Association of Acupuncture Treatment with Mortality of Type 2 Diabetes in China: Evidence of a Real-World Study
Abstract
1. Introduction
1.1. Prevalence of Diabetes
1.2. Introduction of Acupuncture
1.3. Strengthening Acupuncture in China
1.4. The Purpose of the Study
2. Materials and Methods
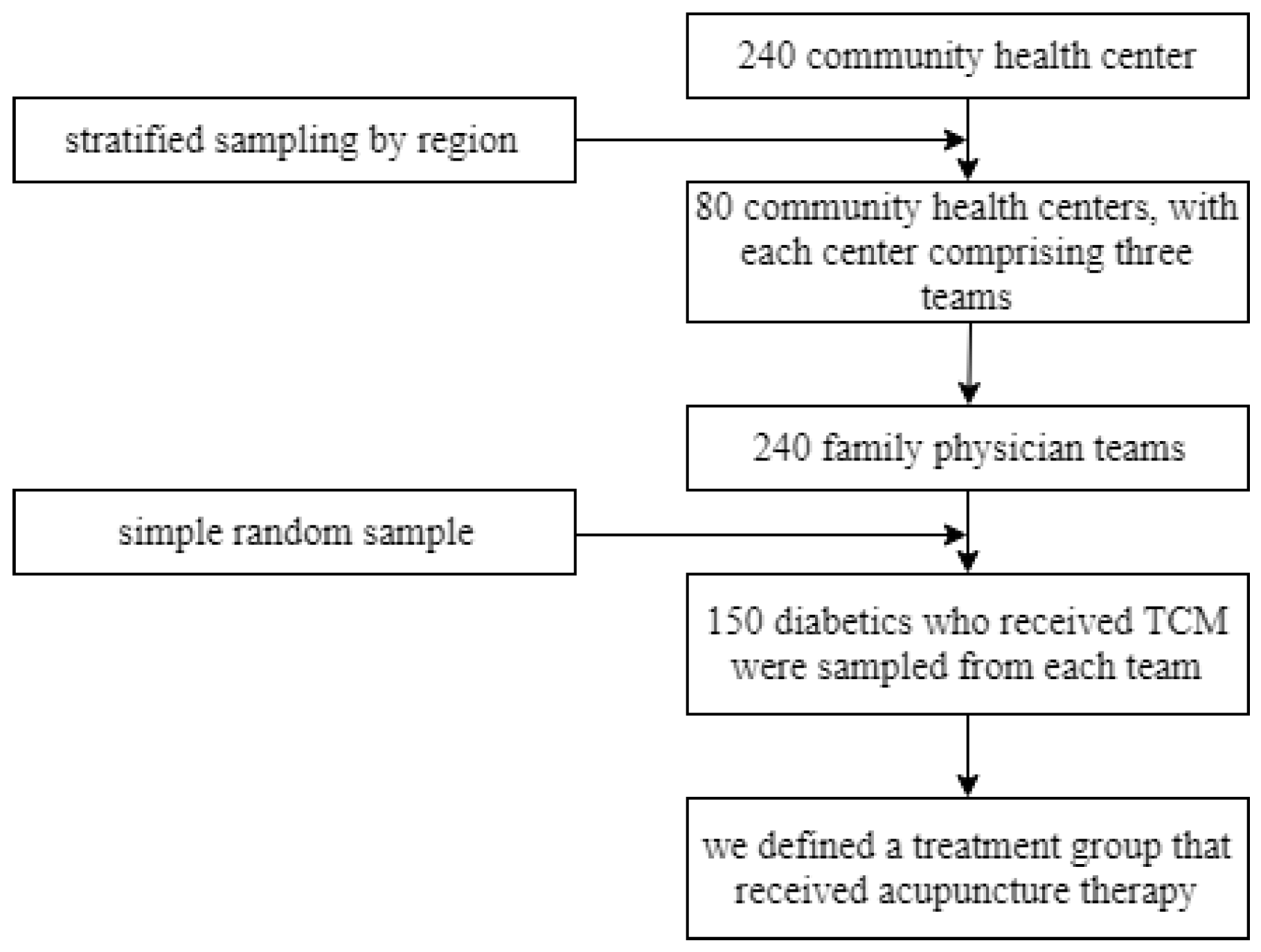
2.1. Study Design
2.2. Data Source and Population Selection
2.3. Research Variables
2.3.1. Dependent Variable
2.3.2. Independent Variable
2.4. Statistical Analysis
3. Results
3.1. Baseline T2DM Patient Characteristics
3.2. Inverse Probability Weighted Regression Results
3.3. Robust Test Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Standl, E.; Khunti, K.; Hansen, T.B.; Schnell, O. The global epidemics of diabetes in the 21st century: Current situation and perspectives. Eur J. Prev Cardiol 2019, 26 (Suppl. 2), 7–14. [Google Scholar] [CrossRef] [PubMed]
- Federation, I.D. IDF Diabetes Atlas, 9th edn. 2019. Available online: http://www.diabetesatlas.org (accessed on 25 July 2020).
