Awareness and Use of Heated Tobacco Products among Youth Smokers in Hong Kong: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
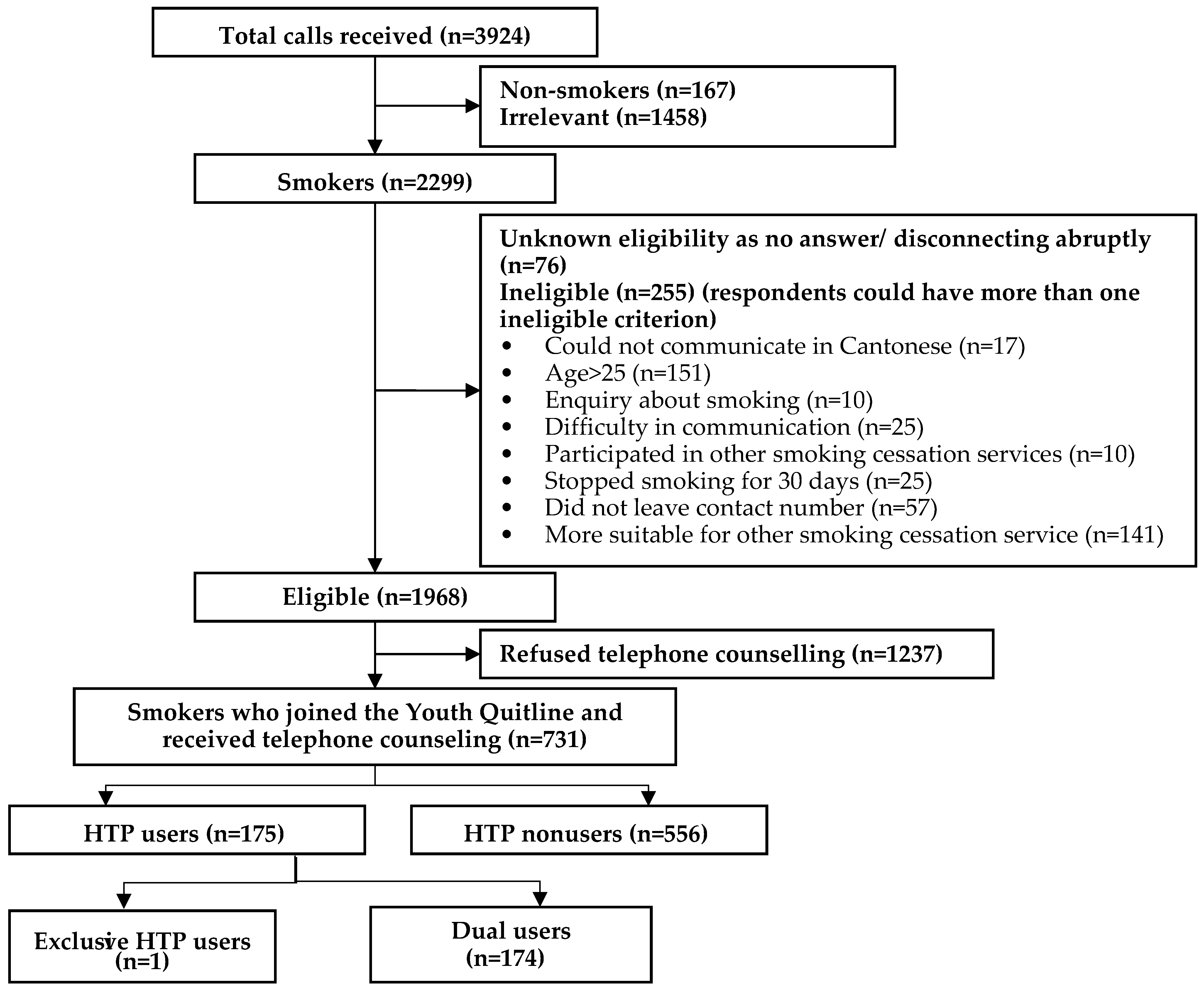
2.1. Study Design and Participants
2.2. Methods
2.3. Statistical Analysis
2.4. Ethical Approval
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Gentzke, A.S.; Creamer, M.; Cullen, K.A.; Ambrose, B.K.; Willis, G.; Jamal, A.; King, B.A. Vital Signs: Tobacco Product Use Among Middle and High School Students—United States, 2011–2018. Morb. Mortal. Wkly. Rep. 2019, 68, 157–164. [Google Scholar] [CrossRef]
- Tam, J. E-cigarette, combustible, and smokeless tobacco product use combinations among youth in the united states, 2014–2019. Addict. Behav. 2020, 112, 106636. [Google Scholar] [CrossRef]
- Kalkhoran, S.; Glantz, S.A. E-cigarettes and smoking cessation in real-world and clinical settings: A systematic review and meta-analysis. Lancet Respir. Med. 2016, 4, 116–128. [Google Scholar] [CrossRef]
- Goniewicz, M.L.; Smith, D.M.; Edwards, K.C.; Blount, B.C.; Caldwell, K.L.; Feng, J.; Wang, L.; Christensen, C.; Ambrose, B.; Borek, N.; et al. Comparison of Nicotine and Toxicant Exposure in Users of Electronic Cigarettes and Combustible Cigarettes. JAMA Netw. Open 2018, 1, e185937. [Google Scholar] [CrossRef]
- Owusu, D.; Huang, J.; Weaver, S.R.; Pechacek, T.F.; Ashley, D.L.; Nayak, P.; Eriksen, M.P. Patterns and trends of dual use of e-cigarettes and cigarettes among U.S. adults, 2015–2018. Prev. Med. Rep. 2019, 16, 101009. [Google Scholar] [CrossRef]
- Hammond, D.; Rynard, V.L.; Reid, J.L. Changes in Prevalence of Vaping Among Youths in the United States, Canada, and England from 2017 to 2019. JAMA Pediatr. 2020, 174, 797. [Google Scholar] [CrossRef]
- USA Food and Drug Administration. FDA’s Deeming Regulations for E-Cigarettes, Cigars, and All Other Tobacco Products. Available online: http://www.fda.gov/tobaccoproducts/labeling/rulesregulationsguidance/ucm394909.htm (accessed on 1 August 2020).
