Mixed and Multi-Methods Protocol to Evaluate Implementation Processes and Early Effects of the Pradhan Mantri Jan Arogya Yojana Scheme in Seven Indian States
Abstract
1. Introduction
2. Materials and Methods
2.1. Pradhan Mantri Jan Arogya Yojana
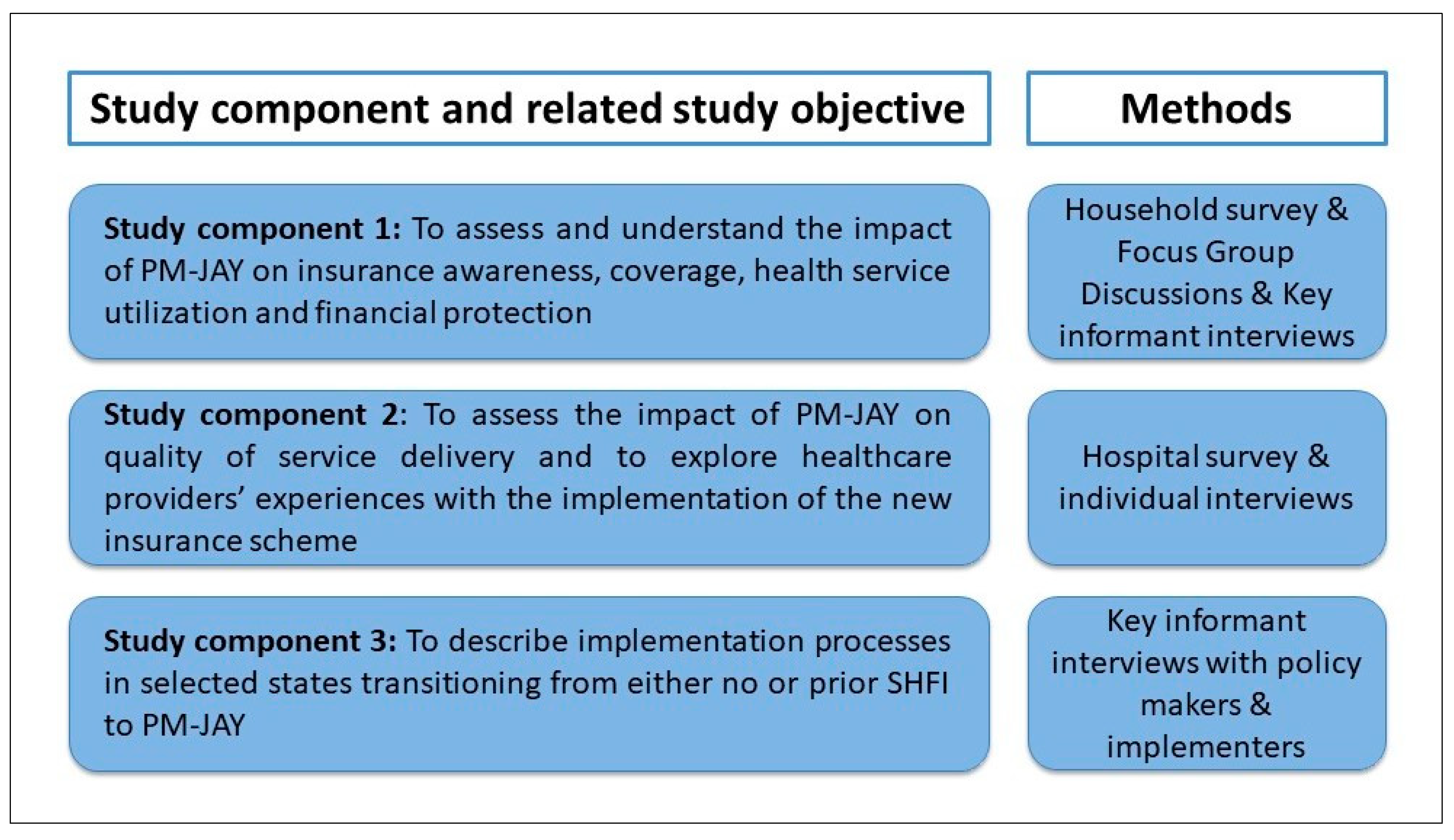
2.2. Conceptual Framework and Study Objectives
- To assess and understand the effects of PM-JAY on the target population’s awareness of PM-JAY features, coverage, health service use, and financial protection, including unraveling effect heterogeneity by population sub-groups (e.g., along socio-economic and gender dimensions);
- To assess the effects of PM-JAY on quality of service delivery and to explore healthcare providers’ experiences with the implementation of PM-JAY; and
- To document implementation processes at the national level, as well as in selected states transitioning from either no or a prior GFHI to PM-JAY.
