Family Income Gradients in Adolescent Obesity, Overweight and Adiposity Persist in Extremely Deprived and Extremely Affluent Neighbourhoods but Not in Middle-Class Neighbourhoods: Evidence from the UK Millennium Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Sources
2.2. Measures
2.2.1. Anthropometric and Body Fat Measures
2.2.2. Family Income
2.2.3. Geographic-Level Deprivation
2.2.4. Covariates
2.3. Statistical Analysis
2.4. Ethical Consideration
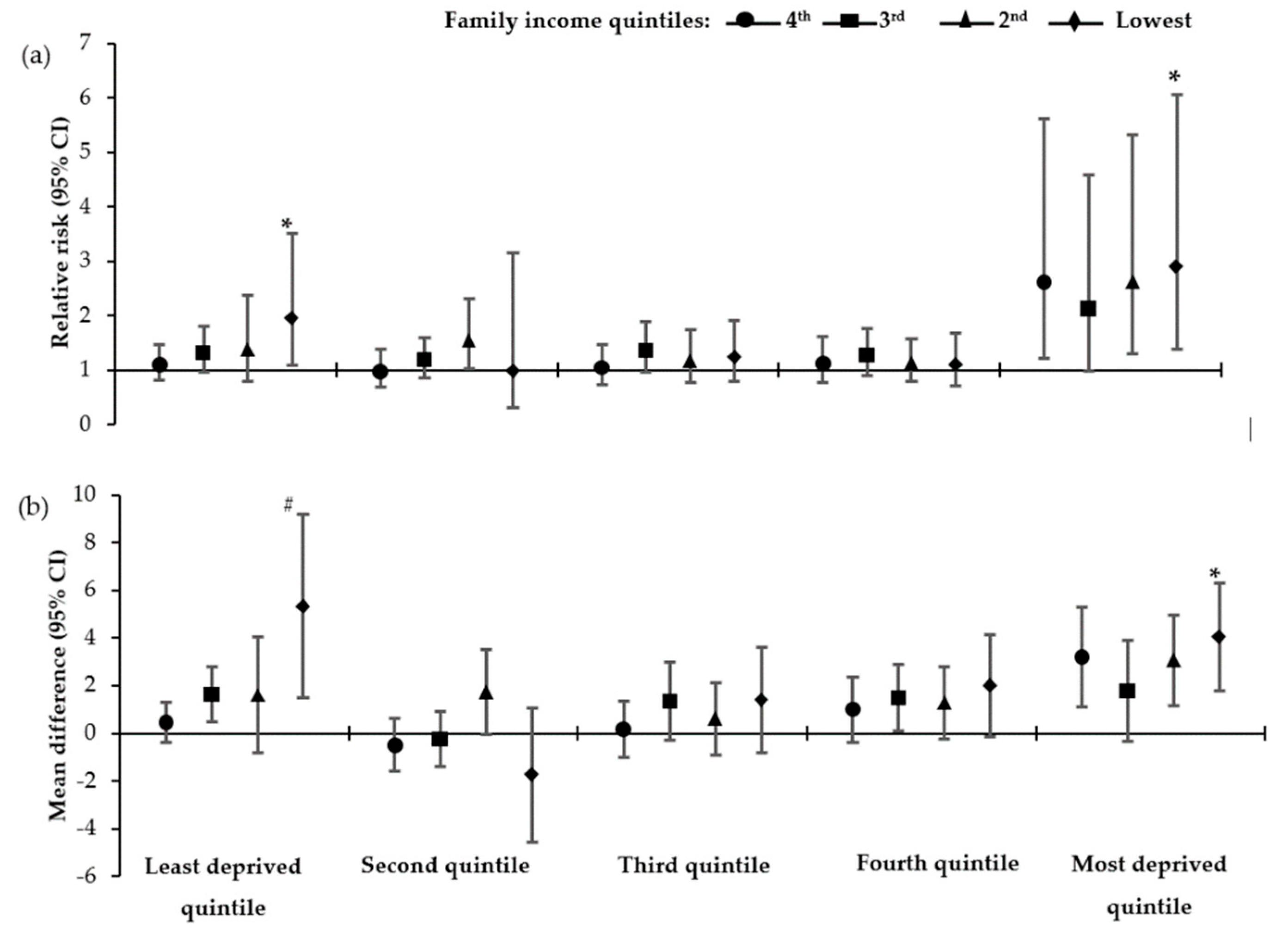
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- The GBD 2015 Obesity Collaborators; Afshin, A.; Forouzanfar, M.H.; Reitsma, M.B.; Sur, P.; Estep, K.; Lee, A.; Marczak, L.; Mokdad, A.H.; Moradi-Lakeh, M.; et al. Health Effects of Overweight and Obesity in 195 Countries over 25 Years. N. Engl. J. Med. 2017, 377, 13–27. [Google Scholar] [CrossRef] [PubMed]
- Abarca-Gómez, L.; Abdeen, Z.A.; Hamid, Z.A.; Abu-Rmeileh, N.M.; Acosta-Cazares, B.; Acuin, C.; Adams, R.J.; Aekplakorn, W.; Afsana, K.; Aguilar-Salinas, C.A.; et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet 2017, 390, 2627–2642. [Google Scholar] [CrossRef]
- World Health Organisation Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 13 November 2019).
