Psychometric Assessment of the European Health Literacy Survey Questionnaire (HLS-EU-Q16) for Arabic/French-Speaking Migrants in Southern Europe
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Instruments
2.3. Translation
2.4. Sample/Participants
2.5. Data Collection
2.6. Data Analysis
2.7. Ethical Considerations
3. Results
3.1. Translation
3.2. Sample Characteristics
3.3. Construct Validity
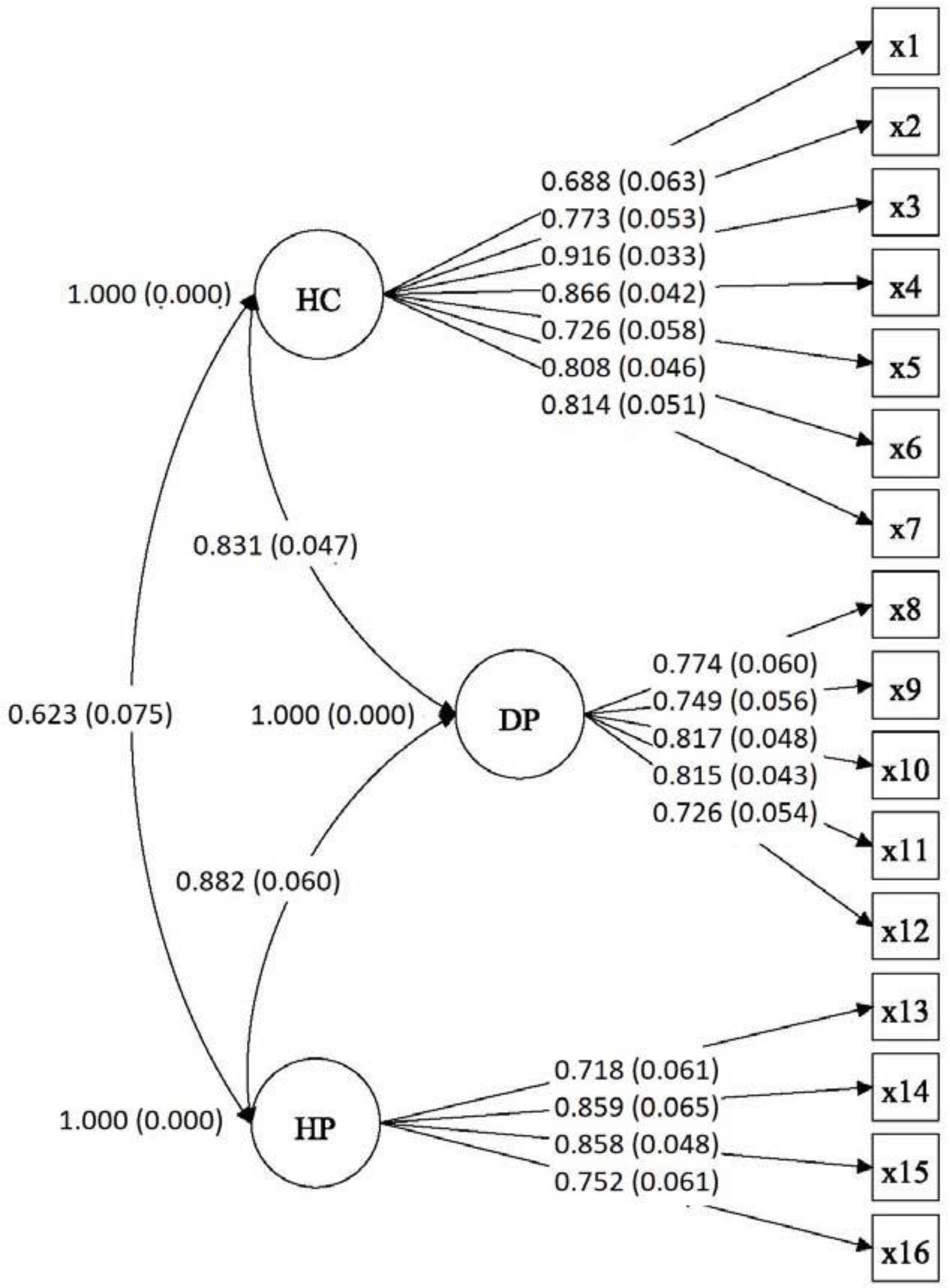
3.3.1. Structural Validity
3.3.2. Hypotheses-Testing (Known Groups Validity)
3.3.3. Criterion Validity
3.4. Distribution of Scores
4. Discussion
Limitations, Strengths, and Practical Implications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Simonds, S.K. Health education as social policy. Health Educ. Monogr. 1974, 2, 1–10. [Google Scholar] [CrossRef]
- Sørensen, K.; Van den Broucke, S.; Fullam, J.; Doyle, G.; Pelikan, J.M.; Slonska, Z.; Brand, H.; HLS-EU Consortium. Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health 2012, 12, 80. [Google Scholar] [CrossRef] [PubMed]
- Sørensen, K.; Van den Broucke, S.; Pelikan, J.M.; Fullam, J.; Doyle, G.; Slonska, Z.; Kondilis, B.; Stoffels, V.; Osborne, R.H.; Brand, H.; et al. Measuring health literacy in populations: