Perspectives of the Elderly with Mild Cognitive Impairment Living Alone on Participating in a Dementia Prevention Program: A Q Methodology Study
Abstract
1. Introduction
2. Method
2.1. Development of Q-statements
2.2. Participants
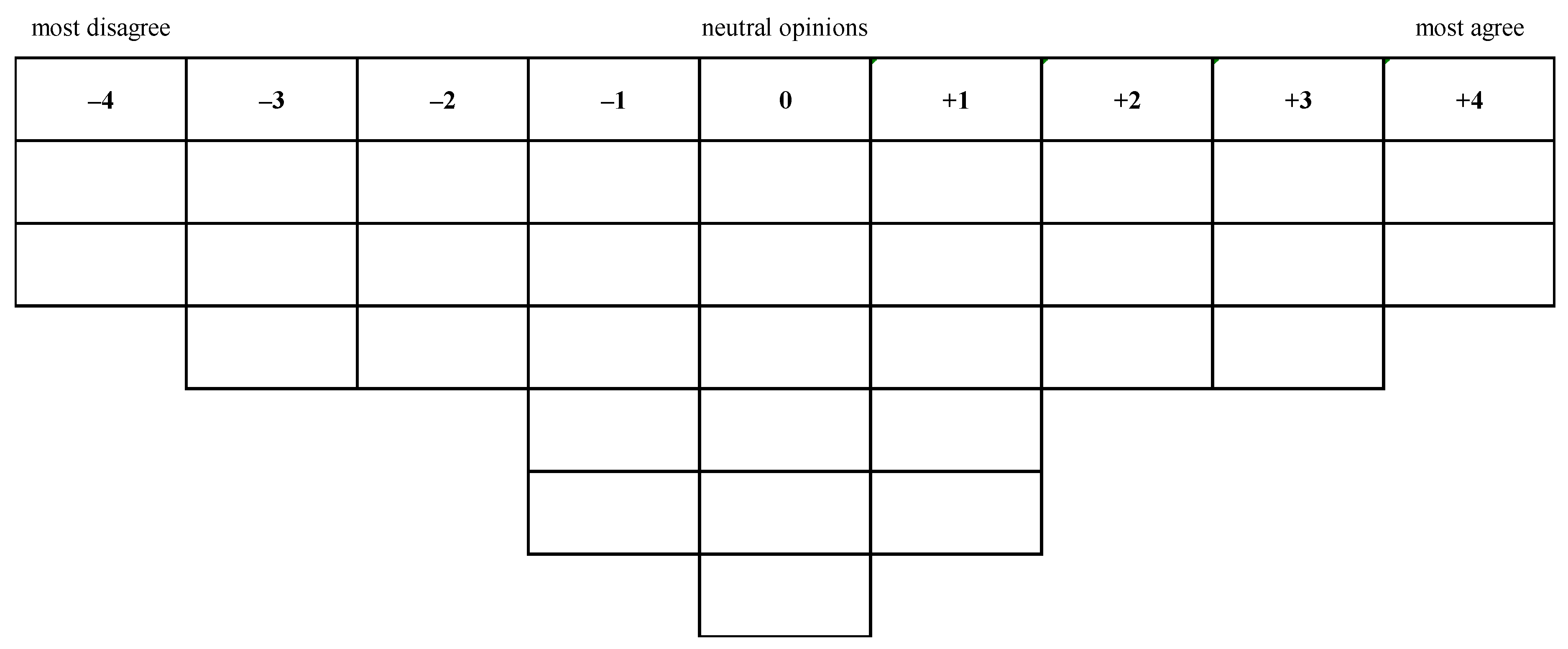
2.3. Q-sorting
2.4. Ethical Considerations
2.5. Data Analysis
3. Results
3.1. Characteristics of Participants
3.2. Factor Analysis
3.3. Group 1: Awareness of Health Benefits and Readiness to Take Preventive Action (Health Promotion)
3.4. Group 2: Emphasis on Cost Considerations and Not Ready to Participate (Cost Considerations)
3.5. Group 3: Concern about Family Attitude and Needing Family Support (Family Ties)
3.6. Group 4: Emphasis on Medical Care and Needing Providers’ Recommendation (Medical Care)
4. Discussion
5. Study Implementations and Limitations
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Department of Statistics. 2018. Available online: https://www.moi.gov.tw/stat/news_detail.aspx?sn=13742 (accessed on 20 July 2020).
