Roles of Physiological Responses and Anthropometric Factors on the Gravitational Force Tolerance for Occupational Hypergravity Exposure
Abstract
1. Introduction
2. Materials and Methods
2.1. Design and Resources
2.2. Study Participants
2.3. Training Protocol
2.4. Definition of Outcome and Covariates
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Burton, R.R.; Whinnery, J.E. Biodynamics: Sustained acceleration. In Fundamentals of Aerospace Medicine, 3rd ed.; DeHart, R.L., Davis, J.R., Eds.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2002; pp. 122–153. [Google Scholar]
- Green, N.D.; Ford, S.A. G-induced loss of consciousness: Retrospective survey results from 2259 military aircrew. Aviat. Space Environ. Med. 2006, 77, 619–623. [Google Scholar]
- Slungaard, E.; McLeod, J.; Green, N.D.C.; Kiran, A.; Newham, D.J.; Harridge, S.D.R. Incidence of g-induced loss of consciousness and almost loss of consciousness in the Royal Air Force. Aerosp. Med. Hum. Perform. 2017, 88, 550–555. [Google Scholar] [CrossRef]
- Green, N.D.C. Effects of long-duration acceleration. In Ernsting’s Aviation Medicine, 4th ed.; Rainford, D.J., Gradwell, D.P., Eds.; Hodder Arnold: London, UK, 2006; pp. 137–158. [Google Scholar]
- Newman, D.G. The cardiovascular system at high Gz. In High G Flight: Physiological Effects and Countermeasures, 1st ed.; Newman, D.G., Ed.; Ashgate: Farnham, UK, 2015; pp. 57–72. [Google Scholar]
- Sevilla, N.L.; Gardner, J.W. G-induced loss of consciousness: Case-control study of 78 G-LOCs in the F-15, F-16, and A-10. Aviat. Space Environ. Med. 2005, 76, 370–374. [Google Scholar]
- van Lieshout, E.J.; van Lieshout, J.J.; Krol, J.; Simons, M.; Karemaker, J.M. Assessment of cardiovascular reflexes is of limited value in predicting maximal +Gz-tolerance. Aviat. Space Environ. Med. 1992, 63, 21–26. [Google Scholar]
- Green, N.; Gaydos, S.; Hutchison, E.; Nicol, E. Prevention of G-LOC. In Handbook of Aviation and Space Medicine, 1st ed.; Green, N., Gaydos, S., Hutchison, E., Nicol, E., Eds.; CPC Press: London, UK, 2019; pp. 103–108. [Google Scholar]
- Ueda, K.; Ogawa, Y.; Yanagida, R.; Aoki, K.; Iwasaki, K. Dose-effect relationship between mild levels of hypergravity and autonomic circulatory regulation. Aerosp. Med. Hum. Perform. 2015, 86, 535–540. [Google Scholar] [CrossRef] [PubMed]
- Borst, C.; Karemaker, J.M. Time delays in the human baroreceptor reflex. J. Auton. Nerv. Syst. 1983, 9, 399–409. [Google Scholar] [CrossRef]
- Forster, E.M.; Whinnery, J.E. Reflex heart rate response to variable onset +Gz. Aviat. Space Environ. Med. 1988, 59, 249–254. [Google Scholar]
- Gillingham, K.K. High-G stress and orientational stress: Physiologic effects of aerial maneuvering. Aviat. Space Environ. Med. 1988, 11, A10–A20. [Google Scholar]
- Gillingham, K.K.; Fosdick, J.P. High-G training for fighter aircrew. Aviat. Space Environ. Med. 1988, 59, 12–19. [Google Scholar] [PubMed]
- Lyons, T.J.; Harding, R.; Freeman, J.; Oakley, C. G-induced loss of consciousness accidents: USAF experience 1982–1990. Aviat. Space Environ. Med. 1992, 63, 60–66. [Google Scholar]
- Webb, J.T.; Oakley, C.J.; Meeker, L.J. Unpredictability of fighter pilot G tolerance using anthropometric and physiologic variables. Aviat. Space Environ. Med. 1991, 62, 128–135. [Google Scholar] [PubMed]
- Park, M.; Yoo, S.; Seol, H.; Kim, C.; Hong, Y. Unpredictability of fighter pilots’ G duration by anthropometric and physiological characteristics. Aerosp. Med. Hum. Perform. 2015, 86, 307–401. [Google Scholar] [CrossRef] [PubMed]
- Yun, C.; Oh, S.; Shin, Y.H. AGSM proficiency and depression are associated with success of high-G training in trainee pilots. Aerosp. Med. Hum. Perform. 2019, 90, 613–617. [Google Scholar] [CrossRef]
- Ministry of National Defense. Aviation physiology and high G training. In Manual of Aviation Medicine; Medical Affairs Bureau: Taipei, Taiwan, 2015; Volume 8, pp. 1–63. [Google Scholar]
- USAF. Fighter Aircrew Acceleration Training Program. Published 27 October 2019. Available online: https://static.e-publishing.af.mil/production/1/af_a3/publication/afman11-404/afman11-404.pdf (accessed on 23 October 2020).
