Prevalence and Economic Burden of Respiratory Diseases in Central Asia and Russia: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Protocol and Registration
2.3. Eligibility Criteria
2.4. Information Sources
2.5. Search
2.6. Study Selection
2.7. Data Extraction Process
2.8. Data Items
2.9. Quality Assessment
2.10. Summary Measures
2.11. Synthesis of Results
3. Results
3.1. Study Selection
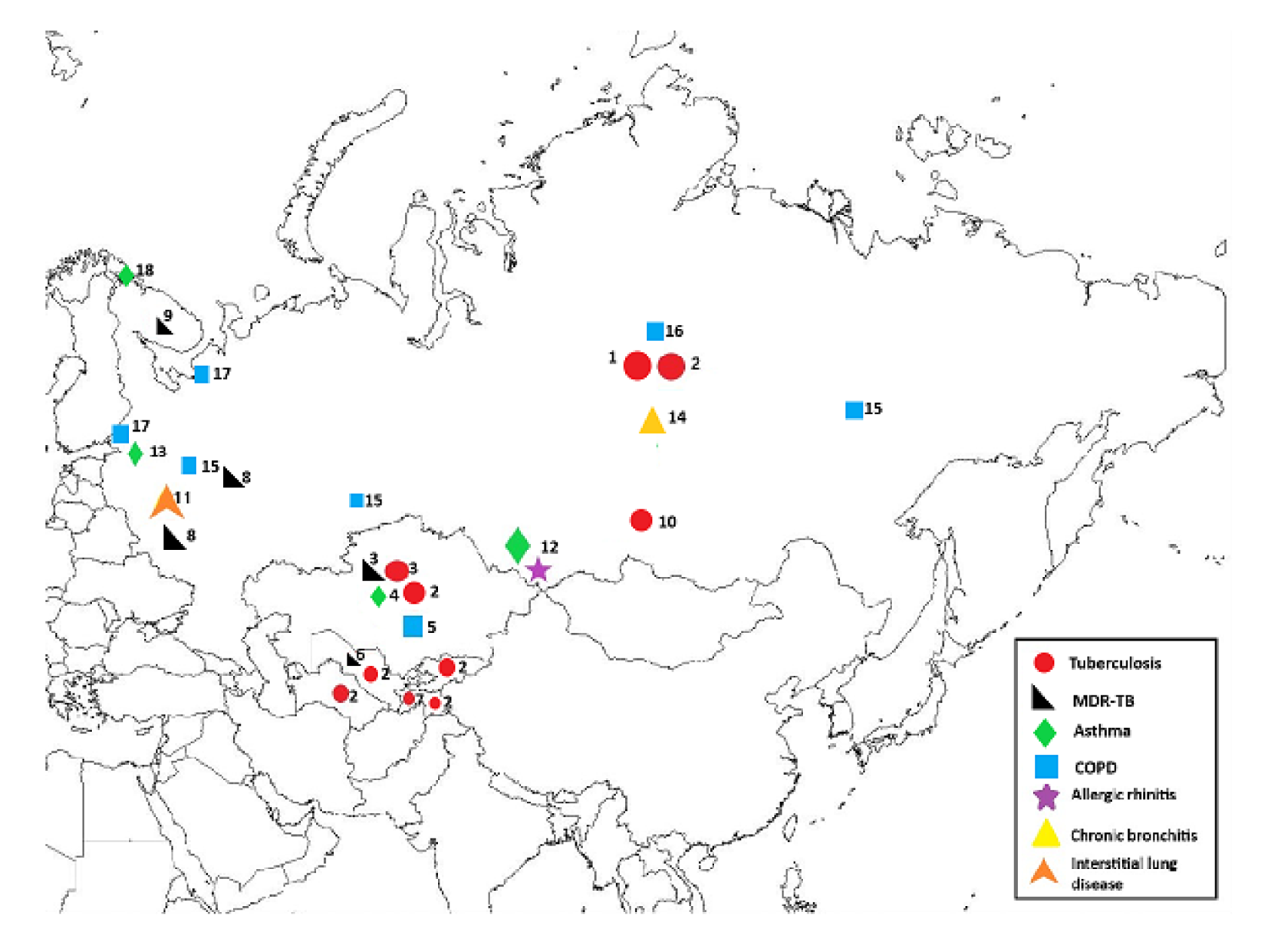
3.2. Prevalence of Respiratory Diseases in Central Asia and Russia
3.3. Economics of Respiratory Diseases in Central Asia and Russia
3.4. Quality of Studies
4. Discussion
4.1. Main Findings
4.2. Interpretation
4.3. Strengths and Limitations
4.4. Recommendations for Future Research and Policy
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Baigenzhin, A. Prevalence of COPD in Kazakhstan. Available online: http://www.who.int/gard/news_events/2_kazakhstan.pdf (accessed on 12 April 2020).
