Mediterranean Lifestyle to Promote Physical, Mental, and Environmental Health: The Case of Chile
Abstract
1. Introduction
2. The Mediterranean Diet in the Current Chronic Disease Context
3. Mediterranean-Type Ecosystem of Central Chile and Local Implications for Chronic Disease Management
4. Beyond a Healthy Eating Pattern: Linking the Mediterranean Lifestyle to Mental Health and Well-Being
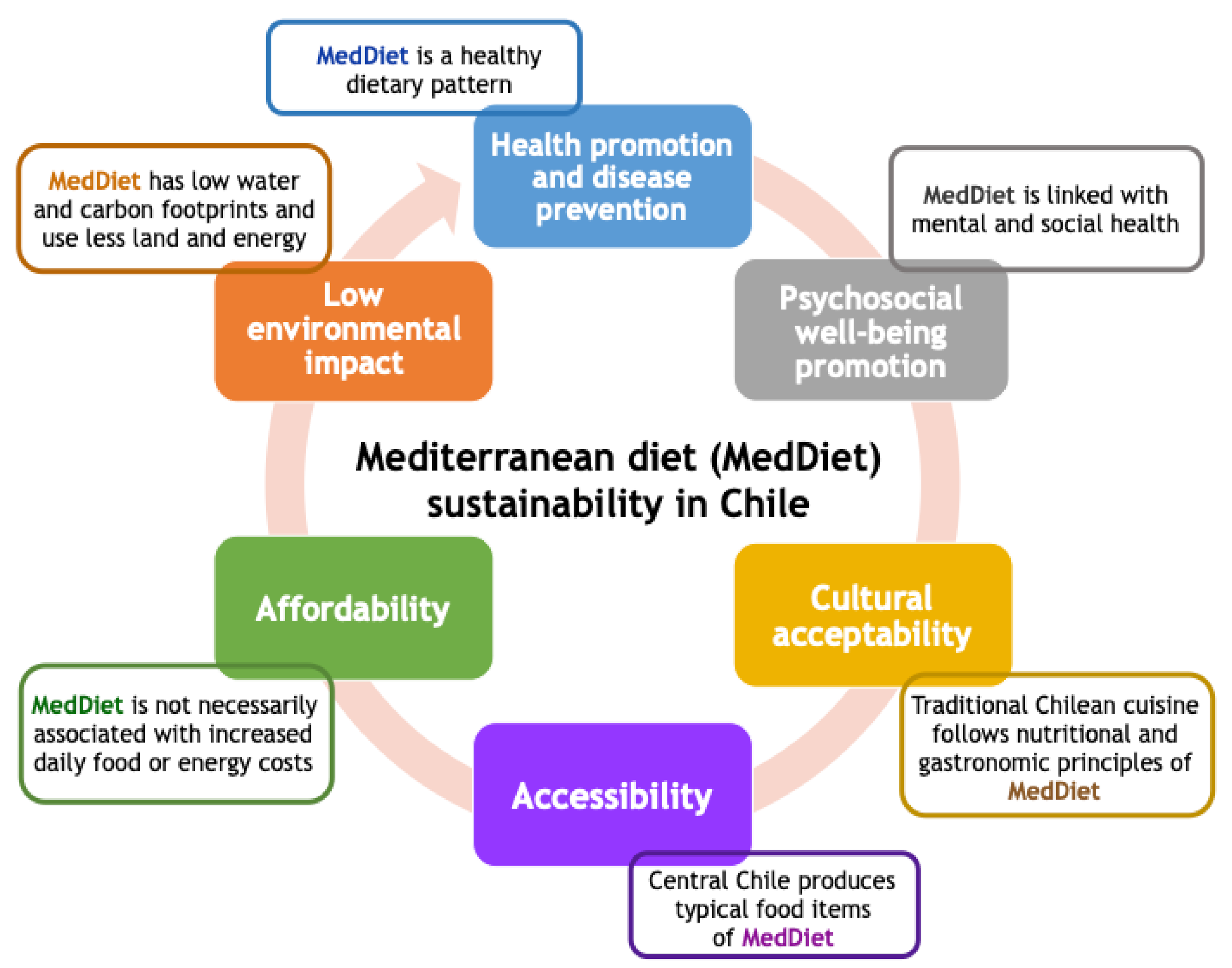
5. Sustainability of the Mediterranean Diet
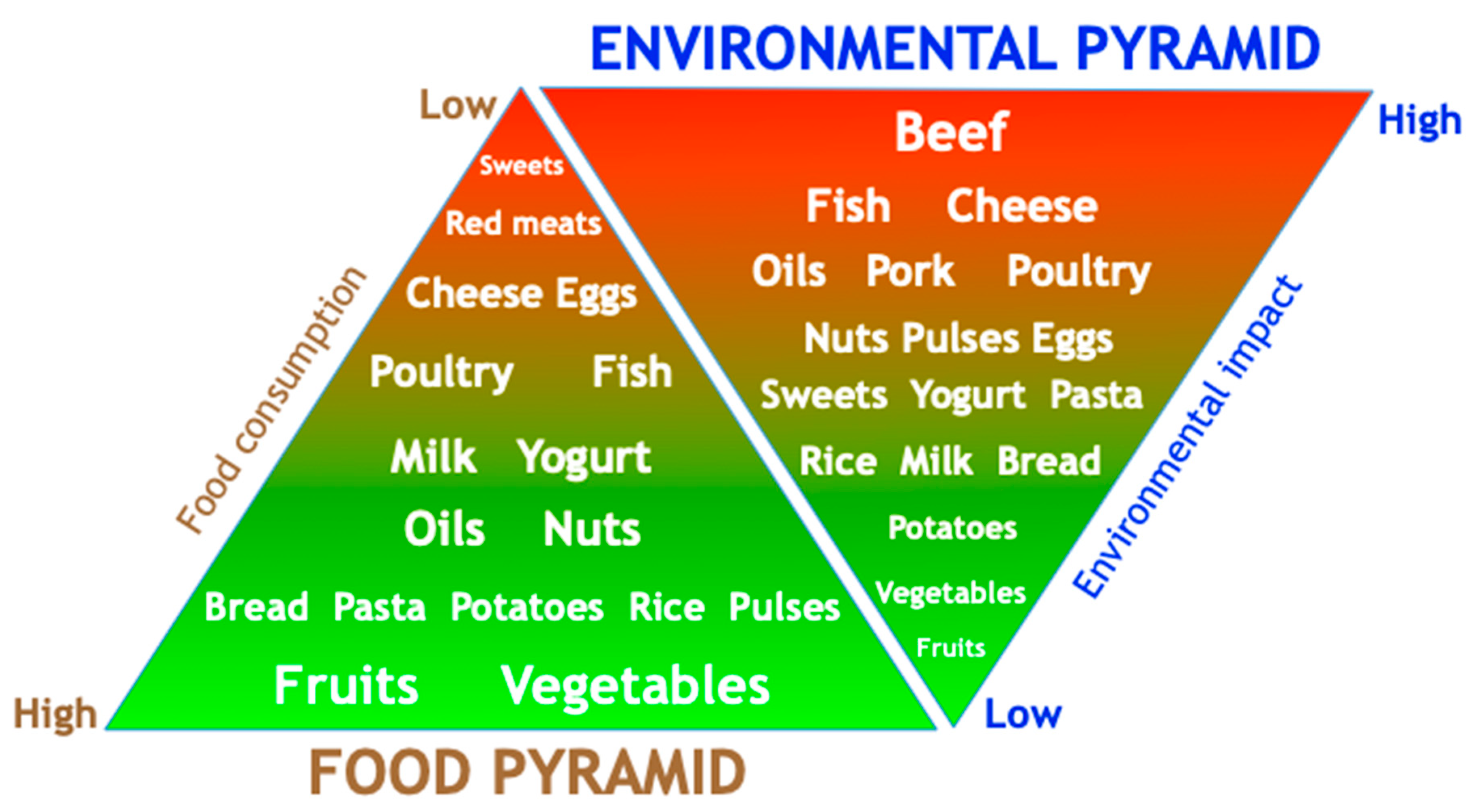
5.1. Mediterranean Diet and the Environment
5.2. Mediterranean Diet and Cultural Acceptance
5.3. Mediterranean Diet and Economical Costs and Accessibility
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- WHO. Global Status Report on Noncommunicable Diseases. Attaining the Nine Global Noncommunicable Diseases Targets: A Shared Responsibility; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Carney, R.M.; Freedland, K.E. Depression and coronary heart disease. Nat. Rev. Cardiol. 2017, 14, 145–155. [Google Scholar] [CrossRef]
- Pan, A.; Keum, N.; Okereke, O.I.; Sun, Q.; Kivimaki, M.; Rubin, R.R.; Hu, F.B. Bidirectional Association Between Depression and Metabolic Syndrome: A systematic review and meta-analysis of epidemiological studies. Diabetes Care 2012, 35, 1171–1180. [Google Scholar] [CrossRef]
- DuBois, C.M. Relationships between positive psychological constructs and health outcomes in patients with cardiovascular disease: A systematic review. Int. J. Cardiol. 2015, 195, 265–280. [Google Scholar] [CrossRef]
- MINSAL Chile 2018. Available online: http://www.deis.cl/defunciones-y-mortalidad-por-causas (accessed on 6 July 2020).
- MINSAL Chile 2018. Available online: https://www.minsal.cl/wp-content/uploads/2017/11/ENS-2016-17_PRIMEROS-RESULTADOS.pdf (accessed on 6 July 2020).
- Pedersen, S.S.; Von Känel, R.; Tully, P.J.; Denollet, J. Psychosocial perspectives in cardiovascular disease. Eur. J. Prev. Cardiol. 2017, 24, 108–115. [Google Scholar] [CrossRef]
- García-Fernández, E.; Rico-Cabanas, L.; Rosgaard, N.; Estruch, R.; Bach-Faig, A. Mediterranean Diet and Cardiodiabesity: A Review. Nutrients 2014, 6, 3474–3500. [Google Scholar] [CrossRef]
- Dussaillant, C.; Echeverría, G.; Urquiaga, I.; Velasco, N.; Rigotti, A. Current evidence on health benefits of the Mediterranean diet. Rev. Med. Chile 2016, 144, 1044–1052. [Google Scholar]
- Dinu, M.; Pagliai, G.; Casini, A.; Sofi, F. Mediterranean diet and multiple health outcomes: An umbrella review of meta-analyses of observational studies and randomised trials. Eur. J. Clin. Nutr. 2017, 72, 30–43. [Google Scholar] [CrossRef]
- Soltani, S.; Jayedi, A.; Shab-Bidar, S.; Becerra-Tomas, N.; Salas-Salvadó, J. Adherence to the Mediterranean Diet in Relation to All-Cause Mortality: A Systematic Review and Dose-Response Meta-Analysis of Prospective Cohort Studies. Adv. Nutr. 2019, 10, 1029–1039. [Google Scholar] [CrossRef]
- Kargın, D.; Tomaino, L.; Serra-Majem, L. Experimental Outcomes of the Mediterranean Diet: Lessons Learned from the Predimed Randomized Controlled Trial. Nutrients 2019, 11, 2991. [Google Scholar] [CrossRef]
