Does Dietary Diversity Reduce the Risk of Obesity? Empirical Evidence from Rural School Children in China
Abstract
1. Introduction
2. Materials and Methods
2.1. Data
2.1.1. Survey
2.1.2. Sampling
2.2. Variables
2.2.1. Outcomes Variables
2.2.2. Dietary Diversity and Dietary Frequency
2.2.3. Control Variables
2.3. Estimation Method
2.3.1. Association between Dietary Diversity and Nutrition Outcomes
2.3.2. The Association between the Added Food Groups and Nutrition Outcomes
3. Results
3.1. Correlation Analysis between Dietary Diversity Score and Obesity and Overweight
3.2. Heterogeneous Effects of Dietary Diversity on Obesity and Overweight
3.2.1. Heterogeneity by Dietary Diversity Tercile
3.2.2. Heterogeneity by Gender and Age
3.2.3. Heterogeneity by Family Characteristics
3.3. Correlation Analysis between Nutrition Outcomes and the Frequency of Six Main Food Groups
4. Discussion
5. Conclusions
Ethical Approval
Author Contributions
Funding
Conflicts of Interest
References
- Daniels, S.R. The consequences of childhood overweight and obesity. Future Child. 2006, 16, 47–67. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.S.; Mulder, C.; Twisk, J.W.; Van Mechelen, W.; Chinapaw, M.J. Tracking of childhood overweight into adulthood: A systematic review of the literature. Obes. Rev. 2008, 9, 474–488. [Google Scholar] [CrossRef]
- Liu, X.; Zhu, C. Will knowing diabetes affect labor income? Evidence from a natural experiment. Econ. Lett. 2014, 124, 74–78. [Google Scholar] [CrossRef]
- Su, W.; Huang, J.; Chen, F.; Iacobucci, W.; Mocarski, M.; Dall, T.; Perreault, L. Modeling the clinical and economic implications of obesity using microsimulation. J. Med. Econ. 2015, 18, 886–897. [Google Scholar] [CrossRef] [PubMed]
- IFPRI. Global Nutrition Report 2016: From Promise to Impact: Ending Malnutrition by 2030; International Food Policy Research Institute: Washington, DC, USA, 2016. [Google Scholar] [CrossRef]
- WHO. World Health Organization Obesity and Overweight Fact Sheet; WHO: Geneva, Switzerland, 2016. [Google Scholar]
- Hales, C.M.; Carroll, M.D.; Fryar, C.D.; Ogden, C.L. Prevalence of Obesity among Adults and Youth: United States, 2015–2016; National Center for Health Statistics: Hyattsville, MD, USA, 2017.
- WHO. World Health Statistics Overview 2019: Monitoring Health for the SDGs, Sustainable Development Goals; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- WHO. Consideration of the Evidence on Childhood Obesity for the Commission on Ending Childhood Obesity: Report of the Ad hoc Working Group on Science and Evidence for Ending Childhood Obesity; WHO: Geneva, Switzerland, 2016. [Google Scholar]
- Wang, Y.; Monteiro, C.; Popkin, B.M. Trends of obesity and underweight in older children and adolescents in the United States, Brazil, China, and Russia. Am. J. Clin. Nutr. 2002, 75, 971–977. [Google Scholar] [CrossRef] [PubMed]
- Zhang, N.; Ma, G. Childhood obesity in China: Trends, risk factors, policies and actions. Glob. Health J. 2018, 2, 1–13. [Google Scholar] [CrossRef]
- Department of Population and Employment Statistics of the National Bureau of Statistics of China. China Population and Employment Statistics Yearbook-2019; China Statistics Press: Beijing, China, 2019.
