Smokers’ and Non-Smokers’ Attitudes towards Smoking Cessation in Saudi Arabia: A Systematic Review
Abstract
1. Introduction
2. Methods
2.1. Approach
2.2. Search Strategy
2.3. Inclusion and Exclusion Criteria
2.4. Outcome Measures
2.5. Critical Appraisal
2.6. Data Extraction
2.7. Data Synthesis
2.8. Ethical Review
3. Results
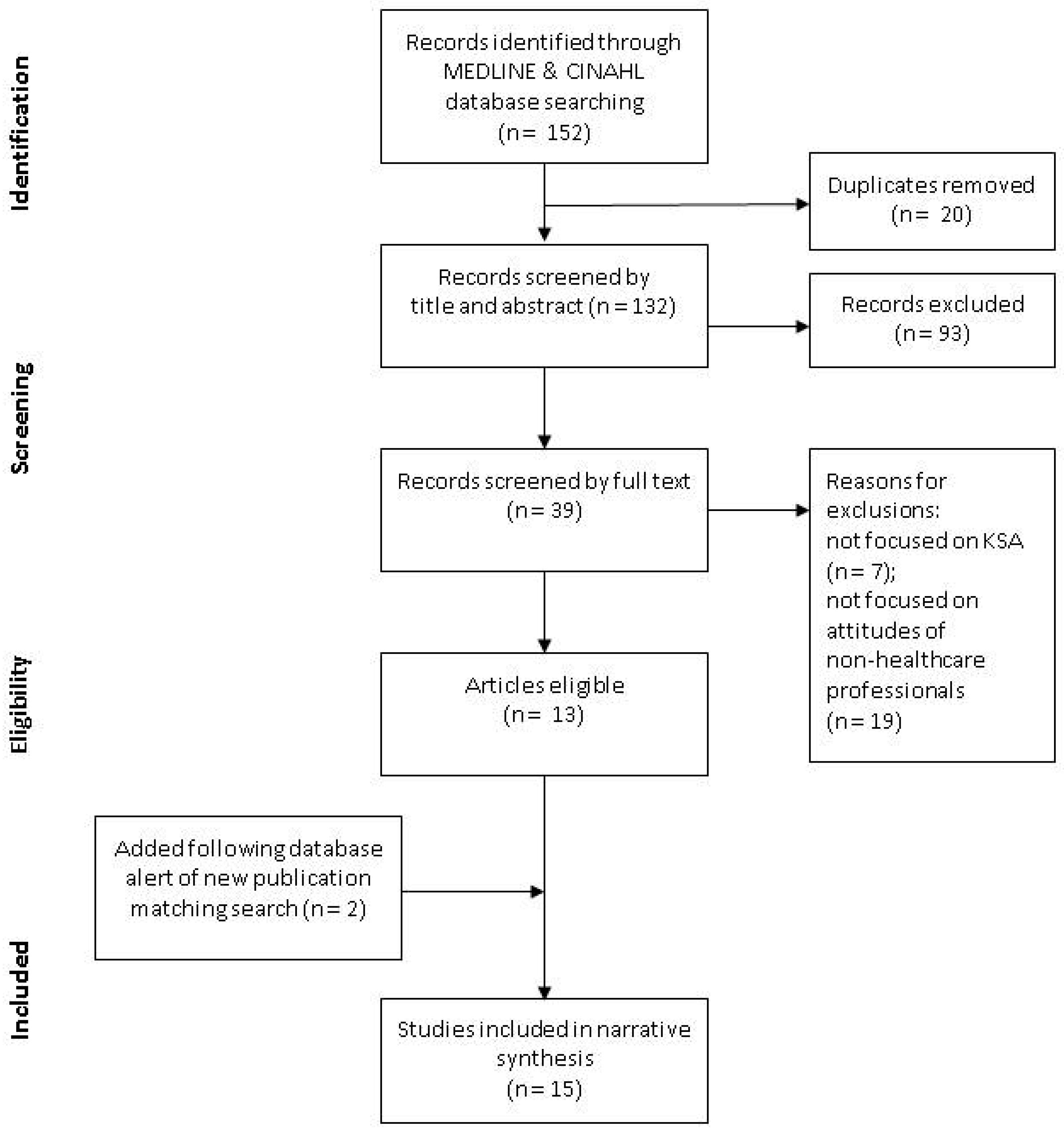
3.1. Search Findings
3.2. Critical Appraisal
3.2.1. Study Types
3.2.2. Research Questions and Methods
3.2.3. Response Rates and Participation Levels
3.2.4. Use of Validated Tools and Guidelines
3.2.5. Quality of Evidence
3.3. Data Extraction
3.4. Secondary Outcome Measures for Context
3.4.1. Smoking Types
3.4.2. Setting
3.4.3. Population and Recruitment
3.4.4. Prevalence of Smoking
3.4.5. Age of Starting Smoking
3.5. Primary Outcome Measures on Smoking Cessation
3.5.1. Reasons for Starting and Not Stopping Smoking
3.5.2. Reasons to Quit Smoking
3.5.3. Attitudes towards Smoke Free Policy and Second-Hand Smoking
3.5.4. Intention to Quit and Quit Attempts
3.5.5. Smoking Cessation Methods and Supports
4. Discussion
4.1. Context and Meaning
4.2. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- WHO Report on the Global Tobacco Epidemic, 2019; World Health Organization: Geneva, Switzerland, 2019; Licence: CC BY-NC-SA 3.0 IGO.