- Sánchez-Sánchez, M.L.; García-Vigara, A.; Hidalgo-Mora, J.J.; García-Pérez, M.Á.; Tarín, J.; Cano, A. Mediterranean diet and health: A systematic review of epidemiological studies and intervention trials. Maturitas 2020, 136, 25–37. [Google Scholar] [CrossRef]
- De Lorgeril, M.; Renaud, S.; Salen, P.; Monjaud, I.; Mamelle, N.; Martin, J.; Guidollet, J.; Touboul, P.; Delaye, J. Mediterranean alpha-linolenic acid-rich diet in secondary prevention of coronary heart disease. Lancet 1994, 343, 1454–1459. [Google Scholar] [CrossRef]
- Estruch, R.; Ros, E.; Salas-Salvadó, J.; Covas, M.-I.; Corella, D.; Arós, F.; Gómez-Gracia, E.; Ruiz-Gutiérrez, V.; Fiol, M.; Lapetra, J.; et al. Primary Prevention of Cardiovascular Disease with a Mediterranean Diet. N. Engl. J. Med. 2013, 368, 1279–1290. [Google Scholar] [CrossRef]
- Estruch, R.; Ros, E.; Salas-Salvadó, J.; Covas, M.I.; Corella, D.; Arós, F.; Gómez-Gracia, E.; Ruiz-Gutiérrez, V.; Fiol, M.; Lapetra, J.; et al. Retraction and Republication: Primary Prevention of Cardiovascular Disease with a Med-iterranean Diet. N. Engl. J. Med. 2018, 378, 2441–2442. [Google Scholar] [CrossRef]
- Salas-Salvadó, J.; Bulló, M.; Babio, N.; Martínez-González, M.Á.; Ibarrola-Jurado, N.; Basora, J.; Estruch, R.; Covas, M.I.; Corella, D.; Arós, F.; et al. Reduction in the Incidence of Type 2 Diabetes With the Mediterranean Diet: Results of the PREDIMED-Reus nutrition intervention randomized trial. Diabetes Care 2010, 34, 14–19. [Google Scholar] [CrossRef]
- Diaz-Lopez, A. Mediterranean diet, retinopathy, nephropathy, and microvascular diabetes complications: A post hoc analysis of a randomized trial. Diabetes Care 2015, 38, 2134–2141. [Google Scholar] [CrossRef]
- Valls-Pedret, C.; Sala-Vila, A.; Serra-Mir, M.; Corella, D.; de la Torre, R.; Martínez-González, M.Á.; Martínez-Lapiscina, E.H.; Fitó, M.; Pérez-Heras, A.; Salas-Salvadó, J.; et al. Mediterranean Diet and Age-Related Cognitive Decline. JAMA Intern. Med. 2015, 175, 1094–1103. [Google Scholar] [CrossRef]
- Toledo, E.; Salas-Salvadó, J.; Donat-Vargas, C.; Cosiales, P.B.; Estruch, R.; Ros, E.; Corella, D.; Fitó, M.; Hu, F.B.; Arós, F.; et al. Mediterranean Diet and Invasive Breast Cancer Risk Among Women at High Cardiovascular Risk in the PREDIMED Trial. JAMA Intern. Med. 2015, 175, 1752–1760. [Google Scholar] [CrossRef]
- Martínez-González, M.; Buil-Cosiales, P.; Corella, D.; Bulló, M.; Fitó, M.; Vioque, J.; Romaguera, D.; Martínez, J.A.; Wärnberg, J.; López-Miranda, J.; et al. Cohort Profile: Design and methods of the PREDIMED-Plus randomized trial. Int. J. Epidemiol. 2018, 48, 387–388. [Google Scholar] [CrossRef]
- Sotos-Prieto, M. Rationale and design of feeding America’s bravest: Mediterranean diet-based intervention to change firefighters’ eating habits and improve cardiovascular risk profiles. Contemp. Clin. Trials 2017, 61, 101–107. [Google Scholar] [CrossRef]
- Itsiopoulos, C.; Kucianski, T.; Mayr, H.L.; Van Gaal, W.J.; Martínez-González, M.Á.; Vally, H.; Kingsley, M.; Kouris-Blazos, A.; Radcliffe, J.; Segal, L.; et al. The AUStralian MEDiterranean Diet Heart Trial (AUSMED Heart Trial): A randomized clinical trial in secondary prevention of coronary heart disease in a multiethnic Australian population: Study protocol. Am. Heart J. 2018, 203, 4–11. [Google Scholar] [CrossRef]