- National Law Information Center. National Health Promotion Act. Available online: https://www.tobaccocontrollaws.org/files/live/South%20Korea/South%20Korea%20-%20National%20Health%20Promotion%20Act%20%28No.%204914%29%20of%201995.pdf (accessed on 1 August 2020).
- Caputi, T.L. Industry watch: Heat-not-burn tobacco products are about to reach their boiling point. Tob. Control. 2017, 26, 609–610. [Google Scholar] [CrossRef]
- Simonavicius, E.; McNeill, A.; Shahab, L.; Brose, L.S. Heat-not-burn tobacco products: A systematic literature review. Tob. Control. 2019, 28, 582–594. [Google Scholar] [CrossRef]
- U.S. Food and Drug Administration. FDA Authorizes Marketing of IQOS Tobacco Heating System with ‘Reduced Exposure’ Information. Available online: https://www.fda.gov/news-events/press-announcements/fda-authorizes-marketing-iqos-tobacco-heating-system-reduced-exposure-information. (accessed on 1 August 2020).
- Papaleontiou, L.; Agaku, I.T.; Filippidis, F.T. Effects of Exposure to Tobacco and Electronic Cigarette Advertisements on Tobacco Use: An Analysis of the 2015 National Youth Tobacco Survey. J. Adolesc. Health 2020, 66, 64–71. [Google Scholar] [CrossRef]
- McKelvey, K.; Popova, L.; Kim, M.; Chaffee, B.W.; Vijayaraghavan, M.; Ling, P.; Halpern-Felsher, B. Heated tobacco products likely appeal to adolescents and young adults. Tob. Control. 2018, 27, s41–s47. [Google Scholar] [CrossRef]
- Tabuchi, T.; Gallus, S.; Shinozaki, T.; Nakaya, T.; Kunugita, N.; Colwell, B. Heat-not-burn tobacco product use in Japan: Its prevalence, predictors and perceived symptoms from exposure to secondhand heat-not-burn tobacco aerosol. Tob. Control. 2018, 27, e25–e33. [Google Scholar] [CrossRef]
- Kang, H.; Cho, S.-I. Heated tobacco product use among Korean adolescents. Tob. Control. 2019, 29, 466–468. [Google Scholar] [CrossRef]
- Census and Statistics Department. Thematic Household Survey Report no. 70: Pattern of Smoking 2020. Available online: https://www.statistics.gov.hk/pub/B11302702020XXXXB0100.pdf (accessed on 1 August 2020).
