Transfers of Care between Healthcare Professionals in Obstetric Units of Different Sizes across Spain and in a Hospital in Ireland: The MidconBirth Study
Abstract
1. Background
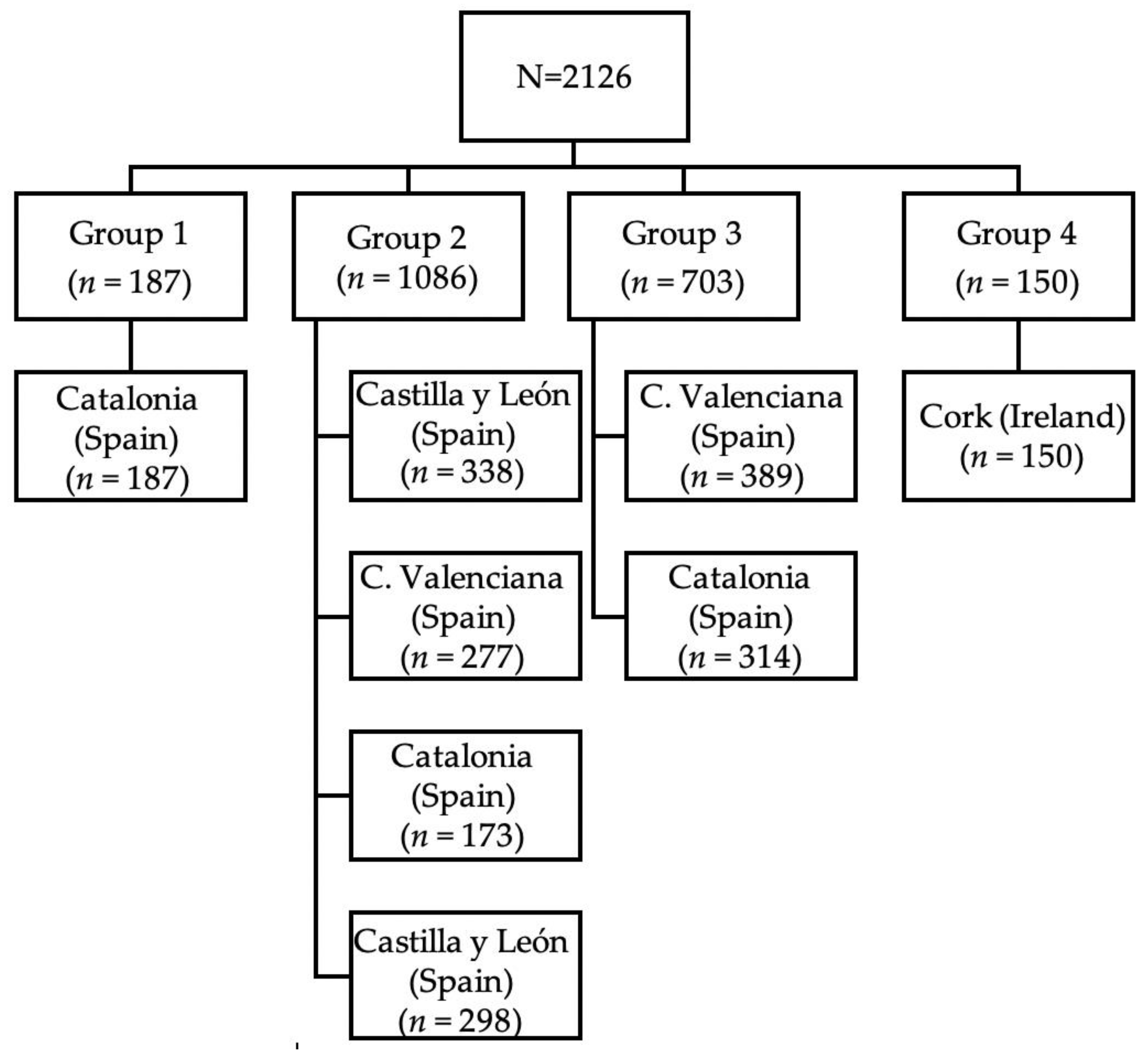
2. Methods
Ethics Approval and Consent to Participate
3. Results
3.1. Characteristics of the Sample
3.2. Transfer Analysis
4. Discussion
4.1. Strengths
4.2. Limitations
4.3. Implications for the Practise and Research
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| LR | Likelihood Ratio |
| OR | Odds Ratio |
| OU | Obstetric Unit |
| OUS | Obstetric Unit Size |
| SVD | Spontaneous Vaginal Delivery |
| S1 | Obstetric unit size 1 (<600 births per year) |
| S2 | Obstetric unit size 2 (from 601 to 1200 births per year) |
| S3 | Obstetric unit size 3 (1201 to 2400 births per year) |
| S4 | Obstetric unit size 4 (>2400 births per year) |
| TOC | Transfer of Care |
References
- Miller, S.; Abalos, E.; Chamillard, M.; Ciapponi, A.; Colaci, D.; Comandé, D.; Diaz, V.; Geller, S.; Hanson, C.; Langer, A.; et al. Beyond too little, too late and too much, too soon: A pathway towards evidence-based, respectful maternity care worldwide. Lancet 2016, 388, 2176–2192. [Google Scholar] [CrossRef]
- Lucas, M.T.B.; Da Rocha, M.J.F.; Costa, K.M.D.M.; De Oliveira, G.G.; Melo, J.D.O. Nursing care during labor in a model maternity unit: Cross-sectional study. Online Braz. J. Nurs. 2015, 14, 32–40. [Google Scholar] [CrossRef]
