Impact of Alarm Fatigue on the Work of Nurses in an Intensive Care Environment—A Systematic Review
Abstract
1. Background
1.1. New Technologies—New Challenges for the Nursing Staff
1.2. Nursing Staff Overload—Causes and Effects
2. Method
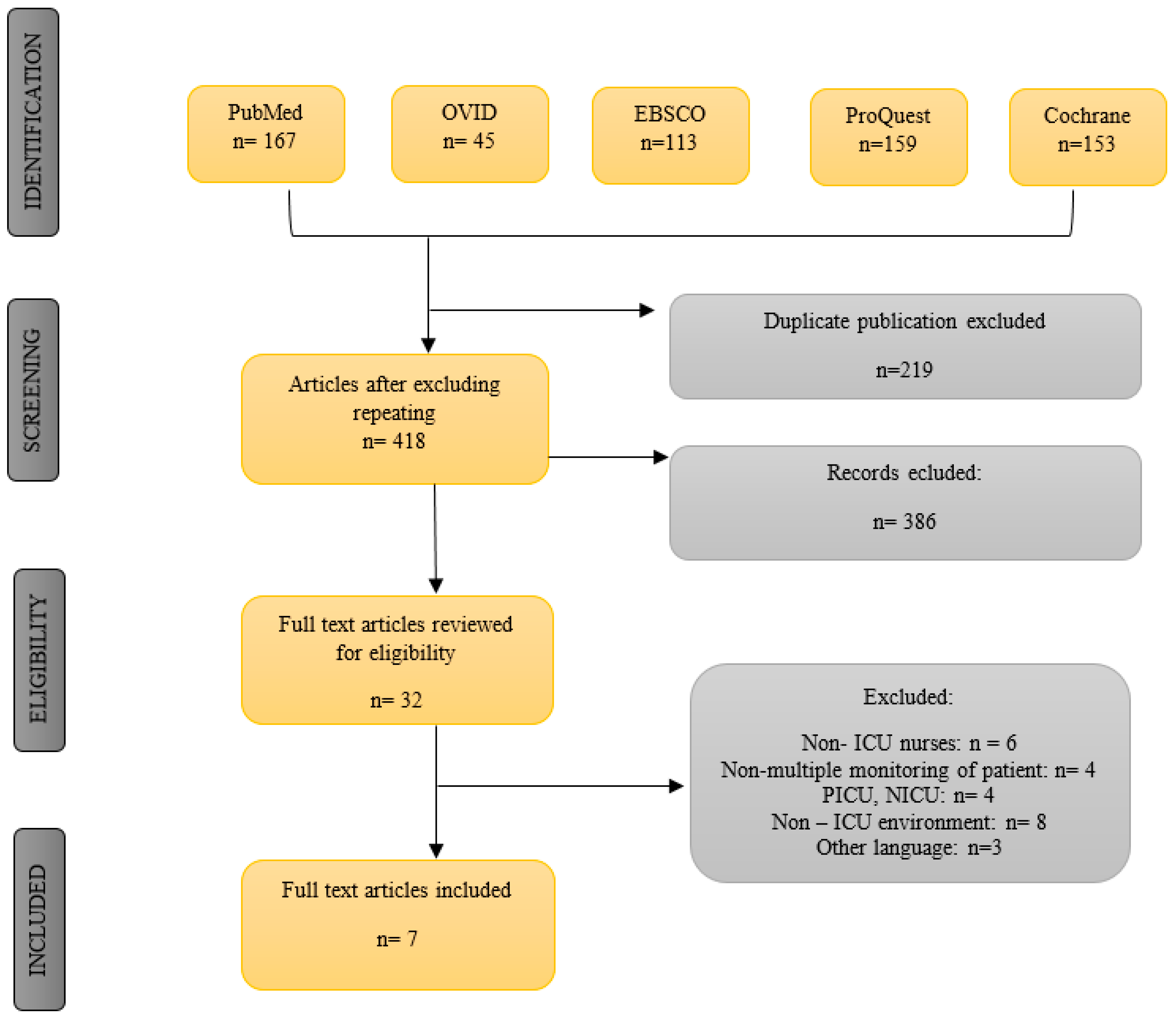
2.1. Research Protocol and Guidelines
2.2. Search Strategy
2.3. Study Selection
- ▪
- articles in English,
- ▪
- research group consisting only of medical personnel,
- ▪
- research carried out among nurses working at adult intensive therapy units, to assess alarm fatigue among personnel,
- ▪
- studies with adult patients, and
- ▪
- studies describing acute and chronic fatigue.