- Köppen, V. Das Geographische System der Climate; Köppen, V., Geiger, R., Eds.; Gebrüder Borntraeger: Berlin, Germany, 1936. [Google Scholar]
- Armesto, J.J. The Mediterranean environment of Central Chile; Oxford University Press: Oxford, UK, 2007. [Google Scholar]
- Chilealimentos. Evolución Exportaciones de Alimentos. Available online: https://chilealimentos.com/ventajas_categoria/evolucion-exportaciones-de-alimentos/ (accessed on 8 July 2020).
- Rozowski, J. Is the Chilean diet a Mediterranean-type diet? Biol. Res. 2004, 37, 313–319. [Google Scholar] [CrossRef] [PubMed]
- Urquiaga, I.; Echeverría, G.; Dussaillant, C.; Rigotti, A. Origin, components and mechanisms of action of the Mediterranean diet. Rev. Med. Chile 2017, 145, 85–95. [Google Scholar] [CrossRef] [PubMed]
- Echeverría, G.; Dussaillant, C.; McGee, E.; Inés, U.; Velasco, N.; Rigotti, A. Mediterranean diet beyond the mediterranean basin: Chronic disease prevention and treatment. In Mediterranean Identities—Environment, Society, Culture; IntechOpen: London, UK, 2017; p. 401. [Google Scholar]
- Echeverría, G.; Dussaillant, C.; McGee, E.E.; Mena, C.; Nitsche, M.P.; Inés, U.; Bitran, M.; Pedrals, N.; Rigotti, A. Promoting and Implementing the Mediterranean Diet in the Southern Hemisphere: The Chilean Experience. Eur. J. Clin. Nutr. 2018, 72, 38–46. [Google Scholar] [CrossRef] [PubMed]
- Panico, S.; Mattiello, A.; Panico, C.; Chiodini, P. Mediterranean Dietary Pattern and Chronic Diseases. Cancer Treat. Res. 2013, 159, 69–81. [Google Scholar] [CrossRef]
- Harmon, B.; Boushey, C.J.; Shvetsov, Y.B.; Ettienne, R.; Reedy, J.; Wilkens, L.R.; Le Marchand, L.; Henderson, B.; Kolonel, L.N. Associations of key diet-quality indexes with mortality in the Multiethnic Cohort: The Dietary Patterns Methods Project. Am. J. Clin. Nutr. 2015, 101, 587–597. [Google Scholar] [CrossRef]
- Mantzioris, E.; Villani, A. Translation of a Mediterranean-Style Diet into the Australian Dietary Guidelines: A Nutritional, Ecological and Environmental Perspective. Nutrients 2019, 11, 2507. [Google Scholar] [CrossRef]
- Echeverria, G.; Urquiaga, I.; Concha, M.J.; Dussaillant, C.; Villarroel, L.; Velasco, N.; Leighton, F.; Rigotti, A. Validation of self-applicable questionnaire for a Mediterranean dietary index in Chile. Rev. Med. Chile 2016, 144, 1531–1543. [Google Scholar]
- Echeverría, G.; McGee, E.E.; Urquiaga, I.; Jiménez, P.; D’Acuña, S.; Villarroel, L.; Velasco, N.; Leighton, F.; Rigotti, A. Inverse Associations between a Locally Validated Mediterranean Diet Index, Overweight/Obesity, and Metabolic Syndrome in Chilean Adults. Nutrients 2017, 9, 862. [Google Scholar] [CrossRef]
- Garcia-Hermoso, A.; Vegas-Heredia, E.D.; Fernández-Vergara, O.; Ceballos-Ceballos, R.; Andrade-Schnettler, R.; Arellano-Ruiz, P.; Ramírez-Vélez, R. Independent and combined effects of handgrip strength and adherence to a Mediterranean diet on blood pressure in Chilean children. Nutrients 2019, 60, 170–174. [Google Scholar] [CrossRef]
- Delgado-Floody, P.; Alvarez, C.; Caamaño-Navarrete, F.; Jerez-Mayorga, D.; Latorre-Román, P. Influence of Mediterranean diet adherence, physical activity patterns, and weight status on cardiovascular response to cardiorespiratory fitness test in Chilean school children. Nutrients 2020, 71, 110621. [Google Scholar] [CrossRef]
