A Blended Cognitive–Behavioral Intervention for the Treatment of Postpartum Depression: Study Protocol for a Randomized Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
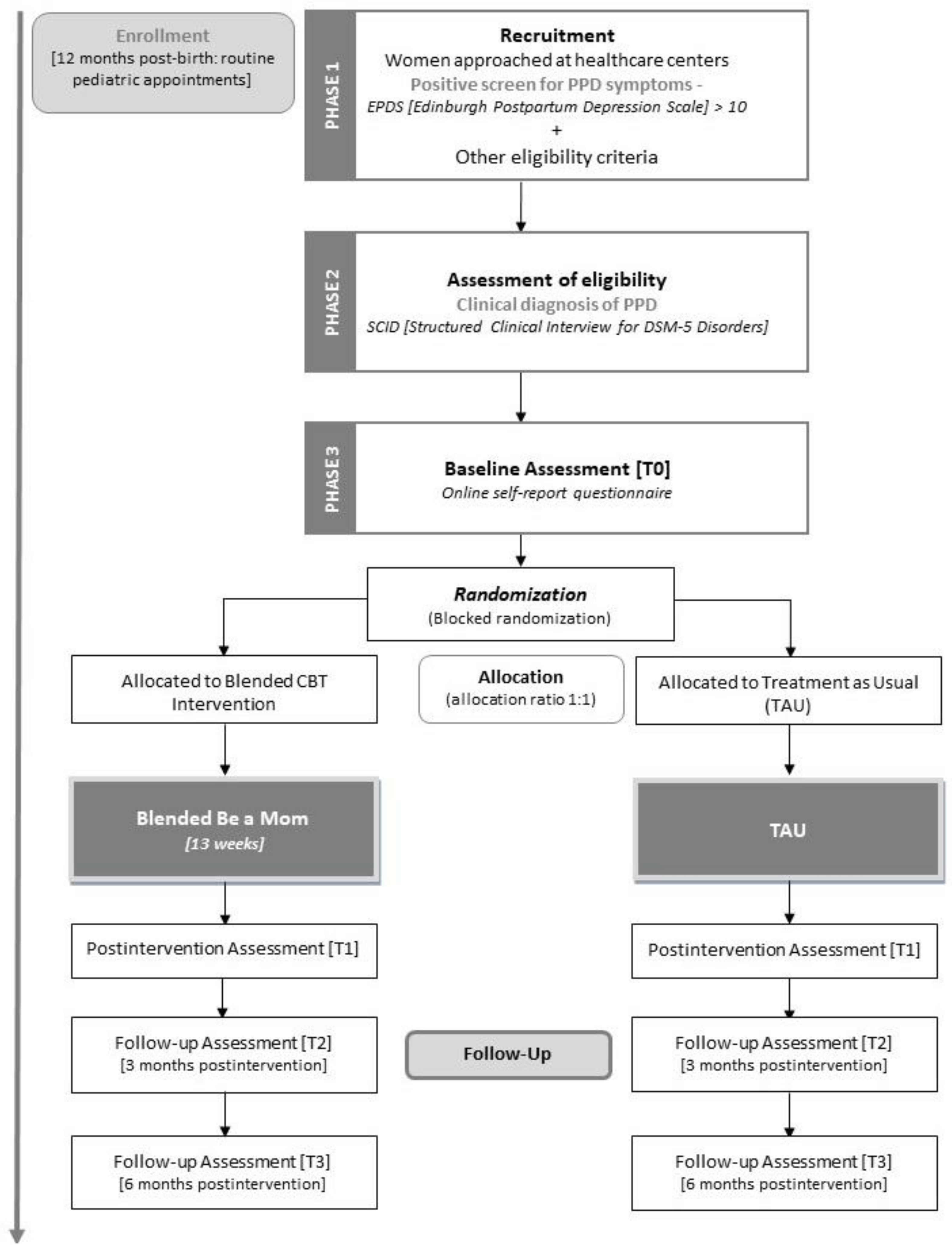
2.1. Study Design
2.2. Ethical Issues
2.3. Participants (Inclusion and Exclusion Criteria)
2.4. Recruitment and Eligibility Assessment
2.5. Randomization
2.6. Interventions
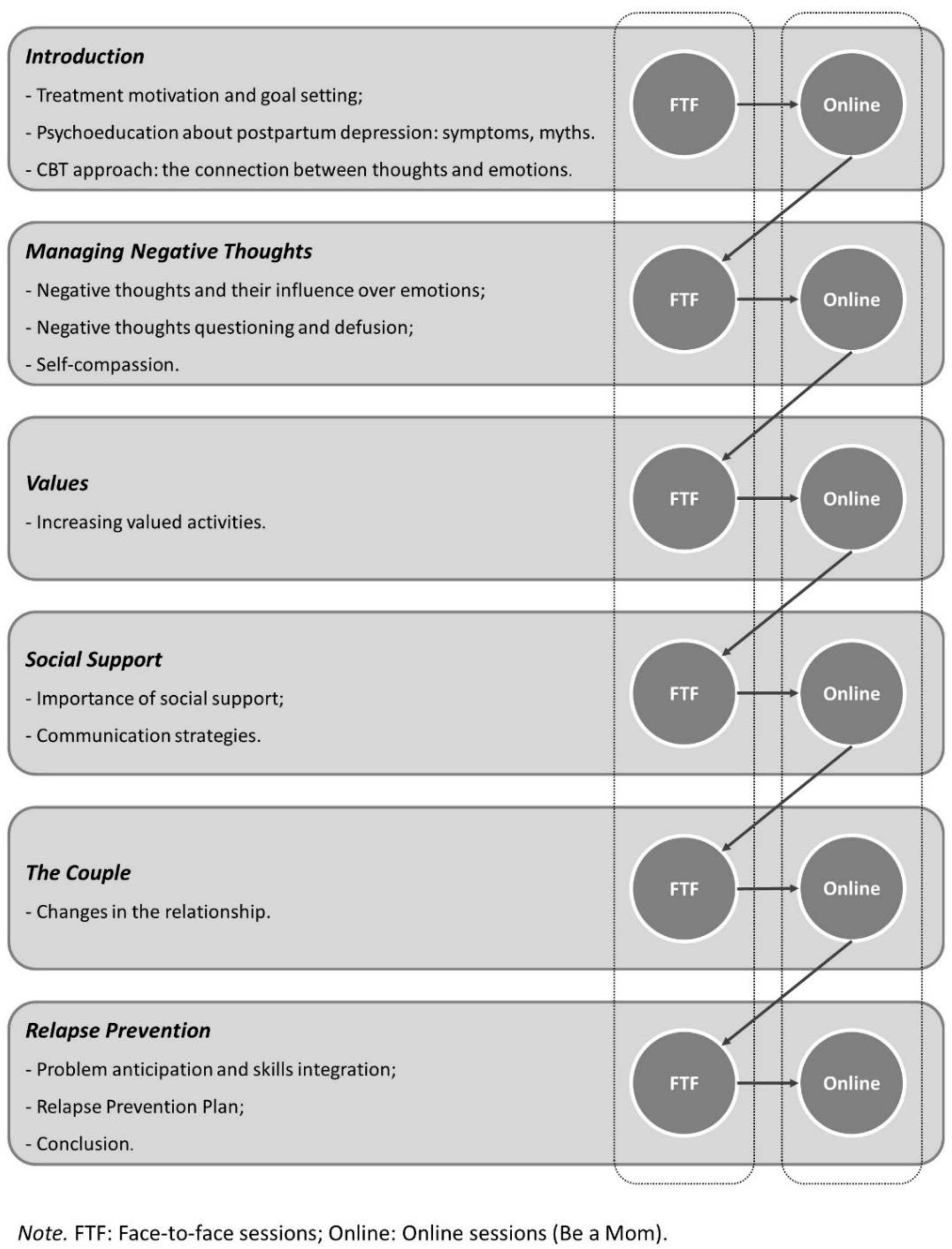
2.6.1. Blended Intervention
2.6.2. Treatment as Usual
2.7. Measures
2.7.1. Sociodemographic, Clinical, and Obstetric Information
2.7.2. Primary Outcome
2.7.3. Secondary Outcomes
2.7.4. Psychological Competences
2.7.5. Intervention-Related Outcomes
2.7.6. Economic Evaluation
2.8. Sample Size and Statistical Analyses
3. Discussion
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Maia, B.R.; Marques, M.; Bos, S.; Pereira, A.T.; Soares, M.J.; Valente, J.; Macedo, A.; Azevedo, M.H. Epidemiology of perinatal depression in Portugal: Categorical and dimensional approach. Acta Med. Port. 2011, 24, 443–448. [Google Scholar]
- Woolhouse, H.; Gartland, D.; Perlen, S.; Donath, S.; Brown, S.J. Physical health after childbirth and maternal depression in the first 12 months post partum: Results of an Australian nulliparous pregnancy cohort study. Midwifery 2014, 30, 378–384. [Google Scholar] [CrossRef] [PubMed]
- Slomian, J.; Honvo, G.; Emonts, P.; Reginster, J.Y.; Bruyère, O. Consequences of maternal postpartum depression: A systematic review of maternal and infant outcomes. Women’s Health 2019, 15, 1–55. [Google Scholar] [CrossRef] [PubMed]
- Field, T. Postpartum depression effects on early interactions, parenting, and safety practices: A review. Infant Behav. Dev. 2010, 33, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Barnes, D.L. Postpartum depression: Its impact on couples and marital satisfaction. J. Syst. Ther. 2006, 25, 25–42. [Google Scholar] [CrossRef]
- Sockol, L.E. A systematic review of the efficacy of cognitive behavioral therapy for treating and preventing perinatal depression. J. Affect. Disord. 2015, 177, 7–21. [Google Scholar] [CrossRef]
- Henshaw, E.; Sabourin, B.; Warning, M. Treatment-seeking behaviors and attitudes survey among women at risk for perinatal depression or anxiety. J. Obs. Gynecol. Neonatal Nurs. 2013, 42, 168–177. [Google Scholar] [CrossRef]
