Randomized Clinical Trial of an Internet-Based Adolescent Depression Prevention Intervention in Primary Care: Internalizing Symptom Outcomes
Abstract
1. Introduction
2. Materials and Methods
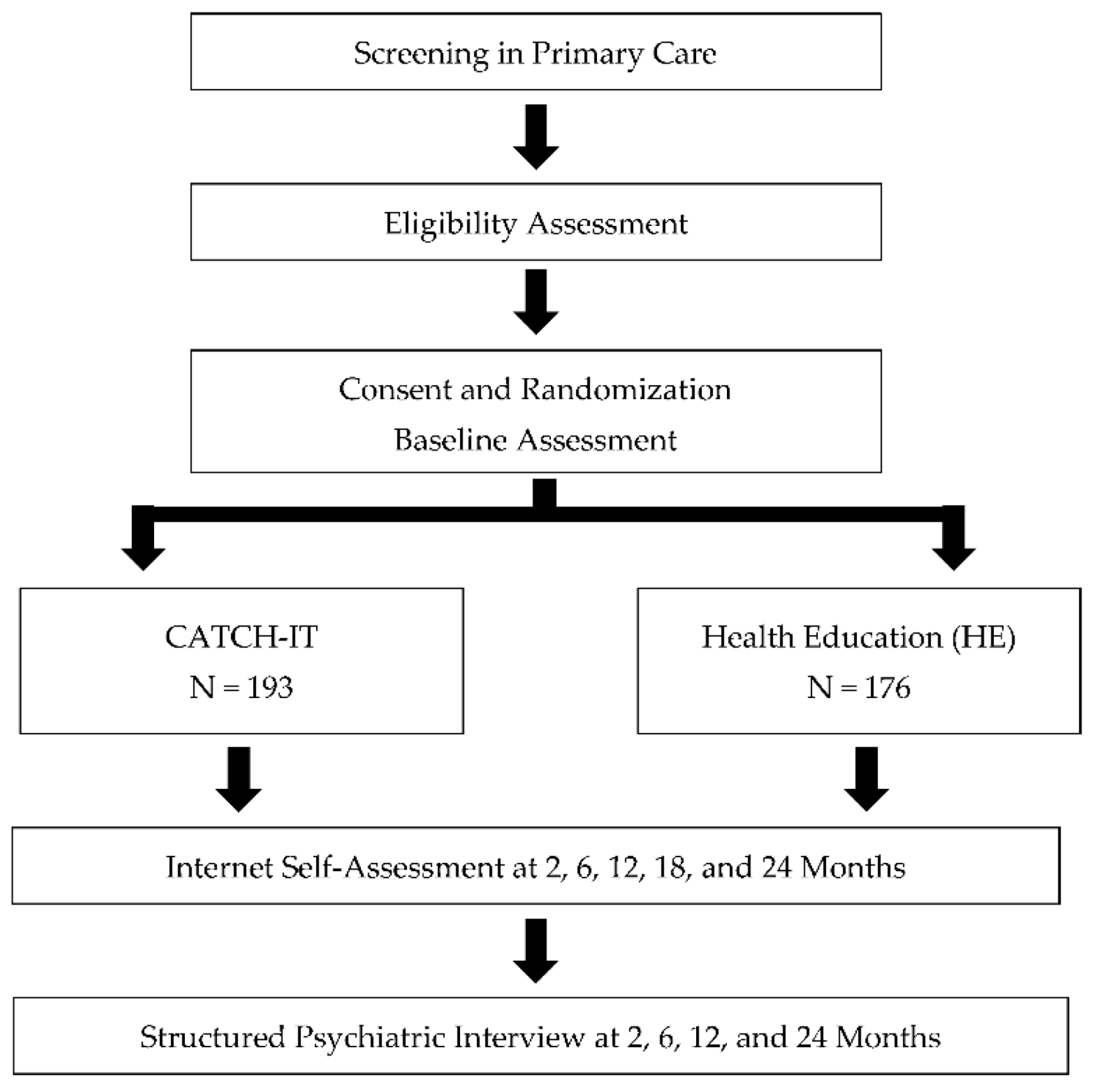
2.1. Study Design and Setting
2.2. Participants
2.3. Study Procedures
2.4. Randomization and Blinding
2.5. Treatment Arms
2.5.1. The CATCH-IT Intervention
2.5.2. The Health Education Intervention
2.6. Measures
2.7. Statistical Analysis
3. Results
3.1. Participants
3.2. Symptoms of Anxiety and Depression
3.3. Analyses of Potential Moderators
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Rushton Jerry, L.; Michelle, F.; Schectman Robin, M. Epidemiology of depressive symptoms in the National Longitudinal Study of Adolescent Health. J. Am. Acad. Child Adolesc. Psychiatry 2002, 41, 199–205. [Google Scholar] [CrossRef] [PubMed]
- Lewinsohn, P.M.; Rohde, P.; Klein, D.N.; Seeley, J.R. Natural course of adolescent major depressive disorder: I. Continuity into young adulthood. J. Am. Acad. Child Adolesc. Psychiatry 1999, 38, 56. [Google Scholar] [CrossRef] [PubMed]
- Weissman, M.M.; Wolk, S.; Goldstein, R.B.; Moreau, D.; Adams, P.; Greenwald, S.; Klier, C.M.; Ryan, N.D.; Dahl, R.E.; Wickramaratne, P. Depressed adolescents grown up. JAMA 1999, 281, 1707. [Google Scholar] [CrossRef] [PubMed]
- Birmaher, B.; Ryan, N.D.; Williamson, D.E.; Brent, D.A.; Kaufman, J.; Dahl, R.E.; Perel, J.; Nelson, B. Childhood and adolescent depression: A review of the past 10 years. Part I. J. Am. Acad. Child Adolesc. Psychiatry 1996, 35, 1427. [Google Scholar] [CrossRef]
- Pine, D.S.; Goldstein, R.B.; Wolk, S.; Weissman, M.M. The Association Between Childhood Depression and Adulthood Body Mass Index. Pediatrics 2001, 107, 1049–1056. [Google Scholar] [CrossRef]
- Balázs, J.; Miklósi, M.; Keresztény, Á.; Hoven, C.W.; Carli, V.; Wasserman, C.; Apter, A.; Bobes, J.; Brunner, R.; Cosman, D.; et al. Adolescent subthreshold-depression and anxiety: Psychopathology, functional impairment and increased suicide risk. J. Child Psychol. Psychiatry 2013, 54, 670–677. [Google Scholar] [CrossRef]
- Georgiades, K.; Lewinsohn, P.M.; Monroe, S.M.; Seeley, J.R. Major depressive disorder in adolescence: The role of subthreshold symptoms. J. Am. Acad. Child Adolesc. Psychiatry 2006, 45, 936–944. [Google Scholar] [CrossRef]
- Birmaher, B.; Ryan, N.D.; Williamson, D.E.; Brent, D.A.; Kaufman, J. Childhood and adolescent depression: A review of the past 10 years. Part II. J. Am. Acad. Child Adolesc. Psychiatry 1996, 35, 1575. [Google Scholar] [CrossRef]
- Buntrock, C.; Berking, M.; Smit, F.; Lehr, D.; Nobis, S.; Riper, H.; Cuijpers, P.; Ebert, D. Preventing depression in adults with subthreshold depression: Health-economic evaluation alongside a pragmatic randomized controlled trial of a web-based intervention. J. Med. Internet Res. 2017, 19, e5. [Google Scholar] [CrossRef]
- Hetrick, S.E.; Cox, G.R.; Witt, K.G.; Bir, J.J.; Merry, S.N. Cognitive behavioural therapy (CBT), third-wave CBT and interpersonal therapy (IPT) based interventions for preventing depression in children and adolescents. Cochrane Database Syst. Rev. 2016. [Google Scholar] [CrossRef]