- ▪
- articles in a language other than English or Polish,
- ▪
- research where a study group consisted of members other than medical personnel,
- ▪
- moreover, articles were eliminated that focused on the perception of alarms generated by a single device (e.g., injection pumps or a pulse oximeter), and
- ▪
- studies concerning pediatric intensive therapy units.
2.4. Study Quality Assessment
2.5. Data Extraction
2.6. Data Analysis
3. Results
3.1. Burdensome and False Alarms
3.2. Alarm Fatigue
3.3. Alarm Management
3.4. Risk of Bias
4. Discussion
4.1. Theoretical Implications
4.2. Practical Implications
4.3. Limitation
5. Conclusions
- (1)
- Alarms are unavoidable in intensive care units. The dynamic development of technology makes their number grow drastically, and this will undoubtedly increase in the future as well. Therefore, it is necessary to introduce effective strategies of alarm management as soon as possible.
- (2)
- Nursing personnel feel overburdened with an excessive amount of duties and a continuous wave of clinical alarms.
- (3)
- Nurses often do not perceive the need for education regarding alarms, which is an important element of any alarm management strategy.
- (4)
- In the future, it is worth focusing on assessing the level of alarm fatigue. This would help provide safety both to patients and nursing personnel and verify the effectiveness of strategies that are introduced.
Author Contributions
Funding
Conflicts of Interest
References
- Simpson, K.R.; Lyndon, A. False alarms and overmonitoring: Major factors in alarm fatigue among labor nurses. J. Nurs. Care Qual. 2019, 34, 66–72. [Google Scholar] [CrossRef] [PubMed]
- Purbaugh, T. Alarm fatigue: A roadmap for mitigating the cacophony of beeps. Dimens. Crit. Care Nurs. 2014, 33, 4–7. [Google Scholar] [CrossRef] [PubMed]
- Sowan, A.K.; Gomez, T.M.; Tarriela, A.F.; Reed, C.C.; Paper, B.M. Changes in Default Alarm Settings and Standard In-Service are Insufficient to Improve Alarm Fatigue in an Intensive Care Unit: A Pilot Project. JMIR Hum. Factors 2016, 3. [Google Scholar] [CrossRef] [PubMed]
- Keller, J.P. Clinical alarm hazards: A top ten health technology safety concern. J. Electrocardiol. 2012, 45, 588–591. [Google Scholar] [CrossRef]
- Bitan, Y.; Meyer, J.; Shinar, D.; Zmora, E. Nurses reactions to alarms in a neonatal intensive care unit. Cogn. Technol. Work 2004, 6, 239–246. [Google Scholar] [CrossRef]
- Lewis, C.L.; Oster, C.A. Research Outcomes of Implementing CEASE: An Innovative, Nurse-Driven, Evidence-Based, Patient-Customized Monitoring Bundle to Decrease Alarm Fatigue in the Intensive Care Unit/Step-down Unit. Dimens. Crit. Care Nurs. 2019, 38, 160–173. [Google Scholar] [CrossRef]
- Sowan, A.K.; Vera, A.G.; Fonseca, E.I.; Reed, C.C.; Tarriela, A.F.; Berndt, A.E. Nurse Competence on Physiologic Monitors Use: Toward Eliminating Alarm Fatigue in Intensive Care Units. Open Med. Inform. J. 2017, 11, 1–11. [Google Scholar] [CrossRef]
- ECRI. Institute Top 10 health Technology Hazards for 2020. Health Devices. 2020. Available online: https://elautoclave.files.wordpress.com/2019/10/ecri-top-10-technology-hazards-2020.pdf (accessed on 10 June 2020).