- Fonseca, A.; Gorayeb, R.; Canavarro, M.C. Women’s help-seeking behaviours for depressive symptoms during the perinatal period: Socio-demographic and clinical correlates and perceived barriers to seeking professional help. Midwifery 2015, 31, 1177–1185. [Google Scholar] [CrossRef]
- Bina, R. Predictors of postpartum depression service use: A theory-informed, integrative systematic review. Women Birth 2019, 33, e24–e32. [Google Scholar] [CrossRef]
- Maloni, J.A.; Przeworski, A.; Damato, E.G. Web recruitment and internet use and preferences reported by women with postpartum depression after pregnancy complications. Arch. Psychiatr. Nurs. 2013, 27, 90–95. [Google Scholar] [CrossRef]
- Riper, H.; Andersson, G.; Christensen, H.; Cuijpers, P.; Lange, A.; Eysenbach, G. Theme issue on e-mental health: A growing field in internet research. J. Med. Internet Res. 2010, 12, e74. [Google Scholar] [CrossRef]
- Lal, S.; Adair, C.E. E-mental health: A rapid review of the literature. Psychiatr. Serv. 2014, 65, 24–32. [Google Scholar] [CrossRef] [PubMed]
- Fonseca, A.; Gorayeb, R.; Canavarro, M.C. Women’s use of online resources and acceptance of e-mental health tools during the perinatal period. Int. J. Med. Inform. 2016, 94, 228–236. [Google Scholar] [CrossRef] [PubMed]
- Jannati, N.; Mazhari, S.; Ahmadian, L.; Mirzaee, M. Effectiveness of an app-based cognitive behavioral therapy program for postpartum depression in primary care: A randomized controlled trial. Int. J. Med. Inform. 2020, 141, 104145. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.W.; Denison, F.C.; Hor, K.; Reynolds, R.M. Web-based interventions for prevention and treatment of perinatal mood disorders: A systematic review. BMC Pregnancy Childbirth 2016, 16, 38. [Google Scholar] [CrossRef] [PubMed]
- Nair, U.; Armfield, N.R.; Chatfield, M.D.; Edirippulige, S. The effectiveness of telemedicine interventions to address maternal depression: A systematic review and meta-analysis. J. Telemed. Telecare 2018, 24, 639–650. [Google Scholar] [CrossRef] [PubMed]
- Danaher, B.G.; Milgrom, J.; Seeley, J.R.; Stuart, S.; Schembri, C.; Tyler, M.S.; Ericksen, J.; Lester, W.; Gemmill, A.; Kosty, D.B.; et al. MomMoodBooster web-based intervention for postpartum depression: Feasibility trial results. J. Med. Internet Res. 2013, 15, 1–20. [Google Scholar] [CrossRef]