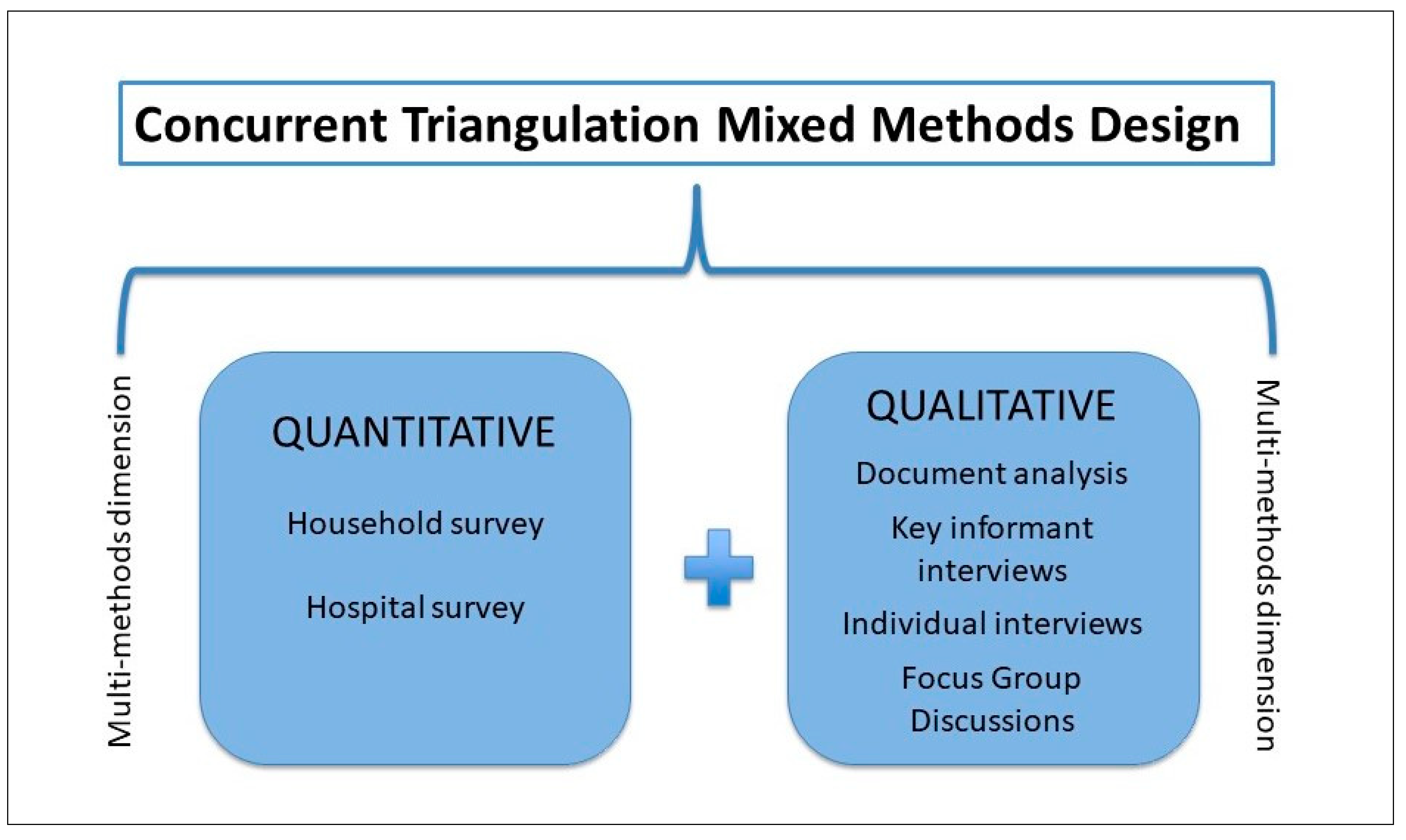
2.3. Study Design
2.4. Study Setting and State and District Selection
2.5. Study Component 1: Demand-Side Household and Individual Study
2.5.1. Quantitative Component
Sampling
Data Collection Tools and Strategies
Analytical Approach
2.5.2. Qualitative Component
Sampling
Data Collection Tools and Strategies
Analytical Approach
2.6. Study Component 2: Supply-Side Hospital Evaluation
2.6.1. Quantitative Component
Sampling
Data Collection Tools and Strategies
Analytical Approach
2.6.2. Qualitative Component
Sampling
Data Collection Tools and Strategies
Analytical Approach
2.7. Study Component 3: Process Documentation
2.7.1. Sampling
2.7.2. Data Collection Tools and Strategies
2.7.3. Analytical Approach
2.8. Ethical Considerations
2.9. Patient and Public Involvement
2.10. Data Sharing
3. Discussion
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Forgia, G.; La Nagpal, S. Government-sponsored health insurance in India: Are you covered? 2012; pp. 1–446. Available online: http://documents.worldbank.org/curated/en/2012/08/16653451/government-sponsored-health-insurance-india-covered%5Cnhttp://www-wds.worldbank.org/external/default/WDSContentServer/WDSP/IB/2012/08/30/000356161_20120830020253/Rendered/PDF/722380PUB0EPI00802902 (accessed on 23 October 2020).
