Effectiveness of Traditional Chinese Exercise for Symptoms of Knee Osteoarthritis: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
Abstract
1. Introduction
2. Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Study Selection
2.4. Data Extraction
2.5. Risk of Bias Assessment in Individual Trials
2.6. Statistical Analysis
3. Results
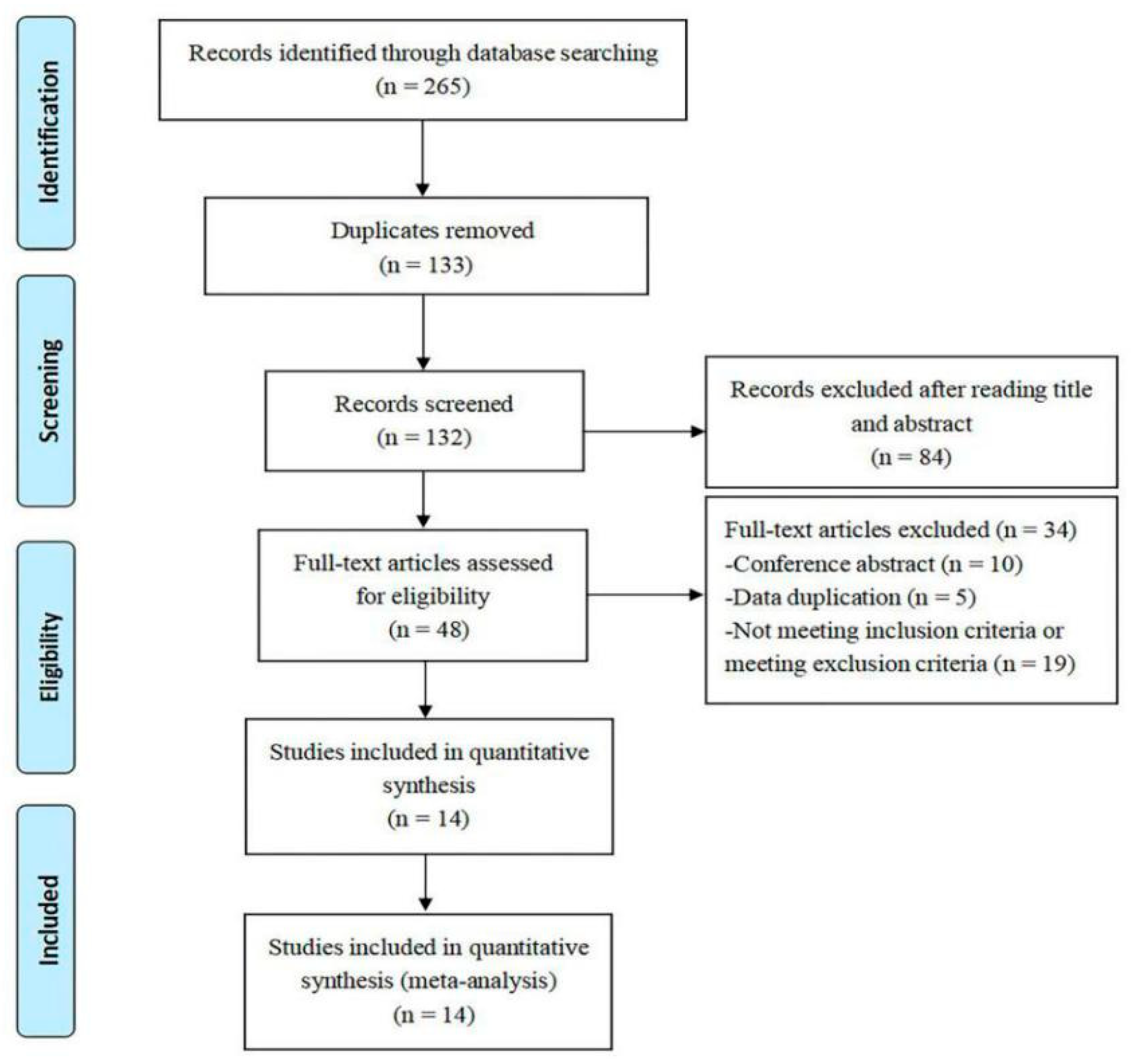
3.1. Study Selection
3.2. Study Characteristics
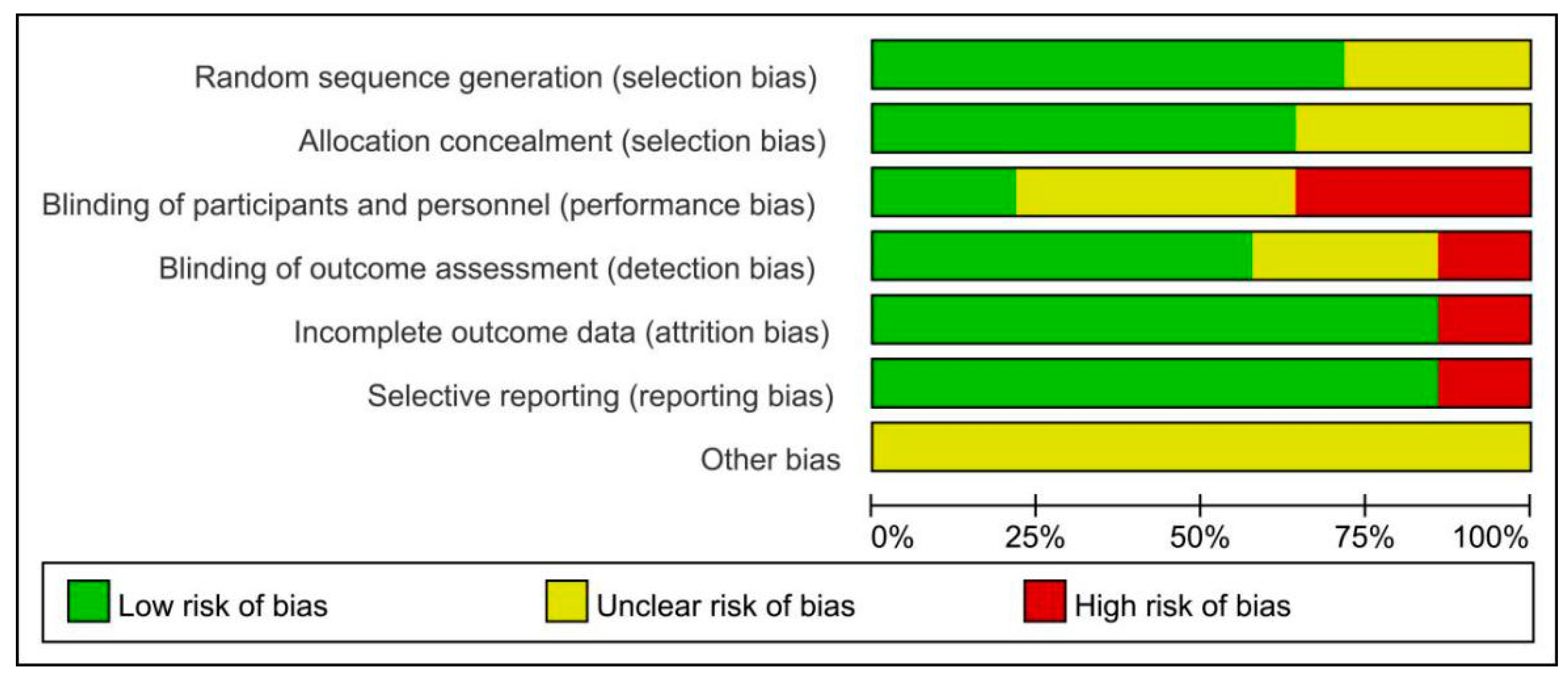
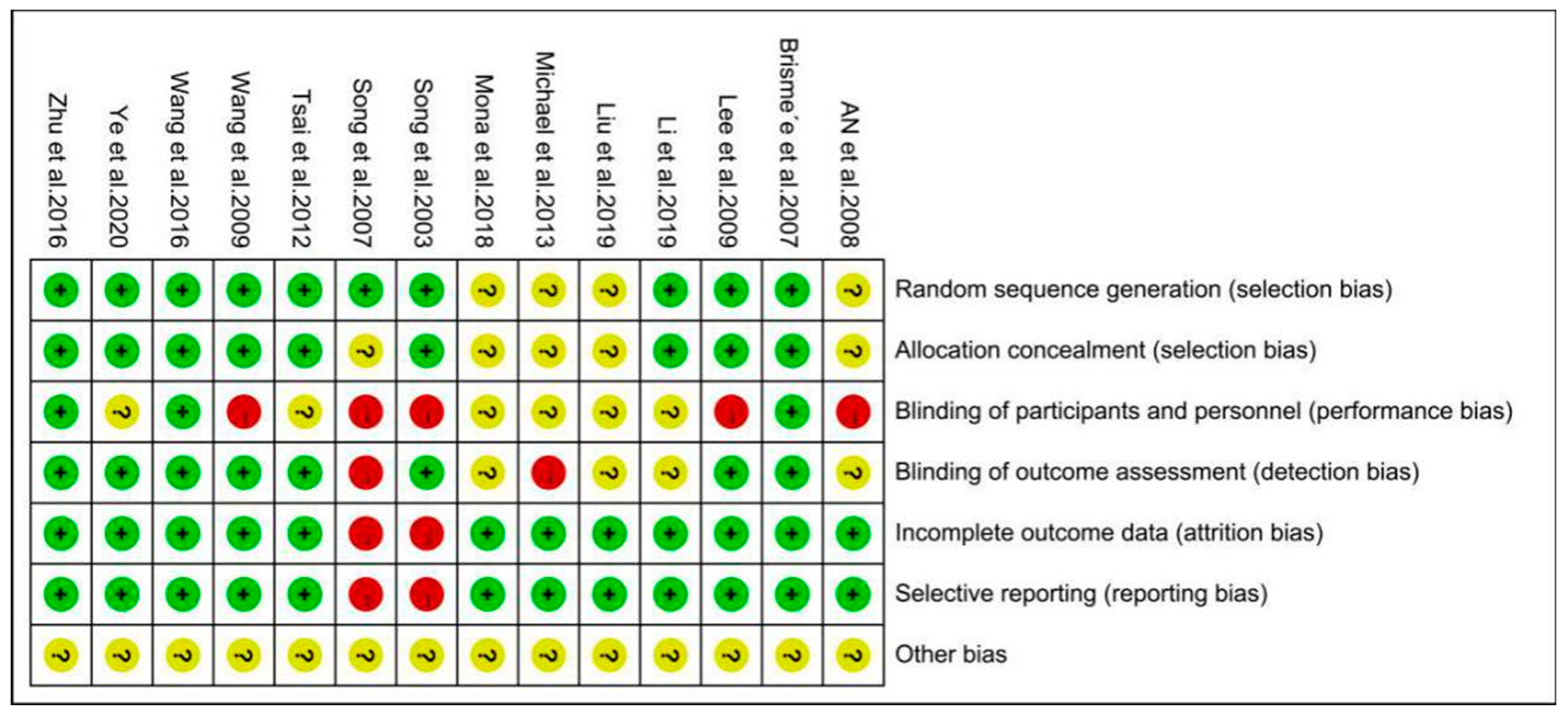
3.3. Assessment of Risk of Bias
3.4. Outcome Measures
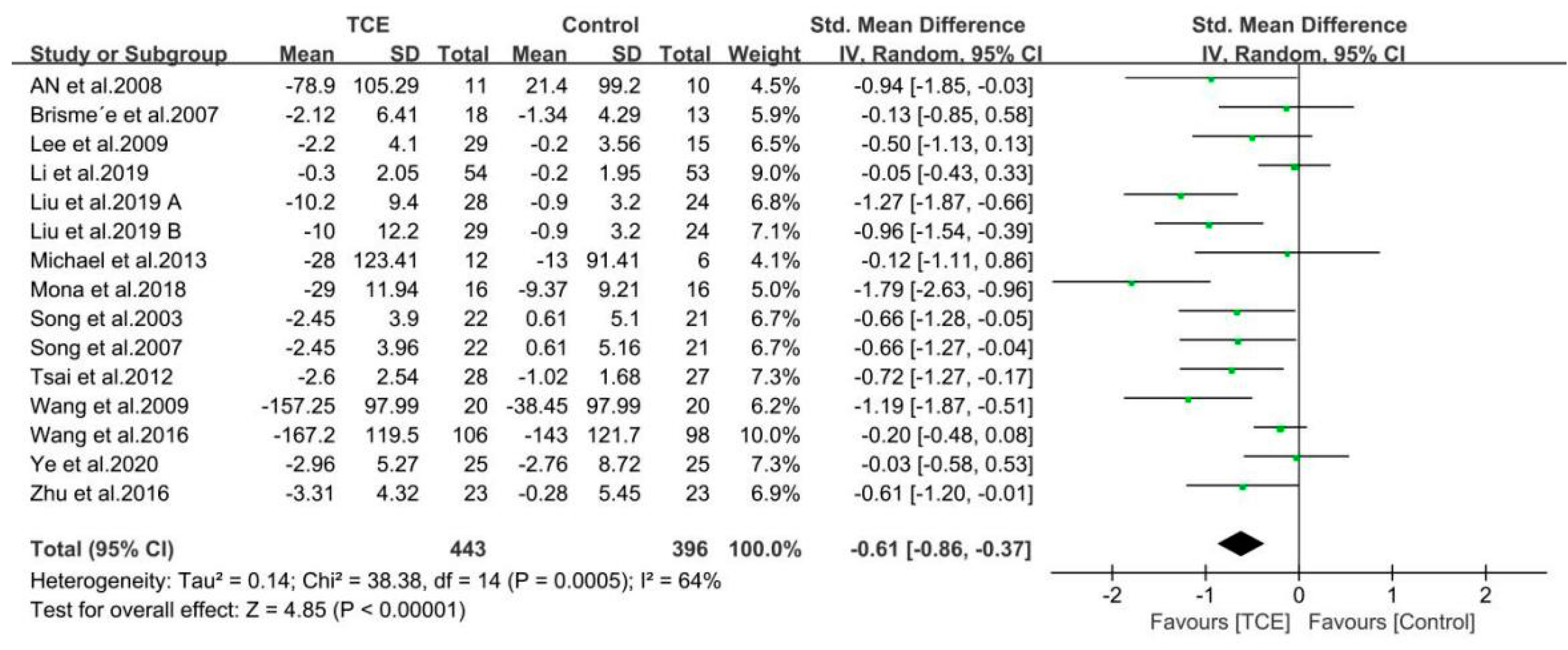
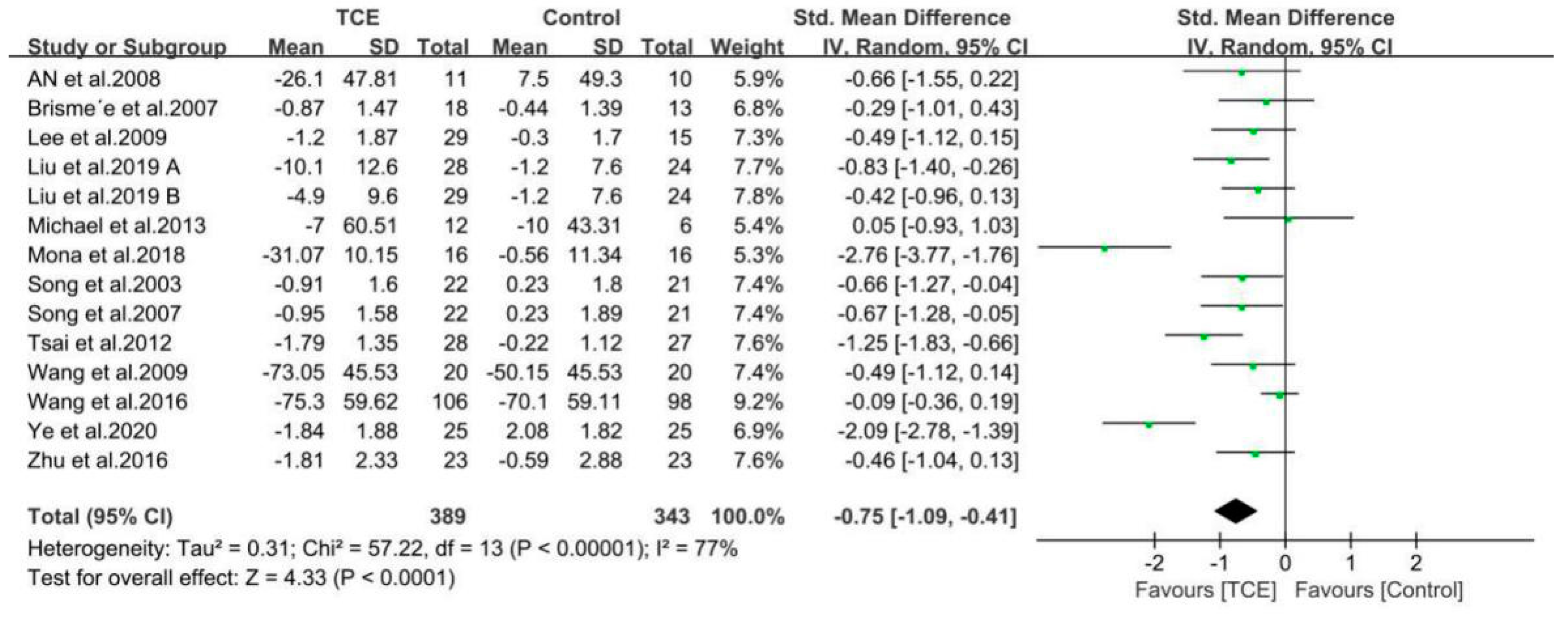
3.4.1. Pain
3.4.2. Stiffness