- Simons, D.; Shahab, L.; Brown, J.; Perski, O. The association of smoking status with SARS-CoV-2 infection, hospitalisation and mortality from COVID-19: A living rapid evidence review. Qeios 2020. pre-print. [Google Scholar] [CrossRef]
- Asma, S.; Mackay, J.; Song, S.Y.; Zhao, L.; Morton, J.; Palipudi, K.M.; Zhao, V.L.; Morton, J.; Palipudi, K.M.; Bettcher, D.; et al. The GATS Atlas; CDC Foundation: Atlanta, GA, USA, 2015; Available online: http://gatsatlas.org/downloads/GATS-whole-book-12.pdf (accessed on 14 April 2020).
- Ministry of Health in Saudi Arabia Government. The Executive Regulations of Anti-Smoking Law; Ministry of Health in Saudi Arabia Government: Makkah, Saudi Arabia, 2015. Available online: https://www.moh.gov.sa/en/Ministry/Rules/Documents/Anti-Tobacco-Executive-Regulations.pdf (accessed on 14 April 2020).
- Ministry of Health in Saudi Arabia. Government Approval on the Amendment of the Executive Regulation of Tobacco Control Law (1853515). Available online: https://www.tobaccocontrollaws.org/files/live/Saudi%20Arabia/Saudi%20Arabia%20-%20Amdts.%20to%20Exec.%20Regs.pdf (accessed on 14 April 2020).
- Good Country Practices in the Implementation of WHO FCTC Article 14 and Its Guidelines. Geneva: Secretariat of the WHO Framework Convention on Tobacco Control and the Protocol to Eliminate Illicit Trade in Tobacco Products. Available online: https://www.who.int/fctc/implementation/Good-country-practices-in-the-implementation-of-article-14.pdf (accessed on 14 April 2020).
- Saudi Arabia National Transformation Program 2020. Available online: https://vision2030.gov.sa/sites/default/files/NTP_En.pdf (accessed on 14 April 2020).
- Tahir, M.Z. Smoking and its risks in Saudi Arabia: Literature review. Hamdan. Med. J. 2019, 12, 152–157. [Google Scholar] [CrossRef]
- Salih, M.A.; Farghaly, A.A. Determinants of outcome among smokers in a smoking cessation program. JFCM 1996, 3, 22–31. [Google Scholar]
- Al-Zalabani, A.H.; Abdallah, A.R.; Alqabshawi, R.I. Intention to Quit Smoking among Intermediate and Secondary School Students in Saudi Arabia. Asian Pac. J. Cancer P. 2015, 16, 6741–6747. [Google Scholar]
- Fida, H.R.; Abdelmoneim, I. Prevalence of smoking among secondary school male students in Jeddah, Saudi Arabia: A survey study. BMC Public Health. 2013, 13, 1010. [Google Scholar] [CrossRef] [PubMed]
- Abolfotouh, M.A.; Aziz, M.A.; Badawi, I.A.; Alakija, W. Smoking intervention program for male secondary-school students in the south-western Saudi Arabia. E. Mediterr. Health J. 1997, 3, 90–100. [Google Scholar]
