Exploring the Impact of COVID-19 on Mental Health Outcomes in Children and Adolescents: A Systematic Review
Abstract
1. Introduction
1.1. Psychosocial Consequences
1.2. Effect of COVID-19 on Children and Adolescents
1.3. The Present Study
- To identify mental health outcomes in children and adolescents during the COVID-19 pandemic.
- To identify correlates, either positive or negative, associated with mental health outcomes in children and adolescents during the COVID-19 pandemic.
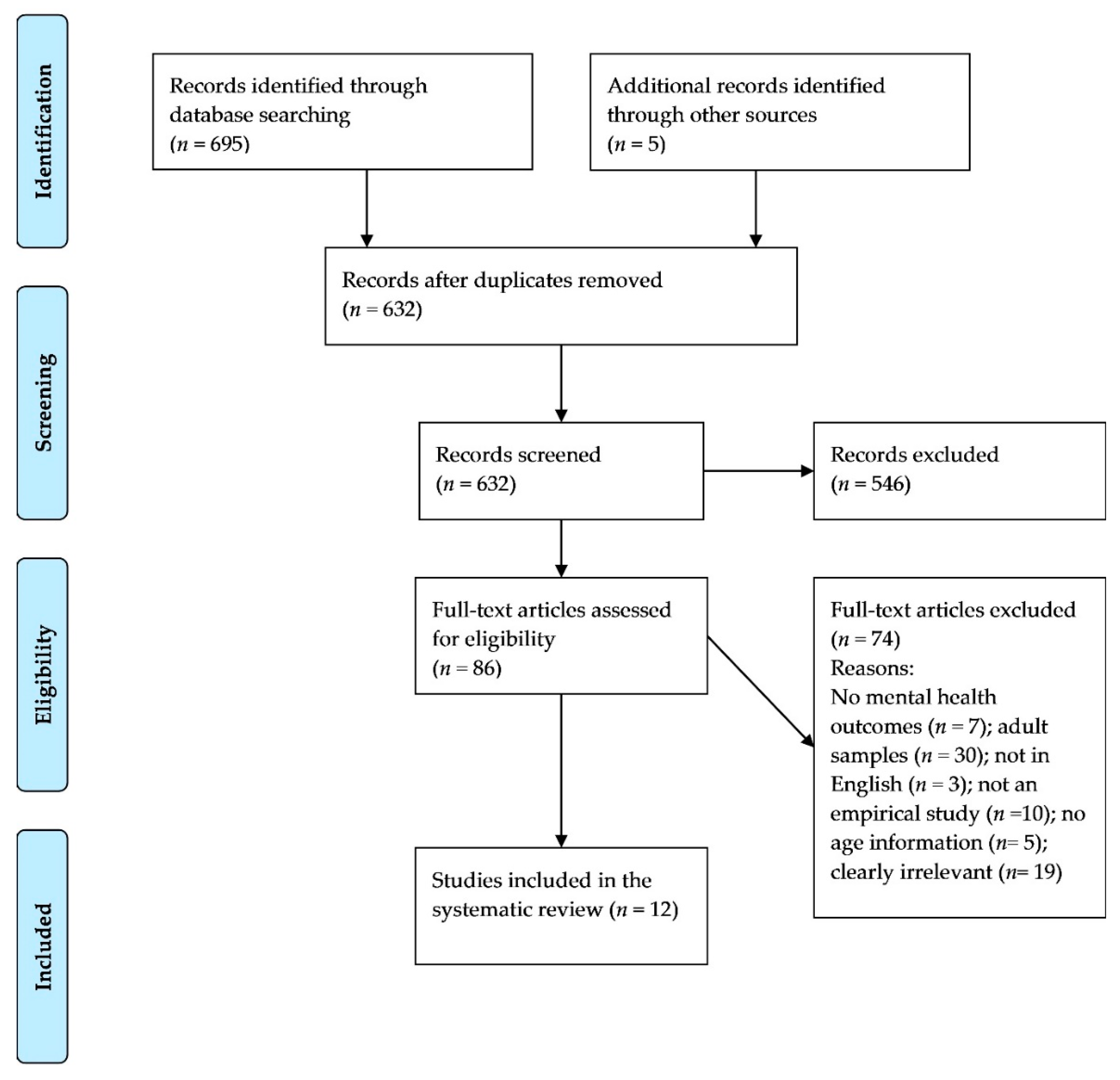
2. Methods
2.1. Design
2.2. Search Strategy
2.3. Screening and Data Extraction
2.4. Quality Assessment
2.5. Data Synthesis
3. Results
3.1. Methodological Characteristics of the Studies
3.2. Mental Health Outcomes
3.2.1. Depression
3.2.2. Anxiety
3.2.3. COVID-19 Emotional Reactions and Mental Health Outcomes
3.2.4. Psychological Distress and Somatic Symptoms
3.3. Positive Domains
3.4. Age Differences
3.5. Gender Differences
4. Discussion
4.1. Impact of COVID-19 on Youth Mental Health
4.2. Age and Gender Differences
4.3. Strengths and Limitations
4.4. Recommendations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- World Health Organization (WHO). Coronavirus Disease (COVID-19); WHO: Geneva, Switzerland, 2020. [Google Scholar]
- Petrosillo, N.; Viceconte, G.; Ergonul, O.; Ippolito, G.; Petersen, E. COVID-19, SARS and MERS: Are they closely related? Clin. Microbiol. Infect. 2020, 26, 729–734. [Google Scholar] [CrossRef] [PubMed]
- Cheng, S.K.W.; Tsang, J.S.K.; Ku, K.H.; Wong, C.W.; Ng, Y.K. Psychiatric complications in patients with severe acute respiratory syndrome (SARS) during the acute treatment phase: A series of 10 cases. Br. J. Psychiatry 2004, 184, 359–360. [Google Scholar] [CrossRef]
- Chua, S.E.; Cheung, V.; McAlonan, G.M.; Cheung, C.; Wong, J.W.S.; Cheung, E.P.T.; Chan, M.T.Y.; Wong, T.K.W.; Choy, K.M.; Chu, C.M.; et al. Stress and psychological impact on SARS patients during the outbreak. Can. J. Psychiatry 2004, 49, 385–390. [Google Scholar] [CrossRef] [PubMed]
- Cheng, S.K.W.; Wong, C.W. Psychological intervention with sufferers from severe acute respiratory syndrome (SARS): Lessons learnt from empirical findings. Clin. Psychol. Psychother. 2005, 12, 80–86. [Google Scholar] [CrossRef]
- Wu, K.K.; Chan, S.K.; Ma, T.M. Posttraumatic stress, anxiety, and depression in survivors of severe acute respiratory syndrome (SARS). J. Trauma Stress 2005, 18, 39–42. [Google Scholar] [CrossRef] [PubMed]
- Mak, I.W.C.; Chu, C.M.; Pan, P.C.; Yiu, M.G.C.; Chan, V.L. Long-term psychiatric morbidities among SARS survivors. Gen. Hosp. Psychiatry 2009, 31, 318–326. [Google Scholar] [CrossRef]