- Betrán, A.P.; Ye, J.; Moller, A.-B.; Zhang, J.; Gülmezoglu, A.M.; Torloni, M.R. The Increasing Trend in Caesarean Section Rates: Global, Regional and National Estimates: 1990-2014. PLoS ONE 2016, 11, e0148343. [Google Scholar] [CrossRef] [PubMed]
- Vila-Candel, R.; Martín, A.; Escuriet-Peiro, R.; Castro-Sánchez, E.; Soriano-Vidal, F.J. Analysis of Caesarean Section Rates Using the Robson Classification System at a University Hospital in Spain. Int. J. Environ. Res. Public Health 2020, 17, 1575. [Google Scholar] [CrossRef] [PubMed]
- Marshall, J.L.; Spiby, H.; McCormick, F. Evaluating the ‘Focus on Normal Birth and Reducing Caesarean section Rates Rapid Improvement Programme: A mixed method study in England. Midwifery 2015, 31, 332–340. [Google Scholar] [CrossRef]
- Sandall, J.; Soltani, H.; Gates, S.; Shennan, A.; DeVane, D. Midwife-led continuity models versus other models of care for childbearing women. Cochrane Database Syst. Rev. 2016, 4, CD004667. [Google Scholar] [CrossRef]
- Sandall, J. Place of birth in Europe. Entre Nous Eur. Mag. Sex. Reprod. Health 2015, 81, 16–17. [Google Scholar]
- Zeitlin, J.; Mohangoo, A.; Delnord, M. Euro-Peristat Project with Scpe and Eurocat. European Perinatal Health Report. The Health and Care of Pregnant Women and Babies in Europe in 2010. Available online: https://www.europeristat.com/images/European%20Perinatal%20Health%20Report_2010.pdf (accessed on 14 February 2020).