- Brakema, E.A.; Tabyshova, A.; van der Kleij, R.M.; Sooronbaev, T.; Lionis, C.; Anastasaki, M.; An, P.L.; Nguyen, L.T.; Kirenga, B.; Walusimbi, S.; et al. The socioeconomic burden of chronic lung disease in low-resource settings across the globe—An observational FRESH AIR study. Respir. Res. 2019, 20, 291. [Google Scholar] [CrossRef]
- World Health Organization. Chronic Respiratory Diaseases Prevalence in Europe. Available online: http://www.who.int/gard/publications/chronic_respiratory_diseases.pdf (accessed on 12 April 2020).
- World Health Organization. Status of the Health-Related SDGs. Available online: http://www.who.int/gho/publications/world_health_statistics/2018/EN_WHS2018_Part2.pdf?ua=1 (accessed on 12 April 2020).
- Feshchenko, Y.; Iashyna, L.; Nugmanova, D.; Gyrina, O.; Polianska, M.; Markov, A.; Moibenko, M.; Makarova, J.; Tariq, L.; Pereira, M.H.S.; et al. Chronic obstructive pulmonary disease, bronchial asthma and allergic rhinitis in the adult population within the commonwealth of independent states: Rationale and design of the CORE study. BMC Pulm. Med. 2017, 17, 131. [Google Scholar]
- Foo, J.; Landis, S.H.; Maskell, J.; Oh, Y.M.; van der Molen, T.; Han, M.K.; Mannino, D.M.; Ichinose, M.; Punekar, Y. Continuing to Confront COPD International COPD Survey: Economic impact of COPD in 12 counties. PLoS ONE 2016, 11, e0152618. [Google Scholar] [CrossRef]
- Kim, J.; Lee, T.J.; Kim, S.; Lee, E. The economic burden of chronic obstructive pulmonary disease from 2004 to 2013. J. Med. Econ. 2016, 19, 113–120. [Google Scholar] [CrossRef] [PubMed]
- Krysanova, V.; Krysanov, I. Economic Burden in Direct Costs of Chronic Obstructive Pulmonary Disease (COPD) in Russia. Value Health 2014, 17, A593–A594. [Google Scholar] [CrossRef][Green Version]
- PRISMA. Preferred Reporting Items of Systematic Reviews and Meta-Analyses. Available online: http://prisma-statement.org (accessed on 5 March 2020).