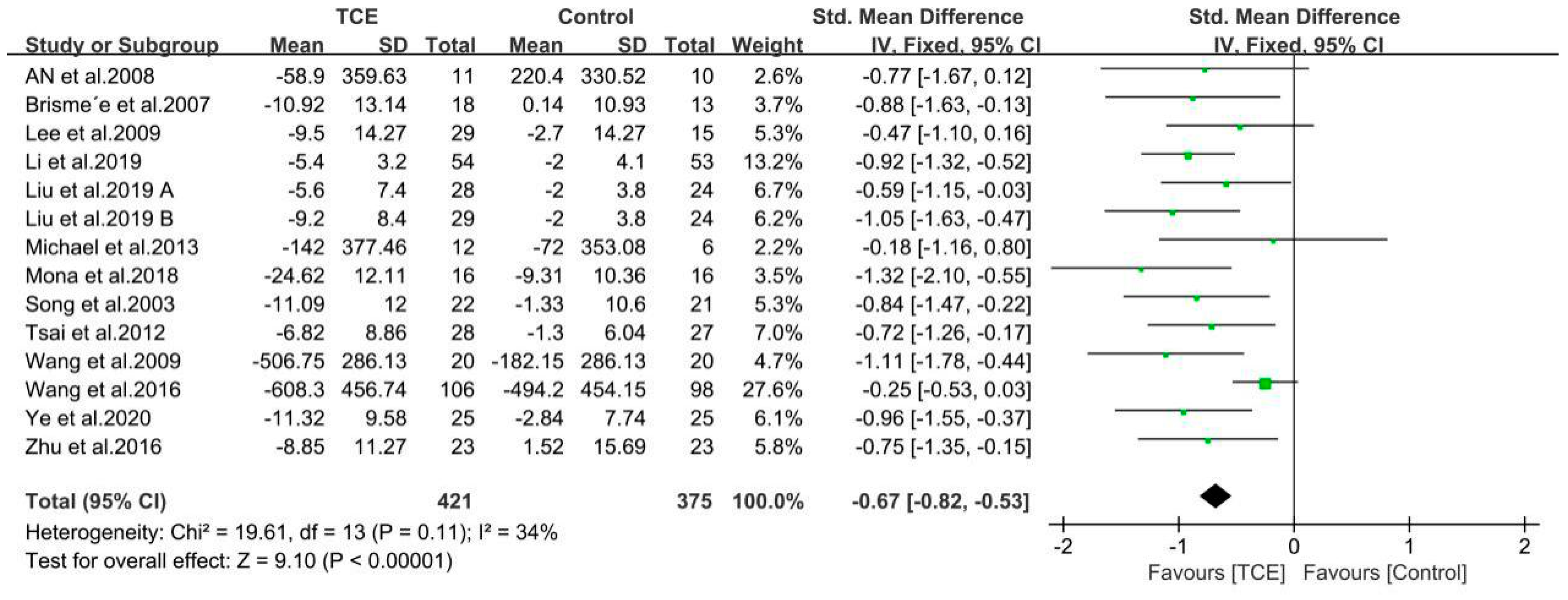
3.4.3. Physical Function
3.5. Evaluation of Publication Bias
3.6. Sensitivity Analysis and Subgroup Meta-Analyses
3.6.1. Sensitivity Analysis
3.6.2. Subgroup Meta-Analyses
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| AAOS | American Academy of Orthopedic Surgeons |
| ACR | American College of Rheumatology classification criteria |
| ACS | Autologous Conditioned Serum |
| ARA | American Rheumatism Association |
| CG | Control Group |
| CI | Confidence Interval |
| HA | Hyaluronic Acid |
| IG | Intervention Group |
| KL | the Kellgren Lawrence classification |
| KOA | Knee Osteoarthritis |
| KOOS | the Knee Injury and Osteoarthritis Outcome Score |
| MSC | Mesenchymal Stem Cell |
| NSAIDs | Non-Steroidal Anti-Inflammatory Drugs |
| OARSI | Osteoarthritis Research Society International |
| PRP | Platelet-Rich Plasma |
| RCT | Randomized Controlled Trial |
| SMD | Standardized Mean Difference |
| TCE | TCE |
| WMD | Weighted Mean Difference |
| WOMAC | the Western Ontario and McMaster Universities Osteoarthritis Index |
References
- World Health Organization (WHO). Chronic Diseases and Health Promotion: Chronic Rheumatic Conditions; World Health Organization: Geneva, Switzerland, 2020; Available online: https://www.who.int/chp/topics/rheumatic/en/ (accessed on 20 October 2020).