- USAF. G Awareness for Aircrew. Published 17 October 2014. Available online: https://static.e-publishing.af.mil/production/1/af_a3_5/publication/afpam11-419/afpam11-419.pdf (accessed on 20 September 2020).
- Chovanec, L.; Gröpel, P. Effects of 8-week endurance and resistance training programmes on cardiovascular stress responses, life stress and coping. J. Sports Sci. 2020, 22, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Lamberts, R.P.; Swart, J.; Noakes, T.D.; Lambert, M.I. Changes in heart rate recovery after high-intensity training in well-trained cyclists. Eur. J. Appl. Physiol. 2009, 105, 705–713. [Google Scholar] [CrossRef]
- Pendergast, D.R.; Olszowka, A.; Farhi, L.E. Cardiovascular and pulmonary responses to increased acceleration forces during rest and exercise. Aviat. Space Environ. Med. 2012, 83, 488–495. [Google Scholar] [CrossRef] [PubMed]
- Newman, D.G.; Callister, R. Cardiovascular training effects in fighter pilots induced by occupational high G exposure. Aviat. Space Environ. Med. 2008, 70, 774–778. [Google Scholar] [CrossRef]
- Fisher, J.P.; Secher, N.H. Regulation of heart rate and blood pressure during exercise in humans. In Muscle and Exercise Physiology, 1st ed.; Zoladz, J.A., Ed.; Academic Press: London, UK, 2019; pp. 541–560. [Google Scholar]
- Lai, C.Y.; Tu, M.Y.; Chu, H.; Liu, C.C. Cardiac performance of cadets during the centrifuge with rapid onset rate [abstract]. Aerosp. Med. Hum. Perform. 2019, 90, 225. [Google Scholar]
- Cao, X.S.; Wang, Y.C.; Xu, L.; Yang, C.B.; Wang, B.; Geng, J.; Gao, Y.; Wu, Y.H.; Wang, X.Y.; Zhang, S.; et al. Visual symptoms and G-induced loss of consciousness in 594 Chinese Air Force aircrew--a questionnaire survey. Mil. Med. 2012, 177, 163–168. [Google Scholar] [CrossRef]
- Mizumoto, C. Relationship between + Gz tolerance and physical characteristics during gradual and rapid onset runs. Jpn. J. Aerosp. Environ. Med. 1998, 25, 37–47. [Google Scholar]
- Gowda, A.; Pipraiya, R.; Baburaj, V.P. Relationship of body fat with relaxed G tolerance. Ind. J. Aerosp. Med. 2013, 57, 9–13. [Google Scholar]
- Park, J.S.; Choi, J.; Kim, J.W.; Jeon, S.Y.; Kang, S. Effects of the optimal flexor/extensor ratio on G-tolerance. J. Phys. Ther. Sci. 2016, 28, 2660–2665. [Google Scholar]