- Ministry of Health and Welfare. 2020. Available online: https://dep.mohw.gov.tw/DOS/cp-1721-9411-113.html (accessed on 20 July 2020).
- Chad, K.E.; Reeder, B.A.; Harrison, E.L.; Ashworth, N.L.; Sheppard, S.M.; Schultz, S.L.; Bruner, B.G.; Fisher, K.L.; Lawson, J.A. Profile of physical activity levels in community-dwelling older adults. Med. Sci. Sports Exerc. 2005, 37, 17741–17784. [Google Scholar] [CrossRef]
- Iliffe, S.; Tai, S.S.; Hai, A.; Gallivan, S.; Goldenberg, E.; Booroff, A.; Morgan, P. Are elderly people living alone an at risk group? BMJ 1992, 305, 1001–1004. [Google Scholar] [CrossRef]
- Magaziner, J.; Cadigan, D.A.; Hebel, J.R.; Parry, R.E. Health and living arrangements among older women: Does living alone increases the risk of illness? J. Gerontol. 1998, 43, 127–133. [Google Scholar] [CrossRef]
- Kuiper, J.S.; Zuidersma, M.; Voshaar, R.C.O.; Zuidema, S.U.; van den Heuvel, E.R.; Stolk, R.P.; Smidt, N. Social relationships and risk of dementia: A systematic review and meta-analysis of longitudinal cohort studies. Ageing Res. Rev. 2015, 22, 39–57. [Google Scholar] [CrossRef]
- Taiwan Alzheimer Disease Association. 2020. Available online: http://www.tada2002.org.tw/About/IsntDementia (accessed on 20 July 2020).
- World Health Organization. 2019. Available online: https://www.who.int/news-room/fact-sheets/detail/dementia. (accessed on 20 July 2020).
- Livingston, G.; Sommerlad, A.; Orgeta, V.; Costafreda, S.G.; Huntley, J.; Ames, D.; Ballard, C.; Banerjee, S.; Burns, A.; Cohen-Mansfield, J.; et al. Dementia prevention, intervention, and care. Lancet 2017, 390, 2673–2734. [Google Scholar] [CrossRef]
- McLaren, A.N.; LaMantia, M.A.; Callahan, C.M. Systematic review of non-pharmacologic interventions to delay functional decline in community-dwelling patients with dementia. Aging Ment. Health 2013, 17, 655–666. [Google Scholar] [CrossRef]
- Dannhauser, T.M.; Cleverley, M.; Whitfield, T.J.; Fletcher, B.C.; Stevens, T.; Walker, Z. A complex multimodal activity intervention to reduce the risk of dementia in mild cognitive impairment—ThinkingFit: Pilot and feasibility study for a randomized controlled trial. BMC Psychiatry 2014, 14, 129. [Google Scholar] [CrossRef]
- Fukuma, M.; Shiwaku, K.; Maniwa, R. Cognitive Function Improvement Effect of Old People by Complex-type Dementia Prevention Program. J. Jpn. Assoc. Rural Med. 2014, 63, 606–617. [Google Scholar]
- Lu, L.T. Investigating the subjective needs of community-dwelling older adults for a “cognitive enhancement program”: A study on the formation of Q-statements using in-depth interviews. J. Health Life Success. Aging 2017, 9, 23–35. [Google Scholar]
- Lefebvre, C. Integrating Cell Phones and Mobile Technologies into Public Health Practice: A Social Marketing Perspective. Health Promot. Pract. 2009, 10, 490–494. [Google Scholar] [CrossRef] [PubMed]
