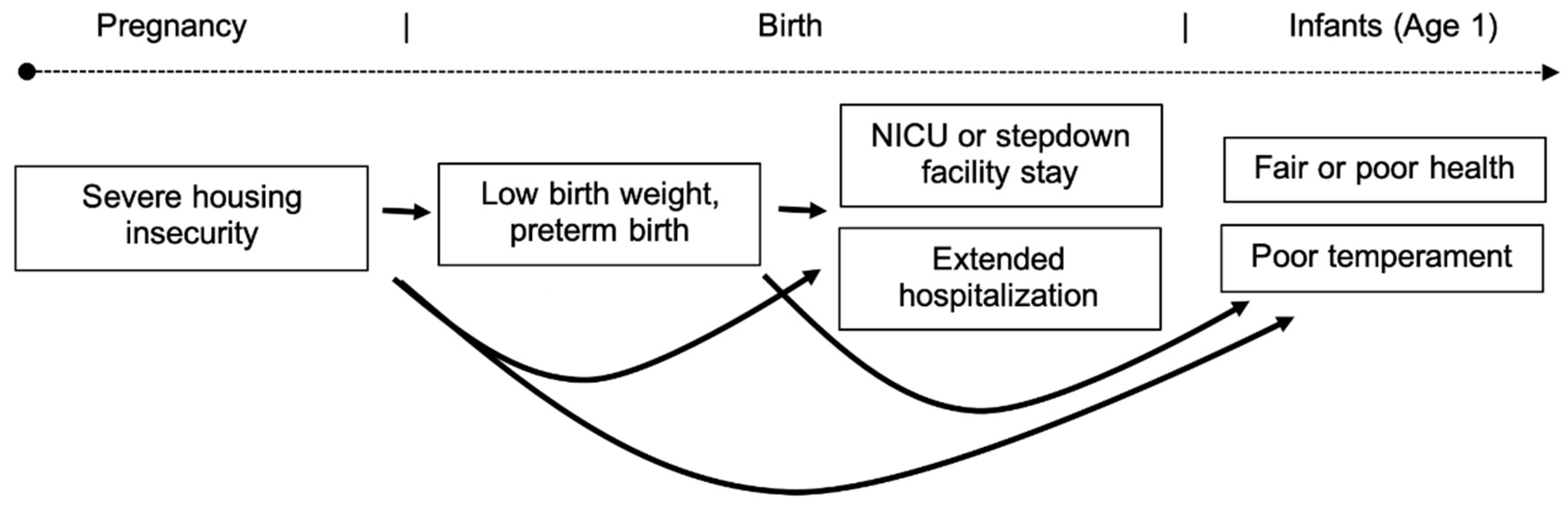
Severe Housing Insecurity during Pregnancy: Association with Adverse Birth and Infant Outcomes
Abstract
1. Introduction
2. Methods
2.1. Study Population
2.2. Measures
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| Full Source Population (N = 4898) | Birth Outcomes Study Population (N = 3428) | Infant Outcomes Study Population (N = 3035) | |
|---|---|---|---|
| Maternal factors (measured at birth) | |||
| Age | |||
| <20 | 853 (17%) | 634 (18%) | 583 (19%) |
| 20–35 | 3585 (73%) | 2484 (72%) | 2180 (72%) |
| ≥35 | 460 (9%) | 310 (9%) | 272 (9%) |
| Race/ethnicity | |||
| Non-Hispanic white | 1030 (21%) | 664 (19%) | 603 (20%) |
| Non-Hispanic Black | 2326 (47%) | 1641 (48%) | 1455 (48%) |
| Hispanic | 1336 (27%) | 979 (29%) | 854 (28%) |
| Other/missing | 206 (4%) | 144 (4%) | 123 (4%) |
| % Federal Poverty | |||
| <50% | 928 (19%) | 652 (19%) | 560 (18%) |
| 50–99% | 843 (17%) | 612 (18%) | 534 (18%) |
| 100–199% | 1262 (26%) | 898 (26%) | 799 (26%) |
| ≥200% | 1864 (38%) | 1266 (37%) | 1142 (38%) |
| Missing | 1 (<1%) | 0 | 0 |
| Education | |||
| <High school | 1699 (35%) | 1258 (37%) | 1076 (35%) |
| High school/GED | 1480 (30%) | 1031 (30%) | 921 (30%) |
| Some college | 1189 (24%) | 803 (23%) | 733 (24%) |
| ≥College degree | 524 (11%) | 332 (10%) | 303 (10%) |
| Missing | 6 (<1%) | 4 (<1%) | 2 (<1%) |
| Married | 1187 (24%) | 793 (23%) | 715 (24%) |
| Pre-pregnancy mental health problems | -- | 444 (13%) | 376 (12%) |
| Substance use during | |||
| pregnancy | |||
| Tobacco | -- | 697 (20%) | 599 (20%) |
| Alcohol | -- | 262 (8%) | 225 (7%) |
| Drugs | -- | 332 (10%) | 266 (9%) |
| Maternal preexisting conditions * | -- | 1441 (42%) | 1281 (42%) |
| Infant factors | |||
| Female sex | 2341 (48%) | 1642 (48%) | 1465 (48%) |
| Exposure | |||
| Severe housing insecurity during pregnancy | -- | 55 (2%) | 39 (1%) |
| Birth Outcomes | |||
| Low birth weight or preterm | -- | 481 (14%) | 398 (13%) |
| NICU stay or stepdown | -- | 554 (16%) | 459 (15%) |
| Extended hospitalization after delivery | -- | 586 (17%) | 499 (16%) |
References
- Desmond, M. Unaffordable America: Poverty, Housing, and Eviction. Fast Focus Inst. Res. Poverty 2015, 22, 1–6. [Google Scholar]
