Affiliate Stigma and Related Factors in Family Caregivers of Children with Attention-Deficit/Hyperactivity Disorder
Abstract
1. Introduction
1.1. Stigma to Attention-Deficit/Hyperactivity Disorder
1.2. Affiliate Stigma in Caregivers of People with Mental Illness
1.3. Affiliate Stigma in Caregivers of Children with ADHD
1.4. Aims of the Present Study
2. Methods
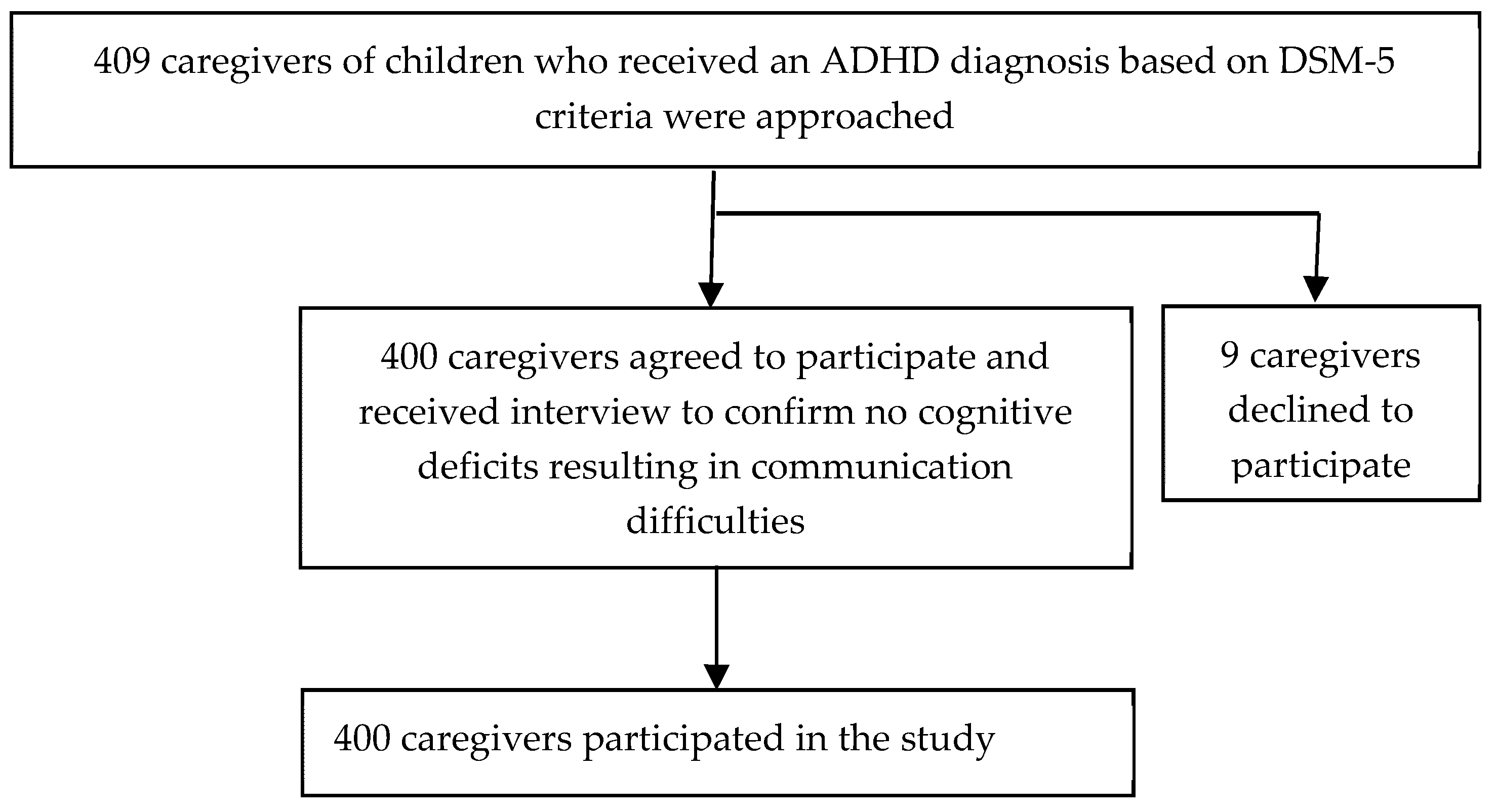
2.1. Participants and Procedure
2.2. Measures
2.2.1. Affiliate Stigma Scale
2.2.2. Caregivers’ Attitudes toward Children’s ADHD
2.2.3. Chinese Version of the SNAP-IV Scale, Parent Form
2.2.4. Caregivers’ and Children’s Factors
2.3. Statistical Analysis
2.4. Ethics
3. Results
4. Discussion
4.1. Components of Affiliate Stigma
4.2. Factors Related to Affiliate Stigma
4.3. Association of Affiliate Stigma with Unfavorable Attitude toward ADHD
4.4. Limitations
4.5. Implications
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Chen, Y.L.; Chen, W.J.; Lin, K.C.; Shen, L.J.; Gau, S.S. Prevalence of DSM-5 mental disorders in a nationally representative sample of children in Taiwan: Methodology and main findings. Epidemiol. Psychiatr. Sci. 2019, 29, e15. [Google Scholar] [CrossRef] [PubMed]
- Paulson, J.F.; Buermeyer, C.; Nelson-Gray, R. Social rejection and ADHD in young adults: An analogue experiment. J. Atten. Disord. 2005, 8, 127–135. [Google Scholar] [CrossRef] [PubMed]
- Martin, J.K.; Pescosolido, B.A.; Olafsdottir, S.; Mcleod, J.D. The construction of fear: Americans’ preferences for social distance from children and adolescents with mental health problems. J. Health Soc. Behav. 2007, 48, 50–67. [Google Scholar] [CrossRef] [PubMed]
- Bussing, R.; Mason, D.M.; Bell, L.; Porter, P.; Garvan, C. Adolescent outcomes of childhood attention-deficit/hyperactivity disorder in a diverse community sample. J. Am. Acad. Child Adolesc. Psychiatry 2010, 49, 595–605. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, R.; Aslani, P. Attention-deficit/hyperactivity disorder: An update on medication adherence and persistence in children, adolescents and adults. Expert Rev. Pharmacoecon. Outcomes Res. 2013, 13, 791–815. [Google Scholar] [CrossRef] [PubMed]
- McKeague, L.; Hennessy, E.; O’Driscoll, C.; Heary, C. Retrospective accounts of self-stigma experienced by young people with attention-deficit/hyperactivity disorder (ADHD) or depression. Psychiatr. Rehabil. J. 2015, 38, 158–163. [Google Scholar] [CrossRef]
- Kellison, I.; Bussing, R.; Bell, L.; Garvan, C. Assessment of stigma associated with attention-deficit hyperactivity disorder: Psychometric evaluation of the ADHD stigma questionnaire. Psychiatry Res. 2010, 178, 363–369. [Google Scholar] [CrossRef]