- Ho, S.-Y.; Chen, J.; Leung, L.T.; Mok, H.Y.; Wang, L.; Wang, M.P.; Lam, T.H. Adolescent Smoking in Hong Kong: Prevalence, Psychosocial Correlates, and Prevention. J. Adolesc. Health 2019, 64, S19–S27. [Google Scholar] [CrossRef]
- Lam, T.H.; He, Y. Lam and He Respond to “The Challenge of Tobacco Control in China”. Am. J. Epidemiol. 2014, 179, 1074–1075. [Google Scholar] [CrossRef][Green Version]
- Pirie, K.; Peto, R.; Reeves, G.K.; Green, J.; Beral, V. The 21st century hazards of smoking and benefits of stopping: A prospective study of one million women in the UK. Lancet 2013, 381, 133–141. [Google Scholar] [CrossRef]
- Thun, M.J.; Carter, B.D.; Feskanich, D.; Freedman, N.D.; Prentice, R.; Lopez, A.D.; Hartge, P.; Gapstur, S.M. 50-Year Trends in Smoking-Related Mortality in the United States. N. Engl. J. Med. 2013, 368, 351–364. [Google Scholar] [CrossRef]
- Chan, S.S.C.; Leung, D.Y.; Abdullah, A.S.M.; Wong, V.T.; Hedley, A.J.; Lam, T.H. A randomized controlled trial of a smoking reduction plus nicotine replacement therapy intervention for smokers not willing to quit smoking. Addiction 2011, 106, 1155–1163. [Google Scholar] [CrossRef]
- Auer, R.; Concha-Lozano, N.; Jacot-Sadowski, I.; Cornuz, J.; Berthet, A. Heat-Not-Burn Tobacco Cigarettes. JAMA Intern. Med. 2017, 177, 1050–1052. [Google Scholar] [CrossRef]
- Davis, B.; Williams, M.; Talbot, P. iQOS: Evidence of pyrolysis and release of a toxicant from plastic. Tob. Control. 2018, 28, 34–41. [Google Scholar]
- Helen, G.S.; Iii, P.J.; Nardone, N.; Benowitz, N.L. IQOS: Examination of Philip Morris International’s claim of reduced exposure. Tob. Control. 2018, 27, s30–s36. [Google Scholar] [CrossRef]
- World Health Organization. Tobacco. Available online: https://www.who.int/news-room/fact-sheets/detail/tobacco (accessed on 11 August 2020).
- Cooper, M.; Loukas, A.; Harrell, M.B.; Perry, C.L. College students’ perceptions of risk and addictiveness of e-cigarettes and cigarettes. J. Am. Coll. Heal. 2016, 65, 103–111. [Google Scholar] [CrossRef] [PubMed]
- Cooper, M.; Creamer, M.R.; Ly, C.; Crook, B.; Harrell, M.B.; Perry, C.L. Social Norms, Perceptions and Dual/Poly Tobacco Use among Texas Youth. Am. J. Health Behav. 2016, 40, 761–770. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Popova, L.; Owusu, D.; Weaver, S.R.; Kemp, C.B.; Mertz, C.K.; Pechacek, T.F.; Slovic, P. Affect, risk perception, and the use of cigarettes and e-cigarettes: A population study of U.S. adults. BMC Public Health 2018, 18, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Elton-Marshall, T.; Driezen, P.; Fong, G.T.; Cummings, K.M.; Persoskie, A.; Wackowski, O.; Choi, K.; Kaufman, A.; Strong, D.; Gravely, S.; et al. Adult perceptions of the relative harm of tobacco products and subsequent tobacco product use: Longitudinal findings from waves 1 and 2 of the population assessment of tobacco and health (PATH) study. Addict. Behav. 2020, 106, 106337. [Google Scholar] [CrossRef]