- Stolar, M. Glycemic control and complications in type 2 diabetes mellitus. Am. J. Med. 2010, 123 (Suppl. 3), S3–S11. [Google Scholar] [CrossRef]
- Diabetes Prevention Program Research Group. Long-term effects of lifestyle intervention or metformin on diabetes development and microvascular complications over 15-year follow-up: The Diabetes Prevention Program Outcomes Study. Lancet Diabet Endocrinol 2015, 3, 866–875. [Google Scholar] [CrossRef]
- Feng, Y.; Fang, Y.; Wang, Y.; Hao, Y. Acupoint Therapy on Diabetes Mellitus and Its Common Chronic Complications: A Review of Its Mechanisms. BioMed Res. Int. 2018, 2018, 3128378. [Google Scholar] [CrossRef] [PubMed]
- Upchurch, D.M.; Rainisch, B.W. A sociobehavioral wellness model of acupuncture use in the United States, 2007. J. Alternat Complement. Med. (New York, N.Y.) 2014, 20, 32–39. [Google Scholar] [CrossRef] [PubMed]
- Ishizaki, N.; Yano, T.; Kawakita, K. Public status and prevalence of acupuncture in Japan. Evid Based Complement. Alternat Med. 2010, 7, 493–500. [Google Scholar] [CrossRef] [PubMed]
- Wu, M.Y.; Lee, Y.C.; Lin, C.L.; Huang, M.C.; Sun, M.F.; Yen, H.R. Trends in use of acupuncture among adults in Taiwan from 2002 to 2011: A nationwide population-based study. PLoS ONE 2018, 13, e0195490. [Google Scholar] [CrossRef]
- Poon, T.Y.; Ong, K.L.; Cheung, B.M. Review of the effects of the traditional Chinese medicine Rehmannia Six Formula on diabetes mellitus and its complications. J. Diabet 2011, 3, 184–200. [Google Scholar] [CrossRef]
- Shi, L.; Feng, L.; Yang, Y.; Li, X.; Zhang, M.; Zhang, Y.; Ni, Q. Prevention of type 2 diabetes mellitus with acupuncture: Protocol for a systematic review and meta-analysis. Medicine 2018, 97, e13355. [Google Scholar] [CrossRef]
- Shu, Z.; Wang, L.; Sun, X. An evaluation of the effects of general practitioner-supported patient noncommunicable diseases control model in Shanghai, China. Int J. Health Plann. Manage. 2019, 34, 947–959. [Google Scholar] [CrossRef]
- Meyer-Hamme, G.; Friedemann, T.; Greten, H.J.; Plaetke, R.; Gerloff, C.; Schroeder, S. ACUDIN—ACUpuncture and laser acupuncture for treatment of DIabetic peripheral Neuropathy: A randomized, placebo-controlled, partially double-blinded trial. BMC Neurol. 2018, 18, 40. [Google Scholar] [CrossRef] [PubMed]
- Chung, V.C.; Ma, P.H.; Wang, H.H.; Wang, J.J.; Hong, L.C.; Wei, X.; Wong, S.Y.; Tang, J.L.; Griffiths, S.M. Integrating traditional Chinese medicine services in community health centers: Insights into utilization patterns in the pearl river region of China. Evid. Based Complement. Alternat Med. 2013, 2013, 426360. [Google Scholar] [CrossRef] [PubMed]
- National Administration of Traditional Chinese Medicine. Implementation Plan for Popularizing Appropriate Technology of Traditional Chinese Medicine for Common and Frequently-Occurring Diseases at Grassroots Level (2009–2010). 2009. Available online: http://yzs.satcm.gov.cn/gongzuodongtai/2018-03-25/6558.html (accessed on 27 July 2020).
- National Administration of Traditional Chinese Medicine. 13th Five-year plan for the development of traditional Chinese medicine. In Medicine, S.A. o. T. C. Ed. 2016. Available online: http://www.gov.cn/xinwen/2016-08/11/content_5098934.htm (accessed on 27 July 2020).
- Fang, Y. Study of the Family-Doctor System in Shanghai; Shanghai University of Engineering Science: Shanghai, China, 2016. [Google Scholar]
- Network, C.B. The Signing Rate of Family Doctors in Shanghai is 30%. 2019. Available online: https://www.yicai.com/news/100095345.html (accessed on 5 August 2020).