- Goffman, E. Stigma: Notes on the Management of Spoiled Identity; Prentice-Hall: Englewood Cliffs, NJ, USA, 1963. [Google Scholar]
- Laugesen, B.; Lauritsen, M.B.; Jørgensen, R.; Sørensen, E.E.; Rasmussen, P.; Grønkjær, M. Living with a child with attention deficit hyperactivity disorder: A systematic review. Int. J. Evid. Based Healthc. 2016, 14, 150–165. [Google Scholar] [CrossRef]
- Song, J.; Mailick, M.R.; Greenberg, J.S. Health of parents of individuals with developmental disorders or mental health problems: Impacts of stigma. Soc. Sci. Med. 2018, 217, 152–158. [Google Scholar] [CrossRef]
- dosReis, S.; Barksdale, C.L.; Sherman, A.; Maloney, K.; Charach, A. Stigmatizing experiences of parents of children with a new diagnosis of ADHD. Psychiatr. Serv. 2010, 61, 811–816. [Google Scholar] [CrossRef]
- Koro-Ljungberg, M.; Bussing, R. The management of courtesy stigma in the lives of families with teenagers with ADHD. J. Fam. Issues 2009, 30, 1175–1200. [Google Scholar] [CrossRef]
- Mak, W.W.; Cheung, R.Y.M. Affiliate stigma among caregivers of people with intellectual disability or mental illness. J. Appl. Res. Intellect. Disabil. 2008, 21, 532–545. [Google Scholar] [CrossRef]
- Mak, W.W.S.; Cheung, R.Y.M. Psychological distress and subjective burden of caregivers of people with mental illness: The role of affiliate stigma and face concern. Community Ment. Health J. 2012, 48, 270–274. [Google Scholar] [CrossRef]
- Girma, E.; Möller-Leimkühler, A.M.; Dehning, S.; Mueller, N.; Tesfaye, M.; Froeschl, G. Self-stigma among caregivers of people with mental illness: Toward caregivers’ empowerment. J. Multidiscip. Healthc. 2014, 7, 37–43. [Google Scholar] [CrossRef]
- Ong, H.C.; Ibrahim, N.; Wahab, S. Psychological distress, perceived stigma, and coping among caregivers of patients with schizophrenia. Psychol. Res. Behav. Manag. 2016, 9, 211–218. [Google Scholar] [CrossRef]
- Wu, H.C.; Chen, F.P. Sociocultural factors associated with caregiver-psychiatrist relationship in Taiwan. Psychiatry Investig. 2016, 13, 288–296. [Google Scholar] [CrossRef]
- Shi, Y.; Shao, Y.; Li, H.; Wang, S.; Ying, J.; Zhang, M.; Li, Y.; Xing, Z.; Sun, J. Correlates of affiliate stigma among family caregivers of people with mental illness: A systematic review and meta-analysis. J. Psychiatr. Ment. Health Nurs. 2019, 26, 49–61. [Google Scholar] [CrossRef]
- Chang, C.C.; Su, J.A.; Tsai, C.S.; Yen, C.F.; Liu, J.H.; Lin, C.Y. Rasch analysis suggested three unidimensional domains for Affiliate Stigma Scale: Additional psychometric evaluation. J. Clin. Epidemiol. 2015, 68, 674–683. [Google Scholar] [CrossRef]
- Mikami, A.Y.; Chong, G.K.; Saporito, J.M.; Na, J.J. Implications of parental affiliate stigma in families of children with ADHD. J. Clin. Child Adolesc. Psychol. 2015, 44, 595–603. [Google Scholar] [CrossRef]