- Brown, C.H.; Brincks, A.; Huang, S.; Perrino, T.; Cruden, G.; Pantin, H.; Howe, G.; Young, J.F.; Beardslee, W.; Montag, S. Two-year impact of prevention programs on adolescent depression: An integrative data analysis approach. Prev. Sci. 2018, 19, 74–94. [Google Scholar] [CrossRef]
- Gladstone, T.; Terrizzi, D.; Stinson, A.; Nidetz, J.; Canel, J.; Ching, E.; Berry, A.; Cantorna, J.; Fogel, J.; Eder, M.; et al. Effect of Internet-based Cognitive Behavioral Humanistic and Interpersonal Training vs. Internet-based General Health Education on Adolescent Depression in Primary Care: A Randomized Clinical Trial. JAMA Netw. Open 2018, 1, e184278. [Google Scholar] [CrossRef]
- Saulsberry, A.; Marko-Holguin, M.; Blomeke, K.; Hinkle, C.; Fogel, J.; Gladstone, T.; Bell, C.; Reinecke, M.; Corden, M.; Van Voorhees, B.W. Randomized Clinical Trial of a Primary Care Internet-based Intervention to Prevent Adolescent Depression: One-year Outcomes. J. Can. Acad. Child Adolesc. Psychiatry 2013, 22, 106–117. [Google Scholar] [PubMed]
- Conejo-Cerón, S.; Moreno-Peral, P.; Rodríguez-Morejón, A.; Motrico, E.; Navas-Campaña, D.; Rigabert, A.; Martín-Pérez, C.; Rodríguez-Bayón, A.; Ballesta-Rodríguez, M.I.; Luna, J.d.D.; et al. Effectiveness of Psychological and Educational Interventions to Prevent Depression in Primary Care: A Systematic Review and Meta-Analysis. Ann. Fam. Med. 2017, 15, 262–271. [Google Scholar] [CrossRef] [PubMed]
- Garber, J.; Clarke, G.N.; Weersing, V.R.; Beardslee, W.R.; Brent, D.A.; Gladstone, T.R.G.; DeBar, L.L.; Lynch, F.L.; D’Angelo, E.; Hollon, S.D.; et al. Prevention of depression in at-risk adolescents: A randomized controlled trial. JAMA 2009, 301, 2215. [Google Scholar] [CrossRef]
- Beardslee, W.R.; Brent, D.A.; Weersing, V.R.; Clarke, G.N.; Porta, G.; Hollon, S.D.; Gladstone, T.R.G.; Gallop, R.; Lynch, F.L.; Iyengar, S.; et al. Prevention of depression in at-risk adolescents: Longer-term effects. JAMA Psychiatry 2013, 70, 1161. [Google Scholar] [CrossRef]
- Gillham, J.E.; Hamilton, J.; Freres, D.R.; Patton, K.; Gallop, R. Preventing Depression Among Early Adolescents in the Primary Care Setting: A Randomized Controlled Study of the Penn Resiliency Program. J. Abnorm. Child Psychol. 2006, 34, 195–211. [Google Scholar] [CrossRef]
- Merikangas, K.R.; He, J.-P.; Burstein, M.; Swanson, S.A.; Avenevoli, S.; Cui, L.; Benjet, C.; Georgiades, K.; Swendsen, J. Lifetime prevalence of mental disorders in U.S. adolescents: Results from the National Comorbidity Survey Replication—Adolescent Supplement (NCS-A). J. Am. Acad. Child Adolesc. Psychiatry 2010, 49, 980. [Google Scholar] [CrossRef] [PubMed]
- Merikangas, K.R.; Nakamura, E.F.; Kessler, R.C. Epidemiology of mental disorders in children and adolescents. Dialogues Clin. Neurosci. 2009, 11, 7–20. [Google Scholar] [PubMed]
- Kessler, R.C.; Berglund, P.; Demler, O.; Jin, R.; Merikangas, K.R.; Walters, E.E. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry 2005, 62, 593–602. [Google Scholar] [CrossRef]
- Kessler, R.; Avenevoli, S.; McLaughlin, K.; Green, J.; Lakoma, M.; Petukhova, M.; Pine, D.; Sampson, N.; Zaslavsky, A.; Merikangas, K. Lifetime co-morbidity of DSM-IV disorders in the US national comorbidity survey replication adolescent supplement (NCS-A). Psychol. Med. 2012, 42, 1997–2010. [Google Scholar] [CrossRef] [PubMed]