- O’Mahen, H.A.; Woodford, J.; McGinley, J.; Warren, F.C.; Richards, D.A.; Lynch, T.R.; Taylor, R.S. Internet-based behavioral activation—Treatment for postnatal depression (Netmums): A randomized controlled trial. J. Affect. Disord. 2013, 150, 814–822. [Google Scholar] [CrossRef]
- Sheeber, L.B.; Seeley, J.R.; Feil, E.G.; Davis, B.; Sorensen, E.; Kosty, D.B.; Lewinsohn, P.M. Development and pilot evaluation of an internet-facilitated cognitive-behavioral intervention for maternal depression. J. Consult. Clin. Psychol. 2012, 80, 739–749. [Google Scholar] [CrossRef]
- Andersson, G.; Titov, N. Advantages and limitations of Internet-based interventions for common mental disorders. World Psychiatry 2014, 13, 4–11. [Google Scholar] [CrossRef]
- Schuster, R.; Pokorny, R.; Berger, T.; Topooco, N.; Laireiter, A.R. The advantages and disadvantages of online and blended therapy: Survey study amongst licensed psychotherapists in Austria. J. Med. Internet Res. 2018, 20, e11007. [Google Scholar] [CrossRef] [PubMed]
- Van der Vaart, R.; Witting, M.; Riper, H.; Kooistra, L.; Bohlmeijer, E.T.; van Gemert-Pijnen, L.J. Blending online therapy into regular face-to-face therapy for depression: Content, ratio and preconditions according to patients and therapists using a delphi study. BMC Psychiatry 2014, 14, 355. [Google Scholar] [CrossRef] [PubMed]
- Wentzel, J.; van der Vaart, R.; Bohlmeijer, E.T.; van Gemert-Pijnen, J.E. Mixing online and face-to-face therapy: How to benefit from blended care in mental health care. JMIR Ment. Health 2016, 3, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Erbe, D.; Eichert, H.C.; Riper, H.; Ebert, D.D. Blending face-to-face and internet-based interventions for the treatment of mental disorders in adults: Systematic review. J. Med. Internet Res. 2017, 19, 1–22. [Google Scholar] [CrossRef]
- Mol, M.; van Genugten, C.; Dozeman, E.; van Schaik, D.J.; Draisma, S.; Riper, H.; Smit, J.H. Why uptake of blended internet-based interventions for depression is challenging: A qualitative study on therapists’ perspectives. J. Clin. Med. 2020, 9, 91. [Google Scholar] [CrossRef]
- Titzler, I.; Saruhanjan, K.; Berking, M.; Riper, H.; Ebert, D.D. Barriers and facilitators for the implementation of blended psychotherapy for depression: A qualitative pilot study of therapists’ perspective. Internet Interv. 2018, 12, 150–164. [Google Scholar] [CrossRef]