- Herzog, R.; Alvarez-Pasquin, M.J.; Diaz, C.; Del Bario, J.L.; Estarda, J.M.; Gil, A. Are healthcare workers’ intentions to vaccinate related to their knowledge, beliefs and attitudes? A systematic review. BMC Public Health 2013, 13, 154. [Google Scholar] [CrossRef]
- van Boven, J.F.; van de Hei, S.J.; Sadatsafavi, M. Making sense of cost-effectiveness analyses in respiratory medicine: A practical guide for non-health economists. Eur. Respir. J. 2019, 53, 1801816. [Google Scholar] [CrossRef]
- Shilova, M.V.; Dye, C. The resurgence of tuberculosis in Russia. Philos. Trans. R. Soc. Lond. Ser. B Biol. Sci. 2001, 356, 1069–1075. [Google Scholar] [CrossRef]
- Kyu, H.H.; Maddison, E.R.; Henry, N.J. The global burden of tuberculosis: Results from the Global Burden of Disease Study 2015. Lancet Infect. Dis. 2018, 18, 261–284. [Google Scholar] [CrossRef]
- Terlikbayeva, A.; Hermosilla, S.; Galea, S.; Schluger, N.; Yegeubayeva, S.; Abildayev, T.; Muminov, T.; Akiyanova, F.; Bartkowiak, L.; Zhumadilov, Z.; et al. Tuberculosis in Kazakhstan: Analysis of risk determinants in national surveillance data. BMC Infect. Dis. 2012, 12, 262. [Google Scholar] [CrossRef]
- Winetsky, D.E.; Almukhamedov, O.; Pulatov, D.; Vezhnina, N.; Dooronbekova, A.; Zhussupov, B. Prevalence, risk factors and social context of active pulmonary tuberculosis among prison inmates in Tajikistan. PLoS ONE 2014, 9, e86046. [Google Scholar] [CrossRef]
- Ulmasova, D.J.; Uzakova, G.; Tillyashayhov, M.N.; Turaev, L.; van Gemert, W.; Dara, M.; Kremer, K.; Gombogaram, T.; Dara, M.; du Cros, P.; et al. Multidrug-resistant tuberculosis in Uzbekistan: Results of a nationwide survey, 2010 to 2011. Eurosurveillance 2013, 18, 42. [Google Scholar] [CrossRef]
- Punga, V.V.; Jakubowiak, W.M.; Danilova, I.D.; Somova, T.R.; Volchenkov, G.V.; Kazionnyy, B.Y.; Nemtsova, E.S.; Kiryanova, E.V.; Kourbatova, E.V. Prevalence of extensively drug-resistant tuberculosis in Vladimir and Orel regions, Russia. Int. J. Tuberc. Lung Dis. 2009, 3, 1309–1312. [Google Scholar]
- Mäkinen, J.; Marjamäki, M.; Haanperä-Heikkinen, M.; Marttila, H.; Endourova, L.B.; Presnova, S.E.; Mathys, V.; Bifani, P.; Ruohonen, R.; Viljanen, M.K.; et al. Extremely high prevalence of multidrug resistant tuberculosis in Murmansk, Russia: A population-based study. Eur. J. Clin. Microbiol. Infect. Dis. 2011, 30, 1119–1126. [Google Scholar] [CrossRef][Green Version]
- Artyukhov, I.; Arshukova, I.; Dobretsova, E.; Dugina, T.; Shulmin, A.; Demko, I. Epidemiology of chronic obstructive pulmonary disease: A population-based study in Krasnoyarsk region, Russia. Int. J. Chronic Obstr. Pulm. Dis. 2015, 10, 1781–1786. [Google Scholar]
- Chuchalin, A.G.; Khaltaev, N.; Antonov, N.S.; Galkin, D.V.; Manakov, L.G.; Antonini, P.; Demko, I.V. Chronic respiratory diseases and risk factors in 12 regions of the Russian Federation. Int. J. Chronic Obstr. Pulm. Dis. 2014, 9, 963–974. [Google Scholar] [CrossRef]
- Gambaryan, M.H.; Shalnova, S.A.; Deev, A.D.; Drapkina, O.M. Chronic Respiratory Diseases in the Regions of Northern Russia: Epidemiological Distinctions in the Results of a National Population Study. Int. J. Environ. Res. Public Health 2017, 14, 841. [Google Scholar] [CrossRef]
- Landis, S.H.; Muellerova, H.; Mannino, D.M.; Menezes, A.M.; Han, M.K.; van der Molen, T.; Davis, K.J. Continuing to Confront COPD International Patient Survey: Methods, COPD prevalence, and disease burden in 2012–2013. Int. J. Chronic Obstr. Pulm. Dis. 2014, 9, 597–611. [Google Scholar]