- Keenan, K.; Feng, X.; Hipwell, A.; Klostermann, S. Depression begets depression: Comparing the predictive utility of depression and anxiety symptoms to later depression. J. Child Psychol. Psychiatry 2009, 50, 1167–1175. [Google Scholar] [CrossRef]
- Snyder, J.; Bullard, L.; Wagener, A.; Leong, P.K. Childhood Anxiety and Depressive Symptoms: Trajectories, Relationship, and Association with Subsequent Depression. J. Clin. Child Adolesc. Psychol. 2009, 38, 837. [Google Scholar] [CrossRef]
- Hale III, W.W.; Raaijmakers, Q.A.; Muris, P.; Van Hoof, A.; Meeus, W.H. One factor or two parallel processes? Comorbidity and development of adolescent anxiety and depressive disorder symptoms. J. Child Psychol. Psychiatry 2009, 50, 1218–1226. [Google Scholar] [CrossRef] [PubMed]
- Lavigne, J.V.; Lavigne, J.V.; Hopkins, J.; Hopkins, J.; Gouze, K.R.; Gouze, K.R.; Bryant, F.B.; Bryant, F.B. Bidirectional Influences of Anxiety and Depression in Young Children. J. Abnorm. Child Psychol. 2015, 43, 163–176. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Merikangas, K.R.; Avenevoli, S. Epidemiology of mood and anxiety disorders in children and adolescents. In Textbook in Psychiatric Epidemiology; Wiley-Liss: Hoboken, NJ, USA, 2002. [Google Scholar]
- Copeland, W.E.; Wolke, D.; Shanahan, L.; Costello, E.J. Adult functional outcomes of common childhood psychiatric problems: A prospective, longitudinal study. JAMA Psychiatry 2015, 72, 892–899. [Google Scholar] [CrossRef] [PubMed]
- Copeland, W.E.; Alaie, I.; Jonsson, U.; Shanahan, L. Associations of Childhood and Adolescent Depression With Adult Psychiatric and Functional Outcomes. J. Am. Acad. Child Adolesc. Psychiatry 2020. [Google Scholar] [CrossRef]
- Weller, B.E.; Blanford, K.L.; Butler, A.M. Estimated Prevalence of Psychiatric Comorbidities in U.S. Adolescents With Depression by Race/Ethnicity, 2011–2012. J. Adolesc. Health 2018, 62, 716–721. [Google Scholar] [CrossRef]
- Costello, E.J.; Mustillo, S.; Erkanli, A.; Keeler, G. Prevalence and development of psychiatric disorders in childhood and adolescence. Arch. Gen. Psychiatry 2003, 60, 837–844. [Google Scholar] [CrossRef]
- Melton, T.; Croarkin, P.; Strawn, J.; Mcclintock, S. Comorbid Anxiety and Depressive Symptoms in Children and Adolescents: A Systematic Review and Analysis. J. Psychiatr. Pract. 2016, 22, 84–98. [Google Scholar] [CrossRef]
- Avenevoli, S.; Swendsen, J.; He, J.-P.; Burstein, M.; Merikangas, K.R. Major depression in the national comorbidity survey-adolescent supplement: Prevalence, correlates, and treatment. J. Am. Acad. Child Adolesc. Psychiatry 2015, 54, 37. [Google Scholar] [CrossRef]
- Angold, A.; Costello, E.J. Depressive comorbidity in children and adolescents. Am. J. Psychiatry 1993, 150, 1779–1791. [Google Scholar] [PubMed]
- Garber, J.; Weersing, V.R. Comorbidity of Anxiety and Depression in Youth: Implications for Treatment and Prevention. Clin. Psychol. 2010, 17, 293–306. [Google Scholar] [CrossRef] [PubMed]