- Escuriet-Peiro, R.; Garcia-Lausin, L.; Salgado-Poveda, I.; Casañas, R.; Robleda, G.; Canet, O.; Pérez-Botella, M.; Frith, L.; Daly, D.; Pueyo, M.J. Midwives’ contribution to normal childbirth care. Cross-sectional study in public health Settings. Midcon Birth Study protocol. Eur. J. Midwifery 2017, 1, 1. [Google Scholar] [CrossRef]
- Renfrew, M.J.; McFadden, A.; Bastos, M.H.; Campbell, J.; Channon, A.A.; Cheung, N.F.; Silva, D.R.A.D.; Downe, S.; Kennedy, H.P.; Malata, A.; et al. Midwifery and quality care: Findings from a new evidence-informed framework for maternal and newborn care. Lancet 2014, 384, 1129–1145. [Google Scholar] [CrossRef]
- Bohren, M.A.; Mehrtash, H.; Fawole, B.; Maung, T.M.; Balde, M.D.; Maya, E.; Thwin, S.S.; Aderoba, A.K.; Vogel, J.P.; Irinyenikan, T.A.; et al. How women are treated during facility-based childbirth in four countries: A cross-sectional study with labour observations and community-based surveys. Lancet 2019, 394, 1750–1763. [Google Scholar] [CrossRef]
- Soriano-Vidal, F.; Vila-Candel, R.; Soriano-Martín, P.; Tejedor-Tornero, A.; Castro-Sánchez, E. The effect of prenatal education classes on the birth expectations of Spanish women. Midwifery 2018, 60, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Escuriet-Peiro, R.; Pueyo, M.J.; Biescas, H.; Colls, C.; Espiga, I.; White, J.; Espada, X.; Fusté, J.; Ortún, V. Obstetric interventions in two groups of hospitals in Catalonia: A cross-sectional study. BMC Pregnancy Childbirth 2014, 14, 143. [Google Scholar] [CrossRef][Green Version]
- Ministry of Health and Social Policy and Equality Report on Attention to Delivery and Birth in the National Health System. Available online: http://www.msssi.gob.es/organizacion/sns/planCalidadSNS/pdf/InformeFinalEAPN_revision8marzo2015.pdf. (accessed on 14 February 2020).
- Department of Health. National Maternity Strategy—Creating a Better Future Together 2016–2026. Available online: https://health.gov.ie/wp-content/uploads/2016/01/Final-version-27.01.16.pdf (accessed on 2 September 2019).
- Walsh, D.; Newburn, M. Towards a social model of childbirth: Part two. Br. J. Midwifery 2002, 10, 540–544. [Google Scholar] [CrossRef]
- Hodnett, E.D. Continuity of caregivers for care during pregnancy and childbirth. Cochrane Database Syst. Rev. 2008, CD000062. [Google Scholar] [CrossRef] [PubMed]
- Vila-Candel, R.; Duke, K.; Soriano-Vidal, F.J.; Castro-Sánchez, E. Affect of Early Skin-to-Skin Mother–Infant Contact in the Maintenance of Exclusive Breastfeeding: Experience in a Health Department in Spain. J. Hum. Lact. 2017, 34, 304–312. [Google Scholar] [CrossRef]
- Petersen, A.; Poetter, U.; Michelsen, C.; Gross, M.M. The sequence of intrapartum interventions: A descriptive approach to the cascade of interventions. Arch. Gynecol. Obstet. 2013, 288, 245–254. [Google Scholar] [CrossRef]
