Aesthetic Treatment Outcomes of Capillary Hemangioma, Venous Lake, and Venous Malformation of the Lip Using Different Surgical Procedures and Laser Wavelengths (Nd:YAG, Er,Cr:YSGG, CO2, and Diode 980 nm)
Abstract
1. Introduction
2. Material and Methods
2.1. Study Design
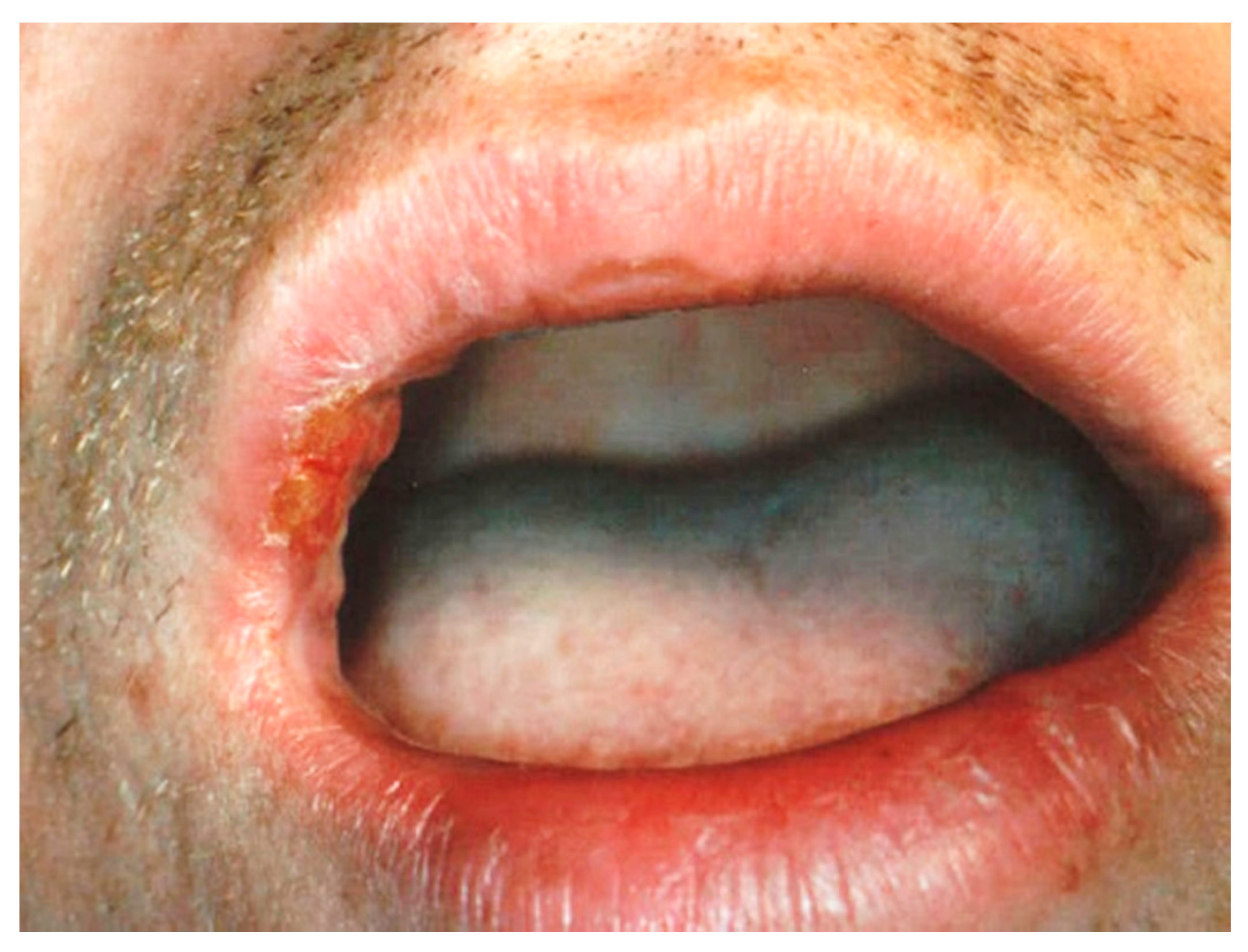
2.2. Participants
Inclusion and Exclusion Criteria
2.3. Surgical Techniques
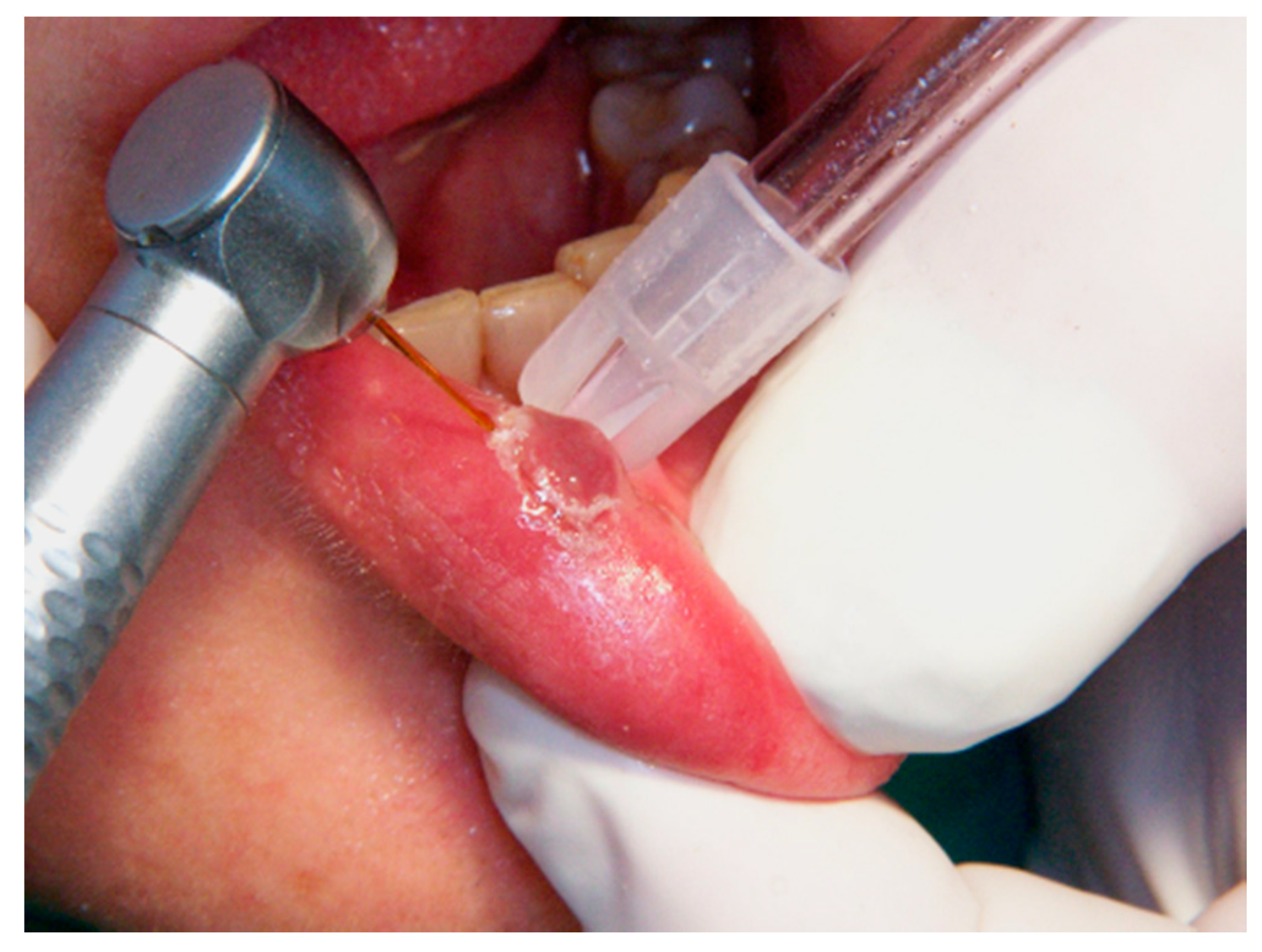
2.3.1. Er,Cr:YSGG Laser
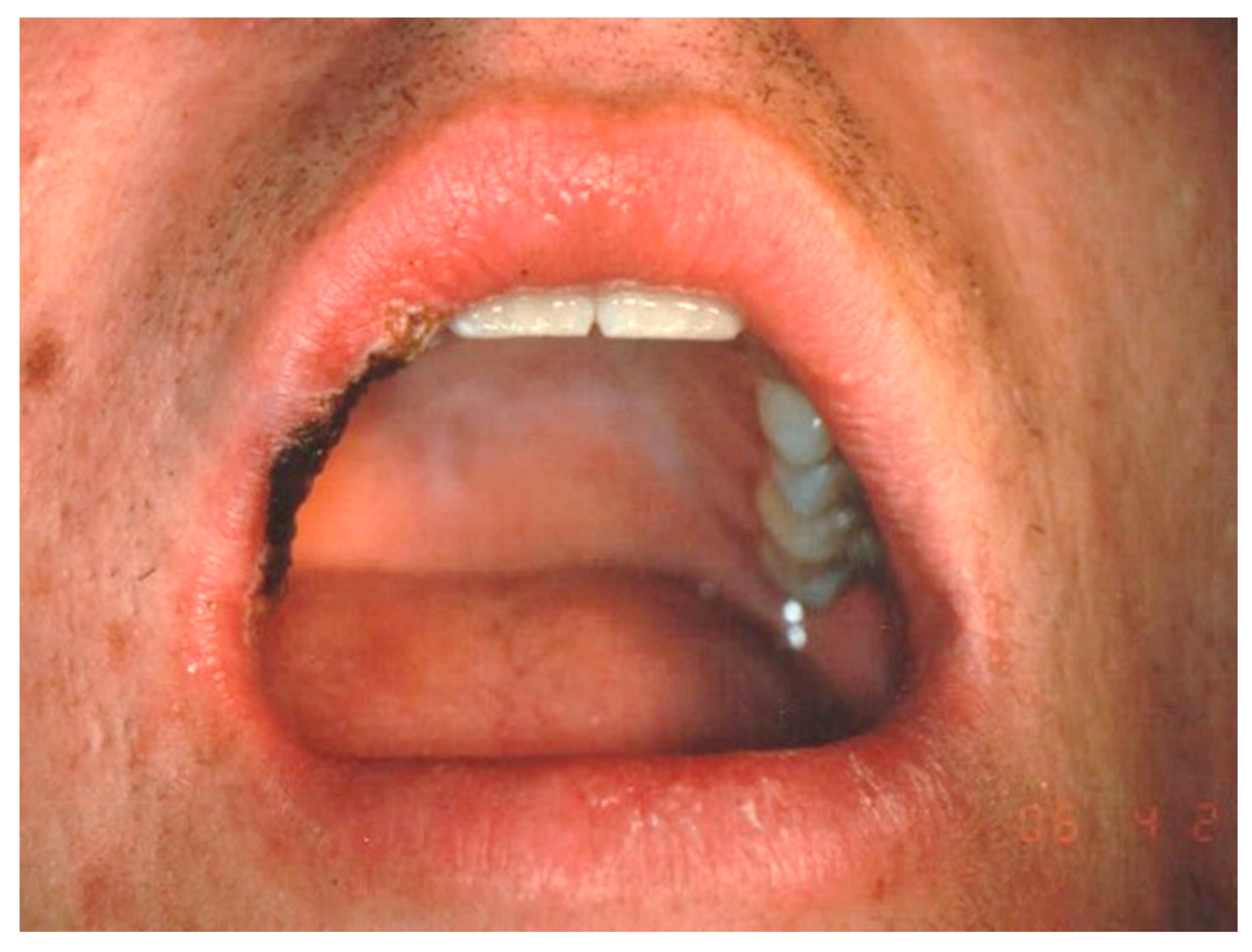
2.3.2. CO2 Laser
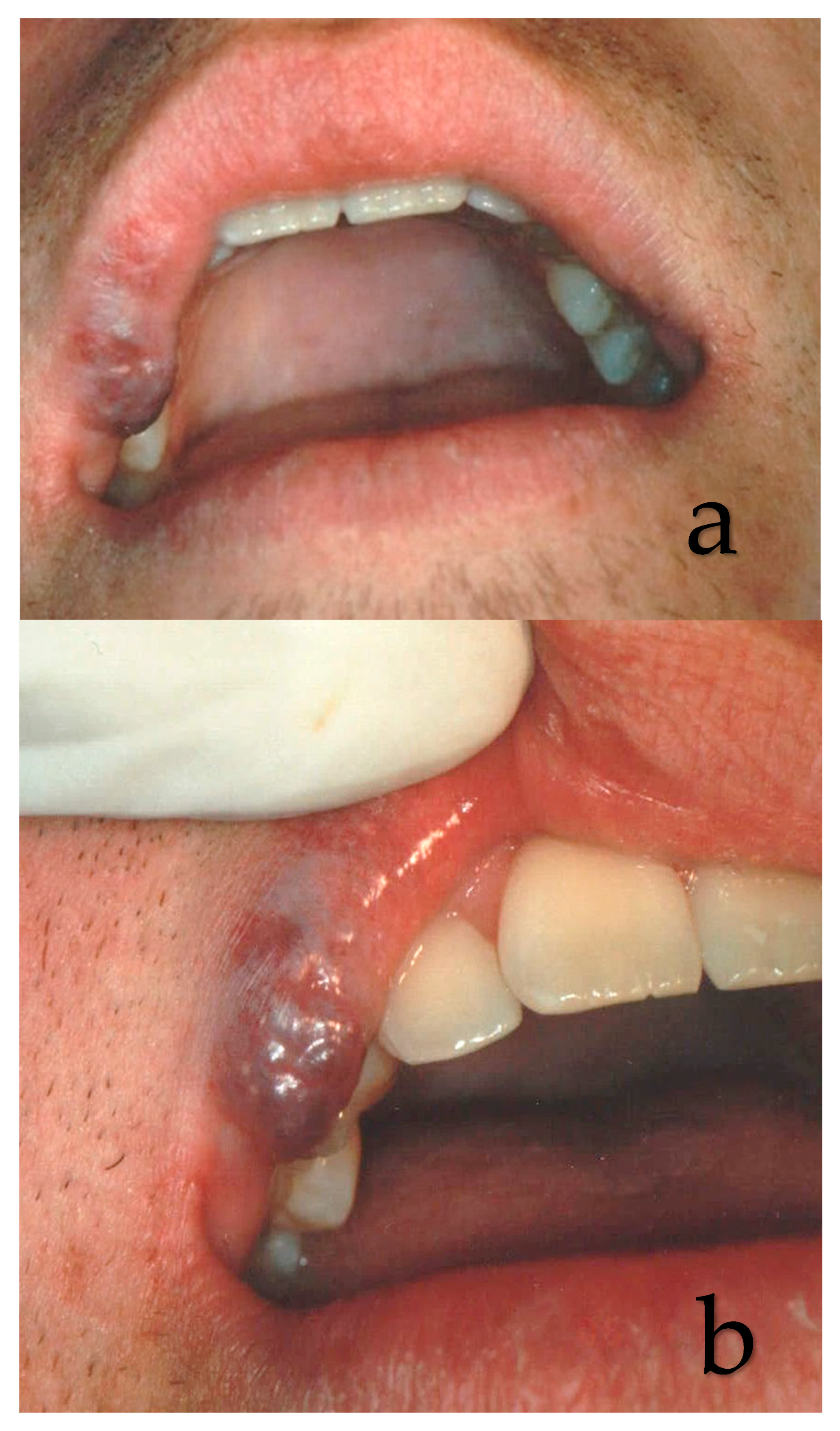
2.3.3. Nd:YAG Laser Irradiation
2.3.4. Diode Laser
2.3.5. Postoperative Instructions and Recommendations
2.4. Evaluation of the Aesthetic Results
2.5. Evaluation of the Recurrence Rate
2.6. Statistical Analysis
3. Results
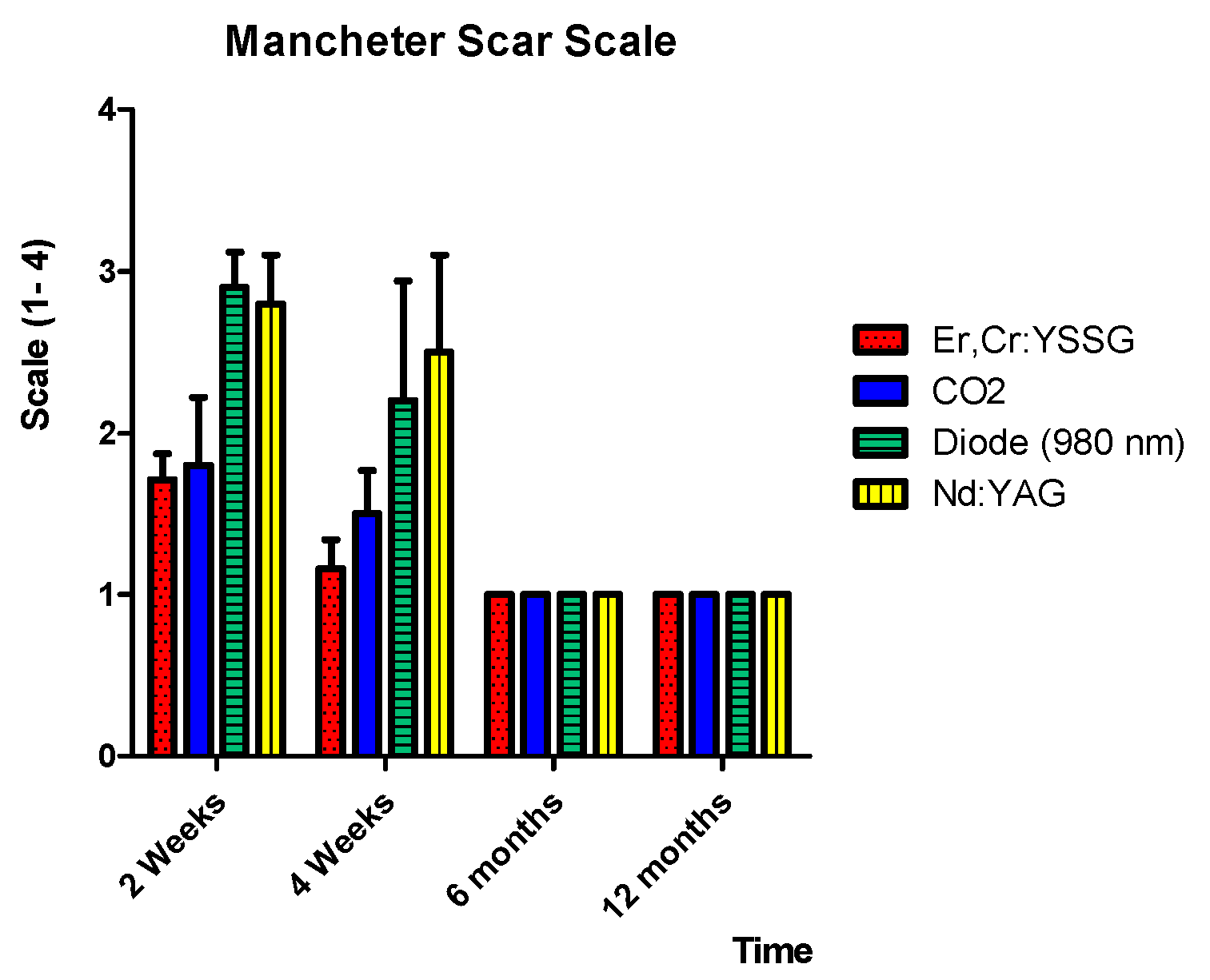
3.1. Results of the Manchester Scar Scale Evaluation
3.2. Recurrence Rate
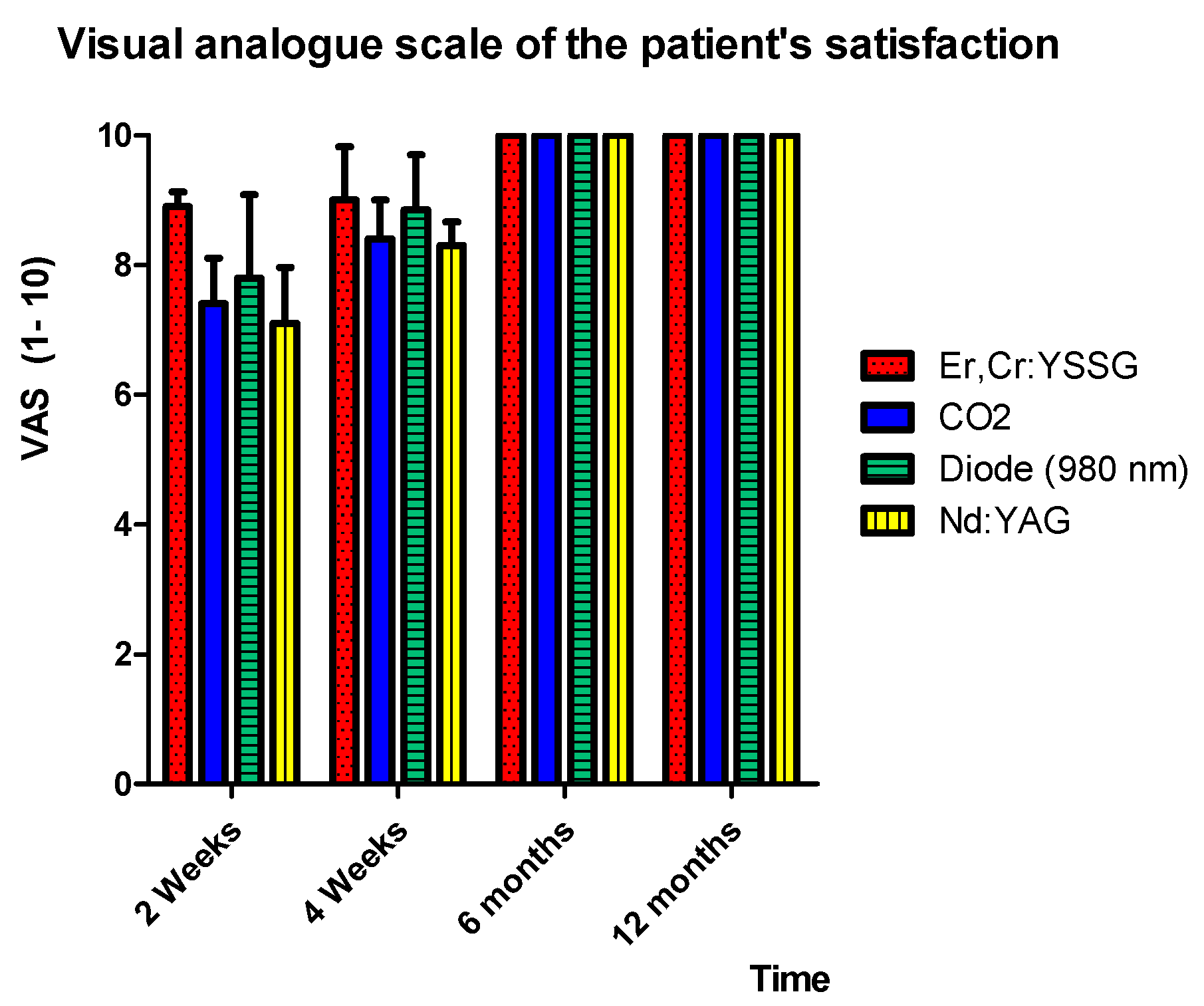
3.3. Patient Satisfaction
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Jackson, I.T.; Carreño, R.; Potparic, Z.; Hussain, K. Hemangiomas, vascular malformations, and lymphovenous malformations: Classification and methods of treatment. Plast. Reconstr. Surg. 1993, 91, 1216–1230. [Google Scholar] [CrossRef] [PubMed]
- Merrow, A.C.; Gupta, A.; Patel, M.N.; Adams, D.M. 2014 Revised classification of vascular lesions from the International Society for the Study of Vascular Anomalies: Radiologic-pathologic update. Radiographics 2016, 36, 1494–1516. [Google Scholar] [CrossRef] [PubMed]
- Cox, J.A.; Bartlett, E.; Lee, E.I. Vascular malformations: A review. Semin. Plast. Surg. 2014, 28, 58. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, D.T.; Hebling, E.; Santos-Silva, A.R.; Lopes, M.A.A. Series of 33 older patients with lip venous lake treated by sclerotherapy. Int. J. Derm. 2019, 59, 42–46. [Google Scholar] [CrossRef]