- Charbonnier, E.; Caparos, S.; Trémolière, B. The role of mothers’ affiliate stigma and child’s symptoms on the distress of mothers with ADHD children. J. Ment. Health 2019, 28, 282–288. [Google Scholar] [CrossRef]
- Mueller, A.K.; Fuermaier, A.B.M.; Koerts, J.; Tucha, L. Stigma in attention deficit hyperactivity disorder. Atten. Defic. Hyperact. Disord. 2012, 4, 101–114. [Google Scholar] [CrossRef]
- Triandis, H.C. Individualism-collectivism and personality. J. Pers. 2001, 69, 907–924. [Google Scholar] [CrossRef]
- Han, K.H. The feeling of “face” in Confucian society: From a perspective of psychosocial equilibrium. Front. Psychol. 2016, 7, 1055. [Google Scholar] [CrossRef]
- Subcommittee on Attention-Deficit/Hyperactivity Disorder; Steering Committee on Quality Improvement and Management; Wolraich, M.; Brown, L.; Brown, R.T.; DuPaul, G.; Earls, M.; Feldman, H.M.; Ganiats, T.G.; Kaplanek, B.; et al. ADHD: Clinical practice guideline for the diagnosis, evaluation, and treatment in children and adolescents. Pediatrics 2011, 128, 1007–1022. [Google Scholar] [CrossRef]
- Brinkman, W.B.; Sucharew, H.; Majcher, J.H.; Epstein, J.N. Predictors of medication continuity in children with ADHD. Pediatrics 2018, 141, e20172580. [Google Scholar] [CrossRef]
- Bussing, R.; Meyer, J.; Zima, B.T.; Mason, D.M.; Gary, F.A.; Garvan, C.W. Childhood ADHD symptoms: Association with parental social networks and mental health service use during adolescence. Int. J. Environ. Res. Public Health 2015, 12, 11893–11909. [Google Scholar] [CrossRef]
- Ferrin, M.; Ruiz-Veguilla, M.; Blanc-Betes, M.; Abd, S.E.; Lax-Pericall, T.; Sinclair, M.; Taylor, E. Evaluation of attitudes towards treatment in adolescents with attention deficit hyperactivity disorder (ADHD). Eur. Child Adolesc. Psychiatry 2012, 21, 387–401. [Google Scholar] [CrossRef]
- Fiks, A.G.; Mayne, S.; Hughes, C.C.; Debartolo, E.; Behrens, C.; Guevara, J.P.; Power, T. Development of an instrument to measure parents’ preferences and goals for the treatment of attention deficit-hyperactivity disorder. Acad. Pediatr. 2012, 12, 445–455. [Google Scholar] [CrossRef]
- Gajria, K.; Lu, M.; Sikirica, V.; Greven, P.; Zhong, Y.; Qin, P.; Xie, J. Adherence, persistence, and medication discontinuation in patients with attention-deficit/hyperactivity disorder—A systematic literature review. Neuropsychiatr. Dis. Treat. 2014, 10, 1543–1569. [Google Scholar] [CrossRef]
- Gau, S.S.; Shang, C.Y.; Liu, S.K. Psychometric properties of the Chinese version of the Swanson, Nolan, and Pelham, version IV scale—Parent form. Int. J. Methods Psychiatr. Res. 2008, 17, 35–44. [Google Scholar] [CrossRef]