- Francisco, V.; Pérez, T.; Pino, J.; López, V.; Franco, E.; Alonso, A.; Gonzalez-Gay, M.A.; Mera, A.; Lago, F.; Gómez, R.; et al. Biomechanics, obesity, and osteoarthritis. The role of adipokines: When the levee breaks. J. Orthop. Res. 2018, 36, 594–604. [Google Scholar] [CrossRef] [PubMed]
- Bennell, K.L.; Hunter, D.J.; Paterson, K.L. Platelet-Rich Plasma for the Management of Hip and Knee Osteoarthritis. Curr. Rheumatol. Rep. 2017, 19, 24. [Google Scholar] [CrossRef] [PubMed]
- Kolasinski, S.L.; Neogi, T.; Hochberg, M.C.; Oatis, C.; Guyatt, G.; Block, J.; Callahan, L.; Copenhaver, C.; Dodge, C.; Felson, D.; et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Management of Osteoarthritis of the Hand, Hip, and Knee. Arthritis Rheumatol. 2020, 2, 220–233. [Google Scholar] [CrossRef] [PubMed]
- Lin, K.W. Treatment of Knee Osteoarthritis. Am. Fam. Physician 2018, 98, 603–606. [Google Scholar] [PubMed]
- Silva, G.S.; Sullivan, J.K.; Katz, J.N.; Messier, S.P.; Hunter, D.J.; Losina, E. Long-term clinical and economic outcomes of a short-term physical activity program in knee osteoarthritis patients. Osteoarthr. Cartil. 2020, 28, 735–743. [Google Scholar] [CrossRef] [PubMed]
- Aweid, O.; Haider, Z.; Saed, A.; Kalairajah, Y. Treatment modalities for hip and knee osteoarthritis: A systematic review of safety. J. Orthop. Surg. 2018, 26, 2309499018808669. [Google Scholar] [CrossRef]
- Kucharz, E.J.; Szántó, S.; Goycheva, M.I.; Petronijević, M.; Šimnovec, K.; Domżalski, M.; Gallelli, L.; Kamenov, Z.; Konstantynowicz, J.; Radunović, G.; et al. Endorsement by Central European experts of the revised ESCEO algorithm for the management of knee osteoarthritis. Rheumatol. Int. 2019, 39, 1117–1123. [Google Scholar] [CrossRef]
- Zhao, J.L.; Huang, H.T.; Liang, G.H.; Zeng, L.F.; Yang, W.Y.; Liu, J. Effects and safety of the combination of platelet-rich plasma (PRP) and hyaluronic acid (HA) in the treatment of knee osteoarthritis: A systematic review and meta-analysis. BMC Musculoskelet. Disord. 2020, 21, 224. [Google Scholar] [CrossRef]
- Vitali, M.; Ometti, M.; Drossinos, A.; Pironti, P.; Santoleri, L.; Salini, V. Autologous conditioned serum: Clinical and functional results using a novel disease modifying agent for the management of knee osteoarthritis. J. Drug Assess. 2020, 9, 43–51. [Google Scholar] [CrossRef]
- Lopa, S.; Colombini, A.; Moretti, M.; Girolamo, L.D. Injective mesenchymal stem cell-based treatments for knee osteoarthritis: From mechanisms of action to current clinical evidences. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 2003–2020. [Google Scholar] [CrossRef]
- Jung, S.Y.; Jang, E.J.; Nam, S.W.; Kwon, H.H.; Im, S.G.; Kim, D.; Cho, S.K.; Kim, D.; Sung, Y.K. Comparative effectiveness of oral pharmacologic interventions for knee osteoarthritis: A network meta-analysis. Mod. Rheumatol. 2018, 28, 1021–1028. [Google Scholar] [CrossRef]
- Sharif, B.; Garner, R.; Hennessy, D.; Sanmartin, C.; Flanagan, W.M.; Marshall, D.A. Productivity costs of work loss associated with osteoarthritis in Canada from 2010 to 2031. Osteoarthr. Cartil. 2017, 25, 249–258. [Google Scholar] [CrossRef]
- Park, H.M.; Kim, H.S.; Lee, Y.J. Knee osteoarthritis and its association with mental health and health-related quality of life: A nationwide cross-sectional study. Geriatr. Gerontol. Int. 2020, 20, 379–383. [Google Scholar] [CrossRef]
- DeRogatis, M.; Anis, H.K.; Sodhi, N.; Ehiorobo, J.O.; Chughtai, M.; Bhave, A.; Mont, M.A. Non-operative treatment options for knee osteoarthritis. Ann. Transl. Med. 2019, 7. [Google Scholar] [CrossRef] [PubMed]
- Bannuru, R.R.; Osani, M.C.; Vaysbrot, E.E.; Arden, N.K.; Bennell, K.; Bierma-Zeinstra, S.M.A.; Kraus, V.B.; Lohmander, L.S.; Abbott, J.H.; Bhandari, M.; et al. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthr. Cartil. 2019, 27, 1578–1589. [Google Scholar] [CrossRef] [PubMed]
- Meiyappan, K.P.; Cote, M.P.; Bozic, K.J.; Halawi, M.J. Adherence to the American Academy of Orthopaedic Surgeons Clinical Practice Guidelines for Nonoperative Management of Knee Osteoarthritis. J. Arthroplast. 2020, 35, 347–352. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.J.; Huang, L.L.; Su, Y.X.; Zhan, Z.G.; Li, Y.N.; Lai, X.Q. The Effects of Traditional Chinese Exercise in Treating Knee Osteoarthritis: A Systematic Review and Meta-Analysis. PLoS ONE 2017, 12, e0170237. [Google Scholar] [CrossRef]
- Koh, T.C. Baduanjin-an ancient Chinese exercise. Am. J. Chin. Med. 1982, 10, 14–21. [Google Scholar] [CrossRef]
- Guo, Y.; Xu, M.M.; Wei, Z.R.; Hu, Q.C.; Chen, Y.; Yan, J.; Wei, Y.L. Beneficial Effects of Qigong Wuqinxi in the Improvement of Health Condition, Prevention, and Treatment of Chronic Diseases: Evidence from a Systematic Review. Evid. Based Complement. Altern. Med. 2018, 2018. [Google Scholar] [CrossRef]
- Wang, X.Q.; Pi, Y.L.; Chen, B.L.; Chen, P.J.; Liu, Y.; Wang, R.; Li, X.; Zhu, Y.; Yang, Y.J.; Niu, Z.B. Effect of traditional Chinese exercise on the quality of life and depression for chronic diseases: A meta-analysis of randomised trials. Sci. Rep. 2015, 5, 15913. [Google Scholar] [CrossRef]
- Zeng, Z.P.; Liu, Y.B.; Fang, J.J.; Liu, Y.; Luo, J.; Yang, M. Effects of Baduanjin exercise for knee osteoarthritis: A systematic review and meta-analysis. Complement. Ther. Med. 2020, 48. [Google Scholar] [CrossRef] [PubMed]
- Palermi, S.; Sacco, A.M.; Belviso, I.; Marino, N.; Gambardella, F.; Loiacono, C.; Sirico, F. Effectiveness of Tai Chi on Balance Improvement in Type 2 Diabetes Patients: A Systematic Review and Meta-Analysis. J. Aging Phys. Act. 2020. [Google Scholar] [CrossRef] [PubMed]