- Nippita, T.A.; Lee, Y.; Patterson, J.; Ford, J.; Morris, J.; Nicholl, M.; Roberts, C. Variation in hospital caesarean section rates and obstetric outcomes among nulliparae at term: A population-based cohort study. BJOG Int. J. Obstet. Gynaecol. 2015, 122, 702–711. [Google Scholar] [CrossRef]
- Glantz, J.C. Obstetric Variation, Intervention, and Outcomes: Doing More but Accomplishing Less. Birth 2012, 39, 286–290. [Google Scholar] [CrossRef]
- Lutomski, J.E.; Morrison, J.J.; Lydon-Rochelle, M.T. Regional variation in obstetrical intervention for hospital birth in the Republic of Ireland, 2005–2009. BMC Pregnancy Childbirth 2012, 12, 123. [Google Scholar] [CrossRef]
- Plough, A.; Galvin, G.; Li, Z.; Lipsitz, S.R.; Alidina, S.; Henrich, N.J.; Hirschhorn, L.R.; Berry, W.R.; Gawande, A.; Peter, D.; et al. Relationship Between Labor and Delivery Unit Management Practices and Maternal Outcomes. Obstet. Gynecol. 2017, 130, 358–365. [Google Scholar] [CrossRef]
- Panda, S.; Begley, C.; Daly, D. Clinicians’ views of factors influencing decision-making for caesarean section: A systematic review and metasynthesis of qualitative, quantitative and mixed methods studies. PLoS ONE 2018, 13, e0200941. [Google Scholar] [CrossRef]
- Behruzi, R.; Hatem, M.; Goulet, L.; Fraser, W.D.W.; Misago, C. Understanding childbirth practices as an organizational cultural phenomenon: A conceptual framework. BMC Pregnancy Childbirth 2013, 13, 205. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, H.; Grant, J.; Walton, C.; Shaw-Battista, J.; Sandall, J. Normalizing Birth in England: A Qualitative Study. J. Midwifery Women’s Health 2010, 55, 262–269. [Google Scholar] [CrossRef] [PubMed]
- Schulkind, L.; Shapiro, T.M. What a difference a day makes: Quantifying the effects of birth timing manipulation on infant health. J. Health Econ. 2014, 33, 139–158. [Google Scholar] [CrossRef] [PubMed]
- Biro, M.A.; Knight, M.; Wallace, E.M.; Papacostas, K.; East, C. Is place of birth associated with mode of birth? The effect of hospital on caesarean section rates in a public metropolitan health service. Aust. N. Z. J. Obstet. Gynaecol. 2013, 54, 64–70. [Google Scholar] [CrossRef] [PubMed]
- Coulm, B.; Le Ray, C.; Lelong, N.; Drewniak, N.; Zeitlin, J.; Blondel, B. Obstetric Interventions for Low-Risk Pregnant Women in France: Do Maternity Unit Characteristics Make a Difference? Birth 2012, 39, 183–191. [Google Scholar] [CrossRef]
- De Jong, J.D.; Groenewegen, P.P.; Westert, G.P. Mutual influences of general practitioners in partnerships. Soc. Sci. Med. 2003, 57, 1515–1524. [Google Scholar] [CrossRef]
- Directive 2005/36/EC of the European Parliament and of the Council of 7 September 2005. Available online: https://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=OJ:L:2005:255:0022:0142:en:PDF (accessed on 19 February 2020).
- Federación de Asociación de Matronas de España. Informe de situación se las matronas en España. Madrid: Federación de Asociación de Matronas de España. Available online: https://federacion-matronas.org/wp-content/uploads/2018/01/informe-situacion-matronas-espana2014-mod3.pdf (accessed on 3 September 2019).
