Breastfeeding in China: A Review of Changes in the Past Decade
Abstract
1. Introduction
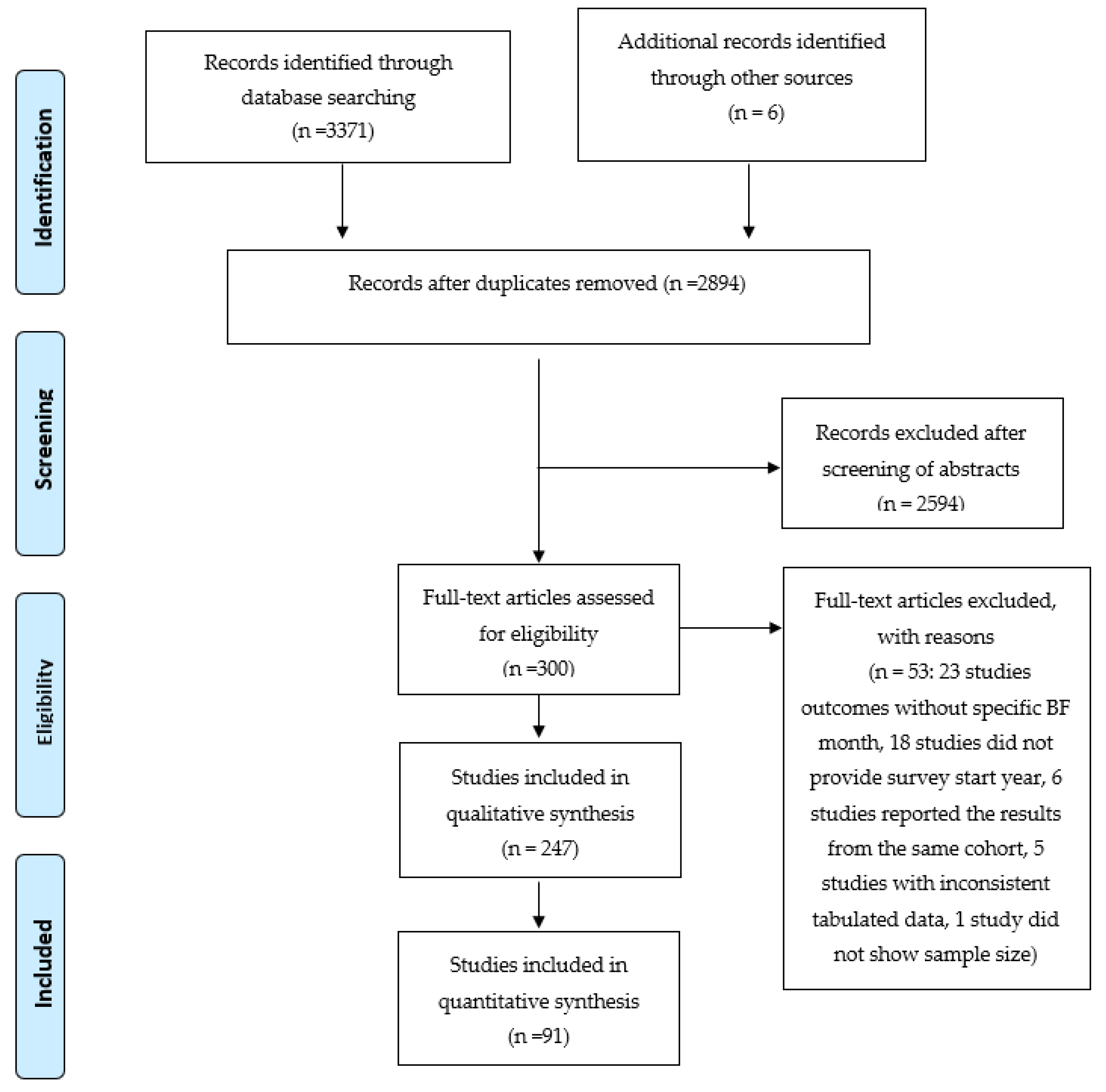
2. Materials and Methods
Definitions of Breastfeeding
3. Results
3.1. Breastfeeding Rates in China from Cohort Studies
3.2. Breastfeeding Rates in China from Other Types of Studies
3.3. Reasons for the Variation in Reported Breastfeeding Rates
3.4. Length of Breastfeeding and Proportion Breastfeeding in China from 2007 to 2017
3.5. Breastfeeding in Minority Areas or Groups
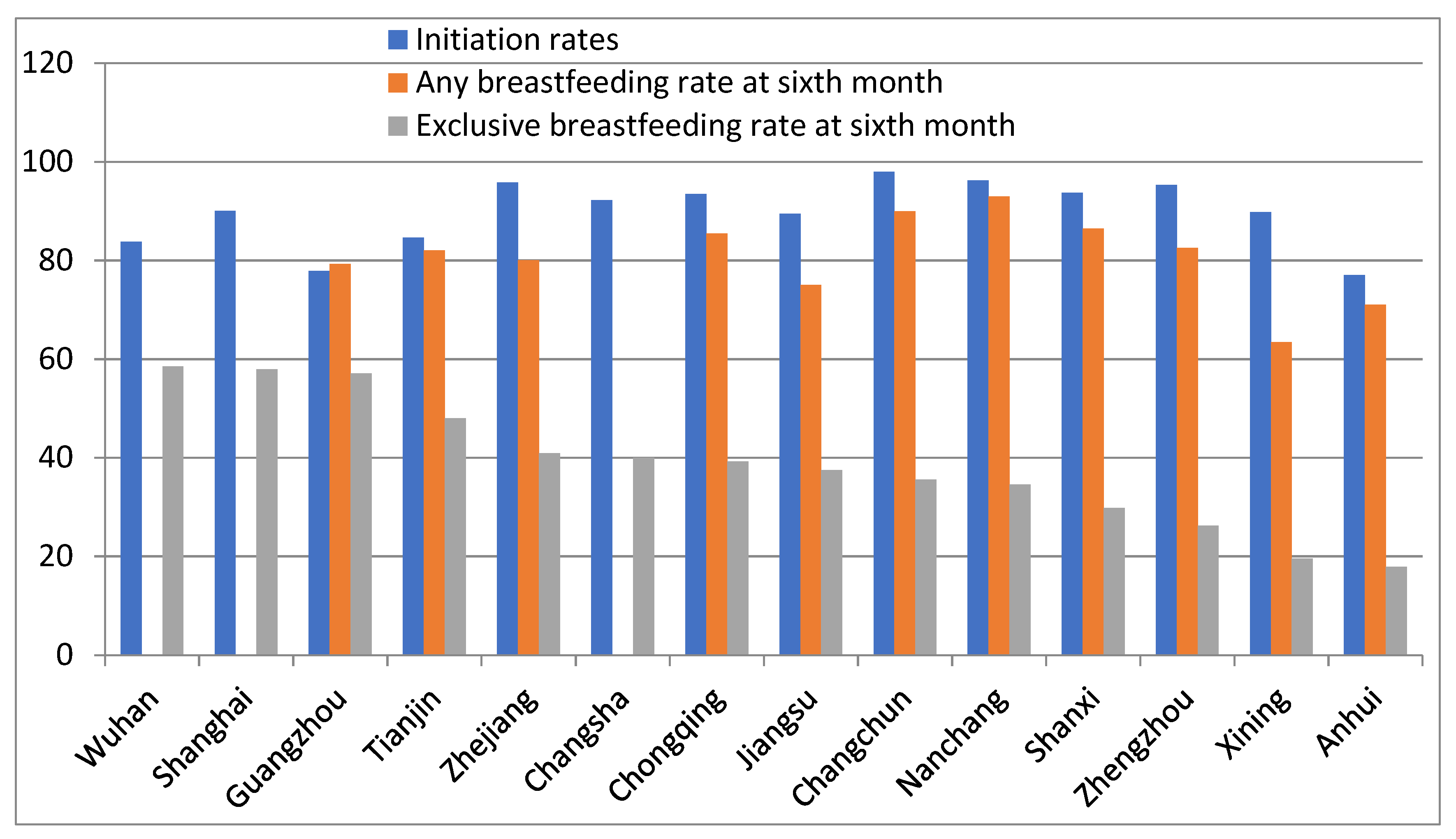
3.6. Changes in Breastfeeding Rates in China from 2007 to 2017
3.7. Reasons for Discontinuing Breastfeeding or Exclusive Breastfeeding before Six Months in China
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Victoria, C.G. Effect of breastfeeding on infant and child mortality due to infectious diseases in less developed countries: A pooled analysis. WHO Collaborative Study Team on the Role of Breastfeeding on the Prevention of Infant Mortality. Lancet 2000, 355, 451–455. [Google Scholar]
- Zhou, Y.; Chen, J.; Li, Q.; Huang, W.; Lan, H.; Jiang, H. Association between breastfeeding and breast cancer risk: Evidence from a meta-analysis. Breastfeed. Med. 2015, 10, 175–182. [Google Scholar] [CrossRef]
- WHO. Breastfeeding. Available online: http://www.who.int/maternal_child_adolescent/topics/child/nutrition/breastfeeding/en (accessed on 13 November 2018).
- WHO. Global Nutrition Targets 2025: Policy, Brief and Series. Available online: http://www.who.int/nutrition/publications/globaltargets2025_policybrief_overview/en/ (accessed on 13 November 2018).
- China State Council. National Program of Action for Child Development in China (2011–2020); 2011-08-09; China People’s Publishing House: Beijing, China, 2011; p. 14.
- Xu, F.; Qiu, L.; Binns, C.W.; Liu, X. Breastfeeding in China: A review. Int. Breastfeed. J. 2009, 4, 6. [Google Scholar] [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. Int. J. Surg. 2014, 12, 1495–1499. [Google Scholar] [CrossRef]
- Zhao, J.; Zhao, Y.; Du, M.; Binns, C.W.; Lee, A.H. Does Caesarean Section Affect Breastfeeding Practices in China? A Systematic Review and Meta-Analysis. Matern. Child Health J. 2017, 21, 2008–2024. [Google Scholar] [CrossRef]
- WHO. Infant and Young Child Feeding: A Tool for Assessing National Practices, Policies and Programmes. Available online: https://www.who.int/nutrition/topics/global_strategy/en/ (accessed on 5 July 2020).
- Shi, D.; Ma, L.; Ying, Q. A survey on breastfeeding among medical workers in Beijing. J. Hyg. Res. 2011, 40, 653–654. [Google Scholar] [CrossRef]
- Zhao, M.; Liu, J.; Wang, Q. A survey of breastfeeding of twin babies. J. Nurs. Sci. 2015, 30, 29–32. [Google Scholar] [CrossRef]
- Mei, H.; Zhai, J.; Luo, X. Promote exclusive breastfeeding by the application of forward control. Chin. J. Fam. Plan. Gynecol. 2017, 9, 45–48. [Google Scholar] [CrossRef]
- Yu, C.; Binns, C.W.; Lee, A.H. Comparison of breastfeeding rates and health outcomes for infants receiving care from hospital outpatient clinic and community health centres in China. J. Child Health Care 2016, 20, 286–293. [Google Scholar] [CrossRef]
- Li, Y.; Ma, J.; Lan, J.; Zhang, X. Analysis of breastfeeding rate and influence factors among 747 infants in one community. Ningxia Med. J. 2016, 38, 845–846. [Google Scholar] [CrossRef]
- Liu, Y.; Fu, L. The status of exclusive breastfeeding for 0–6 month infants and the influence on physical development. Matern. Child Health Care China 2015, 30, 5045–5046. [Google Scholar] [CrossRef]