- Zhang, Q.; Hu, X. Monitoring Report on Nutrition and Health Status of Chinese Residents No. 11: 2010–2013 Nutrition and Health Status of Chinese School Children Aged 6–17; People’s Medical Publishing House: Beijing, China, 2018. [Google Scholar]
- He, Q.; Ding, Z.; Fong, D.; Karlberg, J. Risk factors of obesity in preschool children in China: A population-based case–control study. Int. J. Obes. 2000, 24, 1528–1536. [Google Scholar] [CrossRef] [PubMed]
- Shang, X.W.; Liu, A.L.; Zhang, Q.; Hu, X.Q.; Du, S.M.; Jun, M.; Xu, G.F.; Ying, L.; Guo, H.W.; Lin, D. Report on childhood obesity in China (9): Sugar-sweetened beverages consumption and obesity. Biomed. Environ. Sci. 2012, 25, 125–132. [Google Scholar]
- Li, B.; Adab, P.; Cheng, K.K. The role of grandparents in childhood obesity in China-evidence from a mixed methods study. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 91. [Google Scholar] [CrossRef]
- Schmitz, K.H.; Lytle, L.A.; Phillips, G.A.; Murray, D.M.; Birnbaum, A.S.; Kubik, M.Y. Psychosocial correlates of physical activity and sedentary leisure habits in young adolescents: The Teens Eating for Energy and Nutrition at School study. Prev. Med. 2002, 34, 266–278. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Xue, H.; Wen, M.; Wang, W.; Wang, Y. Nutrition and physical activity related school environment/policy factors and child obesity in China: A nationally representative study of 8573 students in 110 middle schools. Pediatric Obes. 2017, 12, 485–493. [Google Scholar] [CrossRef]
- Zhang, J.; Wang, H.; Wang, Y.; Xue, H.; Wang, Z.; Du, W.; Su, C.; Zhang, J.; Jiang, H.; Zhai, F. Dietary patterns and their associations with childhood obesity in China. Br. J. Nutr. 2015, 113, 1978–1984. [Google Scholar] [CrossRef]
- Liu, W.; Liu, W.; Lin, R.; Li, B.; Pallan, M.; Cheng, K.; Adab, P. Socioeconomic determinants of childhood obesity among primary school children in Guangzhou, China. BMC Public Health 2016, 16, 482. [Google Scholar] [CrossRef]
- Tamayo, T.; Herder, C.; Rathmann, W. Impact of early psychosocial factors (childhood socioeconomic factors and adversities) on future risk of type 2 diabetes, metabolic disturbances and obesity: A systematic review. BMC Public Health 2010, 10, 525. [Google Scholar] [CrossRef]
- Kennedy, G.; Ballard, T.; Dop, M.C. Guidelines for Measuring Household and Individual Dietary Diversity; Food and Agriculture Organization of the United Nations: Rome, Italy, 2011. [Google Scholar]
- Salehi-Abargouei, A.; Akbari, F.; Bellissimo, N.; Azadbakht, L. Dietary diversity score and obesity: A systematic review and meta-analysis of observational studies. Eur. J. Clin. Nutr. 2016, 70, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Azadbakht, L.; Esmaillzadeh, A. Dietary energy density is favorably associated with dietary diversity score among female university students in Isfahan. Nutrition 2012, 28, 991–995. [Google Scholar] [CrossRef]