- Chen, C.; Liu, J.; Sun, M.; Liu, W.; Han, J.; Wang, H. Acupuncture for type 2 diabetes mellitus: A systematic review and meta-analysis of randomized controlled trials. Complement. Ther. Clin. Pract. 2019, 36, 100–112. [Google Scholar] [CrossRef]
- Kumar, R.; Mooventhan, A.; Manjunath, N.K. Immediate effect of needling at CV-12 (Zhongwan) acupuncture point on blood glucose level in patients with type 2 diabetes mellitus: A pilot randomized placebo-controlled trial. J. Acupunct. Meridian Stud. 2017, 10, 240–244. [Google Scholar] [CrossRef] [PubMed]
- Mansournia, M.A.; Altman, D.G. Inverse probability weighting. BMJ 2016, 352, i189. [Google Scholar] [CrossRef]
- Strumpf, E.; Ammi, M.; Diop, M.; Fiset-Laniel, J.; Tousignant, P. The impact of team-based primary care on health care services utilization and costs: Quebec’s family medicine groups. J. Health Econ. 2017, 55, 76–94. [Google Scholar] [CrossRef]
- Xian, W.; Xu, X.; Li, J.; Sun, J.; Fu, H.; Wu, S.; Liu, H. Health care inequality under different medical insurance schemes in a socioeconomically underdeveloped region of China: A propensity score matching analysis. BMC Public Health 2019, 19, 1373. [Google Scholar] [CrossRef] [PubMed]
- Zhang, R. The Clinical Study of Laser Acupuncture and Moxibustion in Treating Type 2 Diabetes with Deficiency of Qi and Yin; Nanjing University of Traditional Chinese Medicine: Nanjing, China, 2020. [Google Scholar] [CrossRef]
- Pan, H.; Huang, H.; Zhang, L.; Ma, S.; Yang, H.; Wang, H. “Adjusting internal organs and dredging channel” electroacupuncture treatment prevents the development of diabetic peripheral neuropathy by downregulating glucose-related protein 78 (GRP78) and caspase-12 in streptozotocin-diabetic rats. J. Diabetes 2019, 11, 928–937. [Google Scholar] [CrossRef]
- Li, Y.; Qian, Z.Y.; Cheng, K.; Zhao, L.; Shen, X.Y.; Deng, H.P. Effect of Compound Laser Acupuncture-Moxibustion on Blood Glucose, Fasting Insulin and Blood Lipids Levels in Type 2 Diabetic Rats. Chin. J. Integrat. Med. 2020, 26, 33–38. [Google Scholar] [CrossRef]
- Cornejo-Garrido, J.; Becerril-Chávez, F.; Carlín-Vargas, G.; Ordoñez-Rodríguez, J.M.; Abrajan-González Mdel, C.; de la Cruz-Ramírez, R.; Ordaz-Pichardo, C. Antihyperglycaemic effect of laser acupuncture treatment at BL20 in diabetic rats. Acupunct Med. J. Brit. Med. Acupunct Soc. 2014, 32, 486–494. [Google Scholar] [CrossRef]
- Firouzjaei, A.; Li, G.C.; Wang, N.; Liu, W.X.; Zhu, B.M. Comparative evaluation of the therapeutic effect of metformin monotherapy with metformin and acupuncture combined therapy on weight loss and insulin sensitivity in diabetic patients. Nutr. Diabet. 2016, 6, e209. [Google Scholar] [CrossRef]
- Wang, L.Q.; Chen, Z.; Zhang, K.; Liang, N.; Yang, G.Y.; Lai, L.; Liu, J.P. Zusanli (ST36) Acupoint Injection for Diabetic Peripheral Neuropathy: A Systematic Review of Randomized Controlled Trials. J. Alternat. Complement. Med. 2018, 24, 1138–1149. [Google Scholar] [CrossRef]
- Zhang, C.; Ma, Y.X.; Yan, Y. Clinical effects of acupuncture for diabetic peripheral neuropathy. J. Tradit. Chin. Med. 2010, 30, 13–14. [Google Scholar] [CrossRef]