- Lavados, P.M.; Mazzon, E.; Rojo, A.; Brunser, A.M.; Olavarría, V.V. Pre-stroke adherence to a Mediterranean diet pattern is associated with lower acute ischemic stroke severity: A cross-sectional analysis of a prospective hospital-register study. BMC Neurol. 2020, 20, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Urquiaga, I.; Strobel, P.; Perez, D.; Martinez, C.; Cuevas, A.; Castillo, O.; Marshall, G.; Rozowski, J.; Leighton, F. Mediterranean diet and red wine protect against oxidative damage in young volunteers. Atherosclerosis 2010, 211, 694–699. [Google Scholar] [CrossRef]
- Urquiaga, I.; Guasch, V.; Marshall, G.; San Martín, A.; Castillo, O.; Rozowski, J.; Leighton, F. Effect of Mediterranean and Occidental diets, and red wine, on plasma fatty acids in humans. An intervention study. Biol. Res. 2004, 37, 253–261. [Google Scholar] [CrossRef] [PubMed]
- Mezzano, D.; Leighton, F.; Strobel, P.; Martínez, C.; Marshall, G.; Cuevas, A.; Castillo, O.; Panes, O.; Muñoz, B.; Rozowski, J.; et al. Complementary effects of Mediterranean diet and moderate red wine intake on haemostatic cardiovascular risk factors. Eur. J. Clin. Nutr. 2001, 55, 444–451. [Google Scholar] [CrossRef]
- Leighton, F.; Cuevas, A.; Guasch, V.; Pérez, D.D.; Strobel, P.; Martín, A.S.; Urzua, U.; Díez, M.S.; Foncea, R.; Castillo, O.; et al. Plasma polyphenols and antioxidants, oxidative DNA damage and endothelial function in a diet and wine intervention study in humans. Drugs Under Exp. Clin. Res. 1999, 25, 133–141. [Google Scholar]
- Rodriguez, J.M. Reduction of serum advanced glycation end-products with a low calorie Mediterra-nean diet. Nutr. Hosp. 2015, 31, 2511–2517. [Google Scholar] [PubMed]
- Leighton, F.; Polic, G.; Strobel, P.; Perez, D.; Martinez, C.; Vásquez, L.; Castillo, O.; Villarroel, L.; Echeverría, G.; Inés, U.; et al. Health impact of Mediterranean diets in food at work. Public Health Nutr. 2009, 12, 1635–1643. [Google Scholar] [CrossRef]
- Willett, W.C.; Sacks, F.; Trichopoulou, A.; Drescher, G.; Ferro-Luzzi, A.; Helsing, E.; Trichopoulos, D. Mediterranean diet pyramid: A cultural model for healthy eating. Am. J. Clin. Nutr. 1995, 61 (Suppl. 6), 1402S–1406S. [Google Scholar] [CrossRef]
- Trichopoulou, A.; Lagiou, P. Healthy Traditional Mediterranean Diet: An Expression of Culture, History, and Lifestyle. Nutr. Rev. 2009, 55, 383–389. [Google Scholar] [CrossRef]
- Bach-Faig, A.; Berry, E.M.; Lairon, D.; Reguant, J.; Trichopoulou, A.; Dernini, S.; Medina, F.X.; Battino, M.; Belahsen, R.; Miranda, G.; et al. Mediterranean Diet Foundation Expert Group. Mediterranean diet pyramid today. Science and cultural updates. Public Health Nutr. 2011, 14, 2274–2284. [Google Scholar] [CrossRef]
- Lăcătușu, C.-M.; Grigorescu, E.-D.; Floria, M.; Onofriescu, A.; Mihai, B.-M. The Mediterranean Diet: From an Environment-Driven Food Culture to an Emerging Medical Prescription. Int. J. Environ. Res. Public Health 2019, 16, 942. [Google Scholar] [CrossRef] [PubMed]
- UNESCO. Mediterranean Diet: UNESCO Intangible Cultural Heritage. Available online: https://ich.unesco.org/es/RL/la-dieta-mediterranea-00884 (accessed on 8 July 2020).