- Ernemann, U.; Kramer, U.; Miller, S.; Bisdas, S.; Rebmann, H.; Breuninger, H.; Zwick, C.; Hoffmann, J. Current concepts in the classification, diagnosis and treatment of vascular anomalies. Eur. J. Radiol. 2010, 75, 2–11. [Google Scholar] [CrossRef]
- Vesnaver, A.; Dovs, D.A. Treatment of vascular lesions in the head and neck using Nd: YAG laser. J. Cranio-Maxillofac. Surg. 2006, 34, 17–24. [Google Scholar] [CrossRef]
- Maguiness, S.M.; Frieden, I.J. Current management of infantile hemangiomas. Inseminars Cutan. Med. Surg. 2010, 30, 106–114. [Google Scholar] [CrossRef]
- Nouri, K. Lasers in Dermatology and Medicine: Dermatologic Applications; Springer: Heidelberg, Germany, 2018. [Google Scholar]
- Almutairi, N.; Alshaiji, J. Lasers for Vascular Lesions. Pediatric chapter 17, Book Editors: Keyvan Nouri, Latanya Benjamin, Jasem Alshaiji, Jan Izakovic, Pediatric Dermatologic Surgery; 2019 John Wiley & Sons Ltd.: Chichester, UK, 2019; pp. 189–196. [Google Scholar]
- Voyatzi, M.; Grammatikopoulou, J.; Karlafti, E.; Mavroudi, A.; Lamprou, F.; Kypri, G.; Tsirmigka, M. Effcacy of lasers on vascular lesions and rejuvenation. SM Dermatol. J. 2017, 3, 1009. [Google Scholar] [CrossRef]
- Bordin-Aykroyd, S.; Dias, R.B.; Lynch, E. Laser-tissue interaction. EC Dent. Sci. 2019, 18, 2303–2308. [Google Scholar]
- Ash, C.; Dubec, M.; Donne, K.; Bashford, T. Effect of wavelength and beam width on penetration in light-tissue interaction using computational methods. Lasers Med. Sci. 2017, 32, 1909–1918. [Google Scholar] [CrossRef]
- Parker, S.; Cronshaw, M.; Anagnostaki, E.; Mylona, V.; Lynch, E.; Grootveld, M. Current Concepts of Laser–Oral Tissue Interaction. Dent. J. 2020, 8, 61. [Google Scholar] [CrossRef] [PubMed]