- Lauterborn, B. New marketing litany; four P’s passe: C-words take over. Advert. Age 1990, 61, 26. [Google Scholar]
- Blackwell, R.D.; Miniard, P.W.; Engel, J.F. Consumer Behavior, 9th ed.; South-Western Thomas Learning: Mason, OH, USA, 2001. [Google Scholar]
- Chen, S.F.; Huang, S.F.; Lu, L.T.; Wang, M.C.; Liao, J.Y.; Guo, J.L. Patterns of perspectives on fall-prevention beliefs by community-dwelling older adults: A Q method investigation. BMC Geriatr. 2016, 16, 132. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Petit dit Dariel, O.; Wharrad, H.; Windle, R. Developing Q-methodology to explore staff views toward the use of technology in nurse education. Nurse Res. 2010, 18, 58–71. [Google Scholar] [CrossRef]
- Gallagher, K.; Porock, D. The use of interviews in Q methodology: Card content analysis. Nurse Res. 2010, 59, 295–300. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.M.; Hung, W.S.; Lai, J.N.; Kao, Y.H.; Wang, C.L.; Guo, J.L. Maternity staff perspectives regarding resource demands of breastfeeding supportive practices in accordance with the Baby-Friendly Hospital Initiative accreditation: A Q methodology approach. J. Adv. Nurs. 2016, 72, 1301–1312. [Google Scholar] [CrossRef]
- Guo, J.l.; Tu Ku, H.Y.; Yang, F.C.; Hsu, H.p.; Lin, Y.h.; Huang, C.M. Patterns of treatment expectation and the physician–patient relationship perceived by women receiving traditional Chinese medicine treatment for menstrual symptoms: A Q- methodology study. Scand. J. Caring. Sci. 2017, 31, 748–758. [Google Scholar] [CrossRef]
- Huang, S.F.; Huang, C.M.; Chen, S.F.; Lu, L.T.; Guo, J.L. New partnerships among single older adults: A Q methodology study. BMC Geriatr. 2019, 19, 74. [Google Scholar] [CrossRef]
- Huang, C.M.; Liao, J.Y.; Huang, S.F.; Hsu, Y.T.; Hsu, H.P.; Guo, J.L. Patterns of parents’ perspectives on protecting young children from secondhand smoke exposure: A Q-methodology study. J. Adv. Nurs. 2019, 75, 2591–2602. [Google Scholar] [CrossRef]
- Guo, J.L.; Hsu, H.P.; Lin, M.H.; Lin, C.Y.; Huang, C.M. Testing the usability of digital educational games for encouraging smoking cessation. Int. J. Environ. Res. Public Health 2020, 17, 2695. [Google Scholar] [CrossRef]
- Huang, C.M.; Liao, J.Y.; Hsu, H.P.; Lin, C.Y.; Guo, J.L. Perspectives emerged from students and supervisory staff interaction on drug use prevention: A Q-Methodology investigation. Int. J. Environ. Res. Public Health 2020, 17, 5621. [Google Scholar] [CrossRef]
- Sun, Y.; Lee, H.J.; Yang, S.C.; Chen, T.F.; Lin, K.N.; Lin, C.C.; Wang, P.N.; Tang, L.Y.; Chiu, M.J. A nationwide survey of mild cognitive impairment and dementia, including very mild dementia, in Taiwan. PLoS ONE 2014, 9, e100303. [Google Scholar] [CrossRef] [PubMed]
- Webler, T.; Danielson, S.; Tuler, S. Using Q Mthod to Reveal Social Perspectives in Environmental Research. 2009. Available online: www.series.org/pubs/Qprimer.pdf (accessed on 20 January 2011).