- Jayawardena, R.; Byrne, N.M.; Soares, M.J.; Katulanda, P.; Yadav, B.; Hills, A.P. High dietary diversity is associated with obesity in Sri Lankan adults: An evaluation of three dietary scores. BMC Public Health 2013, 13, 314. [Google Scholar] [CrossRef]
- Tian, X.; Wu, M.; Zang, J.; Zhu, Y.; Wang, H. Dietary diversity and adiposity in Chinese men and women: An analysis of four waves of cross-sectional survey data. Eur. J. Clin. Nutr. 2017, 71, 506–511. [Google Scholar] [CrossRef]
- Fernandez, C.; Kasper, N.M.; Miller, A.L.; Lumeng, J.C.; Peterson, K.E. Association of dietary variety and diversity with body mass index in US preschool children. Pediatrics 2016, 137, e20152307. [Google Scholar] [CrossRef]
- Rolls, B.J.; Ello-Martin, J.A.; Tohill, B.C. What can intervention studies tell us about the relationship between fruit and vegetable consumption and weight management? Nutr. Rev. 2004, 62, 1–17. [Google Scholar] [CrossRef]
- Spiegel, S.A.; Foulk, D. Reducing overweight through a multidisciplinary school-based intervention. Obesity 2006, 14, 88–96. [Google Scholar] [CrossRef]
- Xu, H.; Ecker, O.; Zhang, Q.; Du, S.; Liu, A.; Li, Y.; Hu, X.; Li, T.; Guo, H.; Li, Y. The effect of comprehensive intervention for childhood obesity on dietary diversity among younger children: Evidence from a school-based randomized controlled trial in China. PLoS ONE 2020, 15, e0235951. [Google Scholar] [CrossRef]
- Foster, G.D.; Sherman, S.; Borradaile, K.E.; Grundy, K.M.; Vander Veur, S.S.; Nachmani, J.; Karpyn, A.; Kumanyika, S.; Shults, J. A policy-based school intervention to prevent overweight and obesity. Pediatrics 2008, 121, e794–e802. [Google Scholar] [CrossRef] [PubMed]
- Zhao, W.; Yu, K.; Tan, S.; Zheng, Y.; Zhao, A.; Wang, P.; Zhang, Y. Dietary diversity scores: An indicator of micronutrient inadequacy instead of obesity for Chinese children. BMC Public Health 2017, 17, 440. [Google Scholar] [CrossRef]
- Arimond, M.; Ruel, M.T. Dietary diversity is associated with child nutritional status: Evidence from 11 demographic and health surveys. J. Nutr. 2004, 134, 2579–2585. [Google Scholar] [CrossRef]
- Hooshmand, S.; Udipi, S.A. Dietary diversity and nutritional status of urban primary school children from Iran and India. J. Nutr. Disord. Ther. 2013, 12. [Google Scholar] [CrossRef]
- Karimbeiki, R.; Pourmasoumi, M.; Feizi, A.; Abbasi, B.; Hadi, A.; Rafie, N.; Safavi, S. Higher dietary diversity score is associated with obesity: A case–control study. Public Health 2018, 157, 127–134. [Google Scholar] [CrossRef]
- Bi, J.; Liu, C.; Li, S.; He, Z.; Chen, K.; Luo, R.; Wang, Z.; Yu, Y.; Xu, H. Dietary diversity among preschoolers: A cross-sectional study in poor, rural, and ethnic minority areas of central south china. Nutrients 2019, 11, 558. [Google Scholar] [CrossRef]
- Yang, Y.X.; Wang, X.L.; Leong, P.M.; Zhang, H.M.; Yang, X.G.; Kong, L.Z.; Zhai, F.Y.; Cheng, Y.Y.; Guo, J.S.; Su, Y.X. New Chinese dietary guidelines: Healthy eating patterns and food-based dietary recommendations. Asia Pac. J. Clin. Nutr. 2018, 27, 908. [Google Scholar] [PubMed]