Illuminating the design and development process of the European Health Literacy Survey Questionnaire (HLS-EU-Q). BMC Public Health 2013, 13, 948. [Google Scholar] [CrossRef] [PubMed]
- Nakayama, K.; Osaka, W.; Togari, T.; Ishikawa, H.; Yonekura, Y.; Sekido, A.; Matsumoto, M. Comprehensive health literacy in Japan is lower than in Europe: A validated Japanese-language assessment of health literacy. BMC Public Health 2015, 15, 505. [Google Scholar] [CrossRef] [PubMed]
- Duong, T.V.; Aringazina, A.; Baisunova, G.; Pham, T.V.; Pham, K.M.; Truong, T.Q.; Nguyen, K.T.; Oo, W.M.; Mohamad, E.; Su, T.T.; et al. Measuring health literacy in Asia: Validation of the HLS-EU-Q47 survey tool in six Asian countries. J. Epidemiol. 2017, 27, 80–86. [Google Scholar] [CrossRef] [PubMed]
- Pelikan, J.M.; Röthlin, F.; Ganahl, K.; Boltzmann, L. Measuring comprehensive health literacy in general populations: Validation of instrument, indices and scales of the HLS-EU study. In Proceedings of the 6th Annual Health Literacy Research Conference, Bethesda, MD, USA, 3–4 November 2014; Available online: http://www.bumc.bu.edu/healthliteracyconference/files/2014/06/Pelikan-et-al-HARC-2014-fin.pdf (accessed on 7 July 2016).