- Nash, J.; Armour, M.; Penkala, S. Acupuncture for the treatment of lower limb diabetic peripheral neuropathy: A systematic review. Acupunct Med. J. Brit. Med. Acupunct Soc. 2019, 37, 3–15. [Google Scholar] [CrossRef]
- Lee, S.; Kim, J.H.; Shin, K.M.; Kim, J.E.; Kim, T.H.; Kang, K.W.; Lee, M.; Jung, S.Y.; Shin, M.S.; Kim, A.R.; et al. Electroacupuncture to treat painful diabetic neuropathy: Study protocol for a three-armed, randomized, controlled pilot trial. Trials 2013, 14, 225. [Google Scholar] [CrossRef]
- Lee, M.; Li, H.; Liu, D. Acupuncture as adjuvant therapy for diabetic foot: A protocol for systematic review. Medicine 2020, 99, e19502. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Acupuncture Group (N = 6865) | Non-Acupuncture Group (N = 30,853) | ||||
|---|---|---|---|---|---|---|
| Mean | SE | 95%CI | Mean | SE | 95% CI | |
| Gender (%) | ||||||
| Male | 34.64 | 0.006 | 33.43–35.87 | 40.98 | 0.002 | 40.44–41.53 |
| Female | 65.35 | 0.006 | 64.13–66.57 | 59.01 | 0.002 | 58.46–59.56 |
| Age (years) | ||||||
| Mean | 70.04 | 0.125 | 69.79–70.28 | 67.91 | 0.057 | 67.79–68.02 |
| <60 | 9.96 | 0.003 | 9.27–10.69 | 19.29 | 0.002 | 18.85–19.73 |
| 60–69 | 33.38 | 0.006 | 32.28–34.51 | 38.79 | 0.003 | 38.25–39.34 |
| 70–79 | 25.53 | 0.005 | 24.51–26.58 | 27.09 | 0.003 | 26.60–27.59 |
| ≥80 | 31.11 | 0.006 | 30.03–32.22 | 14.81 | 0.002 | 14.42–15.21 |
| Residential location (%) | ||||||
| Urban | 44.22 | 0.006 | 42.95–45.49 | 34.93 | 0.002 | 34.39–35.46 |
| Suburban | 55.77 | 0.006 | 54.50–57.04 | 65.07 | 0.002 | 64.53–65.60 |
| Chronic (%) | ||||||
| 0 | 9.77 | 0.003 | 9.09–10.49 | 20.18 | 0.002 | 19.73–20.63 |
| 1 | 19.16 | 0.004 | 18.25–20.11 | 29.91 | 0.002 | 29.40–30.42 |
| 2 | 23.10 | 0.005 | 22.12–24.11 | 23.92 | 0.002 | 23.44–24.40 |
| ≥3 | 47.95 | 0.006 | 46.77–49.13 | 25.99 | 0.002 | 25.50–26.48 |
| Total cost (yuan) | ||||||
| Mean | 16,571.99 | 177.64 | 16,223.74–16,920.24 | 10,098.17 | 61.94 | 9976.74–10,219.60 |
| ≤2000 | 5.07 | 0.002 | 4.57–5.61 | 20.32 | 0.002 | 19.87–20.77 |
| 2001–7000 | 16.35 | 0.004 | 15.50–17.25 | 31.53 | 0.003 | 31.01–32.05 |
| 7001–15,000 | 29.30 | 0.005 | 28.24–30.39 | 27.76 | 0.003 | 27.26–28.26 |
| ≥15,001 | 49.26 | 0.006 | 48.08–50.44 | 20.39 | 0.002 | 19.94–20.84 |
| Outpatient visits | ||||||
| Number of primary-level hospitals | 39.51 | 0.355 | 38.81–40.21 | 26.63 | 0.135 | 26.36–26.90 |
| Number of secondary-level hospitals | 7.43 | 0.138 | 7.16–7.71 | 5.35 | 0.052 | 5.25–5.45 |
| Number of tertiary-level hospitals | 8.82 | 0.144 | 8.53–9.10 | 6.50 | 0.056 | 6.39–6.61 |
| Inpatient visits | ||||||
| Number of primary-level hospitals | 0.012 | 0.002 | 0.01–0.02 | 0.012 | 0.000 | 0.01–0.01 |
| Number of secondary-level hospitals | 0.278 | 0.012 | 0.25–0.30 | 0.145 | 0.003 | 0.13–0.15 |
| Number of tertiary-level hospitals | 0.271 | 0.010 | 0.25–0.29 | 0.149 | 0.003 | 0.14–1.56 |
| Total prescriptions of acupuncture | 3.26 | 0.062 | 3.14–3.38 | 0.00 | 0.000 | 0.00 |
| Death in 2018 | Coefficient | 95%CI | SE | p-Value |
|---|---|---|---|---|
| Treat 2016 | −0.0002 | −0.0024–0.0019 | 0.0011 | 0.857 |
| Gender (%) | ||||
| Male | 0.0040 *** | 0.0016–0.0064 | 0.0012 | 0.001 |