- Swanson, J.M.; Kraemer, H.C.; Hinshaw, S.P.; Arnold, L.E.; Conners, C.K.; Abikoff, H.B.; Clevenger, W.; Davies, M.; Elliott, G.R.; Greenhill, L.L.; et al. Clinical relevance of the primary findings of the MTA: Success rates based on severity of ADHD and ODD symptoms at the end of treatment. J. Am. Acad. Child Adolesc. Psychiatry 2001, 40, 168–179. [Google Scholar] [CrossRef] [PubMed]
- Hwang, Y.J. An analysis of the reliability and validity of the close-ended questionnaire of the occupational survey in the educational research. Bull. Educ. Res. 2005, 51, 43–71. [Google Scholar]
- Hu, H.F.; Liu, T.L.; Hsiao, R.C.; Ni, H.C.; Liang, S.H.Y.; Lin, C.F.; Chan, H.L.; Hsieh, Y.H.; Wang, L.J.; Lee, M.J.; et al. Cyberbullying victimization and perpetration in adolescents with high-functioning autism spectrum disorder: Correlations with depression, anxiety, and suicidality. J. Autism Dev. Disord. 2019, 49, 4170–4180. [Google Scholar] [CrossRef] [PubMed]
- Baron, R.M.; Kenny, D.A. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J. Pers. Soc. Psychol. 1986, 51, 1173–1182. [Google Scholar] [CrossRef] [PubMed]
- Corrigan, P.W.; Watson, A.C. The paradox of self-stigma and mental illness. Clin. Psychol. Sci. Pract. 2002, 9, 35–53. [Google Scholar] [CrossRef]
- Huang, C.H.; Li, S.M.; Shu, B.C. Exploring the relationship between illness perceptions and negative emotions in relatives of people with schizophrenia within the context of an affiliate stigma model. J. Nurs. Res. 2016, 24, 217–223. [Google Scholar] [CrossRef] [PubMed]
- Kohlhoff, J.; Barnett, B. Parenting self-efficacy: Links with maternal depression, infant behaviour and adult attachment. Early Hum. Dev. 2013, 89, 249–256. [Google Scholar] [CrossRef]
- Gau, S.S.; Chang, J.P. Maternal parenting styles and mother-child relationship among adolescents with and without persistent attention-deficit/hyperactivity disorder. Res. Dev. Disabil. 2013, 34, 1581–1594. [Google Scholar] [CrossRef]
- Lee, P.C.; Lin, K.C.; Robson, D.; Yang, H.J.; Chen, V.C.; Niew, W.I. Parent-child interaction of mothers with depression and their children with ADHD. Res. Dev. Disabil. 2013, 34, 656–668. [Google Scholar] [CrossRef]
- Chang, C.C.; Yen, C.F.; Jang, F.L.; Su, J.A.; Lin, C.Y. Comparing affiliate stigma between family caregivers of people with different severe mental illness in Taiwan. J. Nerv. Ment. Dis. 2017, 205, 542–549. [Google Scholar] [CrossRef]
- Fernando, S.M.; Deane, F.P.; McLeod, H.J.; Davis, E.L. A carer burden and stigma in schizophrenia and affective disorders: Experiences from Sri Lanka. Asian J. Psychiatr. 2017, 26, 77–81. [Google Scholar] [CrossRef]