- Kooistra, L.C.; Ruwaard, J.; Wiersma, J.E.; van Oppen, P.; van der Vaart, R.; van Gemert-Pijnen, J.E.; Riper, H. Development and initial evaluation of blended cognitive behavioural treatment for major depression in routine specialized mental health care. Internet Interv. 2016, 4, 61–71. [Google Scholar] [CrossRef]
- Høifødt, R.S.; Lillevoll, K.R.; Griffiths, K.M.; Wilsgaard, T.; Eisemann, M.; Kolstrup, N. The clinical effectiveness of web-based cognitive behavioral therapy with face-to-face therapist support for depressed primary care patients: Randomized controlled trial. J. Med. Internet Res. 2013, 15, e153. [Google Scholar] [CrossRef]
- Kooistra, L.C.; Wiersma, J.E.; Ruwaard, J.; Neijenhuijs, K.; Lokkerbol, J.; van Oppen, P.; Smit, F.; Riper, H. Cost and effectiveness of blended versus standard cognitive behavioral therapy for outpatients with depression in routine specialized mental health care: Pilot randomized controlled trial. J. Med. Internet Res. 2019, 21, e14261. [Google Scholar] [CrossRef]
- Fonseca, A.; Monteiro, F.; Alves, S.; Gorayeb, R.; Canavarro, M.C. Be a mom, a web-based intervention to prevent postpartum depression: The enhancement of self-regulatory skills and its association with postpartum depressive symptoms. Front. Psychol. 2019, 10, 265. [Google Scholar] [CrossRef]
- Fonseca, A.; Pereira, M.; Araújo-Pedrosa, A.; Gorayeb, R.; Ramos, M.M.; Canavarro, M.C. Be a mom: Formative evaluation of a web-based psychological intervention to prevent postpartum depression. Cogn. Behav. Pract. 2018, 25, 473–495. [Google Scholar] [CrossRef]
- Fourianalistyawati, E.; Uswatunnisa, A.; Chairunnisa, A. The role of mindfulness and self compassion toward depression among pregnant women. Int. J. Public Health Sci. 2018, 7, 162–167. [Google Scholar] [CrossRef]
- Stotts, A.L.; Villarreal, Y.R.; Klawans, M.R.; Suchting, R.; Dindo, L.; Dempsey, A.; Spellman, M.; Green, C.; Northrup, T.F. Psychological flexibility and depression in new mothers of medically vulnerable infants: A mediational analysis. Matern. Child Health J. 2019, 23, 821–829. [Google Scholar] [CrossRef] [PubMed]
- World Medical Association. Declaration of Helsinki—Ethical Principles for Medical Research Involving Human Subjects. Available online: https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/ (accessed on 7 September 2020).