- Maunder, R.; Hunter, J.; Vincent, L.; Bennett, J.; Peladeau, N.; Leszcz, M.; Sadavoy, J.; Verhaeghe, L.M.; Steinberg, R.; Mazzulli, T. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. CMAJ 2003, 168, 1245–1251. [Google Scholar]
- Robertson, E.; Hershenfield, K.; Grace, S.L.; Stewart, D.E. The psychosocial effects of being quarantined following exposure to SARS: A qualitative study of Toronto health care workers. Can. J. Psychiatry 2004, 49, 403–407. [Google Scholar] [CrossRef]
- Koller, D.F.; Nicholas, D.B.; Goldie, R.S.; Gearing, R.; Selkirk, E.K. Bowlby and Robertson revisited: The Impact of isolation on hospitalized children during SARS. J. Dev. Behav. Pediatr. 2006, 27, 134–140. [Google Scholar] [CrossRef]
- Sprang, G.; Silman, M. Posttraumatic stress disorder in parents and youth after health-related disasters. Disaster Med. Public Health Prep. 2013, 7, 105–110. [Google Scholar] [CrossRef]
- Viner, R.M.; Russell, S.J.; Croker, H.; Packer, J.; Ward, J.; Stansfield, C.; Mytton, O.; Bonell, C.; Booy, R. School closure and management practices during coronavirus outbreaks including COVID-19: A rapid systematic review. Lancet Child. Adolesc. Health 2020, 4, 397–404. [Google Scholar] [CrossRef]
- Wang, G.; Zhang, Y.; Zhao, J.; Zhang, J.; Jiang, F. Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet 2020, 395, 945–947. [Google Scholar] [CrossRef]
- Ghosh, R.; Dubey, M.J.; Chatterjee, S.; Dubey, S. Impact of COVID-19 on children: Special focus on the psychosocial aspect. Minerva Pediatr. 2020, 72, 226–235. [Google Scholar] [CrossRef]
- Mackler, J.S.; Kelleher, R.T.; Shanahan, L.; Calkins, S.D.; Keane, S.P.; O’Brien, M. Parenting Stress, Parental Reactions, and Externalizing Behavior from Ages 4 to 10. J. Marriage Fam. 2015, 77, 388–406. [Google Scholar] [CrossRef]
- Sanner, C.M.; Neece, C.L. Parental Distress and Child Behavior Problems: Parenting Behaviors as Mediators. J. Child. Fam. Stud. 2018, 27, 591–601. [Google Scholar] [CrossRef]
- Ellis, W.E.; Dumas, T.M.; Forbes, L.M. Physically isolated but socially connected: Psychological adjustment and stress among adolescents during the initial COVID-19 crisis. Can. J. Behav. Sci. 2020, 52, 177–187. [Google Scholar] [CrossRef]
- Thomas, E. Coronavirus: Impact on Young People with Mental Health Needs; Young Minds: London, UK, 2020. [Google Scholar]
- Brazendale, K.; Beets, M.W.; Weaver, R.G.; Pate, R.R.; Turner-McGrievy, G.M.; Kaczynski, A.T.; Chandler, J.L.; Bohnert, A.; von Hippel, P.T. Understanding differences between summer vs. school obesogenic behaviors of children: The structured days hypothesis. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 100. [Google Scholar] [CrossRef]