- Wang, A.; Scherpbier, R.W.; Huang, X.; Guo, S.; Yang, Y.; Josephs-Spaulding, J.; Ma, C.; Zhou, H.; Wang, Y. The dietary diversity and stunting prevalence in minority children under 3 years old: A cross-sectional study in forty-two counties of Western China. Br. J. Nutr. 2017, 118, 840–848. [Google Scholar] [CrossRef]
- Chen, Q.; Pei, C.; Zhao, Q. Eating More but Not Better at School? Impacts of Boarding on Students’ Dietary Structure and Nutritional Status in Rural Northwestern China. Sustainability 2018, 10, 2753. [Google Scholar] [CrossRef]
- Chen, Q.; Pei, C.; Bai, Y.; Zhao, Q. Impacts of Nutrition Subsidies on Diet Diversity and Nutritional Outcomes of Primary School Students in Rural Northwestern China-Do Policy Targets and Incentives Matter? Int. J. Environ. Res. Public Health 2019, 16, 2891. [Google Scholar] [CrossRef]
- Liu, X.; Zhao, Q.; Chen, Q. Better nutrition, healthier mind? Experimental evidence from primary schools in rural northwestern China. J. Integr. Agric. 2019, 18, 1768–1779. [Google Scholar] [CrossRef]
- Liu, J.; Yang, Q.; Liu, J.; Zhang, Y.; Jiang, X.; Yang, Y. Study on the Spatial Differentiation of the Populations on Both Sides of the “Qinling-Huaihe Line” in China. Sustainability 2020, 12, 4545. [Google Scholar] [CrossRef]
- Rozelle, S. Stagnation without equity: Patterns of growth and inequality in China’s rural economy. China J. 1996, 35, 63–92. [Google Scholar] [CrossRef]
- WHO. Physical Status: The Use of and Interpretation of Anthropometry, Report of a WHO Expert Committee; World Health Organization: Geneva, Switzerland, 1995. [Google Scholar]
- Must, A.; Anderson, S. Body mass index in children and adolescents: Considerations for population-based applications. Int. J. Obes. 2006, 30, 590–594. [Google Scholar] [CrossRef] [PubMed]
- Onis, M.d.; Onyango, A.W.; Borghi, E.; Siyam, A.; Nishida, C.; Siekmann, J. Development of a WHO growth reference for school-aged children and adolescents. Bull. World Health Organ. 2007, 85, 660–667. [Google Scholar] [CrossRef]
- Lazzeri, G.; Pammolli, A.; Pilato, V.; Giacchi, M.V. Relationship between 8/9-yr-old school children BMI, parents’ BMI and educational level: A cross sectional survey. Nutr. J. 2011, 10, 76. [Google Scholar] [CrossRef]
- Zhou, S.; Ye, B.; Fu, P.; Li, S.; Yuan, P.; Yang, L.; Zhan, X.; Chao, F.; Zhang, S.; Wang, M.Q. Double Burden of Malnutrition: Examining the Growth Profile and Coexistence of Undernutrition, Overweight, and Obesity among School-Aged Children and Adolescents in Urban and Rural Counties in Henan Province, China. J. Obes. 2020, 2020. [Google Scholar] [CrossRef]
- Song, Y.; Agardh, A.; Ma, J.; Li, L.; Lei, Y.; Stafford, R.S.; Prochaska, J.J. National trends in stunting, thinness and overweight among Chinese school-aged children, 1985–2014. Int. J. Obes. 2019, 43, 402–411. [Google Scholar] [CrossRef]