- Zhang, X.; Pang, M.; Li, N. The investigation of the breastfeeding and its influencing factors. ShaanXi Med. Mag. 2015, 44, 1419–1420. [Google Scholar] [CrossRef]
- LI, Q. The investigation and analysis on breastfeeding of 416 babies and mothers’ dietary. Chin. J. Clin. Ration. Drug Use 2010, 3, 109–110. [Google Scholar] [CrossRef]
- Qiu, H.; Wu, X.; Wu, J. Effect of Individualized Continuous Health Education on Improving the Method of the Breastfeeding of Uyghur Women. J. Nongken Med. 2017, 39, 347–349. [Google Scholar] [CrossRef]
- Cui, X. Study of breastfeeding and 12 months social response. Matern. Child Health Care China 2016, 31, 513–516. [Google Scholar]
- OuYang, F.; Yu, Z.; Wang, X.; Xi, T.; Liu, F. A survey on situation of breastfeeding among 0-6 month infants in urban villages. Chin. J. Gen. Pract. 2015, 13, 1125–1127. [Google Scholar] [CrossRef]
- Jia, X.; Xu, J. Survey on breastfeeding among infants of 0-6 months. J. Community Med. 2014, 12, 12–14. [Google Scholar]
- Chen, R.; Yang, Y.; Tian, N.; Mai, W.; Li, A. The study of the breastfeeding and its influencing factors of primipara. Mod. Prev. Med. 2013, 40, 625–626. [Google Scholar]
- Tang, L.; Lee, A.H.; Binns, C.W. Factors associated with breastfeeding duration: A prospective cohort study in Sichuan Province, China. World J. Pediatr WJP 2015, 11, 232–238. [Google Scholar] [CrossRef]
- Gu, C.; Yan, S.; Li, Q.; Du, Y.; Wang, S.; Zhu, H. Follow-up survey of premature infants’ breastfeeding. Chin. Rural Health Serv. Adm. 2010, 30, 577–579. [Google Scholar]
- Li, J.; Li, Z. Investigation and analysis of breastfeeding practices in Mianyang urban area. Chongqing Med. 2009, 38, 2876–2877. [Google Scholar] [CrossRef]
- Fei, W.; Ying, Y. The impact of effective early sucking on breastfeeding for baby at 6 months. Chin. J. Child Health Care 2009, 17, 481–482. [Google Scholar]
- Chen, Q.; Zhao, W.; Lin, Q.; Wang, E.; Zheng, S.; Chen, Y. The status quo of breastfeeding for baby with 6 months in Wenling city. China Rural Med. 2017, 24, 55–57. [Google Scholar] [CrossRef]
- Lei, J.; Jin, H.; Ye, P.; HE, J.; Zhou, X.; Fu, W.; Liu, L. A study on the influencing factors of breastfeeding for 0-6 month infants. Zhengjiang Prev. Med. 2015, 27, 1115–1118. [Google Scholar] [CrossRef]
- Wu, Y.; Qiu, L. An analysis on the status and influencing factors of breastfeeding among infants within six months of age. Zhengjiang Prev. Med. 2015, 27, 245–248. [Google Scholar] [CrossRef]
- Jiao, Y.; Huang, S. The investigation and analysis of breastfeeding in kang county in Longnan region. Chin. Community Phys. Med. Prof. 2011, 13, 203. [Google Scholar] [CrossRef]
- Xu, F.; Liu, X.; Binns, C.W.; Xiao, C.; Wu, J.; Lee, A.H. A decade of change in breastfeeding in China’s far north-west. Int. Breastfeed. J. 2006, 1, 22. [Google Scholar] [CrossRef]
- Xu, F.; Binns, C.; Zheng, S.; Wang, Y.; Zhao, Y.; Lee, A. Determinants of exclusive breastfeeding duration in Xinjiang, PR China. Asia Pac. J. Clin. Nutr. 2007, 16, 316–321. [Google Scholar] [CrossRef]
- Gao, X. The Status and Influencing Factors of Breastfeeding in Poor Rural Areas of Western China. Master’s Thesis, Shaanxi Normal University, Xi’an, Chian, 2017. [Google Scholar]
- Huang, Y.; Zhang, W.; Fang, L. Duration of breastfeeding and its influencing factors in children from poor areas of Anhui. Chin. J. Child Health Care 2017, 25, 1150–1152. [Google Scholar] [CrossRef]
- Wang, N.; Chen, Q. Study on Factors of Duration of Infants Breastfeeding: Based on Questionnaire Survey of Yuexiu District of Guangzhou City. Chin. J. Soc. Med. 2017, 34, 478–482. [Google Scholar] [CrossRef]