- Crawley, E.; Loades, M.; Feder, G.; Logan, S.; Redwood, S.; Macleod, J. Wider collateral damage to children in the UK because of the social distancing measures designed to reduce the impact of COVID-19 in adults. BMJ Paediatr. Open 2020, 4, e000701. [Google Scholar] [CrossRef]
- Caspi, A.; Harrington, H.L.; Moffitt, T.E.; Milne, B.J.; Poulton, R. Socially isolated children 20 years later: Risk of cardiovascular disease. Arch. Pediatr. Adolesc. Med. 2006, 160, 805–811. [Google Scholar] [CrossRef]
- Matthews, T.; Danese, A.; Wertz, J.; Odgers, C.L.; Ambler, A.; Moffitt, T.E.; Arseneault, L. Social isolation, loneliness and depression in young adulthood: A behavioural genetic analysis. Soc. Psychiatry Psychiatr. Epidemiol. 2016, 51, 339–348. [Google Scholar] [CrossRef]
- Loades, M.E.; Chatburn, E.; Higson-Sweeney, N.; Reynolds, S.; Shafran, R.; Brigden, A.; Linney, C.; McManus, M.N.; Borwick, C.; Crawley, E. Rapid Systematic Review: The Impact of Social Isolation and Loneliness on the Mental Health of Children and Adolescents in the Context of COVID-19. J. Am. Acad. Child. Adolesc. Psychiatry 2020, 59, 1218–1239. [Google Scholar] [CrossRef] [PubMed]
- Bonanno, G.A.; Ho, S.M.Y.; Chan, J.C.K.; Kwong, R.S.Y.; Cheung, C.K.Y.; Wong, C.P.Y.; Wong, V.C.W. Psychological Resilience and Dysfunction Among Hospitalized Survivors of the SARS Epidemic in Hong Kong: A Latent Class Approach. Health Psychol. 2008, 27, 659–667. [Google Scholar] [CrossRef]
- Lee, S.M.; Kang, W.S.; Cho, A.R.; Kim, T.; Park, J.K. Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Compr. Psychiatry 2018, 87, 123–127. [Google Scholar] [CrossRef] [PubMed]
- Lung, F.W.; Lu, Y.C.; Chang, Y.Y.; Shu, B.C. Mental symptoms in different health professionals during the SARS attack: A Follow-up study. Psychiatr. Q. 2009, 80, 107–116. [Google Scholar] [CrossRef] [PubMed]
- Wu, P.; Fang, Y.; Guan, Z.; Fan, B.; Kong, J.; Yao, Z.; Liu, X.; Fuller, C.J.; Susser, E.; Lu, J.; et al. The psychological impact of the SARS epidemic on hospital employees in China: Exposure, risk perception, and altruistic acceptance of risk. Can. J. Psychiatry 2009, 54, 302–311. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Altman, D.; Antes, G.; Atkins, D.; Barbour, V.; Barrowman, N.; Berlin, J.A.; et al. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Veritas Health Innovation Covidence Systematic Review Software; Veritas Health Innovation: Melbourne, Australia, 2020; Available online: www.covidence.org (accessed on 21 June 2020).