- Cho, O.M.; Kim, H.; Lee, Y.W.; Cho, I. Clinical alarms in intensive care units: Perceived obstacles of alarm management and alarm fatigue in nurses. Healthc. Inform. Res. 2016, 22, 46–53. [Google Scholar] [CrossRef]
- Vitoux, R.R.; Schuster, C.; Glover, K.R. Perceptions of infusion pump alarms: Insights gained from critical care nurses. J. Infus. Nurs. 2018, 41, 309–318. [Google Scholar] [CrossRef]
- Petersen, E.M.; Costanzo, C.L. Assessment of Clinical Alarms Influencing Nurses’ Perceptions of Alarm Fatigue. Dimens. Crit. Care Nurs. 2017, 36, 36–44. [Google Scholar] [CrossRef]
- Winwood, P.C.; Winefield, A.H.; Dawson, D.; Lushington, K. Development and validation of a scale to measure work-related fatigue and recovery: The Occupational Fatigue Exhaustion/Recovery scale (OFER). J. Occup. Environ. Med. 2005, 4, 594–606. [Google Scholar] [CrossRef] [PubMed]
- Sendelbach, S. Alarm Fatigue. Nurs. Clin. N. Am. 2012, 47, 375–382. [Google Scholar] [CrossRef] [PubMed]
- Wung, S.F.; Malone, D.C.; Szalacha, L. Sensory Overload and Technology in Critical Care. Crit. Care Nurs. Clin. N. Am. 2018, 30, 179–190. [Google Scholar] [CrossRef] [PubMed]
- Carayon, P.; Alvarado, C.J. Workload and Patient Safety Among Critical Care Nurses. Crit. Care Nurs. Clin. N. Am. 2007, 19, 121–129. [Google Scholar] [CrossRef]
- Padmakumar, A.D.; Bhasin, V.; Wenham, T.N.; Bodenham, A.R. Evaluation of noise levels in intensive care units in two large teaching hospitals—A prospective observational study. J. Intensive Care Soc. 2013, 14, 205–210. [Google Scholar] [CrossRef]
- Stansfeld, S.A.; Matheson, M.P. Noise pollution: Non-auditory effects on health. Br. Med. Bull. 2003, 68, 243–257. [Google Scholar] [CrossRef]
- Health UKD of Health Building Note 03-01. Adult Acute Mental Health Units. 2013; pp. 6–11. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/147864/HBN_03-01_Final.pdf (accessed on 8 April 2020).
- Epp, K. Burnout in critical care nurses: A literature review. Dynamics 2012, 23, 25–31. [Google Scholar]
- Ruskin, K.J.; Hueske-Kraus, D. Alarm fatigue: Impacts on patient safety. Curr. Opin. Anaesthesiol. 2015, 28, 685–690. [Google Scholar] [CrossRef]
- Schmid, F.; Goepfert, M.S.; Reuter, D.A. Patient monitoring alarms in the ICU and in the operating room. Crit. Care 2013. [Google Scholar] [CrossRef]
- The Joint Commission Sentinel Event Alert—Radiation Risks of Diagnostic Imaging. Available online: http://www.jointcommission.org/assets/1/18/SEA_25.pdf (accessed on 21 July 2020).
- Drew, B.J.; Harris, P.; Zègre-Hemsey, J.K.; Mammone, T.; Schindler, D.; Salas-Boni, R.; Bai, Y.; Tinoco, A.; Ding, Q.; Hu, X. Insights into the problem of alarm fatigue with physiologic monitor devices: A comprehensive observational study of consecutive intensive care unit patients. PLoS ONE 2014, 9. [Google Scholar] [CrossRef]
- OCEBM Levels of Evidence Working Group; Durieux, N.; Pasleau, F.; Howick, J. The Oxford 2011 Levels of Evidence. 2011. Available online: https://www.cebm.ox.ac.uk/resources/levels-of-evidence/ocebm-levels-of-evidence (accessed on 22 October 2020).