- Dover, J.S.; Arndt, K.A. New approaches to the treatment of vascular lesions. Lasers Surg. Med. 2000, 26, 158–163. [Google Scholar] [CrossRef]
- Beausang, E.; Floyd, H.; Dunn, K.W.; Orton, C.I.; Ferguson, M.W. A new quantitative scale for clinical scar assessment. Plast. Reconstr. Surg. 1998, 102, 1954–1961. [Google Scholar] [CrossRef] [PubMed]
- Goldman, L. Effects of new laser systems on the skin. Arch. Dermatol. 1973, 108, 385–390. [Google Scholar] [CrossRef]
- Goldman, L.; Dreffer, R.; Rockwell, R.J., Jr.; Perry, E. Treatment of portwine marks by an argon laser. J. Dermatol. Surg. Oncol. 1976, 2, 385–388. [Google Scholar] [CrossRef] [PubMed]
- Goldman, L.; Wilson, R.G. Treatment of basal cell epithelioma by laser radiation. JAMA 1964, 189, 773–775. [Google Scholar] [CrossRef] [PubMed]
- Apfelberg, D.B.; Maser, M.R.; Lash, H. Extended clinical use of the argon laser for cutaneous lesions. Arch. Dermatol. 1979, 115, 719–721. [Google Scholar] [CrossRef] [PubMed]
- Apfelberg, D.B.; Kosek, J.; Maser, M.R.; Lash, H. Histology of port wine stains following argon laser treatment. Br. J. Plast. Surg. 1979, 32, 232–237. [Google Scholar] [CrossRef]
- Cosman, B. Clinical experience in the laser therapy of port wine stains. Lasers Surg. Med. 1980, 1, 133–152. [Google Scholar] [CrossRef]
- Riggle, G.C.; Hoye, R.C.; Ketcham, A.S. Laser effects on normal and tumor tissue. In Laser Applications in Medicine and Biology; Springer: Heidelberg, Germany, 1971; pp. 35–65. [Google Scholar]
- Nelson, J.S.; Jia, W.; Phung, T.L.; Mihm, M.C., Jr. Observations on enhanced port wine stain blanching induced by combined pulsed dye laser and rapamycin administration. Lasers Surg. Med. 2011, 43, 939. [Google Scholar] [CrossRef]
- Bhatnagar, A.; Jindal, M.K. Excision of Capillary Hemangioma by Diode Laser. EC Dent. Sci. 2017, 13, 07–12. [Google Scholar]