- International Institute for Population Sciences. India Fact Sheet. Available online: http://www.indiaenvironmentportal.org.in/files/file/national%20family%20health%20survey%20-%20India%20fact%20sheet.pdf (accessed on 20 October 2020).
- Prinja, S.; Chauhan, A.S.; Karan, A.; Kaur, G.; Kumar, R. Impact of Publicly Financed Health Insurance Schemes on Healthcare Utilization and Financial Risk Protection in India: A Systematic Review. PLoS ONE 2017, 12, e0170996. [Google Scholar] [CrossRef] [PubMed]
- Sood, N.; Bendavid, E.; Mukherji, A.; Wagner, Z.; Nagpal, S.; Mullen, P. Government health insurance for people below poverty line in India: Quasi-experimental evaluation of insurance and health outcomes. BMJ 2014, 349, g5114. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Health Insurance in India: The Rashtriya Swasthya Bima Yojana Assessing Access for Informal Workers. 2012. Available online: https://www.wiego.org/sites/default/files/publications/files/Jain-Health-Insurance-Informal-Economy-India-WIEGO-PB10.pdf (accessed on 23 October 2020).
- Karpagam, S.; Vasan, A.; Seethappa, V. Falling Through the Gaps: Women Accessing Care under Health Insurance Schemes in Karnataka. Indian J. Gend. Stud. 2016, 23, 69–86. Available online: http://journals.sagepub.com/doi/10.1177/0971521515612864 (accessed on 23 October 2020). [CrossRef]
- Nandi, S.; Dasgupta, R.; Garg, S.; Sinha, D.; Sahu, S.; Mahobe, R. Uncovering Coverage: Utilisation of the Universal Health Insurance Scheme, Chhattisgarh by Women in Slums of Raipur. Indian J. Gend. Stud. 2016, 23, 43–68. Available online: http://ijg.sagepub.com (accessed on 23 October 2020). [CrossRef]
- Nandi, S.; Schneider, H.; Dixit, P. Hospital utilization and out of pocket expenditure in public and private sectors under the universal government health insurance scheme in Chhattisgarh State, India: Lessons for universal health coverage. PLoS ONE 2017, 12, e0187904. [Google Scholar] [CrossRef] [PubMed]
- Shaikh, M.; Peters, S.A.; Woodward, M.; Norton, R.; Jha, V. Sex differences in utilisation of hospital care in a state-sponsored health insurance programme providing access to free services in South India. BMJ Glob. Heal. 2018, 3, e000859. [Google Scholar] [CrossRef] [PubMed]
- Nagpal, S. Expanding Health Coverage for Vulnerable Groups in India. Available online: https://openknowledge.worldbank.org/handle/10986/13286 (accessed on 23 February 2019).
- Angell, B.J.; Prinja, S.; Gupt, A.; Jha, V.; Jan, S. The Ayushman Bharat Pradhan Mantri Jan Arogya Yojana and the path to universal health coverage in India: Overcoming the challenges of stewardship and governance. PLoS Med. 2019, 16, e1002759. Available online: http://www.ncbi.nlm.nih.gov/pubmed/30845199 (accessed on 19 July 2019). [CrossRef] [PubMed]
- Morton, M.; Nagpal, S.; Sadanandan, R.; Bauhoff, S. India’s Largest Hospital Insurance Program Faces Challenges In Using Claims Data To Measure Quality. Heal. Aff. 2016, 35, 1792–1799. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Indo German Social Security Programme. Process evaluation of India’s health insurance scheme for the poor rashtriya swasthya bima yojana in north east india Paper I. Available online: http://health.bmz.de/where_we_work/countries/india/Files/NE_Evaluation_Study_2015.pdf (accessed on 10 December 2019).