- Nugmanova, D.; Feshchenko, Y.; Iashyna, L.; Gyrina, O.; Malynovska, K.; Mammadbayov, E.; Vasylyev, A. The prevalence, burden and risk factors associated with chronic obstructive pulmonary disease in Commonwealth of Independent States (Ukraine, Kazakhstan and Azerbaijan): Results of the CORE study. BMC Pulm. Med. 2018, 18, 26. [Google Scholar] [CrossRef]
- Andreeva, E.; Pokhaznikova, M.; Lebedev, A.; Moiseeva, I.; Kutznetsova, O.; Degryse, J.M. The Prevalence of Chronic Obstructive Pulmonary Disease by the Global Lung Initiative Equations in North-Western Russia. Respiration 2016, 91, 43–55. [Google Scholar] [CrossRef] [PubMed]
- Glushkova, A.V.; Grjibovski, A.M. Prevalence and correlates of asthma among children in central St. Petersburg, Russia: Cross-sectional study. Croat. Med. J. 2008, 49, 741–750. [Google Scholar] [CrossRef] [PubMed]
- Nugmanova, D.; Sokolova, L.; Feshchenko, Y.; Iashyna, L.; Gyrina, O.; Malynovska, K.; Tariq, L. The prevalence, burden and risk factors associated with bronchial asthma in commonwealth of independent states countries (Ukraine, Kazakhstan and Azerbaijan): Results of the CORE study. BMC Pulm. Med. 2018, 18, 110. [Google Scholar] [CrossRef] [PubMed]
- Selnes, A.; Odland, J.Ø.; Bolle, R.; Holt, J.; Dotterud, L.K.; Lund, E. Asthma and allergy in Russian and Norwegian schoolchildren: Results from two questionnaire-based studies in the Kola Peninsula, Russia, and northern Norway. Allergy 2001, 56, 344–348. [Google Scholar] [CrossRef] [PubMed]
- Shakhova, N.V.; Kamaltynova, E.M.; Lobanov, Y.F.; Ardatova, T.S.; Nikolaeva, K.S. The prevalence and risk factors of allergic rhinitis among the children of the preschool age. Vestn. Otorinolaryngol. 2017, 82, 47–51. [Google Scholar] [CrossRef]
- Richeldi, L.; Rubin, A.S.; Avdeev, S.; Udwadia, Z.F.; Xu, Z.J. Idiopathic pulmonary fibrosis in BRIC countries: The cases of Brazil, Russia, India, and China. BMC Med. 2015, 13, 237. [Google Scholar] [CrossRef]
- Atun, R.A.; Samyshkin, Y.; Drobniewski, F.; Balabanova, Y.; Fedorin, I.M.; Lord, J.; Coker, R.J. Costs and outcomes of tuberculosis control in the Russian Federation: Retrospective cohort analysis. Health Policy Plan. 2006, 21, 353–365. [Google Scholar] [CrossRef][Green Version]
- Ayé, R.; Wyss, K.; Abdualimova, H.; Saidaliev, S. Factors determining household expenditure for tuberculosis and coping strategies in Tajikistan. Trop. Med. Int. Health 2011, 16, 307–313. [Google Scholar] [CrossRef]
- Skordis-Worrall, J.; Round, J.; Arnold, M.; Abdraimova, A.; Akkazieva, B.; Beran, D. Addressing the double-burden of diabetes and tuberculosis: Lessons from Kyrgyzstan. Glob. Health 2017, 13, 16. [Google Scholar] [CrossRef]
- van den Hof, S.; Collins, D.; Hafidz, F.; Beyene, D.; Tursynbayeva, A.; Tiemersma, E. The socioeconomic impact of multidrug resistant tuberculosis on patients: Results from Ethiopia, Indonesia and Kazakhstan. BMC Infect. Dis. 2016, 16, 470. [Google Scholar] [CrossRef]
- Floyd, K.; Hutubessy, R.; Kliiman, K.; Centis, R.; Khurieva, N.; Jakobowiak, W.; Danilovits, M.; Peremitin, G.; Keshavjee, S.; Migliori, G.B. Cost and cost-effectiveness of multidrug-resistant tuberculosis treatment in Estonia and Russia. Eur. Respir. J. 2012, 40, 133–142. [Google Scholar] [CrossRef]
- Lane, S.; Molina, J.; Plusa, T. An international observational prospective study to determine the Cost Of Asthma eXacerbations (COAX). Respir. Med. 2006, 100, 434–450. [Google Scholar] [CrossRef]