- Shin, S.; Jee, H. ACTN-3 genotype, body composition, fitness, and +Gz tolerance in senior cadets. Aerosp. Med. Hum. Perform. 2019, 90, 1055–1060. [Google Scholar]
- Eiken, O.; Kölegärd, R.; Bergsten, E.; Grönkvist, M. G protection: Interaction of straining maneuvers and positive pressure breathing. Aviat. Space Environ. Med. 2007, 78, 392–398. [Google Scholar]
- Iwasaki, K.; Ogawa, Y.; Aoki, K.; Yanagida, R. Cerebral circulation during mild +Gz hypergrativy by short-arm human centrifuge. J. Appl. Physiol. (1985) 2012, 112, 266–271. [Google Scholar]
- Konishi, T.; Kurazumi, T.; Kato, T.; Takko, C.; Ogawa, Y.; Iwasaki, K.I. Changes in cerebral oxygen saturation and cerebral blood flow velocity under mild +Gz hypergravity. J. Appl. Physiol. (1985) 2019, 127, 190–197. [Google Scholar]
- Guo, H.; Tierney, N.; Schaller, F.; Raven, P.B.; Smith, S.A.; Shi, X. Cerebral autoregulation is preserved during orthostatic stress superimposed with systemic hypotension. J. Appl. Physiol. (1985) 2016, 100, 1785–1792. [Google Scholar]
- Bateman, W.A.; Jacobs, I.; Buick, F. Physical conditioning to enhance +Gz tolerance: Issues and current understanding. Aviat. Space Environ. Med. 2006, 77, 573–580. [Google Scholar]
| Variables | Pass (n = 829) | Fail (n = 44) | p Value |
|---|---|---|---|
| Age (years) | 23.53 ± 1.19 | 23.55 ± 0.66 | 0.920 |
| Height (cm) | 173.72 ± 5.32 | 174.11 ± 6.16 | 0.634 |
| Weight (kg) | 70.30 ± 8.58 | 66.09 ± 6.41 | 0.002 |
| BMI (kg/m2) | 23.27 ± 2.42 | 21.80 ± 1.78 | <0.001 |
| RGT (G) | <0.001 | ||
| ≥4.5 | 649 (78.29%) | 16 (36.36%) | |
| <4.5 | 180 (21.71%) | 28 (63.64%) | |
| SGT (G) | <0.001 | ||
| ≥6.5 | 794 (95.78%) | 28 (63.63%) | |
| <6.5 | 35 (4.22%) | 16 (36.37%) | |
| AGSM score | 0.023 | ||
| ≥8 | 750 (90.47%) | 35 (79.54%) | |
| <8 | 79 (9.53%) | 9 (20.46%) |
| Variables | Pass (n = 829) | Fail (n = 44) | p Value |
|---|---|---|---|
| HR at baseline (bpm) | 107.28 ± 17.37 | 116.09 ± 15.30 | 0.001 |
| Peak HR during 6G profile (bpm) | 168.45 ± 13.99 | 171.14 ± 11.95 | 0.211 |
| HR before 7.5G profile (bpm) | 137.61 ± 18.99 | 146.11 ± 21.04 | 0.004 |
| Peak HR during 1–5 s of 7.5G profile (bpm) | 181.11 ± 21.84 | 172.48 ± 27.51 | 0.012 |
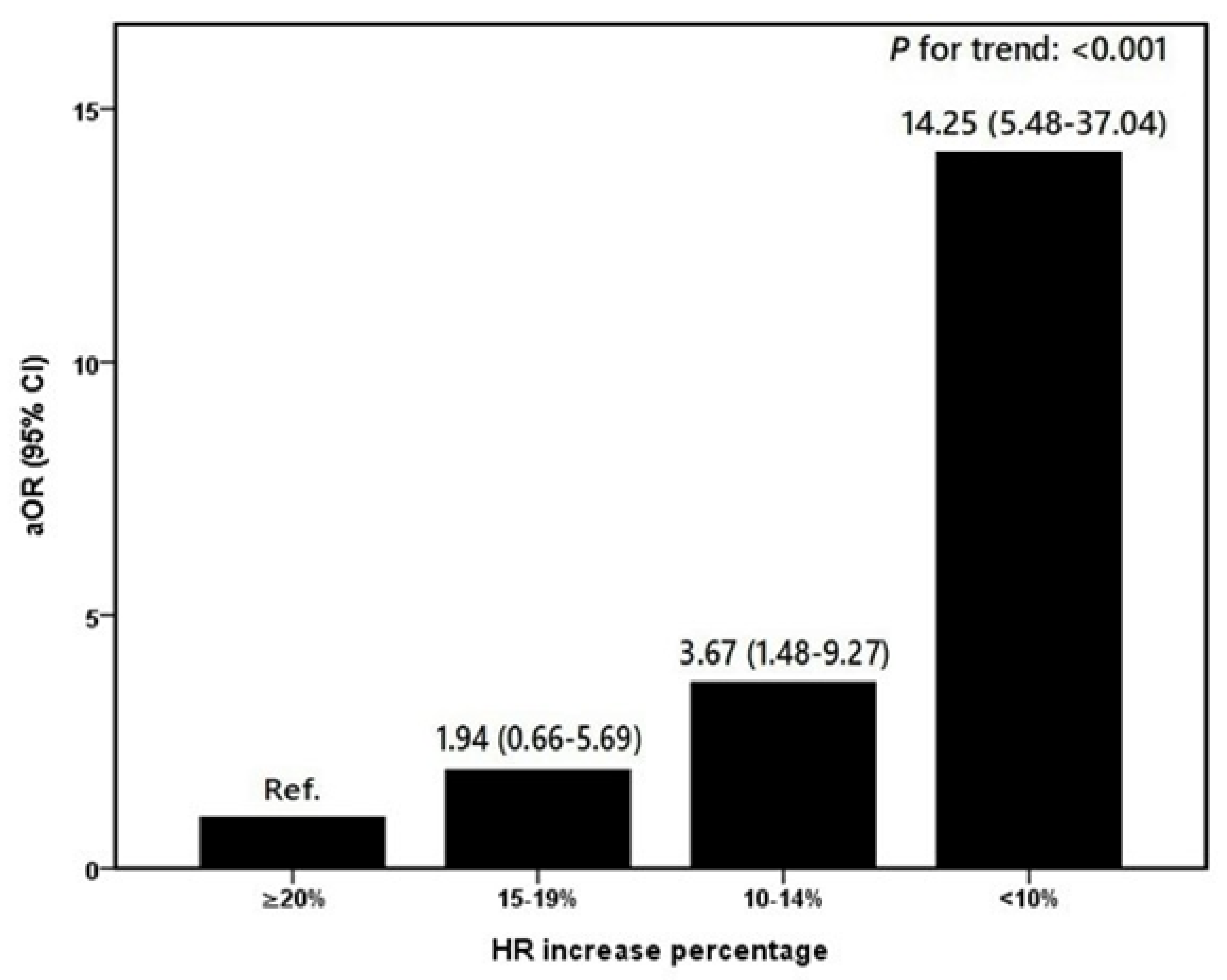
| HR increase percentage * | <0.001 | ||
| ≥10% | 798 (96.26%) | 31 (70.45%) | |
| <10% | 31 (3.74%) | 13 (29.55%) |
| Variables | Pass (n = 829) | Fail (n = 44) | β ± SE | aOR (95%CI) | p Value |