- JBI Critical Appraisal Tools. Joanna Briggs Institute. Available online: https://joannabriggs.org/critical-appraisal-tools (accessed on 15 July 2020).
- Hong, Q.N.; Fàbregues, S.; Bartlett, G.; Boardman, F.; Cargo, M.; Dagenais, P.; Gagnon, M.P.; Griffiths, F.; Nicolau, B.; O’Cathain, A.; et al. The Mixed Methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers. Educ. Inf. 2018, 34, 285–291. [Google Scholar] [CrossRef]
- Rodgers, M.; Sowden, A.; Petticrew, M.; Arai, L.; Roberts, H.; Britten, N.; Popay, J. Testing Methodological Guidance on the Conduct of Narrative Synthesis in Systematic Reviews. Evaluation 2009, 15, 49–73. [Google Scholar] [CrossRef]
- Seçer, İ.; Ulaş, S. An Investigation of the Effect of COVID-19 on OCD in Youth in the Context of Emotional Reactivity, Experiential Avoidance, Depression and Anxiety. Int. J. Ment. Health Addict. 2020. [Google Scholar] [CrossRef]
- Colizzi, M.; Sironi, E.; Antonini, F.; Ciceri, M.L.; Bovo, C.; Zoccante, L. Psychosocial and behavioral impact of COVID-19 in autism spectrum disorder: An online parent survey. Brain Sci. 2020, 10, 341. [Google Scholar] [CrossRef]
- Liu, S.; Liu, Y.; Liu, Y. Somatic symptoms and concern regarding COVID-19 among Chinese college and primary school students: A cross-sectional survey. Psychiatry Res. 2020, 289, 113070. [Google Scholar] [CrossRef] [PubMed]
- Zhou, S.J.; Zhang, L.G.; Wang, L.L.; Guo, Z.C.; Wang, J.Q.; Chen, J.C.; Liu, M.; Chen, X.; Chen, J.X. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur. Child. Adolesc. Psychiatry 2020, 29, 749–758. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Luo, W.T.; Li, Y.; Li, C.N.; Hong, Z.S.; Chen, H.L.; Xiao, F.; Xia, J.Y. Psychological status and behavior changes of the public during the COVID-19 epidemic in China. Infect. Dis. Poverty 2020, 9, 58. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.; Bin, P.; He, A.J. Opinions from the epicenter: An online survey of university students in Wuhan amidst the COVID-19 outbreak11. J. Chin. Gov. 2020, 5, 234–248. [Google Scholar] [CrossRef]
- Xie, X.; Xue, Q.; Zhou, Y.; Zhu, K.; Liu, Q.; Zhang, J.; Song, R. Mental Health Status among Children in Home Confinement during the Coronavirus Disease 2019 Outbreak in Hubei Province, China. JAMA Pediatr. 2020, 174, 898–900. [Google Scholar] [CrossRef]
- Casanova, M.; Pagani Bagliacca, E.; Silva, M.; Patriarca, C.; Veneroni, L.; Clerici, C.A.; Spreafico, F.; Luksch, R.; Terenziani, M.; Meazza, C.; et al. How young patients with cancer perceive the COVID-19 (coronavirus) epidemic in Milan, Italy: Is there room for other fears? Pediatr. Blood Cancer 2020, 67, e28318. [Google Scholar] [CrossRef]
- Jiao, W.Y.; Wang, L.N.; Liu, J.; Fang, S.F.; Jiao, F.Y.; Pettoello-Mantovani, M.; Somekh, E. Behavioral and Emotional Disorders in Children during the COVID-19 Epidemic. J. Pediatr. 2020, 221, 264–266. [Google Scholar] [CrossRef]
- Oosterhoff, B.; Palmer, C.A.; Wilson, J.; Shook, N. Adolescents’ motivations to engage in social distancing during the COVID-19 pandemic: Associations with mental and social health. J. Adolesc. Health 2020, 67, 179–185. [Google Scholar] [CrossRef]
- Trzebiński, J.; Cabański, M.; Czarnecka, J.Z. Reaction to the COVID-19 Pandemic: The Influence of Meaning in Life, Life Satisfaction, and Assumptions on World Orderliness and Positivity. J. Loss Trauma. 2020, 25, 544–557. [Google Scholar] [CrossRef]
- Tian, F.; Li, H.; Tian, S.; Yang, J.; Shao, J.; Tian, C. Psychological symptoms of ordinary Chinese citizens based on SCL-90 during the level I emergency response to COVID-19. Psychiatry Res. 2020, 288, 112992. [Google Scholar] [CrossRef]