- Clark, L.A.; Watson, D. Tripartite model of anxiety and depression: Psychometric evidence and taxonomic implications. J. Abnorm. Psychol. 1991, 100, 316. [Google Scholar] [CrossRef] [PubMed]
- Dozois, D.J.; Beck, A.T. Cognitive schemas, beliefs and assumptions. In Risk Factors in Depression; Elsevier: Amsterdam, The Netherlands, 2008; pp. 119–143. [Google Scholar]
- Kranzler, A.; Young, J.F.; Hankin, B.L.; Abela, J.R.; Elias, M.J.; Selby, E.A. Emotional awareness: A transdiagnostic predictor of depression and anxiety for children and adolescents. J. Clin. Child Adolesc. Psychol. 2016, 45, 262–269. [Google Scholar] [CrossRef]
- Schäfer, J.Ö.; Naumann, E.; Holmes, E.A.; Tuschen-Caffier, B.; Samson, A.C. Emotion regulation strategies in depressive and anxiety symptoms in youth: A meta-analytic review. J. Youth Adolesc. 2017, 46, 261–276. [Google Scholar] [CrossRef]
- Ehrenreich, J.T.; Goldstein, C.R.; Wright, L.R.; Barlow, D.H. Development of a Unified Protocol for the Treatment of Emotional Disorders in Youth. Child Fam. Behav. Ther. 2009, 31, 20–37. [Google Scholar] [CrossRef]
- Barlow, D.H.; Allen, L.B.; Choate, M.L. Toward a unified treatment for emotional disorders. Behav. Ther. 2004, 35, 205–230. [Google Scholar] [CrossRef]
- Garber, J.; Brunwasser, S.M.; Zerr, A.A.; Schwartz, K.T.; Sova, K.; Weersing, V.R. Treatment and prevention of depression and anxiety in youth: Test of cross-over effects. Depress. Anxiety 2016, 33, 939–959. [Google Scholar] [CrossRef]
- Van Voorhees, B.W.; Watson, N.; Bridges, J.F.P.; Fogel, J.; Galas, J.; Kramer, C.; Connery, M.; McGill, A.; Marko, M.; Cardenas, A.; et al. Development and pilot study of a marketing strategy for primary care/internet-based depression prevention intervention for adolescents (the CATCH-IT intervention). Prim. Care Companion J. Clin. Psychiatry 2010, 12, PCC.09m00791. [Google Scholar] [CrossRef]
- Gladstone, T.G.; Marko-Holguin, M.; Rothberg, P.; Nidetz, J.; Diehl, A.; DeFrino, D.T.; Harris, M.; Ching, E.; Eder, M.; Canel, J.; et al. An internet-based adolescent depression preventive intervention: Study protocol for a randomized control trial. Trials 2015, 16, 203. [Google Scholar] [CrossRef] [PubMed]
- Van Voorhees, B.W.; Fogel, J.; Reinecke, M.A.; Gladstone, T.; Stuart, S.; Gollan, J.; Bradford, N.; Domanico, R.; Fagan, B.; Ross, R.; et al. Randomized clinical trial of an Internet-based depression prevention program for adolescents (Project CATCH-IT) in primary care: 12-week outcomes. J. Dev. Behav. Pediatrics 2009, 30, 23–37. [Google Scholar] [CrossRef] [PubMed]
- Richards, K.; Marko-Holguin, M.; Fogel, J.; Anker, L.; Ronayne, J.; Van Voorhees, B.W. Randomized clinical trial of an internet-based intervention to prevent adolescent depression in a primary care setting (Catch-It): 2.5-year outcomes. J. Evid. Based Psychother. 2016, 16, 113. [Google Scholar] [PubMed]
- Christensen, H.; Griffiths, K.M. The prevention of depression using the Internet. Med. J. Aust. 2002, 177, S122–S125. [Google Scholar] [CrossRef] [PubMed]
- Ip, P.; Chim, D.; Chan, K.L.; Li, T.M.; Ho, F.K.W.; Van Voorhees, B.W.; Tiwari, A.; Tsang, A.; Chan, C.W.L.; Ho, M. Effectiveness of a culturally attuned Internet-based depression prevention program for Chinese adolescents: A randomized controlled trial. Depress. Anxiety 2016, 33, 1123–1131. [Google Scholar] [CrossRef] [PubMed]
