child association in physical activity and sedentary behaviour. Health Rep. 2017, 28, 3–11. [Google Scholar]
- Sigmundová, D.; Sigmund, E.; Tesler, R.; Ng, K.W.; Hamrik, Z.; Mathisen, F.K.S.; Inchley, J.; Bucksch, J. Vigorous physical activity in relation to family affluence: Time trends in Europe and North America. Int. J. Public Health 2019, 64, 1049–1058. [Google Scholar] [CrossRef]
- WHO. Global Recommendation on Physical Activity for Health. Available online: https://apps.who.int/ dietphysicalactivity/leaflet-physical-activity-recommendations.pdf?ua=1 (accessed on 23 September 2020).
- Lehnert, M.; Croix, M.D.S.; Šťastný, P.; Maixnerová, E.; Zaatar, A.; Botek, M.; Vařeková, R.; Hůlka, K.; Petr, M.; Elfmark, M.; et al. The Influence of Fatigue on Injury Risk in Male Youth Soccer, 1st ed.; Palacký University Olomouc: Olomouc, Czech Republic, 2019; pp. 1–184. [Google Scholar]
- Liszewska, N.; Scholz, U.; Radtke, T.; Horodyska, K.; Liszewski, M.; Luszczynska, A. Association between children’s physical activity and parental practices enhancing children’s physical activity: The moderating effects of children’s BMI z-score. Front. Psychol. 2017, 8, 2359. [Google Scholar] [CrossRef]
- Rhee, K.E.; Jelalian, E.; Boutelle, K.; Dickstein, S.; Seifer, R.; Wing, R. Warm parenting associated with decreasing or stable child BMI during treatment. Child. Obes. 2016, 12, 94–102. [Google Scholar] [CrossRef]
- Ranucci, C.; Pippi, R.; Buratta, L.; Aiello, C.; Gianfredi, V.; Piana, N.; Reginato, E.; Tirimagni, A.; Chiodini, E.; Tomaro, E.S.; et al. Effects of an intensive lifestyle intervention to treat overweight/obese children and adolescents. BioMed Res. Int. 2017, 2017, 8573725. [Google Scholar] [CrossRef] [PubMed]
- Petersen, T.L.; Møller, L.B.; Brønd, J.C.; Jepsen, R.; Grøntved, A. Association between parent and child physical activity: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 67. [Google Scholar] [CrossRef] [PubMed]
- Stefansen, K.; Smette, I.; Strandbu, Å. Understanding the increase in parents’ involvement in organized youth sports. Sport Educ. Soc. 2018, 23, 162–172. [Google Scholar] [CrossRef]
- Bringolf-Isler, B.; Schindler, C.; Kayser, B.; Suggs, L.S.; Probst-Hensch, N. The SOPHYA Study Group. BMC Public Health 2018, 18, 1024. [Google Scholar]
- Kramoliš, T. Socio-Ekonomické Factory Ovlivňující Pohybové Chování Adolescentů. Master’s Thesis, Palacký University Olomouc, Olomouc, Czech Republic, 29 June 2020. [Google Scholar]
- Corder, K.; Ekelund, U.; Steele, R.M.; Wareham, N.J.; Brage, S. Assessment of physical activity in youth. J. Appl. Physiol. 2008, 105, 977–987. [Google Scholar] [CrossRef]
- Cuberek, R.; El Ansari, W.; Frömel, K.; Sigmund, E. A Comparison pf two motion sensors for the assessment of free-living physical activity for adolescents. Int. J. Environ. Res. Public Health 2010, 7, 1558–1576. [Google Scholar] [CrossRef]
- McNamara, E.; Hudson, Z.; Taylor, S.J.C. Measuring activity levels of young people: The validity of pedometers. Br. Med. Bull. 2010, 95, 121–137. [Google Scholar] [CrossRef]
- Guddal, M.H.; Stensland, S.Ø.; Småstuen, M.C.; Johnsen, M.B.; Zwart, J.-A.; Storheim, K. Physical activity and sport participation among adolescents: Associations with mental health in different age groups. Results from the Young-HUNT study: A cross-sectional survey. BMJ Open 2019, 9, e028555. [Google Scholar] [CrossRef]