- American Psychological Association. Publication Manual of the American Psychological Association; American Psychological Association: Washington, DC, USA, 2020. [Google Scholar]
- Wenzel, A.; Kleiman, K. Cognitive Behavioral Therapy for Perinatal Distress; Routledge: New York, NY, USA, 2014. [Google Scholar]
- Pugh, N.E.; Hadjistavropoulos, H.D.; Dirkse, D. A randomised controlled trial of therapist-assisted, internet-delivered cognitive behavior therapy for women with maternal depression. PLoS ONE 2016, 11, e0149186. [Google Scholar] [CrossRef]
- Beck, J.S. Cognitive Therapy: Basics & Beyond; Guilford Press: New York, NY, USA, 1995. [Google Scholar]
- Shiffman, S. Ecological Momentary Assessment; Oxford Handbooks Online: Oxford, UK, 2014. [Google Scholar]
- Areias, M.E.G.; Kumar, R.; Barros, H.; Figueiredo, E. Comparative incidence of depression in women and men, during pregnancy and after childbirth: Validation of the Edinburgh postnatal depression scale in Portuguese mothers. Br. J. Psychiatry 1996, 169, 30–35. [Google Scholar] [CrossRef]
- Pais-Ribeiro, J.; Silva, I.; Ferreira, T.; Martins, A.; Meneses, R.; Baltar, M. Validation study of a Portuguese version of the hospital anxiety and depression scale. Psychol. Health Med. 2007, 12, 225–237. [Google Scholar] [CrossRef]
- Laranjeira, C.A. Translation and adaptation of the fatigue severity scale for use in Portugal. Appl. Nurs. Res. 2012, 25, 212–217. [Google Scholar] [CrossRef]
- Ferreira, P.L.; Ferreira, L.N.; Pereira, L.N. Contribution for the validation of the Portuguese version of EQ-5D. Acta Med. Port. 2013, 26, 664–675. [Google Scholar]
- Rodrigues, D.; Lopes, D. The investment model scale (IMS): Further studies on construct validation and development of a shorter version (IMS-S). J. Gen. Psychol. 2013, 140, 16–28. [Google Scholar] [CrossRef]
- Barnes, C.R.; Adamson-Macedo, E.N. Perceived maternal parenting self-efficacy (PMP S-E) tool: Development and validation with mothers of hospitalized preterm neonates. J. Adv. Nurs. 2007, 60, 550–560. [Google Scholar] [CrossRef]
- Nazaré, B.; Fonseca, A.; Canavarro, M.C. Avaliação da ligação parental ao bebé após o nascimento: Análise fatorial confirmatória da versão portuguesa do postpartum bonding questionnaire (PBQ). Laboratório Psicol. 2012, 10, 47–61. [Google Scholar]
- Moreira, H.; Gouveia, M.J.; Canavarro, M.C. A bifactor analysis of the difficulties in emotion regulation scale-short form (DERS-SF) in a sample of adolescents and adults. Curr. Psychol. 2020, 1–26. [Google Scholar] [CrossRef]
- Castilho, P.; Pinto-Gouveia, J.; Duarte, J. Evaluating the multifactor structure of the long and short versions of the self-compassion scale in a clinical sample. J. Clin. Psychol. 2015, 71, 856–870. [Google Scholar] [CrossRef] [PubMed]
- Pinto-Gouveia, J.; Gregório, S.; Dinis, A.; Xavier, A. Experiential avoidance in clinical and non-clinical samples: AAQ-II Portuguese version. Int. J. Psychol. Psychol. Ther. 2012, 12, 139–156. [Google Scholar]
- Soares, L.; Lemos, M.S. Escala de Motivação para a Terapia (Versão Portuguesa); Faculdade de Psicologia e de Ciências da Educação da Universidade do Porto: Porto, Portugal, 2003; documento não publicado. [Google Scholar]
- Ramos, M.A.F. Análise das Características Psicométricas da Versão Portuguesa do Working Aliance Inventory—Short Revised. Master’s Thesis, Universidade do Minho, Guimarães, Portugal, 2008. [Google Scholar]