- Wu, J.; Shao, B.; Huang, M.; Gu, L.; Li, M.; Jiang, S.; Mo, M.; Ximusiye, M.; Wang, J.; Jiang, W.; et al. The situation and influencing factors of breastfeeding in Zhoushan from 2002 to 2015. Chin. J. Dis. Control Prev. 2018, 22, 485–489. [Google Scholar] [CrossRef]
- Gao, W. Analysis of breastfeeding and its influencing factors in Heping district of Tianjin. J. Qiqihar Univ. Med. 2016, 37, 3068–3070. [Google Scholar]
- Wang, J. A survey on breastfeeding of infants at 0-6 months. Nei Mong. J. Tradit. Chin. Med. 2014, 33, 60. [Google Scholar] [CrossRef]
- Tang, J. Influencing factors and intervention measures of infant pure breast feeding compliance. China Pract. Med. 2016, 11, 191–193. [Google Scholar] [CrossRef]
- Sun, S.; Zhang, Z.; Wan, H. Survey of influencing factors of postpartum breastfeeding. Chin. Nurs. Res. 2016, 30, 2626–2629. [Google Scholar] [CrossRef]
- Zhang, Y.; Jiang, H. The analysis on the status and influencing factors of the breast-feeding postpartum in 42 days. Today Nurse 2017, 6, 35–37. [Google Scholar]
- Cheng, G. Regulation of the Impact of Children’s Health Management on Children’s 6-month Exclusive Breastfeeding Rate. Syst. Med. 2018, 3, 184–185. [Google Scholar] [CrossRef]
- Zhang, Q.; Shi, Y. The analysis of influencing factors of breastfeeding rates among 612 women. Matern. Child Health Care China 2013, 28, 5095–5096. [Google Scholar] [CrossRef]
- Fu, Y. Investigate the Affect of Post-natal Care Intervention on Breastfeeding Rates and Duration. China Health Stand. Manag. 2015, 6, 256–258. [Google Scholar] [CrossRef]
- Zhou, R. The related factors and intervention for Breastfeeding and its compliance. Med. J. Present Clin. 2017, 30, 3414–3418. [Google Scholar] [CrossRef]
- Deng, Y. A Study on Breastfeeding Self-Efficacy and its Influencing Factors in Postpartum Women from 0 to 6 Months in Wuhan. Mater’s Thesis, Wuhan Polytechnic University, WuHan, China, 2017. [Google Scholar]
- Li, G.; Chen, X.; Pan, Y.; Luo, J.; Fan, X. Survey on the relationship between breastfeeding and anemia in 6-month-old child of flower town in Guangzhou. J. Baotou Med. Coll. 2016, 32, 14–16. [Google Scholar] [CrossRef]
- Chen, Z.; Wang, S.; Zhai, C. The effect of postpartum extended care on promoting breastfeeding practice. Acad. J. Guangzhou Med. Univ. 2015, 43, 119–120. [Google Scholar] [CrossRef]
- Zhou, H.; Kuang, Y.; Hou, D.; Xie, D.; Zhang, J. The status quo of breastfeeding and its influencing factors in Changsha. Pract. Prev. Med. 2017, 24, 210–212. [Google Scholar] [CrossRef]
- Ma, Y.; Xu, D.; Wang, L.; Wang, Y. Breast feeding studies on Hui nationality infants in Xining and Xian areas. Chin. J. Child Health Care 2014, 22, 871–873. [Google Scholar] [CrossRef]
- Lv, F. A survey on breastfeeding of infants at 6 months age in Xining. Qinghai Med. J. 2016, 46, 59–60. [Google Scholar]
- Feng, S.; Liu, Y.; Guo, J.; LI, X.; Zhao, L.; Liu, B.; Zhang, X.; Liu, H. Analysis on neonatal feeding status and influencing factors in Changchun city. Matern. Child Health Care China 2015, 30, 5844–5846. [Google Scholar] [CrossRef]
- Wang, Q.; Ge, M.; Shao, J. A survey on breastfeeding of infants in rural and urban areas in Jilin province in 2007–2010. Matern. Child Health Care China 2012, 27, 4255–4256. [Google Scholar]
- Chen, W.; Liang, X.; Zhou, J. A survey on exclusive breastfeeding of infants before 6 months age and its influencing factors in Nanchang. Chongqing Med. 2014, 43, 3399–3401. [Google Scholar] [CrossRef]