- Baig, M.; Bakarman, M.A.; Gazzaz, Z.J.; Khabaz, M.N.; Ahmed, T.J.; Qureshi, I.A.; Hussain, M.B.; Alzahrani, A.H.; AlShehiri, A.A.; Basendwah, M.A.; et al. Reasons and Motivations for Cigarette Smoking and Barriers against Quitting Among a Sample of Young People in Jeddah, Saudi Arabia. Asian Pac. J. Cancer P. 2016, 17, 3483–3487. [Google Scholar]
- Abdalla, A.M.; Al-Kaabba, A.F.; Saeed, A.A.; Abdulrahman, B.M.; Raat, H. Gender differences in smoking behavior among adolescents in Saudi Arabia. Saudi Med J. 2007, 28, 1102–1108. [Google Scholar]
- Almutairi, K.M. Attitudes of students and employees towards the implementation of a totally smoke free university campus policy at King Saud University in Saudi Arabia: A cross sectional baseline study on smoking behavior following the implementation of policy. J. Community Health 2014, 39, 894–900. [Google Scholar] [CrossRef]
- Almutairi, K.M. Trends in Current Tobacco Use, Smoking Rates and Quit Attempts among Saudi Population during Periods of 17 Years (1996–2012): Narrative Review Article. Iran J. Public. Health 2015, 44, 170. [Google Scholar]
- Al-Arifi, M.N. Prevalence of Smoking and Attitude toward Smoking Cessation among Community Pharmacists, Saudi Arabia. J. Pharm. Technol. 2004, 20, 329–333. [Google Scholar] [CrossRef]
- AlAteeq, M.; Alrashoud, A.M.; Khair, M.; Salam, M. Smoking cessation advice: The self-reported attitudes and practice of primary health care physicians in a military community, central Saudi Arabia. Patient Prefer. Adherence 2016, 10, 651–658. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Jradi, H. Awareness, practices, and barriers regarding smoking cessation treatment among physicians in Saudi Arabia. J. Addict. Dis. 2017, 36, 53–59. [Google Scholar] [CrossRef]
- Al-Jdani, S.; Mashabi, S.; Alsaywid, B.; Zahrani, A. Smoking cessation counseling: Knowledge, attitude and practices of primary healthcare providers at National Guard Primary Healthcare Centers, Western Region, Saudi Arabia. JFCM 2018, 25, 175–182. [Google Scholar]
- Abdelwahab, S.I.; El-Setohy, M.; Alsharqi, A.; Elsanosy, R.; Mohammed, U.Y. Patterns of Use, Cessation Behavior and Socio-Demographic Factors Associated with Smoking in Saudi Arabia: A Cross-Sectional Multi-Step Study. Asian Pac. J. Cancer P. 2016, 17, 655–660. [Google Scholar] [CrossRef]
- Moradi-Lakeh, M.; El Bcheraoui, C.; Tuffaha, M.; Daoud, F.; Al Saeedi, M.; Basulaiman, M.; Mokdad, A.H. Tobacco consumption in the Kingdom of Saudi Arabia, 2013: Findings from a national survey. BMC Public. Health 2015, 15, 611. [Google Scholar] [CrossRef]
- The Ministry of Health in Saudi Arabia Anti-Smoking Clinics. Available online: https://www.moh.gov.sa/en/Ministry/Structure/Programs/TCP/Pages/Anti-smokingClinics.aspx (accessed on 18 February 2019).