- Greenberg, J.S.; Kim, H.W.; Greenley, J.R. Factors associated with subjective burden in siblings of adults with severe mental illness. Am. J. Orthopsychiatry 1997, 67, 231–241. [Google Scholar] [CrossRef]
- Tang, C.S.; Chua, Z.; O, J. A gender perspective on Chinese social relationships and behavior. In The Oxford Handbook of Chinese Psychology; Bond, M.H., Ed.; Oxford University Press: New York, NY, USA, 2010; pp. 533–553. [Google Scholar]
- Ohan, J.L.; Visser, T.A.; Moss, R.G.; Allen, N.B. Parents’ stigmatizing attitudes toward psychiatric labels for ADHD and depression. Psychiatr. Serv. 2013, 64, 1270–1273. [Google Scholar] [CrossRef]
- Pescosolido, B.A.; Jensen, P.S.; Martin, J.K.; Perry, B.L.; Olafsdottir, S.; Fettes, D. Public knowledge and assessment of child mental health problems: Findings from the national stigma study-children. J. Am. Acad. Child Adolesc. Psychiatry 2008, 47, 339–349. [Google Scholar] [CrossRef]
- Fausett, Y.M. Elementary School Children’s Stigmatization of Children with Mental Illness. Master’s Thesis, University of Rhode Island, Kingston, RI, USA, 2003. [Google Scholar]
- Lai, M.; Bond, M.H. Gender stereotypes and the self-concept in Hong Kong youth. Bull. Hong Kong Psychol. Soc. 1997, 38/39, 17–36. [Google Scholar]
- Che, X.; Tse, H.C. Social functioning and adjustment in Canada-born children with Chinese and European background. Dev. Psychol. 2008, 44, 1184–1189. [Google Scholar] [CrossRef]
- Taylor, L.E.; Antshel, K.M. Factors associated with parental treatment attitudes and information-seeking behaviors for childhood ADHD. J. Atten. Disord. 2019, 9, 1087054718821734. [Google Scholar] [CrossRef]
- Singh, I.; Filipe, A.M.; Bard, I.; Bergey, M.; Baker, L. Globalization and cognitive enhancement: Emerging social and ethical challenges for ADHD clinicians. Curr. Psychiatry Rep. 2013, 15, 385. [Google Scholar] [CrossRef]
- Wan, E.S.F.; Ma, J.L.C.; Lai, K.Y.C.; Lo, J.W.K. The subjective experiences of attention-deficit/hyperactivity disorder of Chinese families in Hong Kong: Co-construction of meanings in multiple family groups. Health Soc. Work 2016, 41, 164–172. [Google Scholar] [CrossRef]
| Variables | n (%) | Mean (SD) | Range |
|---|---|---|---|
| Caregivers | |||
| Relationship with the child | |||
| Mother | 287 (71.8) | ||
| Father | 90 (22.5) | ||
| Others | 23 (5.8) | ||
| Age (years) | 43.4 (6.8) | 25–70 | |
| Sex | |||
| Female | 304 (76.0) | ||
| Male | 96 (24.0) | ||
| Education (years) | 13.8 (2.9) | 3–23 | |
| Parental marriage status | |||
| Married | 320 (80) | ||
| Divorced or separated | 80 (20) | ||
| Occupational socioeconomic status | |||
| High | 155 (38.8) | ||
| Low | 245 (61.2) | ||
| Frequency of attending religious activities | |||
| High | 143 (35.8) | ||
| Low | 257 (64.3) | ||
| Level of affiliate stigma | |||