| Age (%) | ||||
| 60–69 | 0.0016 | −0.0005–0.0038 | 0.0011 | 0.140 |
| 70–79 | 0.0056 *** | 0.0030–0.0082 | 0.0013 | 0.000 |
| ≥80 | 0.0192 *** | 0.0144–0.0239 | 0.0024 | 0.000 |
| Chronic (%) | ||||
| 1 | 0.0004 | 0.0032–0.0024 | 0.0014 | 0.774 |
| 2 | 0.0003 | 0.0042–0.0035 | 0.0019 | 0.850 |
| ≥3 | 0.0025 | 0.0061–0.0008 | 0.0017 | 0.145 |
| Residential location (%) | ||||
| Urban | −0.0024 *** | −0.0046–−0.0003 | 0.0011 | 0.027 |
| Cost (%) | ||||
| 2001–7000 | 0.0050 *** | 0.0022–0.0007 | 0.0014 | 0.000 |
| 7001–15,000 | 0.0049 *** | 0.0019–0.0079 | 0.0015 | 0.001 |
| ≥15,001 | 0.0063 *** | 0.0029–0.0095 | 0.0016 | 0.000 |
| Constant | −0.0026 | −0.0055–0.0002 | 0.0014 | 0.075 |
| Characteristics | Before Matching | After Matching | ||||
|---|---|---|---|---|---|---|
| Acupuncture Group | Non-Acupuncture Group | p Value | Acupuncture Group | Non-Acupuncture Group | p Value | |
| Gender (%) | ||||||
| Male | 34.57 | 40.97 | <0.001 | 34.57 | 34.57 | 1.000 |
| Age (%) | ||||||
| 60–69 | 39.15 | 38.84 | 0.647 | 39.15 | 39.15 | 1.000 |
| 70–79 | 29.95 | 27.11 | <0.001 | 29.95 | 29.95 | 1.000 |
| ≥80 | 19.25 | 14.78 | <0.001 | 19.25 | 19.25 | 1.000 |
| Chronic (%) | ||||||
| 1 | 22.49 | 29.92 | <0.001 | 22.49 | 22.49 | 1.000 |
| 2 | 27.07 | 24.01 | <0.001 | 27.07 | 27.07 | 0.979 |
| ≥3 | 39.12 | 26.10 | <0.001 | 39.12 | 39.12 | 0.981 |
| Cost (%) | ||||||
| 2001–7000 | 19.13 | 31.61 | <0.001 | 19.13 | 19.13 | 1.000 |
| 7001–15,000 | 34.39 | 27.88 | <0.001 | 34.39 | 34.39 | 1.000 |
| ≥15,001 | 40.62 | 20.48 | <0.001 | 0.62 | 0.62 | 1.000 |
| Residential location (%) | ||||||
| Urban | 44.22 | 34.88 | <0.001 | 44.22 | 44.22 | 1.000 |
| Method | Coefficient | 95%CI | Standard Error | Z | p |
|---|---|---|---|---|---|
| 1:4 PSM (bootstrap 50 times) | −0.0014 | −0.0072, 0.0042 | 0.0029 | −0.51 | 0.611 |
| 1:3 PSM (bootstrap 50 times) | −0.0034 | −0.0105, 0.0036 | 0.0036 | −0.95 | 0.344 |
| Kernel Matching | −0.0002 | −0.0022, −0.0016 | 0.0009 | −0.30 | 0.766 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sui, M.; Xue, L.; Ying, X. Association of Acupuncture Treatment with Mortality of Type 2 Diabetes in China: Evidence of a Real-World Study. Int. J. Environ. Res. Public Health 2020, 17, 7801. https://doi.org/10.3390/ijerph17217801
Sui M, Xue L, Ying X. Association of Acupuncture Treatment with Mortality of Type 2 Diabetes in China: Evidence of a Real-World Study. International Journal of Environmental Research and Public Health. 2020; 17(21):7801. https://doi.org/10.3390/ijerph17217801
Chicago/Turabian StyleSui, Mengyun, Long Xue, and Xiaohua Ying. 2020. "Association of Acupuncture Treatment with Mortality of Type 2 Diabetes in China: Evidence of a Real-World Study" International Journal of Environmental Research and Public Health 17, no. 21: 7801. https://doi.org/10.3390/ijerph17217801
APA StyleSui, M., Xue, L., & Ying, X. (2020). Association of Acupuncture Treatment with Mortality of Type 2 Diabetes in China: Evidence of a Real-World Study. International Journal of Environmental Research and Public Health, 17(21), 7801. https://doi.org/10.3390/ijerph17217801