- Storms, H.; Claes, N.; Aertgeerts, B.; Van den Broucke, S. Measuring health literacy among low literate people: An exploratory feasibility study with the HLS-EU questionnaire. BMC Public Health 2017, 17, 475. [Google Scholar] [CrossRef]
- Wångdahl, J.; Lytsy, P.; Mårtensson, L.; Westerling, R. Poor health and refraining from seeking healthcare are associated with comprehensive health literacy among refugees: A Swedish cross-sectional study. Int. J. Public Health 2018, 63, 409–419. [Google Scholar] [CrossRef]
- Sørensen, K.; Pelikan, J.M.; Rothlin, F.; Ganahl, K.; Slonska, Z.; Doyle, G.; Fullan, J.; Kondilis, B.; Agrafiotis, D.; Uiters, E.; et al. HLS-EU Consortium. Health literacy in Europe: Comparative results of the European Health Literacy Survey (HLS-EU). Eur. J. Public Health 2015, 25, 1053–1058. [Google Scholar] [CrossRef]
- Gele, A.A.; Pettersen, K.S.; Torheim, L.E.; Kumar, B. Health literacy: The missing link in improving the health of Somali immigrant women in Oslo. BMJ Public Health 2016, 16, 1134. [Google Scholar] [CrossRef]
- Nolasco, A.; Barona, C.; Tamayo-Fonseca, N.; Irles, M.Á.; Más, R.; Tuells, J.; Pereyra-Zamora, P. Alfabetización en salud: Propiedades psicométricas del cuestionario HLS-EU-Q16. Gaceta Sanit. 2018. [Google Scholar] [CrossRef]
- Lorini, C.; Lastrucci, V.; Mantwill, S.; Vettori, V.; Bonaccorsi, G. Florence Health Literacy Research Group. Measuring health literacy in Italy: The validation study of the HLS-EU-Q16 and of the HLS-EU-Q6 in Italian language. Ann. Ist. Super. Sanita 2019, 55, 10–18. [Google Scholar] [CrossRef]
- Hajduchová, H.; Bártlová, S.; Brabcová, I.; Motlová, L.; Šedová, L.; Tóthová, V. Zdravotní gramotnost seniorů a její vliv na zdraví a ćerpání zdravotních slušeb. Prakt. Lek. 2017, 97, 223–227. [Google Scholar]
- Levin-Zamir, D.; Baron-Epel, O.B.; Cohen, V.; Elhayany, A. The Association of Health Literacy with Health Behavior, Socioeconomic Indicators, and Self-Assessed Health from a National Adult Survey in Israel. J. Health Commun. 2016, 21, 61–68. [Google Scholar] [CrossRef]
- Wångdahl, J.; Lytsy, P.; Mårtensson, L.; Westerling, R. Health literacy among refugees in Sweden—A cross-sectional study. BMC Public Health 2014, 14, 1030. [Google Scholar] [CrossRef] [PubMed]
- Almaleh, R.; Helmy, Y.; Farhat, E.; Hasan, H.; Abdelhafez, A. Assessment of health literacy among outpatient clinics attendees at Ain Shams University Hospitals, Egypt: A cross-sectional study. Public Health 2017, 151, 137–145. [Google Scholar] [CrossRef]
- Rouquette, A.; Nadot, T.; Labitrie, P.; Van den Broucke, S.; Mancini, J.; Rigal, L.; Ringa, V. Validity and measurement invariance across sex, age, and education level of the French short versions of the European Health Literacy Survey Questionnaire. PLoS ONE 2018, 13, e0208091. [Google Scholar] [CrossRef]
- Gustafsdottir, S.S.; Sigurdardottir, A.K.; Arnadottir, S.K.; Heimisson, G.T.; Mårtensson, L. Translation and cross-cultural adaptation of the European Health Literacy Survey Questionnaire, HLS-EU-Q16: The Icelandic version. BMC Public Health 2020, 20, 61. [Google Scholar] [CrossRef]
- Duong, T.V.; Lin, I.F.; Sørensen, K.; Pelikan, J.M.; Van den Broucke, S.; Lin, Y.C.; Chang, P.W. Health literacy in Taiwan: A population-based study. Asia Pac. J. Public Health 2015, 27, 871–880. [Google Scholar] [CrossRef]