- Amirhamidi, Z.; Omidvar, N.; Eini-Zinab, H.; Doustmohammadian, A.; Esfandiari, S.; Azadi, R.; Haidari, H. Association of Weight Status with Dietary Intake and Dietary Diversity Score in 10–12-Year-Old Children in Tehran: A Cross-Sectional Study. Iran. J. Pediatrics 2019, 29, e85317. [Google Scholar] [CrossRef]
- Li, Y.; Wedick, N.M.; Lai, J.; He, Y.; Hu, X.; Liu, A.; Du, S.; Zhang, J.; Yang, X.; Chen, C. Lack of dietary diversity and dyslipidaemia among stunted overweight children: The 2002 China National Nutrition and Health Survey. Public Health Nutr. 2011, 14, 896–903. [Google Scholar] [CrossRef]
- Kennedy, E.; Powell, R. Changing eating patterns of American children: A view from 1996. J. Am. Coll. Nutr. 1997, 16, 524–529. [Google Scholar] [PubMed]
- McCrory, M.A.; Fuss, P.J.; McCallum, J.E.; Yao, M.; Vinken, A.G.; Hays, N.P.; Roberts, S.B. Dietary variety within food groups: Association with energy intake and body fatness in men and women. Am. J. Clin. Nutr. 1999, 69, 440–447. [Google Scholar] [CrossRef]
- Natale, R.A.; Lopez-Mitnik, G.; Uhlhorn, S.B.; Asfour, L.; Messiah, S.E. Effect of a child care center-based obesity prevention program on body mass index and nutrition practices among preschool-aged children. Health Promot. Pract. 2014, 15, 695–705. [Google Scholar] [CrossRef]
- Li, Y.; Wang, D.D.; Ley, S.H.; Vasanti, M.; Howard, A.G.; He, Y.; Hu, F.B. Time trends of dietary and lifestyle factors and their potential impact on diabetes burden in China. Diabetes Care 2017, 40, 1685–1694. [Google Scholar] [CrossRef]
- Liu, S.; Willett, W.C.; Manson, J.E.; Hu, F.B.; Rosner, B.; Colditz, G. Relation between changes in intakes of dietary fiber and grain products and changes in weight and development of obesity among middle-aged women. Am. J. Clin. Nutr. 2003, 78, 920–927. [Google Scholar] [CrossRef]
- Motamed Rezaei, O.; Moodi, M.; Tiyuri, A.; ZarShenas, F.; Sharifi, M. Prevalence of obesity and its relationship with food habits among 10–14 years old school boys in Birjand, 2014: A short report. J. Rafsanjan Univ. Med. Sci. 2016, 14, 1085–1094. [Google Scholar]
- Pei, Z.; Flexeder, C.; Fuertes, E.; Standl, M.; Buyken, A.; Berdel, D.; Von Berg, A.; Lehmann, I.; Schaaf, B.; Heinrich, J. Food intake and overweight in school-aged children in Germany: Results of the GINIplus and LISAplus studies. Ann. Nutr. Metab. 2014, 64, 60–70. [Google Scholar] [CrossRef]
- Maffeis, C.; Talamini, G.; Tato, L. Influence of diet, physical activity and parents’ obesity on children’s adiposity: A four-year longitudinal study. Int. J. Obes. 1998, 22, 758–764. [Google Scholar] [CrossRef]
- Zhang, N.; Bécares, L.; Chandola, T.; Callery, P. Intergenerational differences in beliefs about healthy eating among carers of left-behind children in rural China: A qualitative study. Appetite 2015, 95, 484–491. [Google Scholar] [CrossRef]