- Xu, W.; Lei, J.; Zhou, Q. A survey on primipara’s breastfeeding confidence and its influencing factors. J. Tradit. Chin. Med. Manag. 2018, 26, 14–17. [Google Scholar] [CrossRef]
- Liu, L.; Hu, J.; Jin, H.; LEI, J. Investigation and related factors analysis of breast feeding of infants under 6 months in Lishui. Chin. J. Child Health Care 2014, 22, 1092–1095. [Google Scholar] [CrossRef]
- Zhao, F. Status and related factors of exclusive breastfeeding of infants within 6 months in a certain area. Prev. Med. 2018, 3, 105–106. [Google Scholar] [CrossRef]
- Wang, N. A survey on breastfeeding at 4-6 months among primipara. J. Heze Med. Coll. 2015, 27, 85–87. [Google Scholar] [CrossRef]
- Guo, L. The Study of Impact on Social and Psychological Factors in Breastfeeding. Master’s Thesis, Shanxi Medical university, Taiyuan, China, 2010. [Google Scholar]
- Yin, X.; Gui, J.; Wang, H.; Huang, X.; Zhou, M.; Zhu, P. Follow-up survey of risk factors for early cessation of breastfeeding in early infancy. Chin. J. Neonatol. 2012, 27, 148–152. [Google Scholar] [CrossRef]
- Cai, C.; Hao, J.; Tao, F.; Zhang, Y.; Wang, D.; Zhu, P.; Su, P.; Sun, L. Dietary Patterns in Pregnancy, Breastfeeding and Mental Development in Infants: A Population-Based Cohort Study. J. Anhui Med. Univ. 2013, 48, 634–638. [Google Scholar]
- Zhang, Z. The related factors and prevention countermeasures for breastfeeding compliance before 6 months. Contemp. Med. 2017, 23, 32–33. [Google Scholar] [CrossRef]
- Zhu, D. The influence of postpartum visit on exclusive breastfeeding. J. Taishan Med. College 2014, 35, 1190–1191. [Google Scholar] [CrossRef]
- Zhang, Y.; Wang, H.; Luo, Q.; Zhang, L.; Wang, S.; Yao, L. The exclusive breastfeeding of newborns and its influencing factors. Chin. J. Child Health Care 2012, 20, 507–509. [Google Scholar]
- Yang, M.; Liu, N.; Yang, C.; Zheng, X.; Xiong, C.; YANG, S.; Du, Y.; Zhang, J. Analysis on the effect factors of pure breastfeeding among the rural infants in five provinces of Western China. Matern. Child Health Care China 2012, 27, 1035–1037. [Google Scholar]
- Guo, S.; Fu, X.; Scherpbier, R.W.; Wang, Y.; Zhou, H.; Wang, X.; Hipgrave, D.B. Breastfeeding rates in central and western China in 2010: Implications for child and population health. Bull. World Health Org. 2013, 91, 322–331. [Google Scholar] [CrossRef] [PubMed]
- Duan, Y.; Yang, Z.; Lai, J.; Yu, D.; Chang, S.; Pang, X.; Jiang, S.; Zhang, H.; Bi, Y.; Wang, J.; et al. Exclusive Breastfeeding Rate and Complementary Feeding Indicators in China: A National Representative Survey in 2013. Nutrients 2018, 10. [Google Scholar] [CrossRef]
- Zhang, L.; Feng, S.; Wen, F. Analysis of the status and influencing factors of breastfeeding among infants within six months of ages in Haidian neighbourhood of Haidian district of Beijing. Chin. J. Child Health Care 2016, 24, 1081–1083. [Google Scholar] [CrossRef]
- Li, W.; Du, L.; Hu, S.; Zhu, L. Survey on knowledge, attitude, belief and practice of exclusive breastfeeding among mothers of infants aged below 6 months in Shanghai. Chin. J. Dis. Control Prev. 2018, 22, 490–493. [Google Scholar] [CrossRef]
- Su, S.; Qu, W.; Ni, B.; Sun, J. Status quo and influencing factors of breastfeeding among infants aged 6-month and elder in Dalian municipality. Chin. J. Public Health 2017, 33, 792–795. [Google Scholar] [CrossRef]
- Wu, X.; Sun, X.; He, S. Analysis of the status and influencing factors of the exclusive breastfeeding among six months infants. Chin. J. Child Health Care 2017, 25, 90–93. [Google Scholar] [CrossRef]