- Azma, E.; Razaghi, M. Laser Treatment of Oral and Maxillofacial Hemangioma. J. Lasers Med. Sci. 2018, 9, 228. [Google Scholar] [CrossRef] [PubMed]
- Capodiferro, S.; Limongelli, L.; Tempesta, A.; Maiorano, E.; Favia, G. Diode laser treatment of venous lake of the lip. Clin. Case Rep. 2018, 6, 1923–1924. [Google Scholar] [CrossRef] [PubMed]
- Hartmann, F.; Lockmann, A.; Himpel, O.; Kühnle, I.; Hensen, J.; Schön, M.P.; Thoms, K.M. Combination therapy of oral propranolol and combined Nd: YAG/pulsed dye laser therapy in infantile hemangiomas: A retrospective analysis of 48 treated hemangiomas in 30 children. JDDG J. Der Dtsch. Dermatol. Ges. 2020, 18, 984–993. [Google Scholar]
- Fearmonti, R.; Bond, J.; Erdmann, D.; Levinson, H. A review of scar scales and scar measuring devices. Eplasty 2010, 10, 354–362. [Google Scholar]
- Glaessl, A.; Schreyer, A.G.; Wimmershoff, M.B.; Landthaler, M.; Feuerbach, S.; Hohenleutner, U. Laser surgical planning with magnetic resonance imaging–based 3-dimensional reconstructions for intralesional Nd: YAG laser therapy of a venous malformation of the neck. Arch. Dermatol. 2001, 137, 1331–1335. [Google Scholar] [CrossRef][Green Version]
- Acland, K.M.; Barlow, R.J. Lasers for the dermatologist. Br. J. Dermatol. 2000, 143, 244–255. [Google Scholar] [CrossRef]
- Wanitphakdeedecha, R.; Thanomkitti, K.; Bunyaratavej, S.; Manuskiatti, W. Efficacy and safety of 1064-nm Nd: YAG laser in treatment of onychomycosis. J. Dermatol. Treat. 2016, 27, 75–79. [Google Scholar] [CrossRef]
- Sumian, C.C.; Pitre, F.B.; Gauthier, B.E.; Bouclier, M.; Mordon, S.R. Laser skin resurfacing using a frequency doubled Nd: YAG laser after topical application of an exogenous chromophore. Lasers Surg. Med. 1999, 25, 43–50. [Google Scholar] [CrossRef]