- Das, J.K.; Salam, R.A.; Thornburg, K.L.; Prentice, A.M.; Campisi, S.; Lassi, Z.S.; Koletzko, B.; Bhutta, Z.A. Nutrition in adolescents: Physiology, metabolism, and nutritional needs. Ann. N. Y. Acad. Sci. 2017, 1393, 21–33. [Google Scholar] [CrossRef]
| Variable | Definition | Obs | Mean | Standard Deviation |
|---|---|---|---|---|
| Outcome variables | ||||
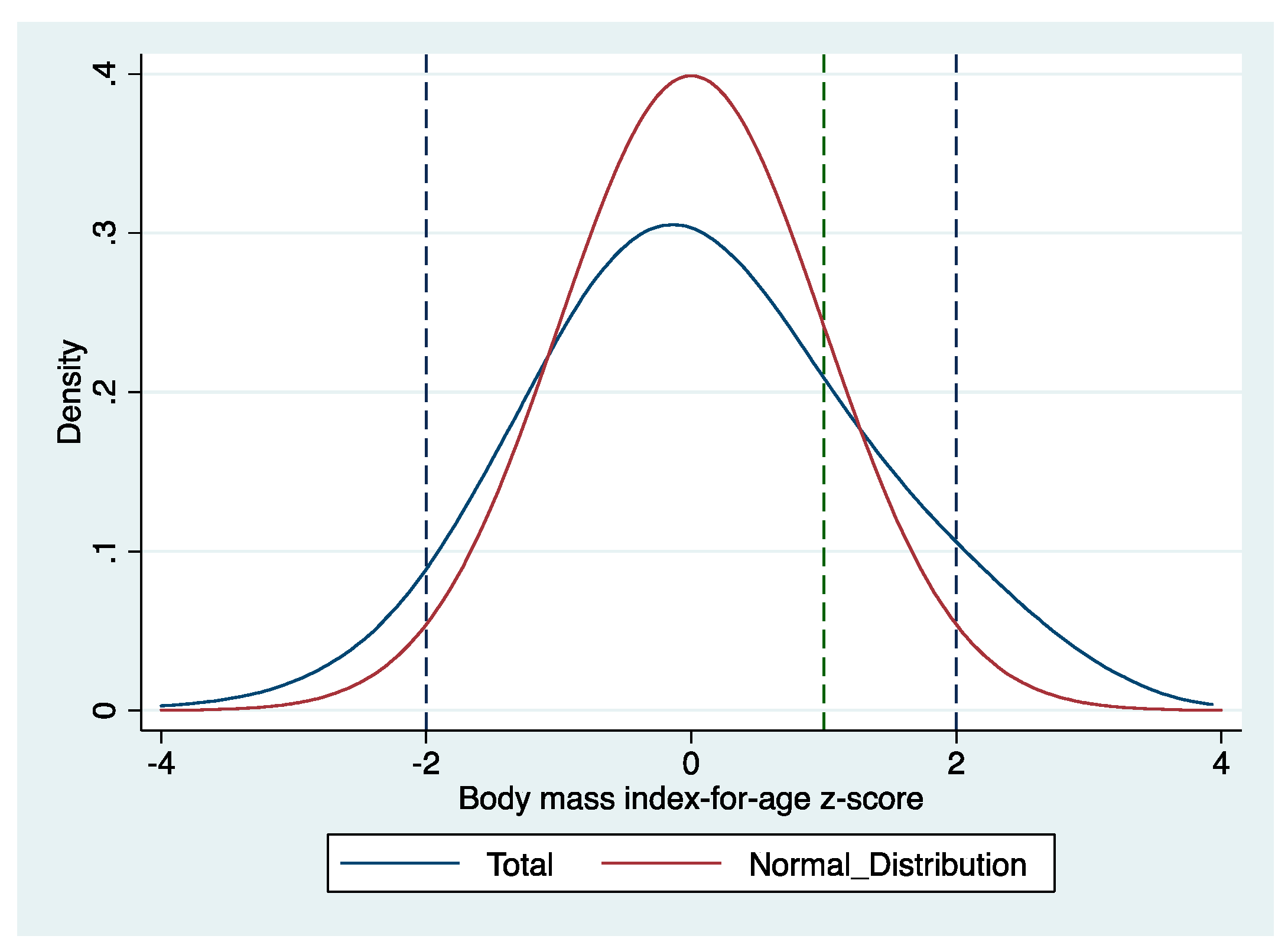
| BMI-for-age z-score (Baz) | Body mass index-for-age z-score | 8388 | 0.06 | 1.24 |
| Overweight | Dummy: =1 if yes (baz > +1 sd); =0 if normal (baz ≥ −2 sd, and baz ≤ +1 sd) | 8041 | 0.23 | 0.42 |
| Obesity | Dummy: =1 if yes (baz > +2 sd); =0 if normal (baz ≥ −2 sd, and baz ≤ +1 sd) | 6797 | 0.09 | 0.28 |
| Thinness | Dummy: =1 if yes (baz < −2 sd); =0 if normal (baz ≥ −2 sd, and baz ≤ +1 sd) | 6548 | 0.05 | 0.22 |
| 1. Food Groups Used to Construct DDS | 2. Food Categories Involved in FAO Guidelines (FAO, 2008) |
|---|---|
| Grains | Grains |
| Tubers | Vitamin A-rich vegetables and tubers; white roots and tubers |
| Vegetables | Dark green leafy vegetables; other vegetables |
| Fruits | Vitamin A-rich fruits; other fruits |
| Meat | Flesh meat, organ meat |
| Eggs | Eggs |
| Fish | Fish and seafood |
| Bean products, nuts, and seeds | Legumes, nuts, and seeds |
| Milk and milk products | Milk and milk products |
| (no corresponding category) | Oil and fat |
| Variable | Definition | Obs | Mean | Standard Deviation |
|---|---|---|---|---|
| Dietary diversity and dietary frequency within 24 h | ||||
| Dietary Diversity Scores | The potential score range is 0–9. | 8388 | 5.56 | 1.91 |
| F_Grains | The potential dietary frequency range is 0–4 | 8388 | 1.34 | 0.54 |
| F_Tubers | The potential dietary frequency range is 0–4 | 8388 | 0.99 | 0.65 |
| F_Vegetables | The potential dietary frequency range is 0–4 | 8388 | 1.23 | 0.44 |
| F_Fruits | The potential dietary frequency range is 0–4 | 8388 | 1.03 | 0.77 |
| F_Bean products, nuts, and seeds | The potential dietary frequency range is 0–4 | 8388 | 0.96 | 0.55 |
| F_Meat | The potential dietary frequency range is 0–4 | 8388 | 1.16 | 0.59 |
| F_Fish | The potential dietary frequency range is 0–4 | 8388 | 0.71 | 0.73 |
| F_Milk and milk products | The potential dietary frequency range is 0–4 | 8388 | 0.98 | 0.75 |
| F_Eggs | The potential dietary frequency range is 0–4 | 8388 | 0.95 | 0.72 |
| Variables 1 | 1. | 2. | 3. |
|---|---|---|---|
| Body Mass Index-for-Age z-Score | Overweight (=1 if Yes) | Obesity (=1 if Yes) | |
| DDS | −0.010 | −0.005 ** | −0.002 |
| (0.007) | (0.003) | (0.002) | |
| Boy (=1 if yes) | 0.296 *** | 0.106 *** | 0.082 *** |
| (0.025) | (0.009) | (0.007) | |
| Agemonth (month) | −0.010 *** | −0.002 *** | −0.002 *** |
| (0.001) | (0.000) | (0.000) | |
| Preschool (=1 if yes) | 0.007 | 0.022 | 0.004 |
| (0.043) | (0.017) | (0.013) | |
| Sibling number | −0.097 *** | −0.030 *** | −0.026 *** |
| (0.019) | (0.007) | (0.005) | |
| Age_father (year) | −0.002 | 0.000 | 0.001 |
| (0.004) | (0.002) | (0.001) | |