- Bouwmans, C.; De Jong, K.; Timman, R.; Zijlstra-Vlasveld, M.; Van der Feltz-Cornelis, C.; Tan, S.S.; Hakkaart-van Roijen, L. Feasibility, reliability and validity of a questionnaire on healthcare consumption and productivity loss in patients with a psychiatric disorder (TiC-P). BMC Health Serv. Res. 2013, 13, 217. [Google Scholar] [CrossRef]
- Eysenbach, G.; CONSORT EHEALTH-Group. CONSORT-EHEALTH: Improving and standardizing evaluation reports of web-based and mobile health interventions. J. Med. Internet Res. 2011, 13, e126. [Google Scholar] [CrossRef]
- Schuster, R.; Schreyer, M.L.; Kaiser, T.; Berger, T.; Klein, J.P.; Moritz, S.; Laireiter, A.; Trutschnig, W. Effects of intense assessment on statistical power in randomized controlled trials: Simulation study on depression. Internet Interv. 2020, 20, 100313. [Google Scholar] [CrossRef]
- Demirci, J.R.; Bogen, D.L. Feasibility and acceptability of a mobile app in an ecological momentary assessment of early breastfeeding. Matern. Child Nutr. 2017, 13, e12342. [Google Scholar] [CrossRef]
- Wenze, S.J.; Miller, I.W. Use of ecological momentary assessment in mood disorders research. Clin. Psychol. Rev. 2010, 30, 794–804. [Google Scholar] [CrossRef]
- SPMS. Ehealth em Portugal: Visão 2020; SPMS: Lisboa, Portugal, 2015.
- European Commission. eHealth Action Plan 2012–2020—Innovative Healthcare for the 21st Century, Communication from the Commission to the European Parliament, the Council, the European Economic and Social Committee and the Committee of the Regions. Available online: http://ec.europa.eu/health/ehealth/docs/com_2012_736_en.pdf (accessed on 7 September 2020).
| Variables | Baseline [T0] | Postintervention [T1] | Follow-Up [T2] | Follow-Up [T3] |
|---|---|---|---|---|
| Sociodemographic, clinical and obstetric information | x | |||
| Depressive symptoms | x | x | x | x |
| Anxiety symptoms | x | x | x | x |
| Fatigue | x | x | x | x |
| Quality of life | x | x | x | x |
| Marital satisfaction | x | x | x | x |
| Maternal self-efficacy | x | x | x | x |
| Mother–child bonding | x | x | x | x |
| Self-compassion | x | x | ||
| Emotion regulation | x | x | ||
| Psychological flexibility | x | x | ||
| Motivation for therapy | x | x | ||
| Therapeutic relationship | x | |||
| Acceptability, satisfaction, and usability | x | |||
| Economic evaluation | x | x |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Branquinho, M.; Canavarro, M.C.; Fonseca, A. A Blended Cognitive–Behavioral Intervention for the Treatment of Postpartum Depression: Study Protocol for a Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2020, 17, 8631. https://doi.org/10.3390/ijerph17228631
Branquinho M, Canavarro MC, Fonseca A. A Blended Cognitive–Behavioral Intervention for the Treatment of Postpartum Depression: Study Protocol for a Randomized Controlled Trial. International Journal of Environmental Research and Public Health. 2020; 17(22):8631. https://doi.org/10.3390/ijerph17228631
Chicago/Turabian StyleBranquinho, Mariana, Maria Cristina Canavarro, and Ana Fonseca. 2020. "A Blended Cognitive–Behavioral Intervention for the Treatment of Postpartum Depression: Study Protocol for a Randomized Controlled Trial" International Journal of Environmental Research and Public Health 17, no. 22: 8631. https://doi.org/10.3390/ijerph17228631
APA StyleBranquinho, M., Canavarro, M. C., & Fonseca, A. (2020). A Blended Cognitive–Behavioral Intervention for the Treatment of Postpartum Depression: Study Protocol for a Randomized Controlled Trial. International Journal of Environmental Research and Public Health, 17(22), 8631. https://doi.org/10.3390/ijerph17228631