- Psaltopoulou, T.; Sergentanis, T.N.; Panagiotakos, D.B.; Sergentanis, I.N.; Kosti, R.; Scarmeas, N. Mediterranean diet, stroke, cognitive impairment, and depression: A meta-analysis. Ann. Neurol. 2013, 74, 580–591. [Google Scholar] [CrossRef] [PubMed]
- Martínez-González, M.A.; Sánchez-Villegas, A. Food patterns and the prevention of depression. Proc. Nutr. Soc. 2016, 75, 139–146. [Google Scholar] [CrossRef] [PubMed]
- Molendijk, M.; Molero, P.; Sánchez-Pedreño, F.O.; van der Does, W.; Martínez-González, M.A. Diet quality and depression risk: A systematic review and dose-response meta-analysis of prospective studies. J. Affect. Disord. 2018, 226, 346–354. [Google Scholar] [CrossRef]
- Lassale, C.; Batty, G.D.; Akbaraly, T. Reply to Veronese and Smith: Healthy dietary indices and risk of depressive outcomes: A systematic review and meta-analysis of observational studies. Mol. Psychiatry 2019, 24, 1–2. [Google Scholar] [CrossRef]
- Shafiei, F.; Salari-Moghaddam, A.; Larijani, B.; Esmaillzadeh, A. Adherence to the Mediterranean diet and risk of depression: A systematic review and updated meta-analysis of observational studies. Nutr. Rev. 2019, 77, 230–239. [Google Scholar] [CrossRef]
- Sanchez-Villegas, D.A.; Martinez-Gonzalez, M.A.; Estruch, R.; Salas-Salvadó, J.; Corella, D.; Covas, M.-I.; Arós, F.; Romaguera, D.; Gómez-Gracia, E.; Lapetra, J.; et al. Mediterranean dietary pattern and depression: The predimed randomized trial. BMC Med. 2013, 11, 208. [Google Scholar] [CrossRef]
- Opie, R.S.; O’Neil, A.; Jacka, F.N.; Pizzinga, J.; Itsiopoulos, C. A modified Mediterranean dietary intervention for adults with major depression: Dietary protocol and feasibility data from the SMILES trial. Nutr. Neurosci. 2017, 21, 487–501. [Google Scholar] [CrossRef]
- Grosso, G.; Marventano, S.; D’Urso, M.; Mistretta, A.; Galvano, F. The Mediterranean healthy eating, ageing, and lifestyle (MEAL) study: Rationale and study design. Int. J. Food Sci. Nutr. 2016, 68, 577–586. [Google Scholar] [CrossRef]
- World Health Organization. Promoting Mental Health. Concepts. Emerging Evidence; World Health Organization: Geneva, Switzerland, 2005. [Google Scholar]
- Diener, E. Subjective well-being. Psychol. Bull. 1984, 95, 542–575. [Google Scholar] [CrossRef]
- Ryff, C.D. Happiness is everything, or is it? Explorations on the meaning of psychological well-being. J. Pers. Soc. Psychol. 1989, 57, 1069–1681. [Google Scholar] [CrossRef]
- Shapiro, A.; Keyes, C.L.M. Marital Status and Social Well-Being: Are the Married Always Better Off? Soc. Indic. Res. 2008, 88, 329–346. [Google Scholar] [CrossRef]
- Diener, E.; Lucas, R.E.; Oishi, S. Advances and Open Questions in the Science of Subjective Well-Being. Collabra Psychol. 2018, 4, 15. [Google Scholar] [CrossRef] [PubMed]
- Diener, E.; Oishi, S.; Tay, L. Advances in subjective well-being research. Nat. Hum. Behav. 2018, 2, 253–260. [Google Scholar] [CrossRef]
- Ryff, C.D. Know yourself and become who you are: A eudaimonic approach to well-being. J. Happiness Stud. 2008, 9, 13–39. [Google Scholar] [CrossRef]
- Ryff, C.D. Psychological Well-Being Revisited: Advances in the Science and Practice of Eudaimonia. Psychother. Psychosom. 2014, 83, 10–28. [Google Scholar] [CrossRef]
- Keyes, C.L.M. The Mental Health Continuum: From Languishing to Flourishing in Life. J. Health Soc. Behav. 2002, 43, 207–222. [Google Scholar] [CrossRef]
- Ryff, C.D.; Boylan, J.M.; Kirsch, J.A. Eudaimonic and Hedonic Well-Being: An Integrative Perspective with Linkages to Socio-demographic Factors and Health. In Measuring Well-being: Interdisciplinary Perspectives from the Social Sciences and the Humanities; Lee, M.T., Kubzansky, L.D., VanderWeele, T.J., Eds.; Oxford University Press: Oxford, UK, 2021. [Google Scholar]
- Radler, B.T.; Rigotti, A.; Ryff, C.D. Persistently high psychological well-being predicts better HDL cholesterol and triglyceride levels: Findings from the midlife in the U.S. (MIDUS) longitudinal study. Lipids Health Dis. 2018, 17, 1. [Google Scholar] [CrossRef]
- Ryff, C.D. The Benefits of Purposeful Life Engagement on Later-Life Physical Function. JAMA Psychiatry 2017, 74, 1046–1047. [Google Scholar] [CrossRef]
- Munoz, M.A. Regicor and hermes investigators. Adherence to the Mediterranean diet is associated with better mental and physical health. Br. J. Nutr. 2009, 101, 1182–1821. [Google Scholar] [CrossRef]
- Costarelli, V.; Koretsi, E.; Georgitsogianni, E. Health-related quality of life of Greek adolescents: The role of the Mediterranean diet. Qual. Life Res. 2013, 22, 951–956. [Google Scholar] [CrossRef] [PubMed]
- Grao-Cruces, A.; Nuviala, A.; Fernández-Martínez, A.; Porcel-Gálvez, A.M.; Moral-García, J.E.; Martínez-López, E.-J. Adherence to the Mediterranean diet in rural and urban adolescents of southern Spain, life satisfaction, anthropometry, and physical and sedentary activities. Nutr. Hosp. 2013, 28, 1129–1135. [Google Scholar] [PubMed]