| Age_mother (year) | −0.008 * | −0.003 * | −0.001 |
| (0.004) | (0.002) | (0.001) | |
| Edu_father (year) | 0.010 ** | 0.004 ** | 0.002 * |
| (0.005) | (0.002) | (0.001) | |
| Edu_mother (year) | −0.007 * | −0.003 * | −0.001 |
| (0.004) | (0.002) | (0.001) | |
| BMI_father | 0.029 *** | 0.009 *** | 0.005 *** |
| (0.004) | (0.001) | (0.001) | |
| BMI_mother | 0.042 *** | 0.011 *** | 0.007 *** |
| (0.004) | (0.001) | (0.001) | |
| Asset | 0.033 *** | 0.011 ** | 0.005 |
| (0.013) | (0.005) | (0.004) | |
| County effects | Yes | Yes | Yes |
| Constant | 0.294 | - | - |
| (0.382) | - | - | |
| Observations | 7975 | 7975 | 6743 |
| R-squared/Chi2 | 0.090 | 382.79 | 319.56 |
| Variables 1 | 1. | 2. | 3. |
|---|---|---|---|
| Body Mass Index-for-Age z-Score | Overweight (=1 if Yes) | Obesity (=1 if Yes) | |
| Panel A: Subgroups | Dietary diversity ≤ 3 food groups | ||
| DDS | 0.026 | 0.013 | −0.006 |
| (0.043) | (0.015) | (0.011) | |
| Controls | Yes | Yes | Yes |
| Observations | 1201 | 1201 | 1023 |
| R-squared/Chi2 | 0.120 | 88.05 | 89.7 |
| Panel B: Subgroups | Dietary diversity ≥ 4 food groups | ||
| DDS | −0.025 *** | −0.012 *** | −0.001 |
| (0.009) | (0.003) | (0.003) | |
| Controls | Yes | Yes | Yes |
| Observations | 6774 | 6774 | 5720 |
| R-squared/Chi2 | 0.090 | 335.36 | 261.89 |
| Panel C: Subgroups | Dietary diversity ≥ 7 food groups | ||
| DDS | −0.066 ** | −0.021 ** | −0.013 * |
| (0.028) | (0.010) | (0.008) | |
| Controls | Yes | Yes | Yes |
| Observations | 2630 | 2630 | 2261 |
| R-squared/Chi2 | 0.112 | 162.47 | 130.04 |
| Variables 1 | 1. | 2. | 3. | 4. | 5. | 6. |
|---|---|---|---|---|---|---|
| Body Mass Index-for-Age z-Score | Over-Weight (=1 if Yes) | Obesity (=1 if Yes) | Body Mass Index-for-Age z-Score | Over-Weight (=1 if Yes) | Obesity (=1 if Yes) | |
| Panel A: Gender | Boys | Girls | ||||
| DDS | −0.007 | −0.005 | −0.004 | −0.013 | −0.006 * | 0.001 |
| (0.010) | (0.004) | (0.003) | (0.009) | (0.003) | (0.002) | |
| Controls | Yes | Yes | Yes | Yes | Yes | Yes |
| Observations | 4098 | 4098 | 3385 | 3877 | 3877 | 3358 |
| R-squared/Chi2 | 0.084 | 170.8 | 149.16 | 0.077 | 136.22 | 84.31 |
| Panel B: Age | Less than 144 months | At least 144 months | ||||
| DDS | −0.015 | −0.007 * | −0.004 | −0.002 | −0.002 | 0.002 |
| (0.009) | (0.004) | (0.003) | (0.011) | (0.004) | (0.002) | |
| Controls | Yes | Yes | Yes | Yes | Yes | Yes |
| Observations | 4848 | 4848 | 4072 | 3127 | 3127 | 2671 |
| R-squared/Chi2 | 0.101 | 273.34 | 210.78 | 0.066 | 119.67 | 122.9 |
| Variables 1 | 1. | 2. | 3. | 4. | 5. | 6. |
|---|---|---|---|---|---|---|
| Body Mass Index-for-Age z-Score | Over-Weight (=1 if Yes) | Obesity (=1 if Yes) | Body Mass Index-for-Age z-Score | Over-Weight (=1 if Yes) | Obesity (=1 if Yes) | |
| Panel A: Sibling number | At least 1 sibling | Only child | ||||
| DDS | −0.010 | −0.005 * | −0.002 | −0.010 | −0.010 | −0.001 |
| (0.007) | (0.003) | (0.002) | (0.023) | (0.008) | (0.006) | |