- Escuriet-Peiro, R.; Goberna-Tricas, J.; Pueyo, M.J.; Garriga-Comas, N.; Úbeda-Bonet, I.; Caja-López, C.; Espiga, I.; Ortún-Rubio, V. Impact of maternity care policy in Catalonia: A retrospective cross-sectional study of service delivery in public and private hospitals. BMC Pregnancy Childbirth 2015, 15, 23. [Google Scholar] [CrossRef]
- Goodman, D.C. Unwarranted Variation in Pediatric Medical Care. Pediatr. Clin. N. Am. 2009, 56, 745–755. [Google Scholar] [CrossRef]
- Joyce, R.; Webb, R.; Peacock, J. Predictors of obstetric intervention rates: Case-mix, staffing levels and organisational factors of hospital of birth. J. Obstet. Gynaecol. 2002, 22, 618–625. [Google Scholar] [CrossRef]
- Coonrod, D.V.; Drachman, D.; Hobson, P.; Manríquez, M. Nulliparous term singleton vertex cesarean delivery rates: Institutional and individual level predictors. Am. J. Obstet. Gynecol. 2008, 198, 694.e1–694.e11. [Google Scholar] [CrossRef] [PubMed]
- Rowe, R.E.; Townend, J.; Brocklehurst, P.; Knight, M.; Macfarlane, A.; McCourt, C.; Newburn, M.; Redshaw, M.; Sandall, J.; Silverton, L.; et al. Service configuration, unit characteristics and variation in intervention rates in a national sample of obstetric units in England: An exploratory analysis. BMJ Open 2014, 4, e005551. [Google Scholar] [CrossRef] [PubMed]
- Campbell, P.T.; Rudisill, P.T. Psychosocial Needs of the Critically Ill Obstetric Patient. Crit. Care Nurs. Q. 2006, 29, 77–80. [Google Scholar] [CrossRef] [PubMed]
- Tracy, S.K.; Hartz, D.L.; Tracy, M.B.; Allen, J.; Forti, A.; Hall, B.; White, J.; Lainchbury, A.; Stapleton, H.; Beckmann, M.; et al. Caseload midwifery care versus standard maternity care for women of any risk: M@NGO, a randomised controlled trial. Lancet 2013, 382, 1723–1732. [Google Scholar] [CrossRef]
- Ryan, P.; Revill, P.; DeVane, D.; Normand, C. An assessment of the cost-effectiveness of midwife-led care in the United Kingdom. Midwifery 2013, 29, 368–376. [Google Scholar] [CrossRef]
- Greenhalgh, T.; Humphrey, C.; Hughes, J.; Macfarlane, F.; Butler, C.; Pawson, R. How Do You Modernize a Health Service? A Realist Evaluation of Whole-Scale Transformation in London. Milbank Q. 2009, 87, 391–416. [Google Scholar] [CrossRef]
- Herron, A. Autonomy and Midwifery. Master’s Thesis, Middlesex University, London, UK, 2009. [Google Scholar]
- International Confederation of Midwives. Strategy 2017–2020. The Hague: International Confederation of Midwives. Available online: https://www.internationalmidwives.org/assets/files/general-files/2018/04/final-copy-icm-strategy-2017-20-online.pdf (accessed on 3 September 2019).
| Obstetric Unit Size | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| S1 n = 187 | S2 n = 1086 | S3 n = 703 | S4 n = 150 | |||||||
| n | % | n | % | N | % | n | % | Total | p * | |
| Onset of labour | ||||||||||
| Spontaneous | 163 | 87.2 | 745 | 68.6 | 492 | 70.0 | 127 | 84.6 | 1527 | <0.001 |