- Christensen, M.; Dodds, A.; Sauer, J.; Watts, N. Alarm setting for the critically ill patient: A descriptive pilot survey of nurses’ perceptions of current practice in an Australian Regional Critical Care Unit. Intensive Crit. Care Nurs. 2014, 30, 204–210. [Google Scholar] [CrossRef] [PubMed]
- Sowan, A.K.; Tarriela, A.F.; Gomez, T.M.; Reed, C.C.; Rapp, K.M. Nurses’ Perceptions and Practices Toward Clinical Alarms in a Transplant Cardiac Intensive Care Unit: Exploring Key Issues Leading to Alarm Fatigue. JMIR Hum. Factors 2015, 2, e3. [Google Scholar] [CrossRef] [PubMed]
- Casey, S.; Avalos, G.; Dowling, M. Critical care nurses’ knowledge of alarm fatigue and practices towards alarms: A multicentre study. Intensive Crit. Care Nurs. 2018, 48, 36–41. [Google Scholar] [CrossRef] [PubMed]
- Ruppel, H.; Funk, M.; Whittemore, R.; Wung, S.F.; Bonafide, C.P.; Powell Kennedy, H. Critical care nurses’ clinical reasoning about physiologic monitor alarm customisation: An interpretive descriptive study. J. Clin. Nurs. 2019, 28, 3033–3041. [Google Scholar] [CrossRef] [PubMed]
- Poncette, A.S.; Spies, C.; Mosch, L.; Schieler, M.; Weber-Carstens, S.; Krampe, H.; Balzer, F. Clinical requirements of future patient monitoring in the intensive care unit: Qualitative study. J. Med. Internet Res. 2019, 7, e13064. [Google Scholar] [CrossRef]
- Funk, M.; Clark, J.T.; Bauld, T.J.; Ott, J.C.; Coss, P. Attitudes and practices related to clinical alarms. Am. J. Crit. Care 2014, 23, e9–e18. [Google Scholar] [CrossRef]
- Ruppel, H.; Funk, M.; Tobey Clark, J.; Gieras, I.; David, Y.; Bauld, T.J.; Coss, P.; Holland, M.L. Attitudes and practices related to clinical alarms: A follow-up survey. Am. J. Crit. Care 2018, 27, 114–123. [Google Scholar] [CrossRef]
- AACN Practice Alert. Alarm Management. Crit. Care Nurse 2013, 33, 83–86. [Google Scholar]
- Turmell, J.W.; Coke, L.; Catinella, R.; Hosford, T.; Majeski, A. Alarm Fatigue: Use of an Evidence-Based Alarm Management Strategy. J. Nurs. Care Qual. 2017, 32, 47–54. [Google Scholar] [CrossRef]
- Torabizadeh, C.; Yousefinya, A.; Zand, F.; Rakhshan, M.; Fararooei, M. A nurses’ alarm fatigue questionnaire: Development and psychometric properties. J. Clin. Monit. Comput. 2017, 31, 1305–1312. [Google Scholar] [CrossRef]
| Author and Year of Publication | Country of Study | Ward of Study | Study Group | Type of Research | Method of Assessing Alarm Fatigue | Conclusions |
|---|---|---|---|---|---|---|
| Christensen et al. (2014) [25] | Australia | ICU/CCU/HDU | 48 nurses | Descriptive, survey design | Proprietary questionnaire: 8 open-ended questions 2 multiple choice questions |
|
| Sowan et al. (2015) [26] | United States of America | TCICU | 39 nurses | A cross-sectional survey Descriptive | Clinical study of alarms HTF (20 statements + 9 ranking positions) |
|
| Cho et al. (2016) [9] | South Korea | ICU | 77 nurses | A cross-sectional survey | Clinical study of alarms HTF (14 statements + 9 ranking positions) |
|
| Petersen et al. (2017) [11] | United States of America | ICU PCU | 26 nurses | A cross-sectional survey | Clinical study of alarms HTF (20 statements + 9 ranking positions) |
|