| Controls | Yes | Yes | Yes | Yes | Yes | Yes |
| Observations | 7153 | 7153 | 6052 | 822 | 822 | 691 |
| R-squared/Chi2 | 0.092 | 335.96 | 297.26 | 0.088 | 57.99 | 34.68 |
| Panel B: Parents’ BMI | BMI_father ≥ 25 or BMI_mother ≥ 25 | BMI_father ≥ 30 or BMI_mother ≥ 30 | ||||
| DDS | −0.021 * | −0.011 ** | −0.007 * | 0.008 | −0.002 | −0.006 |
| (0.012) | (0.005) | (0.004) | (0.028) | (0.012) | (0.011) | |
| Observations | 2864 | 2864 | 2312 | 457 | 457 | 370 |
| Controls | Yes | Yes | Yes | Yes | Yes | Yes |
| R-squared/Chi2 | 0.084 | 142.79 | 138.73 | 0.135 | 55.99 | 55.38 |
| Panel C: Household assets | Low- and medium (<0.5) | High (>0.5) | ||||
| DDS | −0.016 * | −0.008 *** | −0.003 | 0.001 | −0.000 | 0.002 |
| (0.009) | (0.003) | (0.002) | (0.011) | (0.004) | (0.003) | |
| Controls | Yes | Yes | Yes | Yes | Yes | Yes |
| Observations | 4773 | 4773 | 4070 | 3202 | 3202 | 2673 |
| R-squared/Chi2 | 0.094 | 226.94 | 216.41 | 0.086 | 175.05 | 125.74 |
| Estimation | Variables 1 | 1. | 2. | 3. |
|---|---|---|---|---|
| Body Mass Index-for-Age z-Score | Overweight (=1 if Yes) | Obesity (=1 if Yes) | ||
| 1. | F_Tubers | −0.045 ** | −0.018 *** | −0.014 *** |
| (0.019) | (0.007) | (0.005) | ||
| 2. | F_Bean products, nuts and seeds | −0.051 ** | −0.023 *** | −0.007 |
| (0.022) | (0.009) | (0.006) | ||
| 3. | F_Fish | −0.038 ** | −0.012 * | −0.002 |
| (0.018) | (0.007) | (0.005) | ||
| 4. | F_Fruits | −0.030 ** | −0.012 * | −0.005 |
| (0.016) | (0.006) | (0.004) | ||
| 5. | F_Eggs | −0.026 | −0.007 | −0.001 |
| (0.017) | (0.007) | (0.005) | ||
| 6. | F_Milk and milk products | −0.048 *** | −0.020 *** | −0.007 |
| (0.016) | (0.006) | (0.005) | ||
| Observations | 7975 | 7975 | 6743 | |
| R-squared/Chi2 | 0.090 | 380.86 | 319.66 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tao, C.; Zhao, Q.; Glauben, T.; Ren, Y. Does Dietary Diversity Reduce the Risk of Obesity? Empirical Evidence from Rural School Children in China. Int. J. Environ. Res. Public Health 2020, 17, 8122. https://doi.org/10.3390/ijerph17218122
Tao C, Zhao Q, Glauben T, Ren Y. Does Dietary Diversity Reduce the Risk of Obesity? Empirical Evidence from Rural School Children in China. International Journal of Environmental Research and Public Health. 2020; 17(21):8122. https://doi.org/10.3390/ijerph17218122
Chicago/Turabian StyleTao, Chang, Qiran Zhao, Thomas Glauben, and Yanjun Ren. 2020. "Does Dietary Diversity Reduce the Risk of Obesity? Empirical Evidence from Rural School Children in China" International Journal of Environmental Research and Public Health 17, no. 21: 8122. https://doi.org/10.3390/ijerph17218122
APA StyleTao, C., Zhao, Q., Glauben, T., & Ren, Y. (2020). Does Dietary Diversity Reduce the Risk of Obesity? Empirical Evidence from Rural School Children in China. International Journal of Environmental Research and Public Health, 17(21), 8122. https://doi.org/10.3390/ijerph17218122