| Induced | 23 | 12.3 | 331 | 30.5 | 181 | 25.7 | 22 | 14.7 | 557 | |
| C-section | 1 | 0.5 | 10 | 0.9 | 30 | 4.3 | 1 | 0.7 | 42 | |
| Pharmacological stimulation of labour | ||||||||||
| No | 129 | 69.0 | 419 | 38.6 | 208 | 29.6 | 99 | 66.0 | 855 | <0.001 |
| Yes | 58 | 31.0 | 667 | 61.4 | 495 | 70.4 | 51 | 34.0 | 1271 | |
| Epidural analgesia | ||||||||||
| No | 30 | 16.0 | 169 | 15.6 | 102 | 14.5 | 28 | 18.7 | 329 | 0.632 |
| Yes | 157 | 84.0 | 917 | 84.4 | 601 | 85.5 | 122 | 81.3 | 1797 | |
| Type of birth | ||||||||||
| Normal | 145 | 77.5 | 757 | 69.7 | 442 | 62.9 | 104 | 69.3 | 1448 | <0.001 |
| Dystocic | 42 | 22.5 | 329 | 30.3 | 261 | 37.1 | 46 | 30.7 | 678 | |
| Weight of newborn (g) | ||||||||||
| <2500 | 5 | 2.7 | 15 | 1.4 | 6 | 0.9 | 0 | 0.0 | 26 | <0.001 |
| 2501–3000 | 34 | 18.2 | 227 | 20.9 | 142 | 20.2 | 10 | 6.7 | 413 | |
| 3001–3500 | 84 | 44.9 | 505 | 46.5 | 302 | 43.0 | 52 | 34.7 | 943 | |
| 3501–4000 | 49 | 26.2 | 284 | 26.2 | 212 | 30.2 | 53 | 35.3 | 598 | |
| >4001 | 15 | 8.0 | 55 | 5.1 | 41 | 5.8 | 35 | 23.3 | 146 | |
| Perineum | ||||||||||
| No episiotomy or 1st or 2nd degree | 111 | 59.4 | 555 | 51.1 | 398 | 56.6 | 100 | 66.7 | 1164 | 0.001 |
| Presence of episiotomy or 3rd or 4th degree | 76 | 40.6 | 531 | 48.9 | 305 | 43.4 | 50 | 33.3 | 962 | |
| Postpartum haemorrhage | ||||||||||
| No | 182 | 97.3 | 1064 | 98.0 | 676 | 96.2 | 139 | 92.7 | 2061 | 0.002 |
| Yes | 5 | 2.7 | 22 | 2.0 | 27 | 3.8 | 11 | 7.3 | 65 | |
| Early skin-to-skin contact | ||||||||||
| Yes | 180 | 96.3 | 959 | 88.3 | 646 | 91.9 | 141 | 94.0 | 1926 | 0.001 |
| No | 7 | 3.7 | 127 | 11.7 | 57 | 8.1 | 9 | 6.0 | 200 | |
| Early initiation of breastfeeding | ||||||||||
| Yes | 165 | 88.2 | 823 | 75.8 | 552 | 78.6 | 124 | 83.2 | 1664 | 0.001 |
| No | 22 | 11.8 | 263 | 24.2 | 150 | 21.4 | 25 | 16.8 | 460 | |
| Professional attending the onset of labour | ||||||||||
| Midwife | 181 | 96.8 | 901 | 83.0 | 546 | 77.7 | 149 | 99.3 | 1777 | <0.001 |
| Obstetrician | 6 | 3.2 | 185 | 17.0 | 157 | 22.3 | 1 | 0.7 | 349 | |
| Professional attending the birth | ||||||||||
| Midwife | 132 | 70.6 | 677 | 62.3 | 324 | 46.1 | 104 | 69.3 | 1237 | <0.001 |
| Obstetrician | 55 | 29.4 | 409 | 37.7 | 379 | 53.9 | 46 | 30.7 | 889 | |
| Birth attended by midwife from start to end | ||||||||||
| Yes | 132 | 70.6 | 603 | 55.5 | 317 | 45.1 | 104 | 69.3 | 1156 | <0.001 |
| No | 55 | 29.4 | 483 | 44.5 | 386 | 54.9 | 46 | 30.7 | 970 | |
| Obstetric Unit Size | |||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| S1 | S2 | S3 | S4 | Total | |||||||||||||||||||||
| Midwife Start to End | p * | Midwife Start to End | p * | Midwife Start to End | p * | Midwife Start to End | p * | Midwife Start to End | p * | ||||||||||||||||
| Yes (132) | No (54) | Yes (603) | No (473) | Yes (317) | No (356) | Yes (104) | No (45) | Yes (1156) | No (928) | ||||||||||||||||
| n | % col | n | % col | n | % col | n | % col | n | % col | n | % col | n | % col | n | % col | n | % col | n | % col | ||||||