- Yang, S.; Hong, Q.; Sun, X.; Hao, Y.; Deng, Y.; Duan, S. Analysis of the status and influencing factors of breastfeeding in Anhui province. Chin. J. Child Health Care 2017, 25, 1152–1155. [Google Scholar] [CrossRef]
- Wang, F. The Status and Influencing Factors Analysis of the Postpartum Nurse’ Breastfeeding in Third-Grade Class-A Hospitals. Master’s Thesis, Shandong University, Jinan, China, 2018. [Google Scholar]
- Li, C.R.; Du, Y.P. Quantitative analysis of breastfeeding and maternal and infant health care conditions in different fetal times of multiparas under the two-child policy. Chin. Gen. Pract. 2017, 20, 3659–3664. [Google Scholar] [CrossRef]
- Huang, Y.; He, P.; Huang, B.; Wang, F. Analysis on factors that may influence working mother’s breastfeeding practice. Chin. J. Child Health Care 2014, 22, 142–145. [Google Scholar]
- Liu, W.; Li, S. Duration of exclusive breastfeeding and its influence factors in Shandong. Chin. J. Child Health Care 2016, 24, 410–412. [Google Scholar] [CrossRef]
- Hua, J.; Wu, Z.; Deng, W.; Duan, C.; Lei, P.; Gu, G.; Yan, H.; Yao, F.; Wang, Y. Factors influencing exclusive breastfeeding in the rural areas of mid-west China. Chin. J. Child Health Care 2010, 25, 3229–3232. [Google Scholar]
- Zhang, W. The impact of Continuous care on maternal skills and exclusive breastfeeding for women within 6 months after delivering. Today Nurse 2017, 74–75. [Google Scholar]
- Liu, P.; Wang, Y.; Yu, P.; Le, Y.; Tang, L.; Xu, F. Influence of Breastfeeding Handbook on Exclusive Breastfeeding within First Six Months. J. Appl. Clin. Pediatr. 2010, 25, 366–367. [Google Scholar]
- Li, C. Study on the Implementation and Influencing Factors of Breastfeeding and Health Care Service in Eastern China after the Second-Child Policy. Master’s Thesis, Zhejiang University, Hangzhou, China, 2018. [Google Scholar]
- Chinese Government. Special Regulation for Female Employee Protection. Available online: http://www.gov.cn/flfg/2012-05/07/content_2131582.htm (accessed on 8 September 2020).
- Baidu Encylopedia. Maternity Leave. Available online: https://baike.baidu.com/item/%E4%BA%A7%E5%81%87/9380360?fr=aladdin (accessed on 14 September 2020).
- Chinese Government. Modification of Population and Family Planning Law. Available online: http://www.npc.gov.cn/wxzl/gongbao/2016-02/26/content_1987077.htm (accessed on 14 September 2020).
- Baidu Encyclopedia. Second-Child Policy. Available online: https://baike.baidu.com/item/%E4%BA%8C%E5%AD%A9%E6%94%BF%E7%AD%96/18761690?fromtitle=%E4%BA%8C%E8%83%8E%E6%94%BF%E7%AD%96&fromid=4671776 (accessed on 14 September 2020).
- Jiang, H.; Li, M.; Wen, L.M.; Hu, Q.; Yang, D.; He, G.; Baur, L.A.; Dibley, M.J.; Qian, X. Effect of short message service on infant feeding practice: Findings from a community-based study in Shanghai, China. JAMA Pediatr. 2014, 168, 471–478. [Google Scholar] [CrossRef]
- Doan, T.T.D.; Binns, C.; Pham, N.M.; Zhao, Y.; Dinh, T.P.H.; Bui, T.T.H.; Tran, T.C.; Nguyen, X.H.; Giglia, R.; Xu, F.; et al. Improving Breastfeeding by Empowering Mothers in Vietnam: A Randomised Controlled Trial of a Mobile App. Int. J. Environ. Res. Public Health 2020, 17, 5552. [Google Scholar] [CrossRef] [PubMed]
- Chinese Government. The Law of Population and Family Planning. Available online: http://www.gov.cn/banshi/2005-08/21/content_25059.htm (accessed on 14 September 2020).
- China Development Research Founation. Report of Factors Associated with Breastfeeding in China (2017). Available online: https://cdrf.org.cn/jjhdt/4853.jhtml (accessed on 15 September 2020).