- Hämmig, O. Health risks associated with social isolation in general and in young, middle and old age. PLoS ONE 2019, 14, e0219663. [Google Scholar] [CrossRef]
- Rosenberg, P.B.; Mielke, M.M.; Appleby, B.S.; Oh, E.S.; Geda, Y.E.; Lyketsos, C.G. The association of neuropsychiatric symptoms in MCI with incident dementia and Alzheimer disease. Am. J. Geriatr. Psychiatry 2013, 21, 685–695. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Martin, P.; Prieto-Flores, M.E.; Forjaz, M.J.; Fernandez-Mayoralas, G.; Rojo-Perez, F.; Rojo, J.M.; Ayala, A. Components and determinants of quality of life in community-dwelling older adults. Eur. J. Ageing 2012, 9, 255–263. [Google Scholar] [CrossRef]
- Bethancourt, H.J.; Rosenberg, D.E.; Beatty, T.; Arterburn, D.E. Barriers to and facilitators of physical activity program use among older adults. Clin. Med. Res. 2014, 12, 10–20. [Google Scholar] [CrossRef] [PubMed]
- Dickinson, A.; Machen, I.; Horton, K.; Jain, D.; Maddex, T.; Cove, J. Fall prevention in the community: What older people say they need. Br. J. Community Nurs. 2011, 16, 174–180. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bessler, P.; Aung, M.; Jolly, P. Factors affecting uptake of cervical cancer screening among clinic attendees in Trelawny, Jamaica. Cancer Control. 2007, 14, 396–404. [Google Scholar] [CrossRef] [PubMed]
| Interview Questions |
|---|
|
| Variable | All (N = 30) |
|---|---|
| Age, n (%) | |
| under 75 years old | 15 (50.0%) |
| 76–80 years old | 11 (36.7%) |
| over 81 years old | 4 (13.3%) |
| Gender, n (%) | |
| women | 22 (73.3%) |
| men | 8 (26.7%) |
| Marital status, n (%) | |
| ever married | 22 (73.3%) |
| never married | 8 (26.7%) |
| Education level, n (%) | |
| below elementary school | 16 (53.3%) |
| junior or high school | 9 (30.0%) |
| university (college) or above | 5 (16.7%) |
| Economic level, n (%) | |
| not receiving financial assistance | 17 (56.7%) |
| received subsidies from low-income or middle-income | 13 (43.3%) |
| Q-Statement | F1 | F2 | F3 | F4 |
|---|---|---|---|---|
| N = 11 | N = 6 | N = 5 | N = 2 | |
| Attitudes toward participating in a dementia prevention program | ||||
| Concern | ||||
| 1. I worry about memory decline. | 0 | −2 | 2 | −2 |
| 2. I had the experience of a blank brain. | −1 | 0 | −1 | 1 |
| 3. I had experiences of failing to convey meaning and difficulty in expressing myself. | −2 | −1 | 0 | −1 |
| 4. I worry that if I suffer from dementia, my family will need to take care of me. | 1 | −1 | 2 | 0 |
| 5. I am afraid of suffering dementia because I am getting older. | 1 | −2 | 3 | 2 |
| 6. I would like to participate in a dementia prevention program because I have risk factors for dementia (e.g., fall, high blood pressure, high cholesterol, high blood sugar, depression, and inadequate social interaction). | −2 | 0 | 0 | −4 |
| Consumer | ||||
| 7. I think participating in a dementia prevention program can help me find new friends. | 1 | 1 | −1 | 0 |
| 8. I think by participating in a dementia prevention program, I can adequately interact with friends. | 2 | −1 | −2 | 2 |
| 9. I think participating in a dementia prevention program can improve physical and mental health. | 4 | 0 | 1 | −2 |
| 10. I think participating in a dementia prevention program can increase physical activity. | 3 | 1 | 1 | 1 |
| 11. I think participating in a dementia prevention program can increase knowledge. | 3 | −3 | 3 | 3 |
| 12. I think participating in a dementia prevention program can be a good use of my time. | 1 | 0 | 0 | 2 |
| 13. I think participating in a dementia prevention program can maintain my independence. | 2 | 1 | −1 | 3 |
| Cost | ||||
| 14. The distance to travel will influence my participation in a dementia prevention program. | 2 | 4 | 3 | 1 |