- Rajasekhar, D.; Berg, E.; Ghatak, M.; Manjula, R.; Roy, S. Implementing Health Insurance: The Rollout of Rashtriya Swasthya Bima Yojana in Karnataka. Econ. Polit. Wkly 2011, 20, 56–63. [Google Scholar]
- Virk, A.K.; Surender, R. Implementing National Health Insurance In India: Lessons For Policymaking And Practice In Low-Income Countries. Br. J. Interdiscip. Stud. 2016, 3, 1–19. Available online: http://www.bjis-online.org (accessed on 10 December 2019).
- Maurya, D.; Ramesh, M. Program design, implementation and performance: The case of social health insurance in India. Heal. Econ. Policy Law 2018, 14, 487–508. [Google Scholar] [CrossRef] [PubMed]
- Virk, A.; Atun, R. Towards universal health coverage in India: A historical examination of the genesis of Rashtriya Swasthya Bima Yojana – The health insurance scheme for low-income groups. Public Heal 2015, 129, 810–817. [Google Scholar] [CrossRef] [PubMed]
- Nandi, A.; Laxminarayan, R.; Holtzman, E.P.; Malani, A. The need for better evidence to evaluate the health & economic benefits of India′s Rashtriya Swasthya Bima Yojana. Indian J. Med Res. 2015, 142, 383–390. [Google Scholar] [PubMed]
- Government of India. Ayushman Bharat—National Health Protection Mission | National Portal of India. Available online: https://www.india.gov.in/spotlight/ayushman-bharat-national-health-protection-mission (accessed on 9 July 2018).
- Policy & Guidelines Ayushman Bharat. Available online: https://www.pmjay.gov.in/policy-and-guidelines (accessed on 16 September 2019).
- Status of Implementation of PM-JAY Across States Ayushman Bharat I National Health Authority GoI. Available online: https://www.pmjay.gov.in/states (accessed on 3 February 2020).
- Levesque, J.-F.; Harris, M.F.; Russell, G. Patient-centred access to health care: Conceptualising access at the interface of health systems and populations. Int. J. Equity Heal. 2013, 12, 18. Available online: https://equityhealthj.biomedcentral.com/track/pdf/10.1186/1475-9276-12-18 (accessed on 17 July 2018). [CrossRef] [PubMed]
- Creswell, J.W.; Plano Clark, V.L. Designing and conducting mixed methods research. 457p. Available online: https://in.sagepub.com/en-in/sas/designing-and-conducting-mixed-methods-research/book233508 (accessed on 17 July 2018).
- Tashakkori, A.; Teddlie, C. Sage handbook of mixed methods in social & behavioral research. 893p. Available online: https://in.sagepub.com/en-in/sas/sage-handbook-of-mixed-methods-in-social-behavioral-research/book233405 (accessed on 17 July 2018).
- Patton, M.Q. Qualitative research & evaluation methods: Integrating theory and practice. 806p. Available online: https://in.sagepub.com/en-in/sas/qualitative-research-evaluation-methods/book232962 (accessed on 23 July 2018).
- Gale, N.K.; Heath, G.; Cameron, E.; Rashid, S.; Redwood, S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. Available online: http://www.biomedcentral.com/1471-2288/13/117 (accessed on 23 July 2018).
- Smith, J.; Firth, J. Qualitative data analysis: Application of the framework approach. Nurse Res. 2011, 2, 52–62. Available online: http://eprints.hud.ac.uk/id/eprint/18884/1/RepositoryFrameworkNResearcher.pdf (accessed on 23 July 2018). [CrossRef] [PubMed]
- QSR International. NVivo 12.1. Available online: https://www.qsrinternational.com/nvivo/what-is-nvivo (accessed on 1 August 2019).
- World Health Organization. Service Availability and Readiness Assessment (SARA) An Annual Monitoring System for Service Delivery Reference Manual; WHO: Geneva, Switzerland, 2014.
- Government of India. Provider Network Under Pm-Rssm Empanelment and Allied Process. 2018. Available online: https://abnhpm.gov.in/sites/default/files/2018-07/HBP.pdf (accessed on 23 October 2020).