- Desmond, M. Eviction and the Reproduction of Urban Poverty. Am. J. Sociol. 2012, 118, 88–133. [Google Scholar] [CrossRef]
- Desmond, M.; Shollenberger, T. Forced Displacement From Rental Housing: Prevalence and Neighborhood Consequences. Demography 2015, 52, 1751–1772. [Google Scholar] [CrossRef] [PubMed]
- Desmond, M.; An, W.; Winkler, R.; Ferriss, T. Evicting Children. Soc. Forces 2013, 92, 303–327. [Google Scholar] [CrossRef]
- Leifheit, K.; Pollack, C.; Black, M.; Jennings, J. Eviction in the United States: Affected populations, housing and neighborhood-level consequences, and implications for health. In Proceedings of the Society for Epidemiologic Research Meeting, Baltimore, MD, USA, 19 June 2018. [Google Scholar]
- Greenberg, D.; Gershenson, C.; Desmond, M. Discrimination in Evictions: Empirical Evidence and Legal Challenges. Harv. Civ. Rights Civ. Lib. Law Rev. 2016, 51, 115. [Google Scholar]
- Federal Interagency Forum on Child and Family Statistics. America’s Children: Key National Indicators of Well-Being. 2019. Available online: https://www.childstats.gov/pdf/ac2019/ac_19.pdf (accessed on 20 October 2019).
- Glynn, C.; Casey, A. Homelessness Rises Faster Where Rent Exceeds a Third of Income. Available online: https://www.zillow.com/research/homelessness-rent-affordability-22247/ (accessed on 12 February 2020).
- United States Interagency Council on Homelessness. The Importance of Housing Affordability and Stability for Preventing and Ending Homelessness; United States Interagency Council on Homelessness: Washington, DC, USA, 2019. [CrossRef]
- Dunkel Schetter, C.; Tanner, L. Anxiety, depression and stress in pregnancy: Implications for mothers, children, research, and practice. Curr. Opin. Psychiatry 2012, 25, 141–148. [Google Scholar] [CrossRef]
- De Valero Bernabé, J.; Soriano, T.; Albaladejo, R.; Juarranz, M.; Calle, M.E.; Martínez, D.; Domínguez-Rojas, V. Risk factors for low birth weight: A review. Eur. J. Obstet. Gynecol. Reprod. Biol. 2004, 116, 3–15. [Google Scholar] [CrossRef]
- NICHD—Eunice Kennedy Shriver National Institute of Child Health and Human Development. What Are the Risk Factors for Preterm Labor and Birth? Available online: https://www.nichd.nih.gov/health/topics/preterm/conditioninfo/who_risk (accessed on 20 October 2019).