- Bonaccio, M.; Di Castelnuovo, A.; Bonanni, A.; Costanzo, S.; de Lucia, F.; Pounis, G.; Zito, F.; Donati, M.B.; de Gaetano, G.; Iacoviello, L. Adherence to a Mediterranean diet is associated with a better health-related quality of life: A possible role of high dietary antioxidant content. BMJ Open 2013, 3, e003003. [Google Scholar] [CrossRef] [PubMed]
- Sánchez, P.H.; Ruano, C.; De Irala, J.; Ruiz-Canela, M.; Martínez-González, M.A.; Sánchez-Villegas, A. Adherence to the Mediterranean diet and quality of life in the SUN Project. Eur. J. Clin. Nutr. 2012, 66, 360–368. [Google Scholar] [CrossRef] [PubMed]
- Holt, M.E.; Lee, J.W.; Morton, K.R.; Tonstad, S. Mediterranean diet and emotion regulation. Mediterr. J. Nutr. Metab. 2014, 7, 163–172. [Google Scholar] [CrossRef]
- Galilea-Zabalza, I.; Buil-Cosiales, P.; Salas-Salvadó, J.; Toledo, E.; Ortega-Azorín, C.; Díez-Espino, J.; Vázquez-Ruiz, Z.; Zomeño, M.D.; Vioque, J.; Martínez, J.A.; et al. Mediterranean diet and quality of life: Baseline cross-sectional analysis of the predimed-plus trial. PLoS ONE 2018, 13, e0198974. [Google Scholar] [CrossRef]
- Bonaccio, M.; On Behalf of the MOLI-SANI Study Investigators; Di Castelnuovo, A.; Costanzo, S.; Pounis, G.; Persichillo, M.; Cerletti, C.; Donati, M.B.; De Gaetano, G.; Iacoviello, L. Mediterranean-type diet is associated with higher psychological resilience in a general adult population: Findings from the Moli-sani study. Eur. J. Clin. Nutr. 2017, 72, 154–160. [Google Scholar] [CrossRef]
- Veronese, N.; Stubbs, B.; Noale, M.; Solmi, M.; Luchini, C.; Maggi, S. Adherence to the Mediterranean diet is associated with better quality of life: Data from the Osteoarthritis Initiative. Am. J. Clin. Nutr. 2016, 104, 1403–1409. [Google Scholar] [CrossRef]
- Crichton, G.E.; Bryan, J.; Hodgson, J.M.; Murphy, K.J. Mediterranean diet adherence and self-reported psychological functioning in an Australian sample. Appetite 2013, 70, 53–59. [Google Scholar] [CrossRef]
- Perez-Tasigchana, R.F.; León-Muñoz, L.M.; López-García, E.; Banegas, J.R.; Rodríguez-Artalejo, F.; Guallar-Castillón, P. Mediterranean diet and health-related quality of life in two cohorts of community-dwelling older adults. PLoS ONE 2016, 11, e0151596. [Google Scholar]
- Muros, J.J.; Cofre-Bolados, C.; Arriscado, D.; Zurita, F.; Knox, E. Mediterranean diet adherence is associated with lifestyle, physical fitness, and mental wellness among 10-y-olds in Chile. Nutrition 2017, 35, 87–92. [Google Scholar] [CrossRef] [PubMed]
- López-Gil, J.F.; Oriol-Granado, X.; Izquierdo, M.; Ramírez-Vélez, R.; Fernández-Vergara, O.; Olloquequi, J.; García-Hermoso, A. Healthy Lifestyle Behaviors and Their Association with Self-Regulation in Chilean Children. Int. J. Environ. Res. Public Health 2020, 17, 5676. [Google Scholar] [CrossRef] [PubMed]
- Fava, G.A.; Ruini, C. Development and characteristics of a well-being enhancing psychotherapeutic strategy: Well-being therapy. J. Behav. Ther. Exp. Psychiatry 2003, 34, 45–63. [Google Scholar] [CrossRef]
- Ruini, C.; Fava, G.A. Well-being therapy for generalized anxiety disorder. J. Clin. Psychol. 2009, 65, 510–519. [Google Scholar] [CrossRef]
- Ruini, C.; Fava, G.A. Role of Well-Being Therapy in Achieving a Balanced and Individualized Path to Optimal Functioning. Clin. Psychol. Psychother. 2012, 19, 291–304. [Google Scholar] [CrossRef] [PubMed]
- Ruini, C.; Ryff, C.D. Using eudaimonic well-being to improve lives. In The Wiley Handbook of Positive Clinical Psychology; Wiley: Hoboken, NJ, USA, 2016; pp. 153–166. [Google Scholar]
- Friedman, E.M.; Ruini, C.; Foy, C.R.; Jaros, L.; Love, G.; Ryff, C.D. Lighten UP! A Community-Based Group Intervention to Promote Eudaimonic Well-Being in Older Adults: A Multi-Site Replication with 6 Month Follow-Up. Clin. Gerontol. 2019, 42, 387–397. [Google Scholar] [CrossRef] [PubMed]
- Sin, N. Enhancing well-being and alleviating depressive symptoms with positive psychology interventions: A practice-friendly meta-analysis. J. Clin. Psychol. 2009, 65, 467–487. [Google Scholar] [CrossRef]
- Bolier, L.; Haverman, M.; Westerhof, G.J.; Riper, H.; Smit, F.; Bohlmeijer, E. Positive psychology interventions: A meta-analysis of randomized controlled studies. BMC Public Health 2013, 13, 119. [Google Scholar] [CrossRef]
- Weiss, L.A.; Westerhof, G.J.; Bohlmeijer, E.T. Can We Increase Psychological Well-Being? The Effects of Interventions on Psychological Well-Being: A Meta-Analysis of Randomized Controlled Trials. PLoS ONE 2016, 11, e0158092. [Google Scholar] [CrossRef]
- Unützer, J.; Katon, W.J.; Fan, M.-Y.; Schoenbaum, M.C.; Lin, E.H.B.; Della Penna, R.D.; Powers, D. Long-term cost effects of collaborative care for late-life depression. Am. J. Manag. Care 2008, 14, 95–100. [Google Scholar]