- Feng, L. Clinical Research of Compliance Related Influence Factors of Women Breastfeeding in Ili Hospital. XinJiang Med. J. 2016, 46, 1307–1309. [Google Scholar]
- Ma, X. A survey on breastfeeding and its influencing factors in Tuoli county. World Latest Med. Inf. Electron. Vers. 2017, 17, 150–151. [Google Scholar]
- Huang, Y.; Cheng, Z. A survey on breastfeeding at discharge among 200 women. Tibet. Med. J. 2017, 38, 58–60. [Google Scholar]
- Pubu, Q. The investigation on breastfeeding in 0-2 years old infant in Xizang. Xizang Med. 2017, 38, 52–53+49. [Google Scholar]
- Shu, Y. Status Quo and analysis for exclusive breastfeeding in 4 communities in Dongchuan district. Chin. Community Dr. 2011, 13, 306–307. [Google Scholar]
- Qi, M. Status Quo and analysis for breastfeeding in Hailaer area. Women’s Health Res. 2017, 8, 50–51. [Google Scholar] [CrossRef]
- Yang, Y. The analysis for breastfeeding and complementary food among infants at 0-4 months. J. HeBei United Univ. 2010, 12, 360–361. [Google Scholar] [CrossRef]
- Ma, M. The analysis for influencing factors of exclusive breastfeeding among infants during the puerperium. Guaugxi Med. J. 2012, 34, 1704–1705. [Google Scholar]
- Wu, Y. Effect of pregnancy health education on delivery modes and exclusive breastfeeding. Popul. Sci. Technol. 2015, 17, 73–75. [Google Scholar]
- Wei, M. The impact of “the Outline of Development of Chinese Women (2011-2020)” on neonatal exclusive breastfeeding in the community. Shanghai Med. 2018, 39, 61–62. [Google Scholar] [CrossRef]
- Yu, T.; Ye, M.; Dong, H.; Jiang, J. Influencial factors and nursing for breastfeeding behaviors of primiparas. J. Clin. Pathol. Res. 2018, 38, 1573–1578. [Google Scholar]
- UNICEF; WHO. Country Experiences with Baby-Friendly Hospital Initiative, Compendium Case Studies from around World; UNICEF: New York, NY, USA, 2017; p. 61. [Google Scholar]
- Center for Health Statistics and Information NHPC. An Analysis Report National Health Services Survey in China, 2008; China Union Medical University Press: Beijing, China, 2009. [Google Scholar]
- Center for Health Statistics and Information NHPC. The Fifth National Health Service Report, 2013; China Union Medical University Press: Beijing, China, 2015. [Google Scholar]
- Yang, H.; Yin, D.; Xiao, F.; Li, R.; Xin, Q.; Wang, L.; Zheng, X.; Yin, T.; Liu, X.; Chen, B. The assessment of impact of Standard health management for children at 6 months on exclusive breastfeeding rate. Matern. Child Health Care China 2016, 31, 5066–5069. [Google Scholar] [CrossRef]
- Qian, X.; Liu, A.; Yu, W.; Jiang, F.; Zhao, L. Analysis on the status and factors influencing the breastfeeding of children under 2 years of age in poverty stricken areas of China in 2007–2009. J. Hyg. Res. 2012, 41, 56–59. [Google Scholar]
- Robinson, H.; Buccini, G.; Curry, L.; Perez-Escamilla, R. The World Health Organization Code and exclusive breastfeeding in China, India, and Vietnam. Matern. Child Nutr. 2019, 15, e12685. [Google Scholar] [CrossRef] [PubMed]
- Liu, A.; Dai, Y.; Xie, X.; Chen, L. Implementation of international code of marketing breast-milk substitutes in China. Breastfeed. Med. 2014, 9, 467–472. [Google Scholar] [CrossRef]
- Zhu, Y.; Wan, H. Influencing factors of pure breastfeeding behavior at postpartum 4 months on the basis on planned behavior theory. Chin. Nurs. Res. 2016, 30, 3051–3053. [Google Scholar] [CrossRef]
- Zhao, Z.; Li, X.; Ma, P.; Yang, Z. The investigation of early exclusive breastfeeding after delivery among rural migrant women and urban women in the city of Yuncheng. Matern. Child Health Care China 2017, 32, 3016–3018. [Google Scholar] [CrossRef]
- Li, R.; Chen, Y.; Chen, K.; Wei, X.; Zhao, J. Status and the influence factors of the exclusive breast feeding in Panzhihua east rural areas. Chin. J. Child Health Care 2017, 25, 627–630. [Google Scholar] [CrossRef]



| Study Details | Baby’s Age (month a) | Any Breastfeeding | 95% CI | Exclusive Breastfeeding | 95% CI | ||
|---|---|---|---|---|---|---|---|
| Beijing [10] n = 360 Survey year: 2007–2009 | 1 | 95.00 | 92.75 | 97.25 | 64.17 | 59.22 | 69.12 |
| 4 | 89.72 | 86.58 | 92.86 | 40.83 | 35.75 | 45.91 | |
| 6 | 79.44 | 75.27 | 83.61 | 10.56 | 7.39 | 13.73 | |
| Shanghai [11] n = 296 Survey year: 2014 | 0 | 82.09 | 77.72 | 86.46 | 28.72 | 23.57 | 33.87 |
| 1 | 77.03 | 72.24 | 81.82 | 27.70 | 22.60 | 32.80 | |