- Apfelberg, D.B.; Maser, M.R.; Lash, H.; White, D.N. Benefits of the CO2 laser in oral hemangioma excision. Plast. Reconstr. Surg. 1985, 75, 46–50. [Google Scholar] [CrossRef]
- McCaffrey, T.V.; Cortese, D.A. Neodymium: YAG laser treatment of subglottic hemangioma. Otolaryngol. Head Neck Surg. 1986, 94, 382–384. [Google Scholar] [CrossRef] [PubMed]
- Niccoli Filho, W.D.; Americo, M.G.; Guimarães Filho, R.; Rodrigues, N.A.S. Lip hemangioma removed with CO2 laser: A case report. Braz. J. Oral Sci. 2002, 1, 89–91. [Google Scholar]
- Suh, J.J.; Lee, J.; Park, J.C.; Lim, H.C. Lip Repositioning Surgery Using an Er, Cr: YSGG Laser: A Case Series. Int. J. Periodontics Restor. Dent. 2020, 40, 437–444. [Google Scholar] [CrossRef]
- Cercadillo-Ibarguren, I.; España Tost, A.J.; Arnabat Domínguez, J.; Valmaseda Castellón, E.; Berini Aytés, L.; Gay Escoda, C. Histologic evaluation of thermal damage produced on soft tissues by CO2, Er, Cr: YSGG and diode lasers. Med. Oral Patol. Oral Cir. Bucal. 2010, 15, 912–918. [Google Scholar] [CrossRef] [PubMed]
- Vazquez, T.; Forouzandeh, M.; Gurnani, P.; Akhtar, S.; Nouri, K. Cutaneous vascular lesions in the pediatric population: A review of laser surgery applications and lesion-specific device parameters. Lasers Med. Sci. 2020, 35, 1681–1687. [Google Scholar] [CrossRef]
- Buehler, D.; Billings, S.D. Cutaneous vascular lesions. In Soft Tissue Tumors of the Skin; Springer: New York, NY, USA, 2019; pp. 235–306. [Google Scholar]
- Mannschreck, D.B.; Huang, A.H.; Lie, E.; Psoter, K.; Puttgen, K. Topical timolol as adjunct therapy to shorten oral propranolol therapy for infantile hemangiomas. Pediatric Dermatol. 2019, 36, 283–289. [Google Scholar] [CrossRef]
- Polites, S.F.; Watanabe, M.; Crafton, T.; Jenkins, T.M.; Alvarez-Allende, C.R.; Hammill, A.M.; Dasgupta, R. Surgical resection of infantile hemangiomas following medical treatment with propranolol versus corticosteroids. J. Pediatric Surg. 2019, 54, 740–743. [Google Scholar] [CrossRef]