- Curry, L.A.; Youngblade, L.M. Negative affect, risk perception, and adolescent risk behavior. J. Appl. Dev. Psychol. 2006, 27, 468–485. [Google Scholar] [CrossRef]
- Reniers, R.L.; Murphy, L.; Lin, A.; Bartolomé, S.P.; Wood, S.J. Risk Perception and Risk-Taking Behaviour during Adolescence: The Influence of Personality and Gender. PLoS ONE 2016, 11, e0153842. [Google Scholar] [CrossRef]
- Roditis, M.; Delucchi, K.; Cash, D.; Halpern-Felsher, B. Adolescents’ Perceptions of Health Risks, Social Risks, and Benefits Differ Across Tobacco Products. J. Adolesc. Heal. 2016, 58, 558–566. [Google Scholar] [CrossRef]
- Brose, L.S.; Simonavicius, E.; Cheeseman, H. Awareness and Use of ’Heat-not-burn’ Tobacco Products in Great Britain. Tob. Regul. Sci. 2018, 4, 44–50. [Google Scholar] [CrossRef]
- Kim, J.; Yu, H.; Lee, S.; Paek, Y.-J. Awareness, experience and prevalence of heated tobacco product, IQOS, among young Korean adults. Tob. Control. 2018, 27, s74–s77. [Google Scholar] [CrossRef]
- Marynak, K.L.; Wang, T.W.; King, B.A.; Agaku, I.T.; Reimels, E.A.; Graffunder, C.M. Awareness and Ever Use of “Heat-Not-Burn” Tobacco Products Among U.S. Adults, 2017. Am. J. Prev. Med. 2018, 55, 551–554. [Google Scholar] [CrossRef]
- Nyman, A.L.; Weaver, S.R.; Popova, L.; Pechacek, T.F.; Huang, J.; Ashley, D.L.; Eriksen, M.P. Awareness and use of heated tobacco products among US adults, 2016–2017. Tob. Control. 2018, 27, s55–s61. [Google Scholar] [CrossRef] [PubMed]
- Chan, S.; Wong, D.C.N.; Fong, D.Y.T.; Leung, A.Y.M.; Lam, D.O.B.; Mak, Y.-W.; Lam, T.H. The Establishment and Promotion of the First Youth Quitline in Hong Kong Challenges and Opportunities. Eval. Health Prof. 2008, 31, 258–271. [Google Scholar] [CrossRef] [PubMed]
- Li, H.C.W.; Chan, S.S.C.; Wang, M.P.; Ho, K.Y.; Cheung, Y.T.; Chan, V.W.; Lam, T.H. An Evaluation of the Youth Quitline Service Young Hong Kong Smokers. J. Adolesc. Health 2017, 60, 584–591. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.-L.; Lin, H.-H.; Wang, H.-H. The psychometric properties of the Chinese version of the Fagerstrom Test for Nicotine Dependence. Addict. Behav. 2006, 31, 2324–2327. [Google Scholar] [CrossRef] [PubMed]
- Filippidis, F.T.; Laverty, A.A.; Fernandez, E.; Mons, U.; Tigova, O.; Vardavas, C.I. Correlates of self-reported exposure to advertising of tobacco products and electronic cigarettes across 28 European Union member states. Tob. Control. 2017, 26, e130–e133. [Google Scholar] [CrossRef] [PubMed]
- Singh, T.; Agaku, I.T.; Arrazola, R.A.; Marynak, K.L.; Neff, L.J.; Rolle, I.T.; King, B.A. Exposure to Advertisements and Electronic Cigarette Use Among US Middle and High School Students. Pediatrics 2016, 137, e20154155. [Google Scholar] [CrossRef] [PubMed]

| Variable | No./Total No. (%) a | |||
|---|---|---|---|---|
| All (n = 731) | HTP Nonusers (n = 556) | HTP Users (n = 175) | p-Value | |
| Age, mean (SD), y | 19.3 (2.9) | 19.1 (2.9) | 19.7 (3.0) | 0.02 |
| Sex | ||||
| Male | 607/731 (83.0) | 457/556 (82.2) | 150/175 (85.7) | 0.30 |
| Female | 124/731 (17.0) | 99/556 (17.8) | 25/175 (14.3) | |
| Marital Status | ||||