- Prince, L.Y.; Schmidtke, C.; Beck, J.K.; Hadden, K.B. An assessment of organizational health literacy practices at an academic health center. Qual. Manag. Health Care 2018, 27, 93–97. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.Y.D.; Tsai, T.I.; Tsai, Y.W.; Kuo, K.N. Health literacy, health status, and healthcare utilization of Taiwanese adults: Results from a national survey. BMC Public Health 2010, 10, 614. [Google Scholar] [CrossRef] [PubMed]
- Nutbeam, D. The evolving concept of health literacy. Soc. Sci. Med. 2008, 67, 2072–2078. [Google Scholar] [CrossRef]
- Wolf, M.S.; Davis, T.C.; Tilson, H.H.; Bass, P.F.; Parker, R.M. Misunderstanding of prescription drug warning labels among patients with low literacy. Am. J. Health Syst. Pharm. 2006, 63, 1048–1055. [Google Scholar] [CrossRef]
- Dunn, P.; Connard, S. Improving health literacy in patients with chronic conditions: A call to action. Int. J. Cardiol. 2018, 273, 249–251. [Google Scholar] [CrossRef]
- Bas-Sarmiento, P.; Fernández-Gutiérrez, M.; Poza-Méndez, M.; Pelícano-Piri, N. Propuestas de evaluación de la Alfabetización en Salud. Psychol. Lat. 2015, 6, 1–11. [Google Scholar]
- Geltman, P.L.; Adams, J.H.; Penrose, K.L.; Cochran, J.; Rybin, D.; Doros, G.; Henshaw, M.; Paasche-Orlow, M. Health literacy, acculturation, and the use of preventive oral health care by Somali refugees living in Massachusetts. J. Immigr. Minor. Health 2014, 16, 622–630. [Google Scholar] [CrossRef]
- Ng, E.; Omariba, W.R. Immigration, generational status and health literacy in Canada. Health Educ. J. 2013, 27. [Google Scholar] [CrossRef]
- Sentell, T.; Braun, K.L. Low health literacy, limited English proficiency, and health status in Asians, Latinos, and other racial/ethnic groups in California. J. Health Commun. 2012, 17, 82–99. [Google Scholar] [CrossRef]
- Wångdahl, J.; Lytsy, P.; Mårtensson, L.; Westerling, R. Health literacy and refugees’ experiences of the health examination for asylum seekers—A Swedish cross-sectional study. BMC Public Health 2015, 15, 1162. [Google Scholar] [CrossRef] [PubMed]
- Eichler, K.; Wieser, S.; Brugger, U. The costs of limited health literacy: A systematic review. Int. J. Public Health 2009, 54, 313–324. [Google Scholar] [CrossRef]
- Paakkari, L.; Okan, O. COVID-19: Health literacy is an underestimated problem. Lancet Public Health 2020, 5, E249–E250. [Google Scholar] [CrossRef]
- Duong, T.V.; Chang, P.W.; Yang, S.H.; Chen, M.C.; Chao, W.T.; Chen, T.; Chiao, P.; Huang, H.L. A Comprehensive Short-form Health Literacy Survey Tool for Patients in General. Asian Nurs. Res. 2017, 11, 30–35. [Google Scholar] [CrossRef]
- Watson, R. Europeans with poor “health literacy” are heavy users of health services. BMJ 2011, 343, d7741. [Google Scholar] [CrossRef]
- Sundquist, J. Migration, equality and access to health care services. BMJ 2001, 55, 691–692. [Google Scholar] [CrossRef]
- World Health Organization. Report on the Health of Refugees and Migrants in the WHO European Region: No Public Health without Refugees and Migrant Health. 2018. Available online: https://apps.who.int/iris/bitstream/handle/10665/311347/9789289053846eng.pdf?sequence=1&isAllowed=y&ua=1 (accessed on 25 May 2020).
- Instituto Nacional de Estadística. Población Extranjera por Nacionalidad, Provincias, Sexo y año. Available online: https://www.ine.es/jaxi/Tabla.htm?path=/t20/e245/p08/&file=03005.px&L=0 (accessed on 25 May 2020).
- Statista. Número Total de Llegadas de Embarcaciones con Inmigrantes Irregulares a España Entre 2017 y 2019. Available online: https://es.statista.com/estadisticas/1039935/llegadas-de-embarcaciones-con-inmigrantes-ilegales-a-espana/ (accessed on 19 June 2020).