- Van Voorhees, B.G.T.; Sobowale, K.; Brown, C.H.; Aaby, D.; Terrizzi, D.; Canel, J.; Ching, E.; Berry, A.; Cantorna, J. 24-Month Outcomes of Primary Care Web-Based Depression Prevention Intervention in Adolescents: Randomized Clinical Trial. J. Med. Internet Res. 2020, 22. [Google Scholar] [CrossRef]
- Curran, G.M.; Bauer, M.; Mittman, B.; Pyne, J.M.; Stetler, C. Effectiveness-implementation hybrid designs: Combining elements of clinical effectiveness and implementation research to enhance public health impact. Med. Care 2012, 50, 217. [Google Scholar] [CrossRef]
- Mahoney, N.; Gladstone, T.; DeFrino, D.; Stinson, A.; Nidetz, J.; Canel, J.; Ching, E.; Berry, A.; Cantorna, J.; Fogel, J.; et al. Prevention of Adolescent Depression in Primary Care: Barriers and Relational Work Solutions. Calif. J. Health Promot. 2017, 15, 1–12. [Google Scholar] [CrossRef]
- Stuart, S.; Robertson, M. Interpersonal Psychotherapy: A Clinician’s Guide; Oxford University Press: New York, NY, USA, 2003. [Google Scholar]
- Jacobson, N.S.; Martell, C.R.; Dimidjian, S. Behavioral activation treatment for depression: Returning to contextual roots. Clin. Psychol. 2001, 8, 255–270. [Google Scholar] [CrossRef]
- Gagne, R.M.; Briggs, L.J.; Wagner, W. Principles of Instructional Design; HBJ College: Fort Worth, TX, USA, 1992. [Google Scholar]
- Van Voorhees, B.W.; Gladstone, T.; Cordel, S.; Marko-Holguin, M.; Beardslee, W.; Kuwabara, S.; Kaplan, M.A.; Fogel, J.; Diehl, A.; Hansen, C.; et al. Development of a technology-based behavioral vaccine to prevent adolescent depression: A health system integration model. Internet Interv. 2015, 2, 303–313. [Google Scholar] [CrossRef][Green Version]
- Kaufman, J.; Birmaher, B.; Brent, D.; Rao, U.; Flynn, C.; Moreci, P.; Williamson, D.; Ryan, N. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): Initial reliability and validity data. J. Am. Acad. Child Adolesc. Psychiatry 1997, 36, 980–988. [Google Scholar] [CrossRef] [PubMed]
- Radloff, L.S. The use of the Center for Epidemiologic Studies Depression Scale in adolescents and young adults. J. Youth Adolesc. 1991, 20, 149–166. [Google Scholar] [CrossRef] [PubMed]
- Birmaher, B.; Khetarpal, S.; Brent, D.; Cully, M.; Balach, L.; Kaufman, J.; Neer, S.M. The screen for child anxiety related emotional disorders (SCARED): Scale construction and psychometric characteristics. J. Am. Acad. Child Adolesc. Psychiatry 1997, 36, 545–553. [Google Scholar] [CrossRef] [PubMed]
- Silva, R.R.; Alpert, M.; Pouget, E.; Silva, V.; Trosper, S.; Reyes, K.; Dummit, S. A rating scale for disruptive behavior disorders, based on the DSM-IV item pool. Psychiatr. Q. 2005, 76, 327–339. [Google Scholar] [CrossRef] [PubMed]
- Weissman, M.M.; Orvaschel, H.; Padian, N. Children’s symptom and social functioning: Self-report scales. J. Nerv. Ment. Disord. 1980, 168, 736–740. [Google Scholar] [CrossRef]
- Beck, A.T.; Weissman, A.; Lester, D.; Trexler, L. The measurement of pessimism: The hopelessness scale. J. Consult. Clin. Psychol. 1974, 42, 861. [Google Scholar] [CrossRef]