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Guyatt, G.; Oxman, A.D.; Akl, E.A.; Kunz, R.; Vist, G.; Brozek, J.; Jaeschke, R. GRADE guidelines: 1. ntroduction—GRADE evidence profiles and summary of findings tables. J. Clin. Epidemiol. 2011, 64, 383–394. [Google Scholar] [CrossRef]
- Al-Mohrej, O.A.; AlTraif, S.I.; Tamim, H.M.; Fakhoury, H. Will any future increase in cigarette price reduce smoking in Saudi Arabia? Ann. Thorac. Med. 2014, 9, 154. [Google Scholar]
- Alyamani, M.J.; Alkriadees, Y.A.; Alkriadees, K.A.; Sharhili, E.A.; Bin Mesained, A.M. Determinants and Predictors of Smoking Cessation Among Undergraduate and Graduate Medical Students: A Cross-Sectional Study in A Private Medical College. Int. J. Adv. Res. 2016, 4, 1608–1617. [Google Scholar] [CrossRef]
- Hajjar, W.M.; Al-Nassar, S.A.; Alahmadi, R.M.; Almohanna, S.M.; Alhihali, S.M. Behavior, knowledge, and attitude of surgeons and patients toward preoperative smoking cessation. Ann. Thorac. Med. 2016, 11, 132. [Google Scholar] [CrossRef]
- Almogbel, Y.S.; Abughosh, S.M.; Almeman, A.A.; Sansgiry, S.S. Factors associated with the willingness to quit smoking among a cohort of university students in the KSA. J. Taibah Univ. Med. Sci. 2016, 11, 128–133. [Google Scholar] [CrossRef]
- Mahdi, H.A.; Elmorsy, S.A.; Melebari, L.A.; Al-Masudi, S.M.; Sharbini, D.A.; Najjar, A.G. Prevalence and intensity of smoking among healthcare workers and their attitude and behavior towards smoking cessation in the western region of Saudi Arabia: A Cross-sectional study. Tob. Prev. Cessation. 2018, 4. [Google Scholar] [CrossRef]
- Onezi, H.A.; Khalifa, M.; El-Metwally, A.; Househ, M. The impact of social media-based support groups on smoking relapse prevention in Saudi Arabia. Comput. Methods Prog. Biomed. 2018, 159, 135–143. [Google Scholar] [CrossRef]
- Jradi, H.; Saddik, B. Graphic warnings and text warning labels on cigarette packages in Riyadh Kingdom of Saudi Arabia: Awareness and perceptions. Ann. Thorac. Med. 2018, 13, 22. [Google Scholar]
- Alqurashi, A.A.; Alluhaybi, H.F.; Al-raddadi, R. Smoking Cessation Outcomes and Predictors Among Individuals Enrolled in the Anti-Tobacco Program in Jeddah 2018. IAJPS 2019, 6, 14972–14978. [Google Scholar]
- Al-Nimr, Y.M.; Farhat, G.; Alwadey, A. Factors Affecting Smoking Initiation and Cessation Among Saudi Women Attending Smoking Cessation Clinics. Sultan Qaboos Univ. Med. J. 2020, 20, e95. [Google Scholar] [CrossRef]
- Amin, H.S.; Alomair, A.N.; Alhammad, A.H.; Altwijri, F.A.; Altaweel, A.A.; Alandejani, T.A. Tobacco consumption and environmental exposure among healthcare students in King Saud University in Riyadh. JFMPC 2020, 9, 657. [Google Scholar] [CrossRef]
- World Health Organization WHO Report on the Global Tobacco Epidemic, 2017 Country Profile: Saudi Arabia. Available online: https://www.who.int/tobacco/surveillance/policy/country_profile/sau.pdf (accessed on 25 October 2020).
- Itumalla, R.; Aldhmadi, B. Combating tobacco in Saudi Arabia: A review of recent initiatives. East Mediterr. Health J. 2020, 26, 858–863. [Google Scholar] [CrossRef] [PubMed]
- Thomas, D.; Abramson, M.J.; Bonevski, B.; Taylor, S.T.; Poole, S.G.; Weeks, G.R.; Dooley, M.J.; George, J. Quitting experiences and preferences for a future quit attempt: A study among inpatient smokers. BMJ Open 2015, 5, e006959. [Google Scholar] [CrossRef]
- George, J.; Taylor, S.; Hong, T.; Leung, S.; Nguyen, J. A pilot study to investigate the scope for an inpatient smoking cessation programme. Intern. Med. J. 2012, 42, e80–e83. [Google Scholar] [CrossRef] [PubMed]
- Thomas, D.; Mackinnon, A.J.; Bonevski, B.; Abramson, M.J.; Taylor, S.; Poole, S.G.; George, J. Development and validation of a 21-item challenges to stopping smoking (CSS-21) scale. BMJ Open 2016, 6, e011265. [Google Scholar] [CrossRef]
| Year of Publication | Authors | Title | Journal |
|---|---|---|---|
| 1996 [9] | Salih MA & Farghaly AA | Determinants of outcome among smokers in a smoking cessation program | Journal of Family & Community Medicine |