- Rechel, B.; Mladovsky, P.; Ingleby, D.; Mackenbach, J.P.; McKee, M. Migration and health in an increasingly diverse Europe. Lancet 2013, 381, 1235–1245. [Google Scholar] [CrossRef]
- Instituto Nacional de Estadística. Advance on the Municipal Register. Population per Nationality, Autonomous Communities and Provinces. Available online: https://www.ine.es/jaxiPx/Tabla.htm?path=/t20/e245/p04/provi/l0/&file=0ccaa006.px&L=1 (accessed on 20 June 2020).
- Pelikan, J.M.; Ganahl, K.; Van de Broucke, S.; Sorensen, K. Measuring health literacy in Europe: Introducing the European Health Literacy Survey Questionnaire (HLS-EU-Q). In International Handbook of Health Literacy: Research, Practice and Policy across Then Lifespan; Oka, O., Bauer, U., Levin-Zair, D., Pinheiro, P., Sorensen, K., Eds.; Policy Press: Bristol, UK, 2019; pp. 115–138. [Google Scholar]
- Weiss, B.D.; Mays, M.Z.; Martz, W.; Castro, K.M.; DeWalt, D.A.; Pignone, M.P.; Mockbee, J.; Hale, F.A. Quick assessment of literacy in primary care: The Newest Vital Sign. Ann. Fam. Med. 2005, 3, 514–522. [Google Scholar] [CrossRef]
- Luján-Tangarife, J.A.; Cardona-Arias, J.A. Construcción y validación de escalas de medición en salud: Revisión de propiedades psicométricas. Arch. Med. 2015, 11, 1–10. [Google Scholar] [CrossRef]
- Ramada-Rodilla, J.M.; Serra-Pujadas, C.; Delclós-Clanchet, G.L. Adaptación cultural y validación de cuestionarios de salud: Revisión y recomendaciones metodológicas. Salud Pública Mexico 2013, 55, 57–66. [Google Scholar] [CrossRef]
- Beaton, D.E.; Bombardier, C.; Guillemin, F.; Ferraz, M.B. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine 2000, 25, 3186–3191. [Google Scholar] [CrossRef]
- Sousa, V.D.; Rojjanasrirat, W. Translation, adaptation and validation of instruments or scales for use in cross-cultural health care research: A clear and user-friendly guideline. J. Eval. Clin. Pract. 2011, 17, 268–274. [Google Scholar] [CrossRef]
- McCallum, A.; Freitag, D.; Pereira, F. Maximum entropy Markov models for information extraction and segmentation. In Proceedings of the Seventeenth International Conference on Machine Learning (ICML ’00), San Francisco, CA, USA, 29 June–2 July 2000; pp. 591–598. Available online: http://www.ai.mit.edu/courses/6.891-nlp/READINGS/maxent.pdf (accessed on 8 June 2020).
- Thorndike, R.L. Applied Psychometrics; Houghton Mifflin: Boston, MA, USA, 1982. [Google Scholar]
- McDonald, R.P. Test Theory: A Unified Approach; Lawrence Erlbaum: Hillsdale, NJ, USA, 1999. [Google Scholar]
- Crutzen, R.; Peters, G.Y. Scale quality: Alpha is an inadequate estimate and factor—Analytic evidence is needed first of all. Health Psychol. Rev. 2017, 11, 242–247. [Google Scholar] [CrossRef] [PubMed]
- Gerbing, D.W.; Anderson, J.C. An update paradigm for scale development incorporating unidimentionality and its assessment. J. Mark. Res. 1988, 25, 186–192. [Google Scholar] [CrossRef]
- Timmerman, M. Factor Analysis. Available online: http://www.ppsw.rug.nl/~metimmer/FAMET.pdf (accessed on 22 June 2020).