- Torstveit, M.K.; Johansen, B.T.; Haugland, S.H.; Stea, T.H. Participation in organized sports is associated with decreased likelihood of unhealthy lifestyle habits in adolescents. Scan. J. Med. Sci. Sports 2018, 28, 2384–2396. [Google Scholar] [CrossRef]

| Family members | Age (mean ± SD) | Body Mass Index (mean ± SD) | Overweight (%) | Obesity (%) | OLTPA (mean ± SD) |
|---|---|---|---|---|---|
| Mothers (n = 915) | 39.67 ± 4.61 years | 23.91 ± 3.81 kg/m2 | 23.52 | 8.74 | 0.87 ± 1.40 days |
| Fathers (n = 578) | 42.04 ± 5.49 years | 26.89 ± 3.54 kg/m2 | 50.56 | 17.80 | 0.88 ± 1.49 days |
| Daughters (n = 566) | 10.09 ± 2.99 years | 17.51 ± 3.09 kg/m2 | 13.43 | 5.85 | 1.42 ± 1.59 days |
| Sons (n = 548) | 9.89 ± 2.81 years | 17.63 ± 3.26 kg/m2 | 17.20 | 9.79 | 1.54 ± 1.67 days |
| Lifestyle | Obesity of Offspring in Mother/Father-Child Dyad Models | |||||||
|---|---|---|---|---|---|---|---|---|
| Variables | Daughters | Sons | ||||||
| Mother-Daughter (n = 456) | Father-Daughter (n = 288) | Mother-Son (n = 459) | Father-Son (n = 290) | |||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Child: | ||||||||
| SC recommendation | ||||||||
| not achieved | Ref. | Ref. | Ref. | Ref. | ||||
| achieved | 0.65 | 0.29–1.49 | 1.12 | 0.37–3.38 | 0.23 *** | 0.09–0.56 | 0.22 * | 0.07–0.69 |
| OLTPA | ||||||||
| 0 times a week | Ref. | Ref. | Ref. | Ref. | ||||
| 1–2 times a week | 0.96 | 0.40–2.34 | 0.58 | 0.16–2.02 | 0.80 | 0.36–1.75 | 0.87 | 0.34–2.17 |
| ≥ 3 times a week | 0.82 | 0.26–2.65 | 0.71 | 0.18–2.84 | 0.68 | 0.27–1.69 | 0.09 * | 0.01–0.74 |
| Parent: | ||||||||
| Daily SC | ||||||||
| <10,000 steps/day | Ref. | Ref. | Ref. | Ref. | ||||
| ≥10,000 steps/day | 0.85 | 0.37–1.94 | 0.43 | 0.14–1.34 | 0.50 | 0.25–1.02 | 1.31 | 0.53–3.23 |
| OLTPA | ||||||||
| 0 times a week | Ref. | Ref. | Ref. | Ref. | ||||
| ≥1 time a week | 1.08 | 0.46–2.53 | 1.45 | 0.18–4.32 | 0.46 | 0.20–1.07 | 0.81 | 0.29–2.26 |
| Bodyweight status | ||||||||
| non-overweight | Ref. | Ref. | Ref. | Ref. | ||||
| overweight/obesity | 2.91 ** | 1.32–6.40 | 1.44 | 0.43–4.79 | 2.40 * | 1.21–4.77 | 1.81 | 0.63–5.22 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sigmund, E.; Sigmundová, D. The Relationship between Obesity and Physical Activity of Children in the Spotlight of Their Parents’ Excessive Body Weight. Int. J. Environ. Res. Public Health 2020, 17, 8737. https://doi.org/10.3390/ijerph17238737
Sigmund E, Sigmundová D. The Relationship between Obesity and Physical Activity of Children in the Spotlight of Their Parents’ Excessive Body Weight. International Journal of Environmental Research and Public Health. 2020; 17(23):8737. https://doi.org/10.3390/ijerph17238737
Chicago/Turabian StyleSigmund, Erik, and Dagmar Sigmundová. 2020. "The Relationship between Obesity and Physical Activity of Children in the Spotlight of Their Parents’ Excessive Body Weight" International Journal of Environmental Research and Public Health 17, no. 23: 8737. https://doi.org/10.3390/ijerph17238737
APA StyleSigmund, E., & Sigmundová, D. (2020). The Relationship between Obesity and Physical Activity of Children in the Spotlight of Their Parents’ Excessive Body Weight. International Journal of Environmental Research and Public Health, 17(23), 8737. https://doi.org/10.3390/ijerph17238737