- Park, K.H.; Jang, Y.H.; Chung, H.Y.; Lee, W.J.; Kim, D.W.; Lee, S.J. Topical timolol maleate 0.5% for infantile hemangioma; it’s effectiveness and/or adjunctive pulsed dye laser—single center experience of 102 cases in Korea. J. Dermatol. Treat. 2015, 26, 389–391. [Google Scholar] [CrossRef]
- Chang, J.W.; Cho, K.S.; Heo, W.; Lee, J.H. (CONSORT) Wound closure using Dermabond after excision of hemangioma on the lip. Medicine 2019, 98, e15342. [Google Scholar] [CrossRef]
- John, H.E.; Phen, H.S.; Mahaffey, P.J. Treatment of venous lesions of the lips and perioral area with a long-pulsed Nd: YAG laser. Br. J. Oral Maxillofac. Surg. 2016, 54, 376–378. [Google Scholar] [CrossRef]
- Scherer, K.; Waner, M. Nd:YAG lasers (1064 nm) in the treatment of venous malformations of the face and neck: Challenges and benefits. Lasers Med. Sci. 2007, 22, 119–126. [Google Scholar] [CrossRef] [PubMed]
- Mungnirandr, A.; Nuntasunti, W.; Manuskiatti, W. Neodymium-doped yttrium aluminium garnet laser treatment of pediatric venous malformation in the oral cavity. Dermatol. Surg. 2016, 42, 875–879. [Google Scholar] [CrossRef] [PubMed]
- Del Pozo, J.; Martínez-González, C.; Verea, M.M.; Fernández-Torres, R.; Fonseca, E. Venous malformations with lip involvement: Palliative treatment with carbon dioxide laser vaporization in five cases. J. Cosmet. Laser Ther. 2009, 11, 14–18. [Google Scholar] [CrossRef] [PubMed]
- A Bacci, C.; Sacchetto, L.; Zanette, G.; Sivolella, S. Diode laser to treat small oral vascular malformations: A prospective case series study. Lasers Surg. Med. 2018, 50, 111–116. [Google Scholar] [CrossRef]









| Total | Gender | Age Range (years) | Lesion Diameter (mm) | |||