- Tang, X.; Tang, S.; Ren, Z.; Wong, D.F.K. Prevalence of depressive symptoms among adolescents in secondary school in mainland China: A systematic review and meta-analysis. J. Affect. Disord. 2019, 245, 498–507. [Google Scholar] [CrossRef] [PubMed]
- Magiati, I.; Ponniah, K.; Ooi, Y.P.; Chan, Y.H.; Fung, D.; Woo, B. Self-reported depression and anxiety symptoms in school-aged Singaporean children. Asia-Pac. Psychiatry 2015, 7, 91–104. [Google Scholar] [CrossRef] [PubMed]
- Campo, J.V.; Fritsch, S.L. Somatization in Children and Adolescents. J. Am. Acad. Child. Adolesc. Psychiatry 1994, 33, 1223–1235. [Google Scholar] [CrossRef] [PubMed]
- Cerutti, R.; Spensieri, V.; Valastro, C.; Presaghi, F.; Canitano, R.; Guidetti, V. A comprehensive approach to understand somatic symptoms and their impact on emotional and psychosocial functioning in children. PLoS ONE 2017, 12, e0171867. [Google Scholar] [CrossRef] [PubMed]
- Duan, H.; Yan, L.; Ding, X.; Gan, Y.; Kohn, N.; Wu, J. Impact of the COVID-19 pandemic on mental health in the general Chinese population: Changes, predictors and psychosocial correlates. Psychiatry Res. 2020, 293, 113396. [Google Scholar] [CrossRef]
- Burhamah, W.; AlKhayyat, A.; Oroszlányová, M.; AlKenane, A.; Almansouri, A.; Behbehani, M.; Karimi, N.; Jafar, H.; AlSuwaidan, M. The psychological burden of the COVID-19 pandemic and associated lockdown measures: Experience from 4000 participants. J. Affect. Disord. 2020, 277, 977–985. [Google Scholar] [CrossRef]
- Kessler, R.C.; Berglund, P.; Demler, O.; Jin, R.; Merikangas, K.R.; Walters, E.E. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Arch. Gen. Psychiatry 2005, 62, 593–602. [Google Scholar] [CrossRef]
- Paus, T.; Keshavan, M.; Giedd, J.N. Why do many psychiatric disorders emerge during adolescence? Nat. Rev. Neurosci. 2008, 9, 947–957. [Google Scholar] [CrossRef]
- Chen, S.; Jones, P.B.; Underwood, B.R.; Moore, A.; Bullmore, E.T.; Banerjee, S.; Osimo, E.F.; Deakin, J.B.; Hatfield, C.F.; Thompson, F.J.; et al. The early impact of COVID-19 on mental health and community physical health services and their patients’ mortality in Cambridgeshire and Peterborough, UK. J. Psychiatr. Res. 2020, 131, 244–254. [Google Scholar] [CrossRef]
- Aragona, M.; Barbato, A.; Cavani, A.; Costanzo, G.; Mirisola, C. Negative impacts of COVID-19 lockdown on mental health service access and follow-up adherence for immigrants and individuals in socio-economic difficulties. Public Health 2020, 186, 52–56. [Google Scholar] [CrossRef] [PubMed]
- Nearchou, F. Resilience following emotional abuse by teachers: Insights from a cross-sectional study with Greek students. Child. Abus. Negl. 2018, 78, 96–106. [Google Scholar] [CrossRef] [PubMed]
- Oberle, E.; Ji, X.R.; Kerai, S.; Guhn, M.; Schonert-Reichl, K.A.; Gadermann, A.M. Screen time and extracurricular activities as risk and protective factors for mental health in adolescence: A population-level study. Prev. Med. 2020, 141, 106291. [Google Scholar] [CrossRef] [PubMed]
- Moksnes, U.K.; Espnes, G.A.; Haugan, G. Stress, sense of coherence and emotional symptoms in adolescents. Psychol. Health 2014, 29, 32–49. [Google Scholar] [CrossRef] [PubMed]
- Lin, W.H.; Yi, C.C. The Effect of Family Cohesion and Life Satisfaction During Adolescence on Later Adolescent Outcomes: A Prospective Study. Youth Soc. 2019, 51, 680–706. [Google Scholar] [CrossRef]
- Bosqui, T.J.; Marshoud, B. Mechanisms of change for interventions aimed at improving the wellbeing, mental health and resilience of children and adolescents affected by war and armed conflict: A systematic review of reviews. Confl. Health 2018, 12, 15. [Google Scholar] [CrossRef]
- de Rojas, T.; Pérez-Martínez, A.; Cela, E.; Baragaño, M.; Galán, V.; Mata, C.; Peretó, A.; Madero, L. COVID-19 infection in children and adolescents with cancer in Madrid. Pediatr. Blood Cancer 2020, 67, e28397. [Google Scholar] [CrossRef]