- Zou, L.Y.; Zhang, Y.J.; Sasaki, J.E.; Zou, L.Y.; Zhang, Y.J.; Sasaki, J.E.; Yeung, A.S.; Yang, L.; Loprinzi, P.D.; Sun, J.; et al. Wuqinxi Qigong as an Alternative Exercise for Improving Risk Factors Associated with Metabolic Syndrome: A Meta-Analysis of Randomized Controlled Trials. Int. J. Environ. Res. Public Health 2019, 16, 1396. [Google Scholar] [CrossRef] [PubMed]
- Fidan, O.; Seyyar, G.K.; Aras, B.; Colak, E.; Aras, O. The effect of Tai Chi and Qigong on health-related quality of life in Parkinson’s disease: A systematic review and meta-analysis of systematic reviews. Int. J. Rehabil. Res. 2019, 42, 196–204. [Google Scholar] [CrossRef]
- Wu, B.X.; Ding, Y.N.; Zhong, B.Y.; Jin, X.; Cao, Y.T.; Xu, D.P. Intervention Treatment for Myocardial Infarction with Tai Chi: A Systemic Review and Meta-Analysis. Arch. Phys. Med. Rehabil. 2020. [Google Scholar] [CrossRef] [PubMed]
- Reychler, G.; Poncin, W.; Montigny, S.; Luts, A.; Caty, G.; Pieters, T. Efficacy of yoga, tai chi and qi gong on the main symptoms of chronic obstructive pulmonary disease: A systematic review. Respir. Med. Res. 2019, 75, 13–25. [Google Scholar] [CrossRef]
- Ding, M.; Wang, C.Y.; Dong, X.S.; Yi, X.R. The Effects of Qigong on Type 2 Diabetes Mellitus: A Systematic Review and Meta-Analysis. Evid. Based Complement. Altern. Med. 2018, 2018. [Google Scholar] [CrossRef]
- Zou, L.Y.; Zhang, Y.J.; Yang, L.; Loprinzi, P.D.; Yeung, A.S.; Kong, J.; Chen, K.W.; Song, W.; Xiao, T.; Li, H. Are Mindful Exercises Safe and Beneficial for Treating Chronic Lower Back Pain? A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Clin. Med. 2019, 8, 628. [Google Scholar] [CrossRef]
- Zeng, Y.C.; Xie, X.H.; Cheng, A.S.K. Qigong or Tai Chi in Cancer Care: An Updated Systematic Review and Meta-analysis. Curr. Oncol. Rep. 2019, 21, 48. [Google Scholar] [CrossRef]
- Ge, L.; Zheng, Q.X.; Liao, Y.T.; Tan, J.Y.; Xie, Q.L.; Rask, M. Effects of traditional Chinese exercises on the rehabilitation of limb function among stroke patients: A systematic review and meta-analysis. Complement. Ther. Clin. Pract. 2017, 29, 35–47. [Google Scholar] [CrossRef]
- Lauche, R.; Langhorst, J.; Dobos, G.; Cramer, H. A systematic review and meta-analysis of Tai Chi for osteoarthritis of the knee. Complement. Ther. Med. 2013, 21, 396–406. [Google Scholar] [CrossRef]
- Wang, C.C.; Schmid, C.H.; Iversen, M.D.; Harvey, W.F.; Fielding, R.A.; Driban, J.B.; Price, L.L.; Wong, J.B.; Reid, K.F.; Rones, R.; et al. Comparative Effectiveness of Tai Chi Versus Physical Therapy for Knee Osteoarthritis: A Randomized Trial. Ann. Intern. Med. 2016, 165, 77–86. [Google Scholar] [CrossRef] [PubMed]
- Ye, J.J.; Simpson, M.W.; Liu, Y.; Lin, W.; Zhong, W.H.; Cai, S.H.; Zou, L.Y. The Effects of Baduanjin Qigong on Postural Stability, Proprioception, and Symptoms of Patients with Knee Osteoarthritis: A Randomized Controlled Trial. Front. Med. 2020, 6, 307. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Q.G.; Huang, L.Y.; Wu, X.; Wang, L.; Zhang, Y.Y.; Fang, M.; Liu, Y.; Li, J.X. Effects of Tai Ji Quan training on gait kinematics in older Chinese women with knee osteoarthritis: A randomized controlled trial. J. Sport Health Sci. 2016, 5, 297–303. [Google Scholar] [CrossRef]
- Lee, H.J.; Park, H.J.; Chae, Y.; Kim, S.Y.; Kim, S.N.; Kim, S.T.; Kim, J.H.; Yin, C.S.; Lee, H. Tai Chi Qigong for the quality of life of patients with knee osteoarthritis: A pilot, randomized, waiting list controlled trial. Clin. Rehabil. 2009, 23, 504–511. [Google Scholar] [CrossRef] [PubMed]
- Wortley, M.; Zhang, S.N.; Paquette, M.; Byrd, E.; Baumgartner, L.; Klipple, G.; Krusenklaus, J.; Brown, L. Effects of resistance and Tai Ji training on mobility and symptoms in knee osteoarthritis patients. J. Sport Health Sci. 2013, 2, 209–214. [Google Scholar] [CrossRef]
- Shamseer, L.; Moher, D.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: Elaboration and explanation. BMJ 2015, 350, 1. [Google Scholar] [CrossRef]
- Damen, J.; Rijn, R.M.V.; Emans, P.J.; Hilberdink, W.K.H.A.; Wesseling, J.; Oei, E.H.G.; Bierma-Zeinstra, S.M.A. Prevalence and development of hip and knee osteoarthritis according to American College of Rheumatology criteria in the CHECK cohort. Arthritis Res. Ther. 2019, 21, 4. [Google Scholar] [CrossRef]
- Altman, R.; Asch, E.; Bloch, D.; Bole, G.; Borenstein, D.; Brandt, K.; Christy, W.; Cooke, T.D.; Greenwald, R.; Hochberg, M.; et al. Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association. Arthritis Rheumatol. 1986, 29, 1039–1049. [Google Scholar] [CrossRef]
- Schiphof, D.; Klerk, B.M.D.; Kerkhof, H.J.M.; Hofman, A.; Koes, B.W.; Boers, M.; Bierma-Zeinstra, S.M.A. Impact of different descriptions of the Kellgren and Lawrence classification criteria on the diagnosis of knee osteoarthritis. Ann. Rheum. Dis. 2011, 70, 1422–1427. [Google Scholar] [CrossRef]
- Gandek, B. Measurement properties of the Western Ontario and McMaster Universities Osteoarthritis Index: A systematic review. Arthritis Care Res. 2015, 67, 216–229. [Google Scholar] [CrossRef] [PubMed]
- Collins, N.J.; Prinsen, C.A.C.; Christensen, R.; Bartels, E.M.; Terwee, C.B.; Roos, E.M. Knee Injury and Osteoarthritis Outcome Score (KOOS): Systematic review and meta-analysis of measurement properties. Osteoarthr. Cartil. 2016, 24, 1317–1329. [Google Scholar] [CrossRef] [PubMed]
- Guo, L.J.; Kong, Z.W.; Zhang, Y.J. Qigong-Based Therapy for Treating Adults with Major Depressive Disorder: A Meta-Analysis of Randomized Controlled Trials. Int. J. Environ. Res. Public Health 2019, 16, 826. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Altman, D.G.; Sterne, J.A.C. Chapter 8: Assessing risk of bias in included studies. In Cochrane Handbook for Systematic Reviews of Interventions; Version 5.1.0; Higgins, J.P.T., Green, S., Eds.; The Cochrane Collaboration: London, UK, 2011; Available online: www.cochrane-handbook.org (accessed on 20 October 2020).