| 15. The tuition fees will influence my participation in a dementia prevention program. | 2 | 3 | −2 | −4 |
| 16. The total number of sessions will influence my participation in a dementia prevention program. | −1 | 3 | 0 | 0 |
| 17. The duration of each session will influence my participation in a dementia prevention program. | 0 | 3 | −2 | −1 |
| 18. The medical expenses of suffering dementia will influence my participation in a dementia prevention program. | −1 | 1 | 1 | 4 |
| Convenience | ||||
| 19. The face-to-face teaching methods will influence my participation in a dementia prevention program. | −3 | 2 | −1 | −3 |
| 20. The online teaching methods will influence my participation in a dementia prevention program. | −3 | 2 | 0 | 2 |
| 21. The learning difficulty of the program will influence my participation in a dementia prevention program. | 0 | 2 | −2 | −3 |
| 22. The level of physical load will influence my participation in a dementia prevention program. | 3 | 2 | 2 | 0 |
| Communication | ||||
| 23. I would like to participate in a dementia prevention program because I have learned information about dementia. | −2 | −1 | −1 | 1 |
| 24. I would like to participate in a dementia prevention program because of a friend’s suggestion. | 0 | −3 | −3 | 0 |
| 25. I would like to participate in a dementia prevention program because of the influence of social media. | −4 | −4 | −4 | −1 |
| 26. I would like to participate in a dementia prevention program because of an introduction by the staff of the elderly service center. | −2 | −3 | −3 | 1 |
| 27. I would like to participate in a dementia prevention program because of the advice of providers. | −1 | −1 | 0 | 3 |
| Community | ||||
| 28. I would like to participate in a dementia prevention program because my children expect me to come to class. | −3 | −2 | 4 | −2 |
| 29. I would like to participate in a dementia prevention program because of a friend’s invitation. | 0 | −2 | −3 | 0 |
| 30. I would like to participate in a dementia prevention program because I have actually contacted a dementia patient. | 0 | 0 | 2 | −1 |
| 31. I would like to participate in a dementia prevention program because some family or friend suffers from dementia and I would not like to have dementia like them. | −1 | 1 | 1 | −1 |
| 32. I would like to participate in a dementia prevention program because I would not like to become a burden for significant others. | 1 | 0 | 1 | −2 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lu, L.-T.; Huang, C.-M.; Huang, S.-F.; Wu, S.-I.; Guo, J.-L. Perspectives of the Elderly with Mild Cognitive Impairment Living Alone on Participating in a Dementia Prevention Program: A Q Methodology Study. Int. J. Environ. Res. Public Health 2020, 17, 7712. https://doi.org/10.3390/ijerph17217712
Lu L-T, Huang C-M, Huang S-F, Wu S-I, Guo J-L. Perspectives of the Elderly with Mild Cognitive Impairment Living Alone on Participating in a Dementia Prevention Program: A Q Methodology Study. International Journal of Environmental Research and Public Health. 2020; 17(21):7712. https://doi.org/10.3390/ijerph17217712
Chicago/Turabian StyleLu, Li-Ting, Chiu-Mieh Huang, Su-Fei Huang, Shu-I Wu, and Jong-Long Guo. 2020. "Perspectives of the Elderly with Mild Cognitive Impairment Living Alone on Participating in a Dementia Prevention Program: A Q Methodology Study" International Journal of Environmental Research and Public Health 17, no. 21: 7712. https://doi.org/10.3390/ijerph17217712
APA StyleLu, L.-T., Huang, C.-M., Huang, S.-F., Wu, S.-I., & Guo, J.-L. (2020). Perspectives of the Elderly with Mild Cognitive Impairment Living Alone on Participating in a Dementia Prevention Program: A Q Methodology Study. International Journal of Environmental Research and Public Health, 17(21), 7712. https://doi.org/10.3390/ijerph17217712