|---|---|---|---|---|---|---|
| Female | Male | Average | Minimum | Maximum | ||
| 143 | 56% | 44% | 48 | 6 | 3 | 15 |
| (n = 81) | (n = 62) | (min: 43; max: 74) | ||||
| Laser Wavelength (nm) | Number of Patients |
|---|---|
| Nd:YAG, 1064 nm | 47 |
| Er,Cr:YSSG, 2780 nm | 12 |
| CO2, 10,600 nm | 52 |
| Diode laser, 980 nm | 32 |
| 143 |
| Description | Score |
|---|---|
| Color | |
| Perfect | 1 |
| Slight mismatch | 2 |
| Obvious mismatch | 3 |
| Gross mismatch | 4 |
| Matte vs. Shiny | |
| Matte | 1 |
| Shiny | 2 |
| Contour | |
| Flush with surrounding skin | 1 |
| Slightly proud/indented | 2 |
| Hypertrophic | 3 |
| Keloid | 4 |
| Distortion | |
| None | 1 |
| Mild | 2 |
| Moderate | 3 |
| Severe | 4 |
| Texture | |
| Normal | 1 |
| Just palpable | 2 |
| Firm | 3 |
| Hard | 4 |
| Laser Wavelength | MSS at Different Time of Follow-Up | |||
|---|---|---|---|---|
| 2 Weeks | 1 Month | 6 Months | 12 Months | |
| Er,Cr:YSSG | 1.71 ± 0.16 A | 1. 16 ± 0.18 B | 1 B | 1 B |
| CO2 | 1.8 ± 0.42 A | 1.5 ± 0.27 C | 1 B | 1 B |
| Diode | 2.9 ± 0.22 D | 2.2 ± 0.74 E | 1 B | 1 B |
| Nd:YAG | 2.8 ± 0.30 D | 2.5 ± 0.62 E | 1 B | 1 B |
| Laser Wavelength | Er,Cr:YSSG (Excision) | CO2 (Photo-Vaporization) | Diode (Transmucosal Photo-Thermo-Coagulation) | Nd:YAG (Transmucosal Photo-Thermo-Coagulation) |
|---|---|---|---|---|
| Recurrence rate (%) | 0 A | 0 A | 11% ±1.4% B | 8% ± 0.9% C |
| Laser Wavelength | Visual Analogue at Different Time of Follow-Up | |||
|---|---|---|---|---|
| 2 Weeks | 1 Month | 6 Months | 12 Months | |
| Er,Cr:YSSG | 8.9 ± 0.23 A | 9 ± 0.82 A | 10 B | 10 B |
| CO2 | 7.4 ± 0.7 C | 8.4 ± 0.6 D | 10 B | 10 B |
| Diode | 7.8 ± 1.58 E | 8.85 ± 0.85 A | 10 B | 10 B |