- Deeks, J.J.; Higgins, J.P.T.; Altman, D.G. Chapter 9: Analysing data and undertaking Meta-analyses. In Cochrane Handbook for Systematic Reviews of Interventions; Version 5.1.0; Higgins, J.P.T., Green, S., Eds.; The Cochrane Collaboration: London, UK, 2011; Available online: www.cochrane-handbook.org (accessed on 20 October 2020).
- Riley, R.D.; Higgins, J.P.; Deeks, J.J. Interpretation of random effects meta-analyses. BMJ 2011, 10, 342–549. [Google Scholar] [CrossRef] [PubMed]
- An, B.C.; Dai, K.R.; Zhu, Z.A.; Wang, Y.; Hao, Y.Q.; Tang, T.T.; Yan, H.Q. Baduanjin alleviates the symptoms of knee osteoarthritis. J. Altern. Complement. Med. 2008, 14, 167–174. [Google Scholar] [CrossRef]
- Brismée, J.M.; Paige, R.L.; Chyu, M.C.; Boatright, J.D.; Hagar, J.M.; McCaleb, J.A.; Quintela, M.M.; Feng, D.; Xu, K.T.; Shen, C.L. Group and home-based tai chi in elderly subjects with knee osteoarthritis: A randomized controlled trial. Clin. Rehabil. 2007, 21, 99–111. [Google Scholar] [CrossRef]
- Li, L.T.; Cheng, S.H.; Wang, G.D.; Duan, G.Q.; Zhang, Y.M. Tai chi chuan exercises improve functional outcomes and quality of life in patients with primary total knee arthroplasty due to knee osteoarthritis. Complement. Ther. Clin. Pract. 2019, 35, 121–125. [Google Scholar] [CrossRef]
- Liu, J.; Chen, L.D.; Chen, X.L.; Hu, K.; Tu, Y.X.; Lin, M.Q.; Huang, J.; Liu, W.L.; Wu, J.S.; Qiu, Z.J.; et al. Modulatory effects of different exercise modalities on the functional connectivity of the periaqueductal grey and ventral tegmental area in patients with knee osteoarthritis: A randomised multimodal magnetic resonance imaging study. Br. J. Anaesth. 2019, 123, 506–518. [Google Scholar] [CrossRef]
- Nahayatbin, M.; Ghasemi, M.; Rahimi, A.; Khademi, K.; Naimi, S.; Tabatabaee, S.M.; Zarein, D.S. The Effects of Routine Physiotherapy Alone and in Combination with Either Tai Chi or Closed Kinetic Chain Exercises on Knee Osteoarthritis: A Comparative Clinical Trial Study. Iran. Red Crescent Med. J. 2018, 20. [Google Scholar] [CrossRef]
- Song, R.; Lee, E.O.; Lam, P.; Bae, S.C. Effects of tai chi exercise on pain, balance, muscle strength, and perceived difficulties in physical functioning in older women with osteoarthritis: A randomized clinical trial. J. Rheumatol. 2003, 30, 2039–2044. [Google Scholar]
- Song, R.; Lee, E.O.; Lam, P.; Bae, S.C. Effects of a Sun-style Tai Chi exercise on arthritic symptoms, motivation and the performance of health behaviors in women with osteoarthritis. J. Korean Acad. Nurs. 2007, 37, 249–256. [Google Scholar] [CrossRef]
- Tsai, P.F.; Chang, J.Y.; Beck, C.; Kuo, Y.F.; Keefe, F.J. A pilot cluster-randomized trial of a 20-week Tai Chi program in elders with cognitive impairment and osteoarthritic knee: Effects on pain and other health outcomes. J. Pain Symptom Manag. 2013, 45, 660–669. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.C.; Schmid, C.H.; Hibberd, P.L.; Kalish, R.; Roubenoff, R.; Rones, R.; McAlindon, T. Tai Chi is effective in treating knee osteoarthritis: A randomized controlled trial. Arthritis Rheumatol. 2009, 61, 1545–1553. [Google Scholar] [CrossRef] [PubMed]
- Mora, J.C.; Przkora, R.; Cruz-Almeida, Y. Knee osteoarthritis: Pathophysiology and current treatment modalities. J. Pain Res. 2018, 11, 2189–2196. [Google Scholar] [CrossRef] [PubMed]
- Richebé, P.; Capdevila, X.; Rivat, C. Persistent Postsurgical Pain: Pathophysiology and Preventative Pharmacologic Considerations. Anesthesiology. 2018, 129, 590–607. [Google Scholar] [CrossRef]
- Heidari, B. Knee osteoarthritis prevalence, risk factors, pathogenesis and features: Part I. Casp. J. Intern. Med. 2011, 2, 205–212. [Google Scholar]
- Andriacchi, T.P.; Favre, J.; Erhart-Hledik, J.C.; Chu, C.R. A systems view of risk factors for knee osteoarthritis reveals insights into the pathogenesis of the disease. Ann. Biomed. Eng. 2015, 43, 376–387. [Google Scholar] [CrossRef]
- Oo, W.M.; Liu, X.Q.; Hunter, D.J. Pharmacodynamics, efficacy, safety and administration of intra-articular therapies for knee osteoarthritis. Expert Opin. Drug Metab. Toxicol. 2019, 15, 1021–1032. [Google Scholar] [CrossRef]
- Hiligsmann, M.; Cooper, C.; Arden, N.; Boers, M.; Branco, J.C.; Brandi, M.L.; Bruyère, O.; Guillemin, F.; Hochberg, M.C.; Hunter, D.J.; et al. Health economics in the field of osteoarthritis: An expert’s consensus paper from the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO). Semin. Arthritis Rheum. 2013, 43, 303–313. [Google Scholar] [CrossRef]
- Liu, B.Y.; Fan, Z.; Wang, Z.Y.; Li, M.; Lu, T. The efficacy and safety of Health Qigong for ankylosing spondylitis: Protocol for a systematic review and meta-analysis. Medicine 2020, 99. [Google Scholar] [CrossRef]
- Lu, M.L.; Su, Y.X.; Zhang, Y.J.; Zhang, Z.Y.; Wang, W.T.; He, Z.; Liu, F.W.; Li, Y.N.; Liu, C.Y.; Wang, Y.R.; et al. Effectiveness of aquatic exercise for treatment of knee osteoarthritis: Systematic review and meta-analysis. Z. Rheumatol. 2015, 74, 543–552. [Google Scholar] [CrossRef] [PubMed]