- Schaefer, E.S. A configurational analysis of children’s reports of parent behavior. J. Consult. Psychol. 1965, 29, 552. [Google Scholar] [CrossRef]
- Armitage, C.J.; Conner, M. Efficacy of the theory of planned behaviour: A meta-analytic review. Br. J. Soc. Psychol. 2001, 40, 471–499. [Google Scholar] [CrossRef]
- Prochaska, J.O.; Velicer, W.F.; DiClemente, C.C.; Fava, J. Measuring processes of change: Applications to the cessation of smoking. J. Consult. Clin. Psychol. 1988, 56, 520. [Google Scholar] [CrossRef]
- Hankin, B.L.; Abramson, L.Y. Measuring cognitive vulnerability to depression in adolescence: Reliability, validity, and gender differences. J. Clin. Child Adolesc. Psychol. 2002, 31, 491–504. [Google Scholar] [CrossRef]
- Van Voorhees, B.W.; Vanderplough-Booth, K.; Fogel, J.; Gladstone, T.; Bell, C.; Stuart, S.; Gollan, J.; Bradford, N.; Domanico, R.; Fagan, B. Integrative internet-based depression prevention for adolescents: A randomized clinical trial in primary care for vulnerability and protective factors. J. Can. Acad. Child Adolesc. Psychiatry 2008, 17, 184. [Google Scholar] [PubMed]
- Compton, S.N.; March, J.S.; Brent, D.; Albano, A.M.; Weersing, V.R.; Curry, J. Cognitive-behavioral psychotherapy for anxiety and depressive disorders in children and adolescents: An evidence-based medicine review. J. Am. Acad. Child Adolesc. Psychiatry 2004, 43, 930–959. [Google Scholar] [CrossRef] [PubMed]
- Hudson, J.L.; Rapee, R.M.; Deveney, C.; Schniering, C.A.; Lyneham, H.J.; Bovopoulos, N. Cognitive-behavioral treatment versus an active control for children and adolescents with anxiety disorders: A randomized trial. J. Am. Acad. Child Adolesc. Psychiatry 2009, 48, 533–544. [Google Scholar] [CrossRef] [PubMed]
- Martin, F.; Oliver, T. Behavioural activation for children and young people: A systematic review of progress and promise. Eur. Child Adolesc. Psychiatry 2019, 28, 427–441. [Google Scholar] [CrossRef] [PubMed]
- Gladstone, T.R.; Diehl, A.; Thomann, L.O.; Beardslee, W.R. The Association Between Parental Depression and Child Psychosocial Intervention Outcomes: Directions for Future Research. Harv. Rev. Psychiatry 2019, 27, 241–253. [Google Scholar] [CrossRef] [PubMed]
- Eckshtain, D.; Marchette, L.K.; Schleider, J.; Weisz, J.R. Parental depressive symptoms as a predictor of outcome in the treatment of child depression. J. Abnorm. Child Psychol. 2018, 46, 825–837. [Google Scholar] [CrossRef] [PubMed]
- Legerstee, J.; Huizink, A.; Van Gastel, W.; Liber, J.M.; Treffers, P.; Verhulst, F.C.; Utens, E. Maternal anxiety predicts favourable treatment outcomes in anxiety-disordered adolescents. Acta Psychiatr. Scand. 2008, 117, 289–298. [Google Scholar] [CrossRef]
- Toren, P.; Wolmer, L.; Rosental, B.; Eldar, S.; Koren, S.; Lask, M.; Weizman, R.; Laor, N. Case series: Brief parent-child group therapy for childhood anxiety disorders using a manual-based cognitive-behavioral technique. J. Am. Acad. Child Adolesc. Psychiatry 2000, 39, 1309–1312. [Google Scholar] [CrossRef][Green Version]
- Gordon, M.; Antshel, K.M.; Lewandowski, L. Predictors of treatment outcome in a child and adolescent psychiatry clinic: A naturalistic exploration. Child. Youth Serv. Rev. 2012, 34, 213–217. [Google Scholar] [CrossRef]