| Onset of labour | |||||||||||||||||||||||||
| Spontaneous | 120 | 90.9 | 43 | 79.6 | 0.048 | 502 | 83.3 | 243 | 51.4 | <0.001 | 263 | 83 | 229 | 64.3 | <0.001 | 97 | 93.3 | 30 | 66.7 | <0.001 | 982 | 47.1 | 545 | 26.2 | <0.001 |
| Induced | 12 | 9.1 | 11 | 20.4 | 101 | 16.7 | 230 | 48.6 | 54 | 17 | 127 | 35.7 | 7 | 6.7 | 15 | 33.3 | 174 | 8.3 | 383 | 18.4 | |||||
| Pharmacological stimulation | |||||||||||||||||||||||||
| None | 107 | 81.1 | 21 | 38.9 | <0.001 | 288 | 47.8 | 121 | 25.6 | <0.001 | 141 | 44.5 | 65 | 18.3 | <0.001 | 90 | 86.5 | 8 | 17.8 | <0.001 | 626 | 0.3 | 215 | 10.3 | <0.001 |
| Yes | 25 | 18.9 | 33 | 61.1 | 315 | 52.2 | 352 | 74.4 | 176 | 55.5 | 291 | 81.7 | 14 | 13.5 | 37 | 82.2 | 530 | 25.4 | 713 | 34.2 | |||||
| Epidural analgesia | |||||||||||||||||||||||||
| None | 28 | 21.2 | 2 | 3.7 | 0.003 | 128 | 21.2 | 41 | 8.7 | <0.001 | 79 | 24.9 | 23 | 6.5 | <0.001 | 25 | 0.24 | 3 | 6.7 | 0.013 | 260 | 12.5 | 69 | 3.3 | <0.001 |
| Yes | 104 | 78.8 | 52 | 96.3 | 475 | 78.8 | 432 | 91.3 | 238 | 75.1 | 333 | 93.5 | 79 | 0.76 | 42 | 93.3 | 896 | 0.43 | 859 | 41.2 | |||||
| Type of birth | |||||||||||||||||||||||||
| Normal | 132 | 100.0 | 13 | 24.1 | <0.001 | 603 | 1 | 154 | 32.6 | <0.001 | 317 | 1 | 125 | 35.1 | <0.001 | 104 | 1 | 0 | 0 | <0.001 | 1156 | 55.5 | 292 | 0.14 | <0.001 |
| Dystocic | 0 | 0.0 | 41 | 75.9 | 0 | 0 | 319 | 67.4 | 0 | 0 | 231 | 64.9 | 0 | 0 | 45 | 1 | 0 | 0 | 636 | 30.5 | |||||
| Episiotomy | |||||||||||||||||||||||||
| None vs. I-II grade | 100 | 75.8 | 10 | 18.5 | <0.001 | 436 | 72.3 | 118 | 24.9 | <0.001 | 236 | 74.4 | 160 | 44.9 | <0.001 | 98 | 94.2 | 2 | 4.4 | <0.001 | 870 | 41.7 | 290 | 13.9 | <0.001 |
| Yes vs. III-IV grade | 32 | 24.2 | 44 | 81.5 | 167 | 27.7 | 355 | 75.1 | 81 | 25.6 | 196 | 55.1 | 6 | 5.8 | 43 | 95.6 | 286 | 13.7 | 638 | 30.6 | |||||
| Postpartum haemorrhage | |||||||||||||||||||||||||
| None | 129 | 97.7 | 52 | 96.3 | 0.584 | 595 | 98.7 | 459 | 0.97 | 0.06 | 308 | 97.2 | 341 | 95.8 | 0.337 | 98 | 94.2 | 40 | 88.9 | 0.252 | 1130 | 54.2 | 892 | 42.8 | 0.01 |
| Yes | 3 | 2.3 | 2 | 3.7 | 8 | 1.3 | 14 | 0.03 | 9 | 2.8 | 15 | 4.2 | 6 | 5.8 | 5 | 11.1 | 26 | 1.2 | 36 | 1.7 | |||||
| Early skin-to-skin contact | |||||||||||||||||||||||||
| Yes | 128 | 97.0 | 51 | 94.4 | 0.411 | 528 | 87.6 | 424 | 89.6 | 0.289 | 297 | 93.7 | 322 | 90.4 | 0.122 | 98 | 94.2 | 42 | 93.3 | 0.833 | 1051 | 50.4 | 839 | 40.3 | 0.239 |
| None | 4 | 3.0 | 3 | 5.6 | 75 | 12.4 | 49 | 10.4 | 20 | 6.3 | 34 | 9.6 | 6 | 5.8 | 3 | 6.7 | 105 | 0.05 | 89 | 4.3 | |||||
| Early initiation of breastfeeding | |||||||||||||||||||||||||
| Yes | 118 | 89.4 | 46 | 85.2 | 0.42 | 449 | 74.5 | 367 | 77.6 | 0.234 | 242 | 76.6 | 289 | 81.2 | 0.144 | 85 | 82.5 | 39 | 86.7 | 0.529 | 894 | 42.9 | 741 | 35.6 | 0.047 |
| None | 14 | 10.6 | 8 | 14.8 | 154 | 25.5 | 106 | 22.4 | 74 | 23.4 | 67 | 18.8 | 18 | 17.5 | 6 | 13.3 | 260 | 12.5 | 187 | 0.09 | |||||
| p-Value | OR | CI 95% for EXP (B) | |||