| Affect | 2.1 (0.7) | 1–4 | |
| Cognition | 1.6 (0.5) | 1–3.4 | |
| Behavior | 1.6 (0.5) | 1–3.5 | |
| Total | 1.8 (0.5) | 1–3.4 | |
| Unfavorable attitude toward children’s ADHD | |||
| Diagnosis | 173 (43.3) | ||
| Pharmacotherapy | 180 (45) | ||
| Behavioral therapy | 112 (28) | ||
| Biological explanation for etiologies | 108 (27) | ||
| Children | |||
| Age (years) | 10.7 (3.2) | 4–18 | |
| Sex | |||
| Girls | 64 (16.0) | ||
| Boys | 336 (84.0) | ||
| Education | |||
| Primary school or kindergarten | 355 (88.8) | ||
| High school | 45 (11.3) | ||
| ADHD symptoms on the SNAP-IV | |||
| Inattention | 13.4 (3.6) | 0–27 | |
| Hyperactivity/impulsivity | 9.8 (6.0) | 0–27 | |
| Opposition defiance | 10.1 (6.0) | 0–24 |
| Variables | Model I | Model II | ||||
|---|---|---|---|---|---|---|
| Beta | t | p | Beta | t | p | |
| Caregivers factors | ||||||
| Sex (0: female; 1: male) | −0.102 | −1.987 | 0.048 | −0.073 | −1.468 | 0.143 |
| Age | 0.053 | 1.015 | 0.311 | 0.085 | 1.624 | 0.105 |
| Education level | 0.136 | 2.457 | 0.014 | 0.112 | 2.102 | 0.036 |
| Marriage status (0: married; 1: divorced or separated) | −0.029 | −0.572 | 0.568 | −0.040 | −0.830 | 0.407 |
| Frequency of attending religious activities (0: high; 1: low) | 0.088 | 1.744 | 0.082 | 0.087 | 1.799 | 0.073 |
| Occupational socioeconomic status (0: high; 1: low) | 0.084 | 1.541 | 0.124 | 0.034 | 0.643 | 0.521 |
| Children’s factors | ||||||
| Sex (0: girl; 1: boy) | −0.122 | −2.522 | 0.012 | |||
| Age | 0.052 | 0.964 | 0.336 | |||
| Inattention | 0.253 | 4.284 | <0.001 | |||
| Hyperactivity/impulsivity | 0.030 | 0.451 | 0.652 | |||
| Opposition defiance | 0.027 | 0.423 | 0.672 | |||
| Variables | Diagnosis | Pharmacotherapy | Behavioral Therapy | Biological Explanation for Etiologies | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wals χ2 | p | OR (95% CI) | Wals χ2 | p | OR (95% CI) | Wals χ2 | p | OR (95% CI) | Wals χ2 | p | OR (95% CI) | |
| Caregivers’ sex | 1.667 | 0.197 | 0.707 (0.418–1.197) | 0.056 | 0.814 | 1.062 (0.644–1.753) | 2.893 | 0.089 | 1.614 (0.930–2.803) | 0.006 | 0.936 | 0.977 (0.545–1.751) |
| Caregivers’ age | 1.420 | 0.233 | 0.979 (0.946–1.014) | 2.112 | 0.146 | 0.975 (0.943–1.009) | 3.614 | 0.057 | 0.963 (0.927–1.001) | 3.254 | 0.071 | 0.964 (0.927–1.003) |
| Parental education level | 6.160 | 0.013 | 0.900 (0.828–0.978) | 0.938 | 0.333 | 0.962 (0.889–1.041) | 1.250 | 0.263 | 0.950 (0.868–1.039) | 1.815 | 0.178 | 0.939 (0.856–1.029) |
| Caregivers’ marriage status | 0.016 | 0.899 | 0.966 (0.564–1.653) | 0.280 | 0.597 | 0.868 (0.515–1.464) | 0.694 | 0.405 | 0.771 (0.418–1.422) | 1.432 | 0.232 | 0.680 (0.361–1.279) |