| Single | 680/692 (98.3) | 515/525 (98.1) | 165/167 (98.8) | 0.74 |
| Married/cohabitated | 12/692 (1.7) | 10/525 (1.9) | 2/167 (1.2) | |
| Educational attainment | ||||
| Lower secondary | 89/700 (12.7) | 74/533 (13.9) | 15/167 (8.9) | 0.12 |
| Upper secondary | 351/700 (50.1) | 276/533 (51.8) | 75/167 (45.0) | |
| Tertiary | 260/700 (37.2) | 183/533 (34.3) | 77/167 (46.1) | |
| Employment status | ||||
| Full-time students | 228/707 (32.3) | 189/536 (35.3) | 39/171 (22.8) | 0.02 |
| Full-time students and part-time employed | 271/707 (38.3) | 193/536 (36.0) | 78/171 (45.6) | |
| Employed | 182/707 (25.7) | 135/536 (19.1) | 47/171 (27.5) | |
| Unemployed | 26/707 (3.7) | 19/536 (2.7) | 7/171 (4.1) | |
| Age at starting smoking, mean (SD), y | 14.6 (2.9) | 14.6 (2.8) | 14.7 (3.2) | 0.59 |
| Daily cigarette consumption, mean (SD), No. | 9.2 (7.5) | 9.3 (7.8) | 8.7 (6.5) | 0.32 |
| Previous use of other tobacco products (e.g., e-cigarettes) except HTPs | ||||
| Yes | 524/731 (71.7) | 371/556 (66.7) | 153/175 (87.4) | <0.001 |
| No | 207/731 (28.3) | 185/556 (33.3) | 22/175 (12.6) | |
| Previous quit attempts (all tobacco products) | ||||
| Yes | 536/731 (73.3) | 402/556 (72.3) | 134/175 (76.6) | 0.29 |
| No | 195/731 (26.7) | 154/556 (27.7) | 41/175 (23.4) | |
| Readiness to quit (all tobacco products) | ||||
| Pre-contemplation | 292/731 (39.9) | 228/556 (41.0) | 64/175 (36.6) | 0.36 |
| Contemplation | 191/731 (26.1) | 149/556 (26.8) | 42/175 (24.0) | |
| Preparation | 173/731 (23.7) | 124/556 (22.3) | 49/175 (28.0) | |
| Action | 75/731 (10.3) | 55/556 (9.9) | 20/175 (11.4) | |
| Nicotine dependency by the Fagerström Test | ||||
| Mild, 0–3 | 492/719 (68.4) | 369/548 (67.3) | 123/171 (71.9) | 0.52 |
| Moderate, 4–5 | 163/719 (22.7) | 128/548 (23.4) | 35/171 (20.5) | |
| Severe, 6–10 | 64/719 (8.9) | 51/548 (9.3) | 13/171 (7.6) | |
| No./Total No. (%) a | ||||
|---|---|---|---|---|
| All (n = 477) | HTP Nonusers (n = 315) | HTP Users (n = 162) | p-Value | |
| HTPs are e-cigarettes | ||||
| Agree/strongly agree | 135/462 (29.2) | 76/300 (25.3) | 59/162 (36.4) | 0.01 |
| Disagree/strongly disagree | 264/462 (57.1) | 185/300 (61.7) | 79/162 (48.8) | |
| Do not know | 63/462 (13.6) | 39/300 (13.0) | 24/162 (14.8) | |
| HTPs are not addictive | ||||
| Agree/strongly agree | 71/460 (15.4) | 41/300 (13.7) | 30/160 (18.8) | 0.13 |
| Disagree/strongly disagree | 326/460 (70.9) | 219/300 (73.0) | 107/160 (66.9) | |
| Do not know | 63/460 (13.7) | 40/300 (13.3) | 23/160 (14.4) | |
| HTPs are better than conventional cigarettes in terms of health | ||||
| Agree/strongly agree | 125/474 (26.4) | 62/312 (19.9) | 63/162 (38.9) | <0.001 |
| Disagree/strongly disagree | 274/474 (57.8) | 199/312 (63.8) | 75/162 (46.3) | |
| Do not know | 75/474 (15.8) | 51/312 (16.3) | 24/162 (14.8) | |
| HTPs contain less harmful substances than conventional cigarettes | ||||
| Agree/strongly agree | 127/474 (26.8) | 64/312 (20.5) | 63/162 (38.9) | <0.001 |
| Disagree/strongly disagree | 272/474 (57.4) | 197/312 (63.1) | 75/162 (46.3) | |