- Fransen, M.; Nairn, L.; Winstanley, J.; Lam, P.; Edmonds, J. Physical activity for osteoarthritis management: A randomized controlled clinical trial evaluating hydrotherapy or Tai Chi classes. Arthritis Care Res. 2007, 57, 407–414. [Google Scholar] [CrossRef] [PubMed]
- Ni, G.X.; Song, L.; Yu, B.; Huang, C.H.; Lin, J.H. Tai chi improves physical function in older Chinese women with knee osteoarthritis: Retraction. J. Clin. Rheumatol. 2010, 16, 64–67. [Google Scholar] [CrossRef] [PubMed]
- Wu, Q.; Yao, X.; Chen, H.; Liu, Z.; Li, T.; Fan, X.; Zhang, G.; Yu, L.; Chen, M.; Xu, C.; et al. Long-term aspirin use for primary cancer prevention: An updated systematic review and subgroup meta-analysis of 29 randomized clinical trials. J. Cancer 2020, 11, 6460–6473. [Google Scholar] [CrossRef]
- Chen, H.; Yao, X.; Li, T.; Lam, C.W.; Zhang, R.; Zhang, H.; Wang, J.; Zhang, W.; Leung, E.L.; Wu, Q. Compound Kushen injection combined with platinum-based chemotherapy for stage III/IV non-small cell lung cancer: A meta-analysis of 37 RCTs following the PRISMA guidelines. J. Cancer 2020, 11, 1883–1898. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Yao, X.; Li, T.; Lam, C.W.; Zhang, R.; Zhang, H.; Wang, J.; Zhang, W.; Leung, E.L.; Wu, Q. Compound Kushen injection plus platinum-based chemotherapy for stage IIIB/IV non-small cell lung cancer: A protocol for meta-analysis of randomized clinical trials following the PRISMA guidelines. Medicine 2019, 98. [Google Scholar] [CrossRef]
- Wu, Q.; Chen, H.; Yao, X.; Li, T.; Xu, C.; Wang, J.; Sui, X.; Leung, E.L. Long-term aspirin use for cancer primary prevention: A protocol for updated systematic review and subgroup meta-analysis of randomized clinical trials. Medicine 2019, 98. [Google Scholar] [CrossRef]

| Reference | Study Location | Participant Characteristics | Intervention Protocol | Outcomes Measure | Adverse Effects | ||||
|---|---|---|---|---|---|---|---|---|---|
| Patients Diagnostic Criteria | Sample Size (IG/CG) | Mean Age or Age Range | Intervention Group | Control Group | Duration Time | ||||
| AN et al., 2008 [48] | Shanghai, China | ACR | 11/10 | IG:65.4 ± 8.2 CG:64.6 ± 6.7 | Baduanjin 5 × 30 min/week | None | 8 weeks | WOMAC a. Pain b. Stiffness c. Physical function | No adverse event |
| Brisme’e et al., 2007 [49] | Texas, USA | ARA | 18/13 | IG:70.8 ± 9.8 CG:68.8 ± 8.9 | Tai Chi 3 × 40 min/week | Attention control pre-6 weeks 3 × 40 min/week post-6 weeks no attend activity | 12 weeks | WOMAC a. Pain b. Stiffness c. Physical function | No adverse event |
| Lee et al., 2009 [36] | Hwaseong, Korea | KL scale | 29/15 | IG:70.2 ± 4.8 CG:66.9 ± 6.0 | Tai Chi 2 × 60 min/week | None | 8 weeks | WOMAC a. Pain b. Stiffness c. Physical function | No adverse event |
| Li et al., 2019 [50] | Jining, China | Radiographic evidence | 54/53 | IG:69.6 ± 4.3 CG:68.5 ± 3.5 | Tai Chi 5 × 45 min/week | Traditional physical exercises 5 × 45 min/week | 12 weeks | WOMAC a. Pain b. Physical function | No adverse event |
| Liu et al., 2019 [51] | Fujian, China | ARA | 1.28/24 2.29/24 | IG1:40–70 IG2:40–68 CG:40–70 | 1: Tai Chi 5 × 60 min/week 2: Baduanjin 5 × 60 min/week | Healthy education 1 × 60 min/week | 12 weeks | KOOS a. Pain b. Symptoms c. Daily living | No adverse event |
| Michael et al., 2013 [37] | Knoxville, USA | ACR | 12/6 | IG:68.1 ± 5.3 CG:70.5 ± 5.0 | Tai Chi 5 × 60 min/week | Not intervention | 10 weeks | WOMAC a. Pain b. Stiffness c. Physical function | No adverse event |
| Mona et al., 2018 [52] | Tehran, Iran | KL scale | 16/16 | IG:55.25 ± 5.72 CG:56.06 ± 6.13 | Tai Chi 12 × 45 min/4 week and Routin physiotherapy 12 × 20 min/4 week | Routine physiotherapy 12 × 20 min/4 week | 4 weeks | KOOS a. Pain b. Symptoms c. Daily living | No adverse event |
| Song et al., 2003 [53] | Seoul, Korea | ACR | 22/21 | IG:64.8 ± 6.0 CG:62.5 ± 5.6 | Tai Chi pre-2 weeks 3 × 20 min/week post-10 weeks 3 × 20 min/week | None | 12 weeks | WOMAC a. Pain b. Stiffness c. Physical function | No adverse event |
| Song et al., 2007 [54] | Seoul, Korea | Radiographic evidence | 22/21 | IG:64.8 ± 6.0 CG:62.5 ± 5.6 | Tai Chi pre-2 weeks 3 × 60 min/week post-10 weeks 3 × 60 min/week | None | 12 weeks | WOMAC a. Pain b. Stiffness | No adverse event |
| Tsai et al., 2012 [55] | Arkansas, USA | health care provider | 28/27 | IG:78.89 ± 6.91 CG:78.93 ± 8.30 | Tai Chi 3 × 20–40 min/week | Attention control 3 × 20–40 min/week | 20 weeks | WOMAC a. Pain b. Stiffness c. Physical function | No adverse event |
| Wang et al., 2009 [56] | Boston, USA | ACR | 20/20 | IG:63 ± 8.1 CG:68 ± 7.0 | Tai Chi 2 × 60 min/week | Attention control 2 × 60 min/week | 12 weeks | WOMAC a. Pain b. Stiffness c. Physical function | One participant in the Tai Chi group reported an increase in knee pain |