- Suglia, S.F.; Duarte, C.S.; Sandel, M.T. Housing quality, housing instability, and maternal mental health. J. Urban Health 2011, 88, 1105–1116. [Google Scholar] [CrossRef]
- Desmond, M.; Kimbro, R.T. Eviction’s fallout: Housing, hardship, and health. Soc. Forces 2015, 94, 295–324. [Google Scholar] [CrossRef]
- Clark, R.E.; Weinreb, L.; Flahive, J.M.; Seifert, R.W. Homelessness contributes to pregnancy complications. Health Aff. 2019, 38, 139–146. [Google Scholar] [CrossRef]
- Pantell, M.S.; Baer, R.J.; Torres, J.M.; Felder, J.N.; Manchikanti Gomez, A.; Chambers, B.D.; Dunn, J.; Parikh, N.; Pacheco-Werner, T.; Rogers, E.E.; et al. Unstable housing is linked to adverse obstetric outcomes. Am. J. Obstet. Gynecol. 2019, 220. [Google Scholar] [CrossRef]
- Cutts, D.B.; Coleman, S.; Black, M.M.; Chilton, M.M.; Cook, J.T.; de Cuba, S.E.; Heeren, T.C.; Meyers, A.; Sandel, M.; Casey, P.H.; et al. Homelessness During Pregnancy: A Unique, Time-Dependent Risk Factor of Birth Outcomes. Matern. Child Health J. 2015, 19, 1276–1283. [Google Scholar] [CrossRef] [PubMed]
- Stein, J.A.; Lu, M.C.; Gelberg, L. Severity of homelessness and adverse birth outcomes. Health Psychol. 2000, 19, 524–534. [Google Scholar] [CrossRef] [PubMed]
- Carrion, B.V.; Earnshaw, V.A.; Kershaw, T.; Lewis, J.B.; Stasko, E.C.; Tobin, J.N.; Ickovics, J.R. Housing Instability and Birth Weight among Young Urban Mothers. J. Urban Health 2015, 92, 1–9. [Google Scholar] [CrossRef]
- Hazekamp, C.; Yousuf, S.; Day, K.; Daly, M.K.; Sheehan, K. Eviction and Pediatric Health Outcomes in Chicago. J. Community Health 2020, 45, 891–899. [Google Scholar] [CrossRef]
- Sealy-Jefferson, S.; Misra, D.P. Neighborhood tax foreclosures, educational attainment, and preterm birth among urban african american women. Int. J. Environ. Res. Public Health 2019, 16, 904. [Google Scholar] [CrossRef]
- March of Dimes Long-Term Health Effects of Premature Birth. Available online: https://www.marchofdimes.org/complications/long-term-health-effects-of-premature-birth.aspx (accessed on 24 February 2020).
- Reichman, N.E.; Teitler, J.O.; Garfinkel, I.; McLanahan, S.S. Fragile Families: Sample and Design. Child. Youth Serv. Rev. 2001, 23, 303–326. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention Reproductive and Birth Outcomes. Available online: https://ephtracking.cdc.gov/showRbCollectingBirthOutcomeData (accessed on 12 February 2020).
- The Center for Consumer Information and Insurance Oversight. Newborns’ and Mothers’ Health Protection Act (NMHPA) | CMS. Available online: https://www.cms.gov/CCIIO/Programs-and-Initiatives/Other-Insurance-Protections/nmhpa_factsheet (accessed on 12 February 2020).
- Buss, A.H.; Plomin, R. Temperament: Early developing personality traits, 1984. Psychol. Behav. Sci. 2008. [Google Scholar] [CrossRef]
- Walters, G.D. Pathways to early delinquency: Exploring the individual and collective contributions of difficult temperament, low maternal involvement, and externalizing behavior. J. Crim. Justice 2014, 42, 321–326. [Google Scholar] [CrossRef]
- Larkin, S.J.; Otis, M.; Larkin Shelagh, S.J. The Relationship of Child Temperament, Maternal Parenting Stress, Maternal Child Interaction and Child Health Rating. Child Adolesc. Soc. Work J. 2019, 36, 631–640. [Google Scholar] [CrossRef]
- Berryhill, M.B.; Soloski, K.L.; Durtschi, J.A.; Adams, R.R. Family process: Early child emotionality, parenting stress, and couple relationship quality. Pers. Relatsh. 2016, 23, 23–41. [Google Scholar] [CrossRef]
- Miettinen, O.S. Proportion of disease caused or prevented by a given exposure, trait or intervention. Am. J. Epidemiol. 1974, 99, 325–332. [Google Scholar] [CrossRef] [PubMed]
- Rockhill, B.; Newman, B.; Weinberg, C. Use and misuse of population attributable fractions. Am. J. Public Health 1998, 88, 15–19. [Google Scholar] [CrossRef] [PubMed]
- National Center for Health Statistics. Natality public-use data 2016–2019. CDC WONDER Online Database. Available online: https://wonder.cdc.gov/natality-expanded-current.html (accessed on 1 December 2019).
- Kirkby, S.; Greenspan, J.S.; Kornhauser, M.; Schneiderman, R. Clinical outcomes and cost of the moderately preterm infant. Adv. Neonatal Care 2007, 7, 80–87. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, G.L.; Leifheit, K.M.; Berkman, L.; Chen, J.; Arcaya, M. Adverse health selection into eviction: Low birthweight, prematurity, and neonatal medical needs and children’s risk of eviction through age 5. In press. Available online: https://dash.harvard.edu/handle/1/37365869 (accessed on 17 November 2020).