- Hrusak, O.; Kalina, T.; Wolf, J.; Balduzzi, A.; Provenzi, M.; Rizzari, C.; Rives, S.; del Pozo Carlavilla, M.; Alonso, M.E.V.; Domínguez-Pinilla, N.; et al. Flash survey on severe acute respiratory syndrome coronavirus-2 infections in paediatric patients on anticancer treatment. Eur. J. Cancer 2020, 132, 11–16. [Google Scholar] [CrossRef]
- Verbruggen, L.C.; Wang, Y.; Armenian, S.H.; Ehrhardt, M.J.; van der Pal, H.J.H.; van Dalen, E.C.; van As, J.W.; Bardi, E.; Baust, K.; Berger, C.; et al. Guidance regarding COVID-19 for survivors of childhood, adolescent, and young adult cancer: A statement from the International Late Effects of Childhood Cancer Guideline Harmonization Group. Pediatr. Blood Cancer 2020, 67, e28702. [Google Scholar] [CrossRef]
- Neece, C.; McIntyre, L.L.; Fenning, R. Examining the impact of COVID-19 in ethnically diverse families with young children with intellectual and developmental disabilities. J. Intellect. Disabil. Res. 2020, 64, 739–749. [Google Scholar] [CrossRef]
- Narzisi, A.; Muratori, F.; Calderoni, S.; Fabbro, F.; Urgesi, C. Neuropsychological profile in high functioning autism spectrum disorders. J. Autism Dev. Disord. 2013, 43, 1895–1909. [Google Scholar] [CrossRef]
- Hankin, B.L.; Abramson, L.Y.; Moffitt, T.E.; Angell, K.E.; Silva, P.A.; McGee, R. Development of depression from preadolescence to young adulthood: Emerging gender differences in a 10-year longitudinal study. J. Abnorm. Psychol. 1998, 107, 128–140. [Google Scholar] [CrossRef] [PubMed]
- Hankin, B.L.; Young, J.F.; Abela, J.R.Z.; Smolen, A.; Jenness, J.L.; Gulley, L.D.; Technow, J.R.; Gottlieb, A.B.; Cohen, J.R.; Oppenheimer, C.W. Depression from childhood into late adolescence: Influence of gender, development, genetic susceptibility, and peer stress. J. Abnorm. Psychol. 2015, 124, 803–816. [Google Scholar] [CrossRef] [PubMed]
- Boniel-Nissim, M.; Lenzi, M.; Zsiros, E.; De Matos, M.G.; Gommans, R.; Harel-Fisch, Y.; Djalovski, A.; Van Der Sluijs, W. International trends in electronic media communication among 11- to 15-year-olds in 30 countries from 2002 to 2010: Association with ease of communication with friends of the opposite sex. Eur. J. Public Health 2015, 25, 41–45. [Google Scholar] [CrossRef] [PubMed]
- Gao, J.; Zheng, P.; Jia, Y.; Chen, H.; Mao, Y.; Chen, S.; Wang, Y.; Fu, H.; Dai, J. Mental health problems and social media exposure during COVID-19 outbreak. PLoS ONE 2020, 15, e0231924. [Google Scholar] [CrossRef]
- Frey, M.; Obermeier, V.; von Kries, R.; Schulte-Körne, G. Age and sex specific incidence for depression from early childhood to adolescence: A 13-year longitudinal analysis of German health insurance data. J. Psychiatr. Res. 2020, 129, 17–23. [Google Scholar] [CrossRef]
- Galvao, T.F.; Silva, M.T.; Zimmermann, I.R.; Souza, K.M.; Martins, S.S.; Pereira, M.G. Pubertal timing in girls and depression: A systematic review. J. Affect. Disord. 2014, 155, 13–19. [Google Scholar] [CrossRef]
- Avenevoli, S.; Swendsen, J.; He, J.P.; Burstein, M.; Merikangas, K.R. Major Depression in the National Comorbidity Survey–Adolescent Supplement: Prevalence, Correlates, and Treatment. J. Am. Acad. Child. Adolesc. Psychiatry 2015, 54, 37–44. [Google Scholar] [CrossRef] [PubMed]
- Merikangas, K.R.; He, J.P.; Burstein, M.; Swanson, S.A.; Avenevoli, S.; Cui, L.; Benjet, C.; Georgiades, K.; Swendsen, J. Lifetime prevalence of mental disorders in U.S. adolescents: Results from the national comorbidity survey replication-adolescent supplement (NCS-A). J. Am. Acad. Child. Adolesc. Psychiatry 2010, 49, 980–989. [Google Scholar] [CrossRef]