- Mancuso, C.A.; Choi, T.N.; Westermann, H.; Wenderoth, S.; Hollenberg, J.P.; Wells, M.T.; Isen, A.; Jobe, J.B.; Allegrante, J.P.; Charlson, M.E. Increasing Physical Activity in Patients With Asthma Through Positive Affect and Self-affirmation. Arch. Intern. Med. 2012, 172, 337. [Google Scholar] [CrossRef] [PubMed]
- Ogedegbe, G.O. A randomized controlled trial of positive affect intervention and medication adher-ence in hypertensive African Americans. Arch. Intern. Med. 2012, 172, 322–326. [Google Scholar] [CrossRef] [PubMed]
- Peterson, J.C.; Charlson, M.E.; Hoffman, Z.; Wells, M.T.; Wong, S.-C.; Hollenberg, J.P.; Jobe, J.B.; Boschert, K.A.; Isen, A.M.; Allegrante, J.P. A Randomized Controlled Trial of Positive-Affect Induction to Promote Physical Activity After Percutaneous Coronary Intervention. Arch. Intern. Med. 2012, 172, 329–336. [Google Scholar] [CrossRef] [PubMed]
- Celano, C.M. Optimizing a Positive Psychology Intervention to Promote Health Behaviors After an Acute Coronary Syndrome: The Positive Emotions After Acute Coronary Events III (PEACE-III) Random-ized Factorial Trial. Psychosom. Med. 2018, 80, 526–534. [Google Scholar] [CrossRef] [PubMed]
- Massey, C.N.; Feig, E.H.; Duque, L.; Wexler, D.; Moskowitz, J.T.; Huffman, J.C. Well-being interventions for individuals with diabetes: A systematic review. Diabetes Res. Clin. Pract. 2019, 147, 118–133. [Google Scholar] [CrossRef] [PubMed]
- WHO. Sustainable Healthy Diets—Guiding Principles; FAO: Rome, Italy, 2019. [Google Scholar]
- Mbow, C. Food Security. In Special Report on Climate Change, Desertification, Land Degradation, Sustainable Land Management, Food Security, and Greenhouse Gas Fluxes in Terrestrial Ecosystems; IPCC: Ginevra, Switzerland, 2019. [Google Scholar]
- Fardet, A.; Rock, E. Ultra-Processed Foods and Food System Sustainability: What are the Links? Sustainability 2020, 12, 6280. [Google Scholar] [CrossRef]
- Nelson, M.; Hamm, M.W.; Hu, F.B.; Abrams, S.; Griffin, T.S. Alignment of Healthy Dietary Patterns and Environmental Sustainability: A Systematic Review. Adv. Nutr. 2016, 7, 1005–1025. [Google Scholar] [CrossRef]
- Grosso, G.; Fresán, U.; Bes-Rastrollo, M.; Marventano, S.; Galvano, F. Environmental Impact of Dietary Choices: Role of the Mediterranean and Other Dietary Patterns in an Italian Cohort. Int. J. Environ. Res. Public Health 2020, 17, 1468. [Google Scholar] [CrossRef]
- Rosi, A.; Biasini, B.; Donati, M.; Ricci, C.; Scazzina, F. Adherence to the Mediterranean Diet and Environmental Impact of the Diet on Primary School Children Living in Parma (Italy). Int. J. Environ. Res. Public Health 2020, 17, 6105. [Google Scholar] [CrossRef]
- Vanham, D.; Mekonnen, M.M.; Hoekstra, A.Y. Treenuts and groundnuts in the EAT-Lancet reference diet: Concerns regarding sustainable water use. Glob. Food Secur. 2020, 24, 100357. [Google Scholar] [CrossRef]
- González-García, S.; Esteve-Llorens, X.; Moreira, M.T.; Feijoo, G. Carbon footprint and nutritional quality of different human dietary choices. Sci. Total Environ. 2018, 644, 77–94. [Google Scholar] [CrossRef] [PubMed]
- Ruini, L.F.; Ciati, R.; Pratesi, C.A.; Marino, M.; Principato, L.; Vannuzzi, E. Working toward Healthy and Sustainable Diets: The Double Pyramid Model Developed by the Barilla Center for Food and Nutrition to Raise Awareness about the Environmental and Nutritional Impact of Foods. Front. Nutr. 2015, 2, 9. [Google Scholar] [CrossRef] [PubMed]
- Serra-Majem, L. The Mediterranean diet as an example of food and nutrition sustainability: A multi-disciplinary approach. Nutr. Hosp. 2018, 35, 96–101. [Google Scholar] [PubMed]
- Berry, E.M. Sustainable Food Systems and the Mediterranean Diet. Nutrients 2019, 11, 2229. [Google Scholar] [CrossRef] [PubMed]
- FAO; FIDA; OMS; PMA; UNICEF. Executive Summary of El Estado de la Seguridad Alimentaria y la Nutrición en el Mundo 2020. Transformación de los Sistemas Alimentarios para que Promuevan Dietas Asequibles y Saludables; FAO: Roma, Italy, 2020. [Google Scholar]
- Toti, E.; Di Mattia, C.; Serafini, M. Metabolic Food Waste and Ecological Impact of Obesity in FAO World’s Region. Front. Nutr. 2019, 6, 126. [Google Scholar] [CrossRef]
- Edwards, P.; Roberts, I. Population adiposity and climate change. Int. J. Epidemiol. 2009, 38, 1137–1140. [Google Scholar] [CrossRef]
- Rosi, A.; Mena, P.; Pellegrini, N.; Turroni, S.; Neviani, E.; Ferrocino, I.; Di Cagno, R.; Ruini, L.; Ciati, R.; Angelino, D.; et al. Environmental impact of omnivorous, ovo-lacto-vegetarian, and vegan diet. Sci. Rep. 2017, 7, 1–9. [Google Scholar] [CrossRef]
- Dernini, S.; Berry, E.; Serra-Majem, L.; La Vecchia, C.; Capone, R.; Medina, F.; Aranceta-Bartrina, J.; Belahsen, R.; Burlingame, B.; Calabrese, G.; et al. Med Diet 4.0: The Mediterranean diet with four sustainable benefits. Public Health Nutr. 2017, 20, 1322–1330. [Google Scholar] [CrossRef]
- Gastronomía y Marca País. Informe Final. Gerencia de Estudios Imagen Chile. 2016. Available online: https://slideplayer.es/slide/10231701/ (accessed on 20 July 2020).