| 2014 [15] | Almutairi KM | Attitudes of Students and Employees Towards the Implementation of a Totally Smoke Free University Campus Policy at King Saud University in Saudi Arabia: A Cross Sectional Baseline Study on Smoking Behavior Following the Implementation of Policy | Journal of Community Health |
| 2014 [27] | Al-Mohrej OA, AlTraif SI, Tamim HM, et al. | Will any future increase in cigarette price reduce smoking in Saudi Arabia? | Annals of Thoracic Medicine |
| 2015 [10] | Al-Zalabani AH, Abdallah AR, Alqabshawi RI | Intention to Quit Smoking among Intermediate and Secondary School Students in Saudi Arabia | Asian Pacific Journal of Cancer Prevention |
| 2016 [13] | Baig M, Bakarman MA, Gazzaz ZJ, et al. | Reasons and Motivations for Cigarette Smoking and Barriers against Quitting Among a Sample of Young People in Jeddah, Saudi Arabia | Asian Pacific Journal of Cancer Prevention |
| 2016 [21] | Abdelwahab SI, El-Setohy M, Alsharqi A, et al. | Patterns of Use, Cessation Behavior and Socio-Demographic Factors Associated with Smoking in Saudi Arabia: a Cross- Sectional Multi-Step Study | Asian Pacific Journal of Cancer Prevention |
| 2016 [28] | Alyamani MJ, Alkriadees YA, Alkriadees KA, et al. | Determinants and Predictors of Smoking Cessation among Undergraduate and Graduate Medical Students: a Cross-Sectional Study in a Private Medical College | International Journal of Advanced Research |
| 2016 [29] | Hajjar WM, Al-Nassar SA, Alahmadi RM, et al. | Behavior, knowledge, and attitude of surgeons and patients toward preoperative smoking cessation | Annals of Thoracic Medicine |
| 2016 [30] | Almogbel YS, Abughosh SM, Almeman AA, et al. | Factors associated with the willingness to quit smoking among a cohort of university students in the KSA | Journal of Taibah University Medical Sciences |
| 2018 [31] | Mahdi HA, Elmorsy SA, Melebari LA, et al. | Prevalence and intensity of smoking among healthcare workers and their attitude and behavior towards smoking cessation in the western region of Saudi Arabia: A Cross-sectional study | Tobacco Prevention & Cessation |
| 2018 [32] | Onezi HA, Khalifa M, El-Metwally A, et al. | The impact of social media-based support groups on smoking relapse prevention in Saudi Arabia | Computer Methods and Programs in Biomedicine |
| 2018 [33] | Jradi H, Saddik B | Graphic warnings and text warning labels on cigarette packages in Riyadh Kingdom of Saudi Arabia: Awareness and perceptions | Annals of Thoracic Medicine |
| 2019 [34] | Alqurashi AA, Alluhaybi HF, Al-raddadi R | Smoking Cessation Outcomes and Predictors Among Individuals Enrolled in the Anti-Tobacco Program in Jeddah 2018 | Indo American Journal of Pharmaceutical Sciences |
| 2020 [35] | Al-Nimr YM, Farhat G, Alwadey A | Factors Affecting Smoking Initiation and Cessation Among Saudi Women Attending Smoking Cessation Clinics | Sultan Qaboos University Medical Journal |
| 2020 [36] | Amin HS, Alomair AN, Alhammad AH, et al. | Tobacco consumption and environmental exposure among healthcare students in King Saud University in Riyadh | Journal of Family Medicine and Primary Care |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tobaiqy, M.; Thomas, D.; MacLure, A.; MacLure, K. Smokers’ and Non-Smokers’ Attitudes towards Smoking Cessation in Saudi Arabia: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 8194. https://doi.org/10.3390/ijerph17218194
Tobaiqy M, Thomas D, MacLure A, MacLure K. Smokers’ and Non-Smokers’ Attitudes towards Smoking Cessation in Saudi Arabia: A Systematic Review. International Journal of Environmental Research and Public Health. 2020; 17(21):8194. https://doi.org/10.3390/ijerph17218194
Chicago/Turabian StyleTobaiqy, Mansour, Dennis Thomas, Andrew MacLure, and Katie MacLure. 2020. "Smokers’ and Non-Smokers’ Attitudes towards Smoking Cessation in Saudi Arabia: A Systematic Review" International Journal of Environmental Research and Public Health 17, no. 21: 8194. https://doi.org/10.3390/ijerph17218194
APA StyleTobaiqy, M., Thomas, D., MacLure, A., & MacLure, K. (2020). Smokers’ and Non-Smokers’ Attitudes towards Smoking Cessation in Saudi Arabia: A Systematic Review. International Journal of Environmental Research and Public Health, 17(21), 8194. https://doi.org/10.3390/ijerph17218194