| 3 | 66.22 | 60.83 | 71.61 | 24.32 | 19.43 | 29.21 | |
| 6 | 47.30 | 41.61 | 52.99 | 10.81 | 7.27 | 14.35 | |
| Chengdu [12] n = 438 Survey year: 2015–2016 | 0 | 87.90 | 84.85 | 90.95 | 60.96 | 56.39 | 65.53 |
| 1 | 86.07 | 82.83 | 89.31 | 47.95 | 43.27 | 52.63 | |
| 4 | 79.45 | 75.67 | 83.23 | 37.90 | 33.36 | 42.44 | |
| 6 | 66.89 | 62.48 | 71.30 | 23.52 | 19.55 | 27.49 | |
| Chengdu [13] n = 760 Survey year: 2010–2012 | 1 | 88.00 | 85.69 | 90.31 | 60.50 b | 57.02 | 63.98 |
| 3 | 73.40 | 70.26 | 76.54 | 52.90 b | 49.35 | 56.45 | |
| 6 | 55.40 | 51.87 | 58.93 | 3.20 b | 1.95 | 4.45 | |
| Yinchuan [14] n = 747 Survey year: 2014–2015 | 1 | 94.78 | 93.18 | 96.38 | 54.89 | 51.32 | 58.46 |
| 2 | 92.90 | 91.06 | 94.74 | 51.14 | 47.56 | 54.72 | |
| 3 | 83.27 | 80.59 | 85.95 | 35.48 | 32.05 | 38.91 | |
| 4 | 80.59 | 77.75 | 83.43 | 27.31 | 24.11 | 30.51 | |
| Changsha [15] n = 228 Survey year: 2012 | 0 | 92.11 | 88.61 | 95.61 | 71.05 | 65.16 | 76.94 |
| 2 | 88.60 | 84.47 | 92.73 | 63.16 | 56.90 | 69.42 | |
| 4 | 77.60 | 72.22 | 83.04 | 46.05 | 39.58 | 52.52 | |
| 6 | 59.60 | 53.28 | 66.02 | 13.16 | 8.77 | 17.55 | |
| Xi’an [16] n = 3580 Survey year: 2013 | 1 | 94.80 | 94.07 | 95.53 | 76.51 | 75.12 | 77.90 |
| 3 | 75.20 | 73.79 | 76.61 | 47.09 | 45.45 | 48.73 | |
| 6 | 46.20 | 44.57 | 47.83 | 16.31 | 15.10 | 17.52 | |
| Guangzhou [17] n = 416 Survey year: 2005–2006 | 1 | 97.60 | 96.13 | 99.07 | 72.12 | 67.81 | 76.43 |
| 3 | 97.12 | 95.51 | 98.73 | 71.39 | 67.05 | 75.73 | |
| 6 | 77.64 | 73.64 | 81.64 | 29.33 | 24.95 | 33.71 | |
| Ka’shen [18] n = 300 Survey year: 2015 | 1 | 88.67 | 85.08 | 92.26 | 51.33 | 45.67 | 56.99 |
| 3 | 86.67 | 82.82 | 90.52 | 38.00 | 32.51 | 43.49 | |
| 6 | 86.00 | 82.07 | 89.93 | 31.67 | 26.41 | 36.93 | |
| Jinzhou [19] n = 972 Survey year: 2014 | 2 | 83.13 | 80.78 | 85.48 | 49.07 | 45.93 | 52.21 |
| 3 | 80.86 | 78.39 | 83.33 | 49.07 | 45.93 | 52.21 | |
| 4 | 77.06 | 74.42 | 79.70 | 30.56 | 27.66 | 33.46 | |
| 6 | 67.08 | 64.13 | 70.03 | 3.29 | 2.17 | 4.41 | |
| Shenzhen [20] n = 325 Survey year: 2013 | 1 | 90.15 | 86.91 | 93.39 | 87.38 | 83.77 | 90.99 |
| 4 | 82.71 | 78.39 | 87.03 | 59.66 | 54.06 | 65.26 | |
| 6 | 66.20 | 60.70 | 71.70 | 33.45 | 27.96 | 38.94 | |
| Akesu [21] n = 400 Survey year: 2011–2012 | 0 | 99.50 | 98.81 | 100.19 | 96.00 | 94.08 | 97.92 |
| 1 | 99.00 | 98.02 | 99.98 | 79.00 | 75.01 | 82.99 | |
| 3 | 98.25 | 96.96 | 99.54 | 62.50 | 57.76 | 67.24 | |
| 6 | 95.50 | 93.47 | 97.53 | 0.50 | 0.14 | 1.80 | |
| Luzhou [22] n = 486 Survey year: 2012 | 1 | 92.59 | 90.26 | 94.92 | 45.06 | 40.64 | 49.48 |
| 3 | 89.71 | 87.01 | 92.41 | 42.80 | 38.40 | 47.20 | |
| 6 | 81.48 | 78.03 | 84.93 | 14.2 | 11.10 | 17.30 | |
| Jiangyou [23] n = 695 Survey year: 2010–2011 | 0 | 95.10 | 93.40 | 96.70 | - | - | - |
| 1 | 92.70 | 90.70 | 94.70 | - | - | - | |
| 3 | 85.10 | 82.30 | 87.80 | - | - | - | |
| 6 | 65.10 | 61.20 | 69.00 | - | - | - | |
| Ma’anshan [24] n = 343 Survey year: 2009 | 2 | 88.92 | 85.60 | 92.24 | 57.43 | 52.20 | 62.66 |
| 3 | 84.84 | 81.04 | 88.64 | 55.98 | 50.73 | 61.23 | |
| 4 | 81.92 | 77.85 | 85.99 | 51.60 | 46.31 | 56.89 | |
| Mianyang [25] n = 1532 Survey year: 2008 | 1 | 95.04 | 93.95 | 96.13 | 91.06 | 89.63 | 92.49 |
| 4 | 87.79 | 86.15 | 89.43 | 45.82 | 43.32 | 48.32 | |
| 6 | 80.03 | 78.03 | 82.03 | 25.00 | 22.83 | 27.17 | |
| Ningbo [26] n = 318 Survey year: 2008 | 2 | 82.39 | 78.20 | 86.58 | 36.00 | 30.58 | 41.12 |
| 3 | 66.67 | 61.49 | 71.85 | 36.00 | 30.58 | 41.12 | |
| 4 | 50.63 | 45.13 | 56.13 | 23.60 | 18.91 | 28.25 | |
| 5 | 47.80 | 42.31 | 53.29 | 10.00 | 13.8 | 13.30 | |
| Wenling [27] n = 500 Survey year: 2014 | 0 | 91.80 | 89.40 | 94.20 | 80.20 | 76.71 | 83.69 |
| 1 | 91.00 | 88.49 | 93.51 | 70.20 | 66.19 | 74.21 | |
| 4 | 86.00 | 82.96 | 89.04 | 52.60 | 48.22 | 56.98 | |
| 6 | 81.40 | 77.99 | 84.81 | 25.60 | 21.77 | 29.43 | |
| Lishui [28] n = 208 Survey year: 2014 | 1 | 89.90 | 85.80 | 94.00 | 34.62 | 28.15 | 41.09 |
| 3 | 84.82 | 79.73 | 89.91 | 34.62 | 28.15 | 41.09 | |
| 6 | 75.68 | 69.50 | 81.86 | 32.97 | 26.20 | 39.74 | |
| Yongkang [29] n = 667 Survey year: 2013 | 1 | 92.50 | 90.50 | 94.50 | 78.11 | 74.97 | 81.25 |
| 3 | 89.06 | 86.69 | 91.43 | 58.92 | 55.19 | 62.65 | |
| 6 | 77.06 | 73.87 | 80.25 | 29.69 | 26.22 | 33.16 | |
| Longnan [30] n = 480 Survey year: 2009 | 1 | 93.13 | 90.87 | 95.39 | 78.75 | 75.09 | 82.41 |
| 3 | 68.13 | 63.96 | 72.30 | 42.29 | 37.87 | 46.71 | |