|---|---|---|---|---|---|
| Age (year) | 23.53 ± 1.19 | 23.55 ± 0.66 | 0.08 ± 0.18 | 1.08 (0.76–1.54) | 0.661 |
| BMI (kg/m2) | 23.27 ± 2.43 | 21.80 ± 1.78 | −0.23 ± 0.09 | 0.79 (0.66–0.95) | 0.010 |
| RGT (G) | |||||
| ≥4.5 | 649 (78.3%) | 16 (36.4%) | Ref. | ||
| <4.5 | 180 (21.7%) | 28 (63.6%) | 1.13 ± 0.37 | 3.08 (1.51–6.32) | 0.002 |
| SGT (G) | |||||
| ≥6.5 | 794 (95.78%) | 28 (63.63%) | Ref. | ||
| <6.5 | 35 (4.22%) | 16 (36.37%) | 1.93 ± 0.41 | 6.86 (3.08–15.25) | <0.001 |
| AGSM score | |||||
| ≥8 | 750 (90.47%) | 35 (79.54%) | Ref. | ||
| <8 | 79 (9.53%) | 9 (20.46%) | 0.73 ± 0.46 | 2.08 (0.84–5.13) | 0.112 |
| HR increase percentage * | |||||
| ≥10% | 798 (96.26%) | 31 (70.45%) | Ref. | ||
| <10% | 31 (3.74%) | 13 (29.55%) | 2.29 ± 0.45 | 9.91 (4.11–23.88) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tu, M.-Y.; Chu, H.; Chen, H.-H.; Chiang, K.-T.; Hu, J.-M.; Li, F.-L.; Yang, C.-S.; Cheng, C.-C.; Lai, C.-Y. Roles of Physiological Responses and Anthropometric Factors on the Gravitational Force Tolerance for Occupational Hypergravity Exposure. Int. J. Environ. Res. Public Health 2020, 17, 8061. https://doi.org/10.3390/ijerph17218061
Tu M-Y, Chu H, Chen H-H, Chiang K-T, Hu J-M, Li F-L, Yang C-S, Cheng C-C, Lai C-Y. Roles of Physiological Responses and Anthropometric Factors on the Gravitational Force Tolerance for Occupational Hypergravity Exposure. International Journal of Environmental Research and Public Health. 2020; 17(21):8061. https://doi.org/10.3390/ijerph17218061
Chicago/Turabian StyleTu, Min-Yu, Hsin Chu, Hsin-Hui Chen, Kwo-Tsao Chiang, Je-Ming Hu, Fang-Ling Li, Chen-Shu Yang, Chao-Chien Cheng, and Chung-Yu Lai. 2020. "Roles of Physiological Responses and Anthropometric Factors on the Gravitational Force Tolerance for Occupational Hypergravity Exposure" International Journal of Environmental Research and Public Health 17, no. 21: 8061. https://doi.org/10.3390/ijerph17218061
APA StyleTu, M.-Y., Chu, H., Chen, H.-H., Chiang, K.-T., Hu, J.-M., Li, F.-L., Yang, C.-S., Cheng, C.-C., & Lai, C.-Y. (2020). Roles of Physiological Responses and Anthropometric Factors on the Gravitational Force Tolerance for Occupational Hypergravity Exposure. International Journal of Environmental Research and Public Health, 17(21), 8061. https://doi.org/10.3390/ijerph17218061