| Casey et al. (2018) [27] | Ireland | ICU PACU HDU | 166 nurses | A cross-sectional survey | Clinical study of alarms HTF (19 statements + 9 ranking positions) |
|
| Ruppel at al. (2019) [28] | United States of America | ICU | 27 nurses | Quality study | Semi-structured interviews |
|
| Poncette et al. (2019) [29] | Germany | ICU | 6 nurses | Qualitative Study | Semi-structured interviews |
|
| Ranking Statements on Issues That Inhibit Effective Management of Clinical Alarms: | Sowan et al. (2015) [26] | Cho et al. (2016) [9] | Petersen et al. (2017) [11] | Casey et al. (2018) [27] | Weighted Average | |
|---|---|---|---|---|---|---|
| Frequent false alarms, which lead to reduced attention or response to alarms when they occur | Average | 4.15 | 2.75 | 3.83 | 2.43 | 2.84 |
| Quantity | 39 | 77 | 26 | 166 | ||
| Difficulty in understanding the priority of an alarm | Average | 3.06 | 3.53 | 3.48 | 3.69 | 3.55 |
| Quantity | 39 | 77 | 26 | 166 | ||
| Inadequate staff to respond to alarms as they occur | Average | 4.23 | 4.86 | 3.13 | 2.66 | 3.45 |
| Quantity | 39 | 77 | 26 | 166 | ||
| Difficulty in hearing alarms when they occur | Average | 3.93 | 4.94 | 4.83 | 3.8 | 4.18 |
| Quantity | 39 | 77 | 26 | 166 | ||
| Difficulty in identifying the source of an alarm | Average | 2.94 | 5.22 | 3.65 | 3.81 | 4.04 |
| Quantity | 39 | 77 | 26 | 166 | ||
| Over reliance on alarms to call attention to patient problems | Average | 4.77 | 5.35 | 4.87 | 3.4 | 4.18 |
| Quantity | 39 | 77 | 26 | 166 | ||
| Noise competition from non-clinical alarms and pages | Average | 4.45 | 5.74 | 6.04 | 4.1 | 4.73 |
| Quantity | 39 | 77 | 26 | 166 | ||
| Lack of training on alarm systems | Average | 6.6 | 6.21 | 4.83 | 3.86 | 4.87 |
| Quantity | 39 | 77 | 26 | 166 | ||
| Difficulty in setting alarms properly | Average | 4.44 | 6.39 | 4.25 | 4.14 | 5.02 |
| Quantity | 39 | 77 | 26 | 166 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lewandowska, K.; Weisbrot, M.; Cieloszyk, A.; Mędrzycka-Dąbrowska, W.; Krupa, S.; Ozga, D. Impact of Alarm Fatigue on the Work of Nurses in an Intensive Care Environment—A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 8409. https://doi.org/10.3390/ijerph17228409
Lewandowska K, Weisbrot M, Cieloszyk A, Mędrzycka-Dąbrowska W, Krupa S, Ozga D. Impact of Alarm Fatigue on the Work of Nurses in an Intensive Care Environment—A Systematic Review. International Journal of Environmental Research and Public Health. 2020; 17(22):8409. https://doi.org/10.3390/ijerph17228409
Chicago/Turabian StyleLewandowska, Katarzyna, Magdalena Weisbrot, Aleksandra Cieloszyk, Wioletta Mędrzycka-Dąbrowska, Sabina Krupa, and Dorota Ozga. 2020. "Impact of Alarm Fatigue on the Work of Nurses in an Intensive Care Environment—A Systematic Review" International Journal of Environmental Research and Public Health 17, no. 22: 8409. https://doi.org/10.3390/ijerph17228409
APA StyleLewandowska, K., Weisbrot, M., Cieloszyk, A., Mędrzycka-Dąbrowska, W., Krupa, S., & Ozga, D. (2020). Impact of Alarm Fatigue on the Work of Nurses in an Intensive Care Environment—A Systematic Review. International Journal of Environmental Research and Public Health, 17(22), 8409. https://doi.org/10.3390/ijerph17228409