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Quantitative, qualitative, mixed methods studies Human studies Peer-reviewed papers Mental disorders Neurodevelopmental disorders/any other disorder Any mental health outcome COVID-19 related research | Not in English Studies [that only included] of adults 18 years old or older Studies that did not report age |
| Authors | Country | Date of Data Collection | Sample Characteristics | Sampling Strategy/Data Collection Method | Measures | Analytical Approach | Mental Health Outcomes and Correlates | Quality Appraisal |
|---|---|---|---|---|---|---|---|---|
| Casanova et al., 2020 [40] | Italy | 2–7 March 2020 | Pediatric oncology patients adolescents and young adults, n = 26 < 18 years (14 males) receiving treatment n = 10 follow up after completed treatment | Directly contacted participants recruited for other projects, data collected by email | Questionnaire including items developed by authors, no reliability other information reported | Descriptives | Fear of contracting COVID-19 and of implications; worry about family; relationships with peers; anger and fear about changing daily habits | Low |
| Colizzi et al., 2020 [34] | Italy | 6–20 April 2020 | n = 527 children diagnosed with autism spectrum disorders mean age = 13 year, SD = 8.1, no age range reported, no information on gender | Convenience sampling online parent survey distributed by healthcare professionals, autism advocacy and family support networks | Self-reported diagnosis of ASD; 40-item questionnaire developed for study purposes using focus groups (no reliability reported for the present sample) | Descriptives; Logistic Regressions | Well-being measured via frequency and intensity of behavioural problems | Medium |
| Jiao et al., 2020 [41] | China | Second week of February 2020 | n = 320 children and adolescents aged 3–18 years old (168 females), no other information reported | Parent survey, no other information | Questionnaire incorporated DSM- 5 criteria; no reliability or other information reported | Descriptives; Age group differences examined no information reported on statistical tests used | Poor sleep; nightmares; poor appetite; physical discomfort and agitation; inattention; clinginess; worry; irritability; fear of the health of relatives; obsessive request for updates; sleeping disorders | Low |
| Liu, Liu et al., 2020 [36] | China | February and March, 2020 | n = 209 primary school students (5th and 6th grade; 116 females) no other age information | Cluster sampling (unclear whether how data collection was conducted) | SSS; (no reliability reported for the present sample) | Descriptives, T-tests, Kruskal–Wallis test; Spearman rank correlations; logistic regressions | Concerns regarding COVID-19; somatic symptoms; depression; anxiety | Medium |
| Liu, Luo et al., 2020 [37] | China | 30 January to 3 February 2020 | n = 608 adults, n = 34 < 18 years old, no information on age range and gender | Snowball sampling, online via social media platforms | SDS; SCL-90 (reliability not reported for the present sample) single item measuring COVID-19 worry | Descriptives; T-tests; ANOVAs; chi-square | Worry about contracting COVID-19 depression; ‘Psychological abnormalities’ | Medium |
| Oosterhoff et al., 2020 [42] | United States | 28–29 March 2020 | n = 683 adolescents, mean age = 16.35, SD = 1.13, range 13–18 years, 75.3% females | No information on sampling strategy, online via social media platforms, | PROMIS anxiety scale; PROMIS depression scale; INQ burdensomeness; INQ Belongingness (reliability not reported for all measures for the present sample) | Descriptives; correlations regressions | Anxiety; depression; burdensomeness; belongingness | Medium |