- Tabyshova, A.; Hurst, J.R.; Soriano, J.B.; Checkley, W.; Huang, E.; Trofor, A.C.; Flores-Flores, O.; Alupo, P.; Gianella, G.; Ferdous, T.; et al. Gaps in COPD guidelines of low- and middle-income countries: A systematic scoping review. Chest 2020. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |

| Study (1st Author, Year) | Study Design | Sample Size | Country/Region | Population Characteristics (Age, Gender) | Disease and Disease Characteristics (e.g., Severity) | Disease Prevalence |
|---|---|---|---|---|---|---|
| Shilova et al. [12], 2001 | Retrospective study | 2,512,300 | Russia | Not specified | TB | 245 per 100,000 |
| Kyu et al. [13], 2018 | Model based study | Total national populations | Kazakhstan, Kyrgyzstan, Tajikistan, Turkmenistan, Uzbekistan, Russia | Not specified | TB | * Kazakhstan: 107 per 100,000; Kyrgyzstan: 66 per 100,000; Tajikistan: 54 per 100,000; Turkmenistan: 84 per 100,000; Uzbekistan: 66 per 100,000; Russia: 81 per 100,000 |
| Terlikbaeva et al. [14], 2012 | Epidemiological study | Total national population | Kazakhstan | Not reported | TB and MDR-TB | TB: 166.3 per 100,000 (0.16%) MDR-TB: 61.6 per 100,000 (0.06%) |
| Winetsky et al. [15], 2014 | Cross-sectional study | 1317 | Sughd province, Tajikistan | Prison population Mean age: 36 Male: 100% | Pulmonary TB | 4.5% |
| Ulmasova et al. [16], 2013 | Country wide survey | 1037 | Uzbekistan | Mean age: 60% under 45 years Male: 56% | MDR-TB in TB patients | MDR-TB (new cases): 23.2% MDR-TB (previously treated): 62% |
| Punga et al. [17], 2009 | Cross-sectional retrospective survey | 1882 | Vladimir and Orel regions, Russia | Mean age: 44 Male: 21% | MDR-TB in TB patients | MDR-TB Vladimir: 19% Orel: 20% |
| Mäkinen et al. [18], 2011 | Population-based survey | 1226 | Murmansk region, Russia | Not reported | MDR-TB in TB | MDR-TB (new cases): 26%, MDR-TB (previously treated): 72.9% |
| Artyukhov et al. [19], 2015 | Population-based epidemiological study | 15,000 | Krasnoyarsk region, Russia | Age group: 18 and older | COPD | COPD: 21.2 per 1000 (2%) inhabitants |
| Chuchalin et al. [20], 2014 | Cross-sectional population-based epidemiological study | 7164 | Russia | Mean age: 43.4 Female: 57.2% | Asthma related symptoms, chronic bronchitis, COPD | Asthma related symptoms: 25.7% chronic bronchitis: −8.6%; COPD (extrapolated): 15.3% |
| Gambaryan et al. [21], 2017 | Cross-sectional epidemiological study | 3771 | Vologda, Chelyabinsk, Yakutsk, Russia | Mean age: 48.8 Male: 36.9% Female: 63.1% | COPD | Males: 14.7–12.9%, Females: 15.7% |
| Landis et al. [22], 2014 | Population-based study | 4343 | Russia | Age group: 40–70+ Male: 39% | COPD | Russia, Overall: 9.2%, Males: 11.4%, Females: 8.3% |
| Nugmanova et al. [23], 2018 | Population-based cross-sectional study | 945 | Almaty, Kazakhstan | Mean age: 42.5 (SD: 15.3) Male: 36.8% Female: 63.2% | COPD | 66.7 per 1000 (6.7%) |
| Andreeva et al. [24], 2016 | Population-based cross-sectional study | 3133 | St. Petersburg and Arkhangelsk, Russia | Mean age: 54 (SD: 9.25) Male: 31.8% | COPD | 6.8% |
| Glushkova et al. [25], 2008 | Cross-sectional study | 1464 | St. Petersburg, Russia | Age group: 0–18 Boys: 8.5% Girls: 6.2% | Asthma | 7.4% |
| Nugmanova et al. [26], 2018 | Cross-sectional population-based epidemiological study | 945 | Almaty, Kazakhstan | Mean age: 42.5 (SD 15.3) Male: 36.8% Female: 63.2% | Bronchial asthma |
Doctor diagnosed: 19.5 per 1000 (2%); wheezing symptoms: 254.8 per 1000 (25%) |