- Iacus, S.M.; King, G.; Porro, G. Causal Inference without Balance Checking: Coarsened Exact Matching. Politi- Anal. 2012, 20, 1–24. [Google Scholar] [CrossRef]
- Adams, P. Exploring social constructivism: Theories and practicalities. Education 3-13 2006, 34, 243–257. [Google Scholar] [CrossRef]
- Brownson, R.C.; Colditz, G.A.; Proctor, E.K. Dissemination and Implementation Research in HealthTranslating Science to Practice; Oxford University Press: Oxford, UK, 2012. [Google Scholar]
- DFID. How To Note Political Economy Analysis Contents. 2009. Available online: www.gsdrc.org/go/topic-guides/political-economy-analysis (accessed on 23 July 2018).
- De Allegri, M.; Brenner, S.; Kambala, C.; Mazalale, J.; Muula, A.S.; Chinkhumba, J.; Wilhelm, D.; Lohmann, J. Exploiting the emergent nature of mixed methods designs: Insights from a mixed methods impact evaluation in Malawi. Health Policy Plan. 2020, 35, 102–106. Available online: https://academic.oup.com/heapol/article-abstract/35/1/102/5591518 (accessed on 7 April 2020). [CrossRef] [PubMed]
- Lavrakas, P. External Validity. In Encyclopedia of Survey Research Methods; Sage Publications, Inc.: New York, NY, USA, 2013. [Google Scholar]


| State | Implementation Model | Districts | Previously Implemented GFHI in 2018 |
|---|---|---|---|
| Bihar | Trust mode | Gaya, Muzaffarpur and Patna | None |
| Chhattisgarh | Mixed mode * | Raigarh and Bilaspur | Mukhyamantri Swasthya Bima Yojana |
| Gujarat | Mixed mode | Ahmedabad and Surat | Mukhyamantri Amrutam |
| Karnataka | Trust mode | Raichur and Tumkur | Vajpayee Arograsri Scheme |
| Meghalaya | Insurance mode | South West Garo Hills and East Khasi Hills | Megha Health Insurance Scheme |
| Tamil Nadu | Mixed mode | Coimbatore and Sivagangai | Chief Minister’s Comprehensive Health Insurance Scheme |
| Uttar Pradesh | Trust mode | Allahabad, Ghazipur and Rampur | None |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Allegri, M.D.; Srivastava, S.; Strupat, C.; Brenner, S.; Parmar, D.; Parisi, D.; Walsh, C.; Mahajan, S.; Neogi, R.; Ziegler, S.; et al. Mixed and Multi-Methods Protocol to Evaluate Implementation Processes and Early Effects of the Pradhan Mantri Jan Arogya Yojana Scheme in Seven Indian States. Int. J. Environ. Res. Public Health 2020, 17, 7812. https://doi.org/10.3390/ijerph17217812
Allegri MD, Srivastava S, Strupat C, Brenner S, Parmar D, Parisi D, Walsh C, Mahajan S, Neogi R, Ziegler S, et al. Mixed and Multi-Methods Protocol to Evaluate Implementation Processes and Early Effects of the Pradhan Mantri Jan Arogya Yojana Scheme in Seven Indian States. International Journal of Environmental Research and Public Health. 2020; 17(21):7812. https://doi.org/10.3390/ijerph17217812
Chicago/Turabian StyleAllegri, Manuela De, Swati Srivastava, Christoph Strupat, Stephan Brenner, Divya Parmar, Diletta Parisi, Caitlin Walsh, Sahil Mahajan, Rupak Neogi, Susanne Ziegler, and et al. 2020. "Mixed and Multi-Methods Protocol to Evaluate Implementation Processes and Early Effects of the Pradhan Mantri Jan Arogya Yojana Scheme in Seven Indian States" International Journal of Environmental Research and Public Health 17, no. 21: 7812. https://doi.org/10.3390/ijerph17217812
APA StyleAllegri, M. D., Srivastava, S., Strupat, C., Brenner, S., Parmar, D., Parisi, D., Walsh, C., Mahajan, S., Neogi, R., Ziegler, S., Basu, S., & Jain, N. (2020). Mixed and Multi-Methods Protocol to Evaluate Implementation Processes and Early Effects of the Pradhan Mantri Jan Arogya Yojana Scheme in Seven Indian States. International Journal of Environmental Research and Public Health, 17(21), 7812. https://doi.org/10.3390/ijerph17217812