| Seçer et al., 2020 [33] | Turkey | Data collected during 15 days, no other information reported | n = 568 adolescents, mean age = 16.4, SD = 2.14, age range 14–18 years (61.1% males) | Convenience sampling online via the provincial education directorate using social media apps and emails | OCI- Child Version; ERS; DAS-CV; Fear of COVID-19 Scale; | Confirmatory factor analyses; structural equation modeling | Obsessive-compulsive symptoms; emotional reactivity; depression; anxiety; fear of COVID-19 | Medium |
| Tian et al., 2020 [44] | China | 31 January to 2 February 2020 | n = 1060 adults, n = 22 < 18 years old, no information on gender | Online via the Wenjuanxing survey platform, no other information provided | SCL-90 using the Global Severity Index (reliability not reported for the present sample) | Descriptives; T-tests; Anovas | Psychological distress through the nine dimensions of SCL-90 | Medium |
| Trzebiński et al., 2020 [43] | Poland | 1–4 April 2020 | n = 317 adults, n = 17 < 18 years, no information on gender | Online via open access forums, no other information provided | COVID-19 SS; STAI; SWLS; MIL; BH | Correlations, Between groups comparisons Correlations and Mediation analysis (total sample) | COVID-19 stress; state-trait anxiety; satisfaction with life; meaning in life; hope | Medium |
| Xie et al., 2020 [39] | China | 28 February to 5 March 2020 | n = 1784 primary school students grades 2 through 6 (56.7% boys) | Online via the Wenjuanxing survey platform, two primary schools in Hubei province | CDI-S; SCARED (reliability not reported for the present sample) | Descriptives Generalised and Logistic regressions | Worry about being infected with COVID-19; Anxiety; Depression | Medium |
| Yang et al., 2020 [38] | China | 28 –30 January 2020 | n = 8252 university students, n = 1118, mean age = 17.9, SD = 0.30, range 16–18 years, no information on gender | Online survey via social media, sms, email, four key universities in Wuhan | A five-point Likert scale created by authors to measure levels of anxiety and fear | Descriptives | Anxiety; Fear | Low |
| Zhou et al., 2020 [36] | China | 8–15 March 2020 | n = 8140 students invited (median age 16, range 12–18 years), n = 8072 included in the study (4326 females) | Online via the Wenjuanxing survey platform, junior and senior high school students in China aged 12–18 years | PHQ-9; GAD-7 (reliability not reported for the present sample) | Desrciptives; Chi-square tests; T-tests; Logistic regressions | Depression; Anxiety | Medium |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nearchou, F.; Flinn, C.; Niland, R.; Subramaniam, S.S.; Hennessy, E. Exploring the Impact of COVID-19 on Mental Health Outcomes in Children and Adolescents: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 8479. https://doi.org/10.3390/ijerph17228479
Nearchou F, Flinn C, Niland R, Subramaniam SS, Hennessy E. Exploring the Impact of COVID-19 on Mental Health Outcomes in Children and Adolescents: A Systematic Review. International Journal of Environmental Research and Public Health. 2020; 17(22):8479. https://doi.org/10.3390/ijerph17228479
Chicago/Turabian StyleNearchou, Finiki, Clodagh Flinn, Rachel Niland, Sheena Siva Subramaniam, and Eilis Hennessy. 2020. "Exploring the Impact of COVID-19 on Mental Health Outcomes in Children and Adolescents: A Systematic Review" International Journal of Environmental Research and Public Health 17, no. 22: 8479. https://doi.org/10.3390/ijerph17228479
APA StyleNearchou, F., Flinn, C., Niland, R., Subramaniam, S. S., & Hennessy, E. (2020). Exploring the Impact of COVID-19 on Mental Health Outcomes in Children and Adolescents: A Systematic Review. International Journal of Environmental Research and Public Health, 17(22), 8479. https://doi.org/10.3390/ijerph17228479