- Aidala, A.A.; Lee, G.; Abramson, D.M.; Messeri, P.; Siegler, A. Housing need, housing assistance, and connection to HIV medical care. AIDS Behav. 2007, 11, 101–115. [Google Scholar] [CrossRef]
- Leifheit, K.M.; Schwartz, G.L.; Pollack, C.E.; Black, M.M.; Edin, K.J.; Althoff, K.N.; Jennings, J.M. Eviction in early childhood and neighborhood poverty, food security, and obesity in later childhood and adolescence: Evidence from a longitudinal birth cohort. SSM Popul. Health 2020, 11, 100575. [Google Scholar] [CrossRef]
- Kennedy, M.C.; McNeil, R.; Milloy, M.J.; Dong, H.; Kerr, T.; Hayashi, K. Residential eviction and exposure to violence among people who inject drugs in Vancouver, Canada. Int. J. Drug Policy 2017, 41, 59–64. [Google Scholar] [CrossRef]
- Goodling, E. Intersecting hazards, intersectional identities: A baseline Critical Environmental Justice analysis of US homelessness. Environ. Plan. E Nat. Sp. 2020, 3, 833–856. [Google Scholar] [CrossRef]
- US Census Bureau. Household Pulse Survey. Available online: https://www.census.gov/programs-surveys/household-pulse-survey.html (accessed on 21 August 2020).
- Benfer, E.; Bloom Robinson, D.; Butler, S.; Edmonds, L.; Gilman, S.; Mckay, K.L.; Neumann, Z.; Owens, L.; Steinkamp, N.; Yentel, D. The COVID-19 Eviction Crisis: An Estimated 30–40 Million People in America Are at Risk. Aspen Inst. 2020. [Google Scholar] [CrossRef]


| No Severe Housing Insecurity during Pregnancy (N = 3373) | Severe Housing Insecurity during Pregnancy (N = 55) | |
|---|---|---|
| Maternal Factors (Measured at Birth) | ||
| Age | ||
| <20 | 623 (18%) | 11 (20%) |
| 20–35 | 2446 (73%) | 38 (69%) |
| ≥35 | 304 (9%) | 6 (11%) |
| Race/ethnicity | ||
| Non-Hispanic white | 658 (20%) | 6 (11%) |
| Non-Hispanic Black | 1599 (47%) | 42 (76%) |
| Hispanic | 973 (29%) | 6 (11%) |
| Other/missing | 143 (4%) | 1 (2%) |
| % Federal Poverty | ||
| <50% | 637 (19%) | 15 (27%) |
| 50–99% | 594 (18%) | 18 (33%) |
| 100–199% | 882 (26%) | 16 (29%) |
| ≥200% | 1260 (37%) | 6 (11%) |
| Education | ||
| <High school | 1220 (36%) | 38 (69%) |
| High school/GED | 1022 (30%) | 9 (16%) |
| Some college | 796 (24%) | 7 (13%) |
| ≥College degree | 331 (10%) | 1 (2%) |
| Missing | 4 (<1%) | 0 |
| Married | 790 (23%) | 3 (5%) |
| Pre-pregnancy mental health problems | 409 (12%) | 35 (64%) |
| Substance use during pregnancy | ||
| Tobacco | 669 (20%) | 28 (51%) |
| Alcohol | 248 (7%) | 14 (25%) |
| Drugs | 308 (9%) | 24 (44%) |
| Maternal preexisting conditions * | 1406 (42%) | 35 (64%) |
| Infant factors | ||
| Female sex | 1611 (48%) | 31 (56%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Leifheit, K.M.; Schwartz, G.L.; Pollack, C.E.; Edin, K.J.; Black, M.M.; Jennings, J.M.; Althoff, K.N. Severe Housing Insecurity during Pregnancy: Association with Adverse Birth and Infant Outcomes. Int. J. Environ. Res. Public Health 2020, 17, 8659. https://doi.org/10.3390/ijerph17228659
Leifheit KM, Schwartz GL, Pollack CE, Edin KJ, Black MM, Jennings JM, Althoff KN. Severe Housing Insecurity during Pregnancy: Association with Adverse Birth and Infant Outcomes. International Journal of Environmental Research and Public Health. 2020; 17(22):8659. https://doi.org/10.3390/ijerph17228659
Chicago/Turabian StyleLeifheit, Kathryn M., Gabriel L. Schwartz, Craig E. Pollack, Kathryn J. Edin, Maureen M. Black, Jacky M. Jennings, and Keri N. Althoff. 2020. "Severe Housing Insecurity during Pregnancy: Association with Adverse Birth and Infant Outcomes" International Journal of Environmental Research and Public Health 17, no. 22: 8659. https://doi.org/10.3390/ijerph17228659
APA StyleLeifheit, K. M., Schwartz, G. L., Pollack, C. E., Edin, K. J., Black, M. M., Jennings, J. M., & Althoff, K. N. (2020). Severe Housing Insecurity during Pregnancy: Association with Adverse Birth and Infant Outcomes. International Journal of Environmental Research and Public Health, 17(22), 8659. https://doi.org/10.3390/ijerph17228659