- Solanto, M.V. Commentary: Development of a new, much-needed, cognitive-behavioral intervention for adolescents with ADHD–a reflection on Sprich et al.(2016). J. Child Psychol. Psychiatry 2016, 57, 1227–1228. [Google Scholar] [CrossRef]
| Unadjusted Means | Within-Group Slopes 1 | Btw Grp Diff | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Outcome Variables | CATCH-IT (N = 193) | HE (N = 176) | CATCH-IT | HE | ||||||||||
| N | Mean | SD | N | Mean | SD | Time Variable | b | SE | p | b | SE | p | p | |
| SCARED 2 total score (0–82) | Months | −0.13 | (0.06) | 0.04 | −0.11 | (0.06) | 0.07 | 0.79 | ||||||
| Baseline | 171 | 25.5 | (12.7) | 141 | 25.2 | (11.9) | ||||||||
| 2 months | 94 | 26.2 | (13.1) | 90 | 25.7 | (14.3) | ||||||||
| 6 months | 74 | 25.1 | (15.0) | 92 | 24.0 | (13.9) | ||||||||
| 12 months | 83 | 22.4 | (13.0) | 73 | 23.2 | (13.6) | ||||||||
| 18 months | 64 | 25.6 | (13.3) | 81 | 23.2 | (13.4) | ||||||||
| 24 months | 39 | 19.6 | (12.2) | 54 | 20.9 | (13.7) | ||||||||
| CES-D10 (0–30) | Months | −0.06 | (0.02) | 0.01 | −0.04 | (0.02) | 0.10 | 0.44 | ||||||
| Baseline | 190 | 9.5 | (4.5) | 172 | 9.4 | (4.6) | Sqrt (months) | −0.31 | (0.11) | 0.004 | −0.27 | (0.10) | 0.009 | 0.80 |
| 2 months | 123 | 9.2 | (4.2) | 140 | 7.9 | (5.2) | ||||||||
| 6 months | 116 | 8.2 | (4.9) | 133 | 7.9 | (4.7) | ||||||||
| 12 months | 115 | 7.9 | (5.3) | 126 | 7.1 | (4.7) | ||||||||
| 18 months | 67 | 7.9 | (5.9) | 81 | 7.5 | (5.6) | ||||||||
| 24 months | 79 | 7.7 | (5.8) | 103 | 8.1 | (5.6) | ||||||||
| Moderator | N1 | Beta | Standard Error | p2 |
|---|---|---|---|---|
| Sex = male (reference = female) | 362 | 0.16 | 0.19 | 0.41 |
| Race = not white (reference = white) 3 | 362 | 0.14 | 0.18 | 0.43 |
| Ethnicity = Hispanic (reference = not Hispanic) | 362 | −0.17 | 0.25 | 0.50 |
| Site = Boston (reference = Chicago) | 362 | 0.29 | 0.17 | 0.09 |
| Maternal education= college degree (reference = no college degree) | 352 | 0.15 | 0.19 | 0.43 |
| Teen GAS, baseline | 360 | 0.00 | 0.01 | 0.66 |
| Teen CES-D10, baseline | 362 | 0.02 | 0.02 | 0.17 |
| Parent CES-D10, baseline | 332 | −0.05 | 0.02 | 0.004 |
| ADHD (DBD-A), baseline | 196 | 0.12 | 0.26 | 0.64 |
| ODCD (DBD-A), baseline | 193 | 0.28 | 0.52 | 0.59 |
| Social adjustment (SAS-SR), baseline | 212 | 0.15 | 0.23 | 0.51 |
| Hopelessness (BHS), baseline | 270 | −0.01 | 0.03 | 0.74 |
| Maternal acceptance (CRPBI), baseline | 196 | −0.04 | 0.02 | 0.06 |
| Maternal control (CRPBI), baseline | 197 | 0.04 | 0.03 | 0.18 |
| Maternal monitoring (CRPBI), baseline | 187 | −0.10 | 0.06 | 0.12 |
| Paternal acceptance (CRPBI), baseline | 176 | −0.04 | 0.02 | 0.07 |
| Paternal control (CRPBI), baseline | 176 | 0.00 | 0.03 | 0.88 |
| Paternal monitoring (CRPBI), baseline | 170 | −0.04 | 0.04 | 0.25 |
| Positive relationships in primary care, 2 months | 133 | −0.41 | 0.16 | 0.009 |
| Theory of planned behavior, baseline | 164 | −0.47 | 0.25 | 0.06 |
| Stressful life events (LEQ), baseline | 300 | −0.02 | 0.02 | 0.24 |
| Trans-theoretical model, baseline | 191 | −0.07 | 0.05 | 0.12 |
| Teen modules completed | 362 | 0.00 | 0.01 | 0.83 |