| Selnes et al. [27], 2001 | Cross-sectional study | 1143 | Nikel, Russia | Age group: 7–13; Boys: 50% | Asthma | Pediatric asthma: 5.1% |
| Shakhova et al. [28], 2017 | Cross-sectional study | 3205 | Altay region, Russia | Age group: 3–6; Boys: 48.9% | Asthma-like symptoms and allergic rhinitis | Asthma-like symptoms: 11.1%, allergic rhinitis: 18% |
| Richeldi et al. [29], 2015 | Narrative review (extrapolation of survey) | Not reported | Moscow, Russia | Mean age: 60 Male: 66% | Idiopathic pulmonary fibrosis | 9–11 cases per 100,000 population (0.006%) |
| Study (1st Author, Year) | Study Design | Sample Size | Country | Population Characteristics (Age, Gender) | Disease and Disease Characteristics (e.g., Severity) | Economic Impact Data |
|---|---|---|---|---|---|---|
| Atun et al. [30], 2006 | Retrospective cohort study | 2682 | Russia | Mean age females: 38.2 and males: 40.7 Female: 20% Male: 80% | TB | The mean cumulative cost of treating a TB case over 3 years was estimated at US$886. |
| Ayé et al. [31], 2011 | Epidemiological study | 282 | Tajikistan | Age group: 15–45+ | TB | Mean costs for an episode of TB was US$396. |
| Skordis-Worrall et al. [32], 2017 | Cross-sectional study | 309 | Kyrgyzstan | Mean age: 30.28 (12.79) Female: 58.3% | TB | Monthly costs for TB were US$6. |
| van den Hof et al. [33], 2016 | Cross-sectional study | 54 TB and 94 MDR-TB | Kazakhstan | Age group: 21–50+ | TB and MDR-TB | Median costs of DS-TB treatment: US$ 929; MDR-TB treatment: US$ 3125. |
| Floyd et al. [34], 2012 | Retrospective cohort study | 124 | Tomsk oblast, Russia | Mean age: 38 Male: 70% Female: 30% | MDR-TB | Annual per patient cost: US$10,088. |
| Foo et al. [6], 2016 | Cross-sectional, population-based survey | 4343 | Russia | Mean age: 57 | COPD stage I: 26%, stage II: 67%, stage III-IV: 7% | Annual societal cost: US$1721 (direct cost: US$742; indirect cost: US$979). |
| Lane et al. [35], 2006 | Observational study | 100 | Russia | Mean age: 51.1 (SD 14.1) Male: 34% | Asthma (exacerbation) | Direct costs in primary care: €219 (US$^288.9), Secondary care: €693 (US$^914.3). |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tabyshova, A.; Emilov, B.; Postma, M.J.; Chavannes, N.H.; Sooronbaev, T.; van Boven, J.F.M. Prevalence and Economic Burden of Respiratory Diseases in Central Asia and Russia: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 7483. https://doi.org/10.3390/ijerph17207483
Tabyshova A, Emilov B, Postma MJ, Chavannes NH, Sooronbaev T, van Boven JFM. Prevalence and Economic Burden of Respiratory Diseases in Central Asia and Russia: A Systematic Review. International Journal of Environmental Research and Public Health. 2020; 17(20):7483. https://doi.org/10.3390/ijerph17207483
Chicago/Turabian StyleTabyshova, Aizhamal, Berik Emilov, Maarten J. Postma, Niels H. Chavannes, Talant Sooronbaev, and Job F. M. van Boven. 2020. "Prevalence and Economic Burden of Respiratory Diseases in Central Asia and Russia: A Systematic Review" International Journal of Environmental Research and Public Health 17, no. 20: 7483. https://doi.org/10.3390/ijerph17207483
APA StyleTabyshova, A., Emilov, B., Postma, M. J., Chavannes, N. H., Sooronbaev, T., & van Boven, J. F. M. (2020). Prevalence and Economic Burden of Respiratory Diseases in Central Asia and Russia: A Systematic Review. International Journal of Environmental Research and Public Health, 17(20), 7483. https://doi.org/10.3390/ijerph17207483