| Caregivers’ frequency of religious activities | 0.008 | 0.930 | 0.980 (0.625–1.537) | 0.022 | 0.883 | 1.033 (0.668–1.597) | 0.346 | 0.557 | 1.161 (0.706–1.908) | 1.295 | 0.255 | 1.345 (0.807–2.241) |
| Caregivers’ socioeconomic status | 0.227 | 0.634 | 1.124 (0.695–1.818) | 0.105 | 0.746 | 0.926 (0.580–1.477) | 0.202 | 0.653 | 1.129 (0.665–1.917) | 0.180 | 0.671 | 1.124 (0.656–1.925) |
| Children’s sex | 0.135 | 0.713 | 1.115 (0.625–1.989) | 0.074 | 0.785 | 0.924 (0.524–1.631) | 0.059 | 0.808 | 1.080 (0.579–2.016) | 0.103 | 0.748 | 0.904 (0.488–1.676) |
| Children’s age | 5.071 | 0.024 | 0.917 (0.850–0.989) | 1.469 | 0.226 | 0.956 (0.889–1.028) | 0.988 | 0.320 | 1.042 (0.961–1.129) | 0.009 | 0.924 | 1.004 (0.925–1.090) |
| Inattention | 0.547 | 0.460 | 0.982 (0.936–1.031) | 0.014 | 0.905 | 1.003 (0.957–1.051) | 0.394 | 0.530 | 0.983 (0.933–1.036) | 0.491 | 0.484 | 0.981 (0.930–1.035) |
| Hyperactivity/impulsivity | 3.689 | 0.055 | 0.952 (0.905–1.001) | 0.217 | 0.642 | 0.989 (0.942–1.037) | 1.339 | 0.247 | 0.968 (0.916–1.023) | 0.386 | 0.534 | 1.018 (0.963–1.076) |
| Opposition defiance | 0.000 | 0.985 | 1.000 (0.955–1.049) | 0.055 | 0.814 | 0.995 (0.950–1.041) | 0.877 | 0.349 | 0.976 (0.927–1.027) | 3.161 | 0.075 | 0.953 (0.904–1.005) |
| Affiliate stigma | 31.984 | <0.001 | 3.888 (2.429–6.225) | 21.410 | <0.001 | 2.862 (1.833–4.468) | 26.033 | <0.001 | 3.667 (2.226–6.040) | 25.932 | <0.001 | 3.800 (2.273–6.352) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chang, C.-C.; Chen, Y.-M.; Liu, T.-L.; Hsiao, R.C.; Chou, W.-J.; Yen, C.-F. Affiliate Stigma and Related Factors in Family Caregivers of Children with Attention-Deficit/Hyperactivity Disorder. Int. J. Environ. Res. Public Health 2020, 17, 576. https://doi.org/10.3390/ijerph17020576
Chang C-C, Chen Y-M, Liu T-L, Hsiao RC, Chou W-J, Yen C-F. Affiliate Stigma and Related Factors in Family Caregivers of Children with Attention-Deficit/Hyperactivity Disorder. International Journal of Environmental Research and Public Health. 2020; 17(2):576. https://doi.org/10.3390/ijerph17020576
Chicago/Turabian StyleChang, Chih-Cheng, Yu-Min Chen, Tai-Ling Liu, Ray C. Hsiao, Wen-Jiun Chou, and Cheng-Fang Yen. 2020. "Affiliate Stigma and Related Factors in Family Caregivers of Children with Attention-Deficit/Hyperactivity Disorder" International Journal of Environmental Research and Public Health 17, no. 2: 576. https://doi.org/10.3390/ijerph17020576
APA StyleChang, C.-C., Chen, Y.-M., Liu, T.-L., Hsiao, R. C., Chou, W.-J., & Yen, C.-F. (2020). Affiliate Stigma and Related Factors in Family Caregivers of Children with Attention-Deficit/Hyperactivity Disorder. International Journal of Environmental Research and Public Health, 17(2), 576. https://doi.org/10.3390/ijerph17020576