| Nd:YAG | 7.10 ± 0.86 F | 8.30 ± 0.36 D | 10 B | 10 B |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nammour, S.; El Mobadder, M.; Namour, M.; Namour, A.; Arnabat-Dominguez, J.; Grzech-Leśniak, K.; Vanheusden, A.; Vescovi, P. Aesthetic Treatment Outcomes of Capillary Hemangioma, Venous Lake, and Venous Malformation of the Lip Using Different Surgical Procedures and Laser Wavelengths (Nd:YAG, Er,Cr:YSGG, CO2, and Diode 980 nm). Int. J. Environ. Res. Public Health 2020, 17, 8665. https://doi.org/10.3390/ijerph17228665
Nammour S, El Mobadder M, Namour M, Namour A, Arnabat-Dominguez J, Grzech-Leśniak K, Vanheusden A, Vescovi P. Aesthetic Treatment Outcomes of Capillary Hemangioma, Venous Lake, and Venous Malformation of the Lip Using Different Surgical Procedures and Laser Wavelengths (Nd:YAG, Er,Cr:YSGG, CO2, and Diode 980 nm). International Journal of Environmental Research and Public Health. 2020; 17(22):8665. https://doi.org/10.3390/ijerph17228665
Chicago/Turabian StyleNammour, Samir, Marwan El Mobadder, Melanie Namour, Amaury Namour, Josep Arnabat-Dominguez, Kinga Grzech-Leśniak, Alain Vanheusden, and Paolo Vescovi. 2020. "Aesthetic Treatment Outcomes of Capillary Hemangioma, Venous Lake, and Venous Malformation of the Lip Using Different Surgical Procedures and Laser Wavelengths (Nd:YAG, Er,Cr:YSGG, CO2, and Diode 980 nm)" International Journal of Environmental Research and Public Health 17, no. 22: 8665. https://doi.org/10.3390/ijerph17228665
APA StyleNammour, S., El Mobadder, M., Namour, M., Namour, A., Arnabat-Dominguez, J., Grzech-Leśniak, K., Vanheusden, A., & Vescovi, P. (2020). Aesthetic Treatment Outcomes of Capillary Hemangioma, Venous Lake, and Venous Malformation of the Lip Using Different Surgical Procedures and Laser Wavelengths (Nd:YAG, Er,Cr:YSGG, CO2, and Diode 980 nm). International Journal of Environmental Research and Public Health, 17(22), 8665. https://doi.org/10.3390/ijerph17228665