- Kline, R.B. Principles and Practice of Structural Equation Modeling, 4th ed.; Guilford Press: New York, NY, USA, 2010. [Google Scholar]
- Meredith, W. Measurement invariance, factor analysis, and factorial invariance. Psychometrika 1993, 58, 525–543. [Google Scholar] [CrossRef]
- Vandenberg, R.J.; Lance, C.E. A Review and Synthesis of the Measurement Invariance Literature: Suggestions, Practices, and Recommendations for Organizational Research. Organ. Res. Methods 2000, 3, 4–70. [Google Scholar] [CrossRef]
- Millsap, R.E.; Yun-Tein, J. Assessing factorial invariance in ordered—Categorical measures. Multivar. Behav. Res. 2004, 39, 479–515. [Google Scholar] [CrossRef]
- Chen, F. Sensitivity of goodness of fit indexes to lack of measurement invariance. Struct. Equ. Model. A Multidiscip. J. 2007, 14, 464–504. [Google Scholar] [CrossRef]
- Higgins, C.; Lavin, T.; Metcalfe, O. Health Impacts of Education: A Review. 2008. Available online: https://www.drugsandalcohol.ie/11734/1/IPH_HealthImpactsofEducation.pdf (accessed on 2 August 2020).
- Streiner, D.; Norman, G. Health Measurement Scales. A Practical Guide to their Development and Use, 2nd ed.; Oxford University Press: Oxford, UK, 1995. [Google Scholar]
- Muthén, L.K.; Muthén, B.O. Mplus User’s Guide, 8th ed.; Muthén & Muthén: Los Angeles, CA, USA, 2017; Available online: www.statmodel.com (accessed on 8 July 2020).
- Flaherty, J.A.; Gaviria, F.M.; Pathak, D.; Mitchell, T.; Wintrob, R.; Richman, J.A.; Birz, S. Developing instruments for cross-cultural psychiatric research. J. Ner. Ment. Dis. 1988, 176, 257–263. [Google Scholar] [CrossRef]
- Maneesriwongul, W.; Dixon, J. Instrument translation process: A methods review. J. Adv. Nurs. 2014, 48, 175–186. [Google Scholar] [CrossRef]
- Emiral, G.O.; Aygar, H.; Isiktekin, B.; Göktas, S.; Dagtekin, G.; Arslantas, D.; Unsal, A. Health Literacy Scale-European unión-Q16: A validity and reliability study in Turkey. Int. Res. J. Med. Sci. 2018, 6, 1–7. [Google Scholar]
- U.S. Department of Health and Human Services. National Action Plan to Improve Health Literacy. 2010. Available online: http://health.gov/communication/initiatives/health-literacy-action-plan.asp (accessed on 8 February 2019).
- Johnson, S.E.; Baur, C.; Meissner, H.I. Back to basics: Why basic research in needed to create effective health literacy interventions. J. Health Commun. 2011, 16, 22–29. [Google Scholar] [CrossRef] [PubMed]
- Svendsen, M.T.; Bak, C.K.; Sørensen, K.; Pelikan, J.M.; Riddersholm, S.J.; Skals, R.K.; Mortensen, R.N.; Maindal, H.T.; Boggil, H.; Nielsen, G.; et al. Associations of health literacy with socioeconomic position, health risk behavior, and health status: A large national population-based survey among Danish adults. BMC Public Health 2020, 20, 565. [Google Scholar] [CrossRef]
- Fernández-Gutiérrez, M.; Bas-Sarmiento, P.; Albar-Marín, M.J.; Paloma-Castro, O.; Romero-Sánchez, J.M. Health literacy interventions for immigrant populations: A systematic review. Int. Nurs. Rev. 2018, 65, 54–64. [Google Scholar] [CrossRef]