| Parent modules completed | 340 | −0.03 | 0.04 | 0.45 |
| Moderator | N1 | Estimate | SE | p2 |
|---|---|---|---|---|
| Sex = male (reference = female) | 369 | 0.06 | 0.33 | 0.86 |
| Race = not white (reference = white) | 369 | 0.54 | 0.30 | 0.07 |
| Ethnicity = Hispanic (reference = not Hispanic) | 369 | −0.09 | 0.38 | 0.81 |
| Site = Boston (reference = Chicago) | 369 | 0.01 | 0.31 | 0.98 |
| Maternal education = college degree (reference = no college degree) | 359 | 0.03 | 0.31 | 0.91 |
| Teen GAS, baseline | 367 | 0.00 | 0.02 | 0.93 |
| Anxiety (SCARED), baseline | 312 | 0.00 | 0.01 | 0.99 |
| Parent CES-D10, baseline | 338 | 0.01 | 0.03 | 0.84 |
| ADHD (DBD-A), baseline | 196 | 1.42 | 0.48 | 0.004 |
| ODCD (DBD-A), baseline | 193 | 2.37 | 0.93 | 0.01 |
| Social adjustment (SAS-SR), baseline | 212 | −0.22 | 0.45 | 0.64 |
| Hopelessness (BHS), baseline | 270 | 0.03 | 0.05 | 0.55 |
| Maternal acceptance (CRPBI), baseline | 196 | −0.04 | 0.05 | 0.40 |
| Maternal control (CRPBI), baseline | 197 | 0.07 | 0.06 | 0.23 |
| Maternal monitoring (CRPBI), baseline | 187 | 0.02 | 0.10 | 0.86 |
| Paternal acceptance (CRPBI), baseline | 176 | −0.05 | 0.04 | 0.21 |
| Paternal control (CRPBI), baseline | 176 | 0.06 | 0.06 | 0.35 |
| Paternal monitoring (CRPBI), baseline | 170 | −0.07 | 0.07 | 0.29 |
| Positive relationships in primary care, 2 months | 134 | −0.60 | 0.30 | 0.046 |
| Theory of planned behavior, baseline | 164 | −0.91 | 0.50 | 0.07 |
| Stressful life events (LEQ), baseline | 302 | 0.05 | 0.03 | 0.10 |
| Trans-theoretical model, baseline | 191 | 0.08 | 0.10 | 0.42 |
| Teen modules completed | 369 | 0.00 | 0.03 | 0.88 |
| Parent modules completed | 346 | −0.05 | 0.08 | 0.52 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gladstone, T.; Buchholz, K.R.; Fitzgibbon, M.; Schiffer, L.; Lee, M.; Voorhees, B.W.V. Randomized Clinical Trial of an Internet-Based Adolescent Depression Prevention Intervention in Primary Care: Internalizing Symptom Outcomes. Int. J. Environ. Res. Public Health 2020, 17, 7736. https://doi.org/10.3390/ijerph17217736
Gladstone T, Buchholz KR, Fitzgibbon M, Schiffer L, Lee M, Voorhees BWV. Randomized Clinical Trial of an Internet-Based Adolescent Depression Prevention Intervention in Primary Care: Internalizing Symptom Outcomes. International Journal of Environmental Research and Public Health. 2020; 17(21):7736. https://doi.org/10.3390/ijerph17217736
Chicago/Turabian StyleGladstone, Tracy, Katherine R. Buchholz, Marian Fitzgibbon, Linda Schiffer, Miae Lee, and Benjamin W. Van Voorhees. 2020. "Randomized Clinical Trial of an Internet-Based Adolescent Depression Prevention Intervention in Primary Care: Internalizing Symptom Outcomes" International Journal of Environmental Research and Public Health 17, no. 21: 7736. https://doi.org/10.3390/ijerph17217736
APA StyleGladstone, T., Buchholz, K. R., Fitzgibbon, M., Schiffer, L., Lee, M., & Voorhees, B. W. V. (2020). Randomized Clinical Trial of an Internet-Based Adolescent Depression Prevention Intervention in Primary Care: Internalizing Symptom Outcomes. International Journal of Environmental Research and Public Health, 17(21), 7736. https://doi.org/10.3390/ijerph17217736