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Haemorrhage | S4 (Ref) | 0.001 | |||
| S1 | 0.045 | 0.3 | 0.1 | 0.9 | |
| S2 | 0.000 | 0.2 | 0.9 | 0.4 | |
| S3 | 0.014 | 0.4 | 0.9 | 0.8 | |
| Induced | 0.028 | 1.8 | 1.1 | 3.1 | |
| Episiotomy | 0.001 | 2.6 | 1.5 | 4.4 | |
| Constant | 0.001 | 0.1 | |||
| Breastfeeding | Skin-to-skin contact | 0.001 | 45.9 | 28.9 | 72.8 |
| Constant | 0.001 | 0.2 | |||
| p-Value | OR | 95% CI OR | ||
|---|---|---|---|---|
| Lower | Upper | |||
| Unit Size | ||||
| S4 (Ref) | 0.001 | |||
| S1 | 0.498 | 0.8 | 0.5 | 1.4 |
| S2 | 0.273 | 1.3 | 0.8 | 2.0 |
| S3 | 0.001 | 2.3 | 1.5 | 3.6 |
| Parity | ||||
| Multiparous (Ref) | ||||
| Nulliparous | 0.001 | 2 | 1.6 | 2.4 |
| Beginning of delivery | ||||
| Spontaneous (Ref) | ||||
| Induction | 0.001 | 3 | 2.3 | 3.8 |
| Pharmacologic stimulation | ||||
| None (Ref) | ||||
| Yes | 0.011 | 1.4 | 1.1 | 1.8 |
| Epidural analgesia | ||||
| None (Ref) | ||||
| Yes | 0.001 | 1.7 | 1.2 | 2.4 |
| Episiotomy | ||||
| None (Ref) | ||||
| Yes | 0.001 | 5.3 | 4.3 | 6.6 |
| Constant | 0.001 | 0.1 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martín-Arribas, A.; Vila-Candel, R.; O’Connell, R.; Dillon, M.; Vila-Bellido, I.; Beneyto, M.Á.; De Molina-Fernández, I.; Rodríguez-Conesa, N.; González-Blázquez, C.; Escuriet, R. Transfers of Care between Healthcare Professionals in Obstetric Units of Different Sizes across Spain and in a Hospital in Ireland: The MidconBirth Study. Int. J. Environ. Res. Public Health 2020, 17, 8394. https://doi.org/10.3390/ijerph17228394
Martín-Arribas A, Vila-Candel R, O’Connell R, Dillon M, Vila-Bellido I, Beneyto MÁ, De Molina-Fernández I, Rodríguez-Conesa N, González-Blázquez C, Escuriet R. Transfers of Care between Healthcare Professionals in Obstetric Units of Different Sizes across Spain and in a Hospital in Ireland: The MidconBirth Study. International Journal of Environmental Research and Public Health. 2020; 17(22):8394. https://doi.org/10.3390/ijerph17228394
Chicago/Turabian StyleMartín-Arribas, Anna, Rafael Vila-Candel, Rhona O’Connell, Martina Dillon, Inmaculada Vila-Bellido, M. Ángeles Beneyto, Inmaculada De Molina-Fernández, Nerea Rodríguez-Conesa, Cristina González-Blázquez, and Ramón Escuriet. 2020. "Transfers of Care between Healthcare Professionals in Obstetric Units of Different Sizes across Spain and in a Hospital in Ireland: The MidconBirth Study" International Journal of Environmental Research and Public Health 17, no. 22: 8394. https://doi.org/10.3390/ijerph17228394
APA StyleMartín-Arribas, A., Vila-Candel, R., O’Connell, R., Dillon, M., Vila-Bellido, I., Beneyto, M. Á., De Molina-Fernández, I., Rodríguez-Conesa, N., González-Blázquez, C., & Escuriet, R. (2020). Transfers of Care between Healthcare Professionals in Obstetric Units of Different Sizes across Spain and in a Hospital in Ireland: The MidconBirth Study. International Journal of Environmental Research and Public Health, 17(22), 8394. https://doi.org/10.3390/ijerph17228394