- Fernández-Gutiérrez, M.; Bas-Sarmiento, P.; Poza-Méndez, M. Effect of an mHealth Intervention to Improve Health Literacy in Immigrant Populations: A Quasi-Experimental Study. CIN Comput. Inform. Nurs. 2019, 37, 142–150. [Google Scholar] [CrossRef]
- Paasche-Orlow, M.K.; Parker, R.M.; Gazmararian, J.A.; Nielson-Bohlman, L.T.; Rudd, R.R. The prevalence of limited health literacy. J. Gen. Inter. Med. 2005, 20, 175–184. [Google Scholar] [CrossRef]
- Tiller, D.; Herzog, B.; Kluttig, A.; Haerting, J. Health literacy in an urban elderly East-German population—Results from the population-based CARLA study. BMC Public Health 2015, 15, 883. [Google Scholar] [CrossRef] [PubMed]
- Niedorys, B.; Chrzan-Rodak, A.; Ślusarska, B. Health Literacy—A review of research using the European Health Literacy Questionnaire (HLS-EU-Q16) in 2010–2018. Nurs. 21st Century 2020, 19. [Google Scholar] [CrossRef]
- Amoah, A. Social participation, health literacy, and health and well-being: A cross-sectional study in Ghana. SSM Popul. Health 2018, 4, 263–270. [Google Scholar] [CrossRef] [PubMed]
- Baker, D.W.; Gazmararian, J.A.; Sudano, J.; Patterson, M. The association between age and health literacy among elderly persons. J. Gerontol. B Psychol. Sci. Soc. Sci. 2000, 55, S368–S374. [Google Scholar] [CrossRef]
- Kaphingst, K.A.; Goodman, M.S.; MacMillan, W.D.; Carpenter, C.R.; Griffey, R.T. Effect of cognitive dysfunction on the relationship between age and health literacy. Patient Educ. Couns. 2014, 95, 218–225. [Google Scholar] [CrossRef]
| Socio-Demographic Characteristics | n | % |
|---|---|---|
| Sex | ||
| Male | 83 | 40.5 |
| Female | 122 | 59.5 |
| Age | ||
| Under 35 Years | 121 | 59 |
| From 36 to 50 Years | 67 | 32.7 |
| From 51 to 65 Years | 12 | 5.9 |
| Older than 65 Years | 3 | 1.5 |
| Missing values | 2 | 0.9 |
| Country/Region of Origin (grouped) | ||
| Moroccan | 110 | 53.7 |
| Sub-Saharan | 56 | 27.3 |
| Other | 39 | 19.0 |
| Time in Spain | ||
| Less than a Year | 39 | 19.0 |
| From 1 to 3 Years | 34 | 16.6 |
| More than 3 Years | 131 | 63.9 |
| Missing Values | 1 | 0.5 |
| Education Level | ||
| No Formal Education | 14 | 6.8 |
| Primary | 15 | 7.3 |
| Secondary | 128 | 62.4 |
| University Studies | 18 | 8.8 |
| Does not know/does not answer | 30 | 14.6 |
| Status of Employment | ||
| Working | 51 | 24.9 |
| Unemployed/Inactive | 92 | 44.9 |
| Student | 11 | 5.4 |
| Retired/Permanent Disability | 6 | 2.9 |
| Housewife | 23 | 11.2 |
| Does not know/does not answer | 22 | 10.7 |
| Difficulties to pay Bills at the End of a Month | ||
| Yes | 115 | 56.1 |
| No | 40 | 19.5 |
| Does not know/does not answer | 50 | 24.4 |
| Household’s Net Income per Month | ||
| Less than EUR 800 | 76 | 37.1 |
| Between EUR 800 and 1350 | 24 | 11.7 |
| Between EUR 1350 and 2400 | 7 | 3.4 |
| More than EUR 2400 | 1 | 0.5 |
| Does not know/does not answer | 97 | 47.3 |
| Comparisons | WLSMV χ2 (df) | p | CFI | TLI | RMSEA | Δχ2 (df) | p | ΔCFI | ΔTLI | ΔRMSEA |
|---|---|---|---|---|---|---|---|---|---|---|