| Do not know | 75/474 (15.8) | 51/312 (16.3) | 24/162 (14.8) | |
| HTPs can help with smoking cessation | ||||
| Agree/strongly agree | 92/451 (20.4) | 43/300 (14.3) | 49/151 (32.5) | <0.001 |
| Disagree/strongly disagree | 303/451 (67.2) | 212/300 (70.7) | 91/151 (60.2) | |
| Do not know | 56/451 (12.4) | 45/300 (15.0) | 11/151 (7.3) | |
| HTPs can reduce conventional cigarette consumption | ||||
| Agree/strongly agree | 106/461 (23.0) | 54/299 (18.1) | 52/162 (32.1) | 0.001 |
| Disagree/strongly disagree | 287/461 (62.3) | 200/299 (66.9) | 87/162 (53.7) | |
| Do not know | 68/461 (14.8) | 45/299 (15.1) | 23/162 (14.2) | |
| HTPs should be banned | ||||
| Agree/strongly agree | 101/466 (21.7) | 66/307 (21.5) | 35/159 (22.0) | 0.79 |
| Disagree/strongly disagree | 285/466 (61.2) | 182/307 (59.3) | 103/159 (64.8) | |
| Do not know/No comment | 80/466 (17.2) | 59/307 (19.2) | 21/159 (13.2) | |
| Government should regulate HTPs but not ban | ||||
| Agree/strongly agree | 228/462 (49.4) | 140/300 (46.7) | 88/162 (54.3) | 0.12 |
| Disagree/strongly disagree | 168/462 (36.4) | 116/300 (38.7) | 52/162 (32.1) | |
| Do not know/No comment | 66/462 (14.3) | 44/300 (14.7) | 22/162 (13.6) | |
| Banning of e-cigarettes and HTPs would be more efficient to control the consumptions of these products than promoting smoking cessation | ||||
| Agree/strongly agree | 141/462 (30.5) | 97/300 (32.3) | 44/162 (27.2) | 0.21 |
| Disagree/strongly disagree | 251/462 (54.3) | 157/300 (52.3) | 94/162 (58.0) | |
| Do not know/No comment | 70/462 (15.2) | 46/300 (15.3) | 24/162 (14.8) | |
| Reason for Using HTPs b | No./Total No. (%) a |
|---|---|
| Curiosity | 70/150 (46.7) |
| Peer influence | 50/150 (33.3) |
| Perceived health benefits | 14/150 (9.3) |
| Use as a smoking cessation aid | 13/150 (8.7) |
| Others | 3/150 (2.0) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ho, L.L.K.; Li, W.H.C.; Cheung, A.T.; Xia, W.; Lam, T.H. Awareness and Use of Heated Tobacco Products among Youth Smokers in Hong Kong: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2020, 17, 8575. https://doi.org/10.3390/ijerph17228575
Ho LLK, Li WHC, Cheung AT, Xia W, Lam TH. Awareness and Use of Heated Tobacco Products among Youth Smokers in Hong Kong: A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2020; 17(22):8575. https://doi.org/10.3390/ijerph17228575
Chicago/Turabian StyleHo, Laurie Long Kwan, William Ho Cheung Li, Ankie Tan Cheung, Wei Xia, and Tai Hing Lam. 2020. "Awareness and Use of Heated Tobacco Products among Youth Smokers in Hong Kong: A Cross-Sectional Study" International Journal of Environmental Research and Public Health 17, no. 22: 8575. https://doi.org/10.3390/ijerph17228575
APA StyleHo, L. L. K., Li, W. H. C., Cheung, A. T., Xia, W., & Lam, T. H. (2020). Awareness and Use of Heated Tobacco Products among Youth Smokers in Hong Kong: A Cross-Sectional Study. International Journal of Environmental Research and Public Health, 17(22), 8575. https://doi.org/10.3390/ijerph17228575