| 6 | 43.13 | 38.70 | 47.56 | 20.63 | 17.01 | 24.25 | |
| Province or Big City | Survey Commencement | Women (n) | Any BF Rate (%) | 95% CI | |
|---|---|---|---|---|---|
| Shaanxi [33] | 2014 | 1350 | 73.26 | 70.90 | 75.62 |
| Anhui [34] | 2012 | 1332 | 27.40 | 25.00 | 29.80 |
| Shanghai [11] | 2014 | 296 | 14.19 | 10.21 | 18.17 |
| Sichuan [23] | 2010 | 695 | 12.90 | 9.90 | 15.80 |
| Guangzhou [35] | 2013 | 383 | 10.97 | 7.84 | 14.10 |
| Study Site | Initiation Rate | Any Breastfeeding Rate at Six Months | Exclusive Breastfeeding Rate at Six Months | Study Details |
|---|---|---|---|---|
| Changchun * [52,53] | 98.00 | 89.97 | 35.53 | a. Cross-sectional study 2013, n = 349; b. Cohort study 2007–2010, n = 1600 |
| Nanchang * [54] | 96.21 a | 92.93 | 34.53 | Cohort study 2011–2013, n = 976 |
| Zhejiang p [55,56] | 95.80 | 80.00 | 40.89 | a. Retrospective study 2015–2017, n = 429; b. Cross-sectional study 2013, n = 675 |
| Zhengzhou * [43,44] | 95.26 | 82.50 | 26.25 | a. Cross-sectional study 2011–2012, n = 612; b. 2013–2014, n = 800 |
| Shanxi p [57,58,59] | 93.75 | 86.45 b | 29.78 | a. Cross-sectional studies 2016, n = 1193 b. 2014, n = 487 c. 2009, n = 240 |
| Chongqing ** [41,42] | 93.49 | 85.47 | 39.25 | a. Cohort study 2015–2016, n = 215; b. 2016–2018, n = 57,382 |
| Changsha * [49] | 92.20 | - | 40.00 | a. Cross-sectional study 2014, n = 1014 |
| Shanghai ** [39,40] | 90.00 | - | 57.91 | a. Cross-sectional study 2016, n = 200; b. Cohort study 2014, n = 815 |
| Xining * [50,51] | 89.80 | 63.41 | 19.51 | a. Cross-sectional study 2012–2015, n = 1148; b. Cohort study 2013, n = 287 |
| Jiangsu p [62,63] | 89.46 | 75.00 | 37.50 | a. Cross-sectional study 2014–2015, n = 320; b. Cohort study 2010–2013, n = 759 |
| Tianjin ** [37,38] | 84.60 a | 82.00 | 48.00 | a. Cross-sectional study 2015, n = 818 b. Cohort study 2011–2012, n = 200 |
| Wuhan * [45,46] | 83.75 | - | 58.50 | a. Cross-sectional studies 2013–2015, n = 2000; b. 2016–2017, n = 494 |
| Guangzhou * [47,48] | 77.90 | 79.24 | 57.12 | a. Cross-sectional studies 2011–2014 n = 1180; b. 2013–2014, n = 289 |
| Anhui p [34,60,61] | 77.02 | 71.02 | 17.87 c | a. Cross-sectional studies 2008, n = 1736; b. Cohort study 2012–2013, n = 1332; c. 2008–2010, n = 2747 |
| Research Site | Insufficient Breast Milk (%) | Return to Work (%) | Maternal or Child Illness (%) | Mother Dislikes Breastfeeding (%) | Concerns on Nutrition of Breastmilk or Available Formula Milk (%) | Other Reason(s) (%) |
|---|---|---|---|---|---|---|
| Xi’an and Xining * (n = 240, 2013, [50]) | 76.25 | 8.33 | 6.25 | - | 3.75 | 5.42 |
| Shenzhen * (n = 388, 2015, [71]) | 42.01 | 17.01 | - | - | 10.31 | 8.25 |
| Kunming *(n = 216, 2010, [93]) | 38.0 | 23.9 | 22.6 | 5.8 | - | 7.9 |
| Panzhihua ** (n = 293, 2014, [109]) | 62.4 (R) | 18.3 (R) | 32.1 (R) | - | 27.1 (R) | |
| Yuncheng ** (n = 1200, 2016, [108]) | 56.89 (U) 40.15 (R) | 14.08 (U) 8.88 (R) | 3.81 (U) 4.25 (R) | 2.35 (U) 4.05 (R) | 10.41 (U) 22.20 (R) | 12.47 (U) 21.27 (R) |
| Xining ** (n = 1148, 2012–2015, [50]) | 44.6 | 12.5 | 9.4 | 1.7 | 13.2 | 18.5 |
| Hangzhou, Shanghai **(n = 1046, 2017, [80]) | 38.5 | 23.1 | 6.2 | - | 22.9 | 32.2 |
| Yongkang ** (n = 274, 2014, [29]) | 32.85 | 18.25 | 8.39 | - | - | 22.63 |
| Shanghai ** (n = 5672, 2017, [69]) | 26.90 | 32.75 | 18.87 | - | - | 21.48 |
| Shanghai ** (n = 272, 2013–2014, [107]) | 14.70 | 26.10 | - | - | 8.82 | 6.25 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, Q.; Tian, J.; Xu, F.; Binns, C. Breastfeeding in China: A Review of Changes in the Past Decade. Int. J. Environ. Res. Public Health 2020, 17, 8234. https://doi.org/10.3390/ijerph17218234
Li Q, Tian J, Xu F, Binns C. Breastfeeding in China: A Review of Changes in the Past Decade. International Journal of Environmental Research and Public Health. 2020; 17(21):8234. https://doi.org/10.3390/ijerph17218234
Chicago/Turabian StyleLi, Qing, Jianli Tian, Fenglian Xu, and Colin Binns. 2020. "Breastfeeding in China: A Review of Changes in the Past Decade" International Journal of Environmental Research and Public Health 17, no. 21: 8234. https://doi.org/10.3390/ijerph17218234
APA StyleLi, Q., Tian, J., Xu, F., & Binns, C. (2020). Breastfeeding in China: A Review of Changes in the Past Decade. International Journal of Environmental Research and Public Health, 17(21), 8234. https://doi.org/10.3390/ijerph17218234