- D’Innocenzo, S.; Biagi, C.; Lanari, M. Obesity and the Mediterranean Diet: A Review of Evidence of the Role and Sustainability of the Mediterranean Diet. Nutrients 2019, 11, 1306. [Google Scholar] [CrossRef] [PubMed]
- Drewnowski, A.; Monsivais, P. Taste, cost, convenience, and food choices. Present Knowl. Nutr. 2020, 2, 185–200. [Google Scholar] [CrossRef]
- Garnett, T.; Mathewson, S.; Angelides, P.; Borthwick, F. Policies and actions to shift eating patterns: What works? Foresight 2015, 515, 518–522. [Google Scholar]
- FAO; IFAD; UNICEF; WFP; WHO. The State of Food Security and Nutrition in the World 2019 Safeguarding Against Economic Slowdowns and Downturns; FAO: Rome, Italy, 2019. [Google Scholar]
- Saulle, R.; Semyonov, L.; la Torre, G. Cost and Cost-Effectiveness of the Mediterranean Diet: Results of a Systematic Review. Nutrients 2013, 5, 4566–4586. [Google Scholar] [CrossRef] [PubMed]
- Drewnowski, A.; Eichelsdoerfer, P. The Mediterranean diet: Does it have to cost more? Public Health Nutr. 2009, 12, 1621–1628. [Google Scholar] [CrossRef] [PubMed]
- Vlismas, K.; Panagiotakos, D.B.; Pitsavos, C.; Chrysohoou, C.; Skoumas, Y.; Sitara, M.; Yfantopoulos, J.N.; Stavrinos, V.; Stefanadis, C. Quality, but not cost, of diet is associated with 5-year incidence of CVD: The ATTICA study. Public Health Nutr. 2010, 13, 1890–1897. [Google Scholar] [CrossRef]
- Lopez, C.N. Costs of Mediterranean and western dietary patterns in a Spanish cohort and their relationship with prospective weight change. J. Epidemiol. Community Health 2009, 63, 920–927. [Google Scholar] [CrossRef]
- Schröder, H.; Marrugat, J.; Covas, M. High monetary costs of dietary patterns associated with lower body mass index: A population-based study. Int. J. Obes. 2006, 30, 1574–1579. [Google Scholar] [CrossRef]
- Goulet, J.; Lamarche, B.; Lemieux, S. A Nutritional Intervention Promoting a Mediterranean Food Pattern Does Not Affect Total Daily Dietary Cost in North American Women in Free-Living Conditions. J. Nutr. 2008, 138, 54–59. [Google Scholar] [CrossRef]
- OECD. The Heavy Burden of Obesity and the Economics of Prevention; Organisation for Economic Co-Operation and Development (OECD): Paris, France, 2019; p. 13. [Google Scholar]
- Dalziel, K.M.; Segal, L.; De Lorgeril, M. A Mediterranean Diet Is Cost-Effective in Patients with Previous Myocardial Infarction. J. Nutr. 2006, 136, 1879–1885. [Google Scholar] [CrossRef]
- Dalziel, K.M.; Segal, L. Time to give nutrition interventions a higher profile: Cost-effectiveness of 10 nutrition interventions. Health Promot. Int. 2007, 22, 271–283. [Google Scholar] [CrossRef]
- Panagiotakos, D. Estimating the 10-year risk of cardiovascular disease and its economic consequences, by the level of adherence to the Mediterranean diet: The ATTICA study. J. Med. Food 2007, 10, 239–243. [Google Scholar] [CrossRef]
- Catastro Nacional de Ferias Libres. 2016. Available online: https://www.catastroferiaslibres.cl/doc/catastro_ferias.pdf (accessed on 23 July 2020).
- Vilarnau, C.; Stracker, D.M.; Funtikov, A.; da Silva, R.; Estruch, R.; Bach-Faig, A. Worldwide adherence to Mediterranean Diet between 1960 and 2011. Eur. J. Clin. Nutr. 2018, 72, 83–91. [Google Scholar] [CrossRef] [PubMed]
- Belahsen, R.; Rguibi, M. Population health and Mediterranean diet in southern Mediterranean countries. Public Health Nutr. 2006, 9, 1130–1135. [Google Scholar] [CrossRef] [PubMed]
- Willett, W.; Rockström, J.; Loken, B.; Springmann, M.; Lang, T.; Vermeulen, S.; Garnett, T.; Tilman, D.; Declerck, F.; Wood, A.; et al. Food in the Anthropocene: The EAT–Lancet Commission on healthy diets from sustainable food systems. Lancet 2019, 393, 447–492. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Echeverría, G.; Tiboni, O.; Berkowitz, L.; Pinto, V.; Samith, B.; von Schultzendorff, A.; Pedrals, N.; Bitran, M.; Ruini, C.; Ryff, C.D.; et al. Mediterranean Lifestyle to Promote Physical, Mental, and Environmental Health: The Case of Chile. Int. J. Environ. Res. Public Health 2020, 17, 8482. https://doi.org/10.3390/ijerph17228482
Echeverría G, Tiboni O, Berkowitz L, Pinto V, Samith B, von Schultzendorff A, Pedrals N, Bitran M, Ruini C, Ryff CD, et al. Mediterranean Lifestyle to Promote Physical, Mental, and Environmental Health: The Case of Chile. International Journal of Environmental Research and Public Health. 2020; 17(22):8482. https://doi.org/10.3390/ijerph17228482
Chicago/Turabian StyleEcheverría, Guadalupe, Ornella Tiboni, Loni Berkowitz, Victoria Pinto, Bárbara Samith, Andrea von Schultzendorff, Nuria Pedrals, Marcela Bitran, Chiara Ruini, Carol D. Ryff, and et al. 2020. "Mediterranean Lifestyle to Promote Physical, Mental, and Environmental Health: The Case of Chile" International Journal of Environmental Research and Public Health 17, no. 22: 8482. https://doi.org/10.3390/ijerph17228482
APA StyleEcheverría, G., Tiboni, O., Berkowitz, L., Pinto, V., Samith, B., von Schultzendorff, A., Pedrals, N., Bitran, M., Ruini, C., Ryff, C. D., Del Rio, D., & Rigotti, A. (2020). Mediterranean Lifestyle to Promote Physical, Mental, and Environmental Health: The Case of Chile. International Journal of Environmental Research and Public Health, 17(22), 8482. https://doi.org/10.3390/ijerph17228482