| MI for MA/SS | ||||||||||
| Config. model (H0) | 253.83(202) | 0.008 | 0.962 | 0.954 | 0.056 | |||||
| Scalar model (H1) | 267.69(212) | 0.006 | 0.959 | 0.953 | 0.056 | 17.45(10) | 0.065 | 0.003 | 0.001 | 0.000 |
| MI for MA/ON | ||||||||||
| Config. model (H0) | 240.45(202) | 0.033 | 0.952 | 0.942 | 0.051 | |||||
| Scalar model (H1) | 252.26(212) | 0.030 | 0.949 | 0.943 | 0.05 | 15.78(10) | 0.106 | 0.003 | -0.001 | 0.001 |
| MI for SS/ON | ||||||||||
| Config. model (H0) | 214.22(202) | 0.264 | 0.987 | 0.985 | 0.036 | |||||
| Scalar model (H1) | 228.94(212) | 0.200 | 0.982 | 0.980 | 0.041 | 20.23(10) | 0.027 | 0.005 | 0.005 | −0.005 |
| Variables | N | (95% CI) | SD | MEN | WOMEN | (p) (CI) | ||
|---|---|---|---|---|---|---|---|---|
(95% CI) | SD | (95% CI) | SD | |||||
| HLS-EU-Q16 | 205 | 9.65 (9.03–10.28) | 4.51 | 8.86 (7.78–9.95) | 4.97 | 10.19 (9.46–10.93) | 4.10 | (0.046) (−2.63–0.23) |
| Health Care HC-HL | 205 | 4.09 (3.77–4.41) | 2.33 | 3.81 (3.27–4.35) | 2.47 | 4.27 (3.88–4.67) | 2.22 | (0.167) |
| Prevention DP-HL | 205 | 2.72 (2.49–2.96) | 1.69 | 2.51 (2.10–2.93) | 1.90 | 2.86 (2.59–3.14) | 1.53 | (0.165) |
| Promotion HP-HL | 205 | 2.83 (2.65–3.01) | 1.30 | 2.53 (2.21–2.84) | 1.44 | 3.04 (2.83–3.25) | 1.17 | (0.007) (−0.89–0.14) |
| Age | Mean Score | SD | X2 (p) |
|---|---|---|---|
| Less than 35 years | 9.05 | 4.62 | 6.512 (0.089) |
| 36–50 years | 10.74 | 3.90 | |
| 51–65 years | 11.08 | 4.35 | |
| Over 65 years | 10.33 | 5.03 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bas-Sarmiento, P.; Poza-Méndez, M.; Fernández-Gutiérrez, M.; González-Caballero, J.L.; Falcón Romero, M. Psychometric Assessment of the European Health Literacy Survey Questionnaire (HLS-EU-Q16) for Arabic/French-Speaking Migrants in Southern Europe. Int. J. Environ. Res. Public Health 2020, 17, 8181. https://doi.org/10.3390/ijerph17218181
Bas-Sarmiento P, Poza-Méndez M, Fernández-Gutiérrez M, González-Caballero JL, Falcón Romero M. Psychometric Assessment of the European Health Literacy Survey Questionnaire (HLS-EU-Q16) for Arabic/French-Speaking Migrants in Southern Europe. International Journal of Environmental Research and Public Health. 2020; 17(21):8181. https://doi.org/10.3390/ijerph17218181
Chicago/Turabian StyleBas-Sarmiento, Pilar, Miriam Poza-Méndez, Martina Fernández-Gutiérrez, Juan Luis González-Caballero, and María Falcón Romero. 2020. "Psychometric Assessment of the European Health Literacy Survey Questionnaire (HLS-EU-Q16) for Arabic/French-Speaking Migrants in Southern Europe" International Journal of Environmental Research and Public Health 17, no. 21: 8181. https://doi.org/10.3390/ijerph17218181
APA StyleBas-Sarmiento, P., Poza-Méndez, M., Fernández-Gutiérrez, M., González-Caballero, J. L., & Falcón Romero, M. (2020). Psychometric Assessment of the European Health Literacy Survey Questionnaire (HLS-EU-Q16) for Arabic/French-Speaking Migrants in Southern Europe. International Journal of Environmental Research and Public Health, 17(21), 8181. https://doi.org/10.3390/ijerph17218181