| Wang et al., 2016 [33] | Boston, USA | ACR | 106/98 | IG:60.3 ± 10.5 CG:60.1 ± 10.5 | Tai Chi 2 × 60 min/week | Physical therapy pre-6 weeks 2 × 30 min/week post-6 weeks 4 × 30 min/week | 12 weeks | WOMAC a. Pain b. Stiffness c. Physical function | No adverse event |
| Ye et al., 2020 [34] | Fujian, China | ACR | 25/25 | IG:64.48 ± 7.81 CG:63.08 ± 3.65 | Baduanjin 3 × 40 min/week | None | 12 weeks | WOMAC a. Pain b. Stiffness c. Physical function | No adverse event |
| Zhu et al., 2016 [35] | Shanghai, China | ACR | 23/23 | IG:64.61 ± 3.40 CG:64.53 ± 3.43 | Tai Chi 3 × 60 min/week | Healthy education 1 × 60 min/week | 24 weeks | WOMAC a. Pain b. Stiffness c. Physical function | No adverse event |
| Subgroups | Outcomes | No. of Studies | No. of Sample Size | SMD (95% CI) | Statistical Method | p-Value for Heterogeneity |
|---|---|---|---|---|---|---|
| Exercise type | ||||||
| Tai Chi | Pain | 12 | 715 | −0.62 [−0.90, −0.34] | Random effect | <0.0001 ** |
| Stiffness | 11 | 608 | −0.67 [−1.02, −0.32] | Random effect | 0.0002 ** | |
| Physical function | 11 | 672 | −0.62 [−0.78, −0.46] | Fix effect | <0.00001 ** | |
| Baduanjin | Pain | 3 | 124 | −0.61 [−1.28, 0.06] | Random effect | 0.07 |
| Stiffness | 3 | 124 | −1.05 [−2.13, 0.02] | Random effect | 0.05 * | |
| Physical function | 3 | 124 | −0.97 [−1.34, −0.59] | Fix effect | <0.00001 ** | |
| Geographical location | ||||||
| Asian populations | Pain | 9 | 467 | −0.69 [−1.02, −0.36] | Random effect | <0.0001 * |
| Stiffness | 8 | 360 | −0.94 [−1.38, −0.50] | Random effect | <0.0001 ** | |
| Physical function | 8 | 424 | −0.85 [−1.04, −0.65] | Fix effect | <0.00001 ** | |
| Non−Asian populations | Pain | 5 | 348 | −0.47 [−0.87, −0.08] | Random effect | 0.02 * |
| Stiffness | 5 | 348 | −0.43 [−0.90, 0.04] | Random effect | 0.08 | |
| Physical function | 5 | 348 | −0.60 [−0.97, −0.22] | Random effect | 0.002 ** | |
| Duration time | ||||||
| 8 weeks | Pain | 2 | 65 | −0.64 [−1.16, −0.12] | Fix effect | 0.02 * |
| Stiffness | 2 | 65 | −0.55 [−1.06, −0.03] | Fix effect | 0.04 * | |
| Physical function | 2 | 65 | −0.57 [−1.09, −0.05] | Fix effect | 0.03 * | |
| 12 weeks | Pain | 8 | 599 | −0.54 [−0.85, −0.23] | Random effect | 0.0007 ** |
| Stiffness | 7 | 492 | −0.66 [−1.06, −0.26] | Random effect | 0.001 ** | |
| Physical function | 7 | 556 | −0.78 [−1.05, −0.50] | Random effect | <0.00001 ** | |
| Sample size | ||||||
| n ≥ 30 | Pain | 12 | 776 | −0.62 [−0.89, −0.36] | Random effect | <0.00001 ** |
| Stiffness | 11 | 669 | −0.81 [−1.19, −0.44] | Random effect | <0.0001 ** | |
| Physical function | 11 | 733 | −0.68 [−0.83, −0.53] | Fix effect | <0.00001 ** | |
| n < 30 | Pain | 2 | 39 | −0.56 [−1.23, 0.11] | Fix effect | 0.1 |
| Stiffness | 2 | 39 | −0.34 [−1.00, 0.31] | Fix effect | 0.31 | |
| Physical function | 2 | 39 | −0.50 [−1.17, 0.16] | Fix effect | 0.13 | |
| Control group type | ||||||
| Active control group | Pain | 8 | 596 | −0.71 [−1.07, −0.35] | Random effect | 0.0001 ** |
| Stiffness | 7 | 489 | −0.74 [−1.19, −0.29] | Random effect | 0.001 ** | |
| Physical function | 8 | 596 | −0.78 [−1.04, −0.52] | Random effect | <0.00001 ** | |
| Passive control group | Pain | 6 | 219 | −0.46 [−0.73, −0.18] | Fix effect | 0.001 ** |
| Stiffness | 6 | 219 | −0.78 [−1.32, −0.23] | Random effect | 0.005 ** | |
| Physical function | 5 | 176 | −0.71 [−1.02, −0.40] | Fix effect | <0.00001 ** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, R.; Chen, H.; Feng, J.; Xiao, Y.; Zhang, H.; Lam, C.W.-K.; Xiao, H. Effectiveness of Traditional Chinese Exercise for Symptoms of Knee Osteoarthritis: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Int. J. Environ. Res. Public Health 2020, 17, 7873. https://doi.org/10.3390/ijerph17217873
Li R, Chen H, Feng J, Xiao Y, Zhang H, Lam CW-K, Xiao H. Effectiveness of Traditional Chinese Exercise for Symptoms of Knee Osteoarthritis: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. International Journal of Environmental Research and Public Health. 2020; 17(21):7873. https://doi.org/10.3390/ijerph17217873
Chicago/Turabian StyleLi, Ruojin, Hongwei Chen, Jiahao Feng, Ying Xiao, Haoyang Zhang, Christopher Wai-Kei Lam, and Hong Xiao. 2020. "Effectiveness of Traditional Chinese Exercise for Symptoms of Knee Osteoarthritis: A Systematic Review and Meta-Analysis of Randomized Controlled Trials" International Journal of Environmental Research and Public Health 17, no. 21: 7873. https://doi.org/10.3390/ijerph17217873
APA StyleLi, R., Chen, H., Feng, J., Xiao, Y., Zhang, H., Lam, C. W.-K., & Xiao, H. (2020). Effectiveness of Traditional Chinese Exercise for Symptoms of Knee Osteoarthritis: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. International Journal of Environmental Research and Public Health, 17(21), 7873. https://doi.org/10.3390/ijerph17217873