- Stamatakis, E.; Wardle, J.; Cole, T.J. Childhood obesity and overweight prevalence trends in England: Evidence for growing socioeconomic disparities. Int. J. Obes. 2010, 34, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Franks, P.W.; Hanson, R.L.; Knowler, W.C.; Sievers, M.L.; Bennett, P.H.; Looker, H.C. Childhood Obesity, Other Cardiovascular Risk Factors, and Premature Death. Available online: https://www.nejm.org/doi/10.1056/NEJMoa0904130?url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org&rfr_dat=cr_pub%3Dwww.ncbi.nlm.nih.gov (accessed on 22 December 2019).
- Dietz, W.H. Health Consequences of Obesity in Youth: Childhood Predictors of Adult Disease. Pediatrics 1998, 101, 518–525. [Google Scholar] [PubMed]
- Kantomaa, M.T.; Stamatakis, E.; Kankaanpää, A.; Kaakinen, M.; Rodriguez, A.; Taanila, A.; Ahonen, T.; Järvelin, M.-R.; Tammelin, T. Physical activity and obesity mediate the association between childhood motor function and adolescents’ academic achievement. Proc. Natl. Acad. Sci. USA 2013, 110, 1917–1922. [Google Scholar] [CrossRef]
- Guo, S.S.; Chumlea, W.C. Tracking of body mass index in children in relation to overweight in adulthood. Am. J. Clin. Nutr. 1999, 70, 145S–148S. [Google Scholar] [CrossRef]
- Friedemann, C.; Heneghan, C.; Mahtani, K.; Thompson, M.; Perera, R.; Ward, A.M. Cardiovascular disease risk in healthy children and its association with body mass index: Systematic review and meta-analysis. BMJ 2012, 345, e4759. [Google Scholar] [CrossRef]
- Franks, P.W.; Hanson, R.L.; Knowler, W.C.; Moffett, C.; Enos, G.; Infante, A.M.; Krakoff, J.; Looker, H.C. Childhood Predictors of Young-Onset Type 2 Diabetes. Diabetes 2007, 56, 2964–2972. [Google Scholar] [CrossRef]
- Celermajer, D.S.; Ayer, J.G.J. Childhood risk factors for adult cardiovascular disease and primary prevention in childhood. Heart 2006, 92, 1701–1706. [Google Scholar] [CrossRef]
- Evans, G.W.; Jones-Rounds, M.L.; Belojevic, G.; Vermeylen, F. Family income and childhood obesity in eight European cities: The mediating roles of Neighborhood characteristics and physical activity. Soc. Sci. Med. 2012, 75, 477–481. [Google Scholar] [CrossRef]
- Massion, S.; Wickham, S.; Pearce, A.; Barr, B.; Law, C.; Taylor-Robinson, D. Exploring the impact of early life factors on inequalities in risk of overweight in UK children: Findings from the UK Millennium Cohort Study. Arch. Dis. Child. 2016, 101, 724–730. [Google Scholar] [CrossRef] [PubMed]
- Ogden, C.L.; Carroll, M.D.; Fakhouri, T.H.; Hales, C.M.; Fryar, C.D.; Li, X.; Freedman, D.S. Prevalence of Obesity Among Youths by Household Income and Education Level of Head of Household—United States 2011–2014. MMWR Morb. Mortal. Wkly. Rep. 2018, 67, 186–189. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Lim, H. The global childhood obesity epidemic and the association between socio-economic status and childhood obesity. Int. Rev. Psychiatry 2012, 24, 176–188. [Google Scholar] [CrossRef]
- Albuquerque, D.; Nóbrega, C.; Manco, L.; Padez, C. The contribution of genetics and environment to obesity. Br. Med. Bull. 2017, 123, 159–173. [Google Scholar] [CrossRef] [PubMed]
- Kinra, S.; Nelder, R.P.; Lewendon, G.J. Deprivation and childhood obesity: A cross sectional study of 20 973 children in Plymouth, United Kingdom. J. Epidemiol. Community Health 2000, 54, 456–460. [Google Scholar] [CrossRef]
- Dinsa, G.; Goryakin, Y.; Fumagalli, E.; Suhrcke, M. Obesity and socioeconomic status in developing countries: A systematic review. Obes. Rev. 2012, 13, 1067–1079. [Google Scholar] [CrossRef]
- Noonan, R.J. Prevalence of Childhood Overweight and Obesity in Liverpool between 2006 and 2012: Evidence of Widening Socioeconomic Inequalities. Int. J. Environ. Res. Public Health 2018, 15, 2612. [Google Scholar] [CrossRef]
- Connelly, R.; Platt, L. Cohort Profile: UK Millennium Cohort Study (MCS). Int. J. Epidemiol. 2014, 43, 1719–1725. [Google Scholar] [CrossRef]
- University of London, Institute of Education, Centre for Longitudinal Studies. Millennium Cohort Study: Sixth Survey, 4th ed.; University of London: London, UK, 2018. [Google Scholar]
- Cole, T.J.; Bellizzi, M.C.; Flegal, K.M.; Dietz, W.H. Establishing a standard definition for child overweight and obesity worldwide: International survey. BMJ 2000, 320, 1240. [Google Scholar] [CrossRef] [PubMed]
- Hansen, K. Millennium Cohort Study: First, Second, Third and Fourth Surveys, 7th ed.; Centre for Longitudinal Studies: London, UK, 2012. [Google Scholar]
- Fitzsimons, E. Millennium Cohort Study Sixth Survey 2015-2016 User Guide, 1st ed.; Center for Longitudinal Studies: London, UK, 2017. [Google Scholar]
- Lissner, L.; Wijnhoven, T.M.A.; Mehlig, K.; Sjöberg, A.; Kunesova, M.; Yngve, A.; Petrauskiene, A.; Duleva, V.; Rito, A.I.; Breda, J. Socioeconomic inequalities in childhood overweight: Heterogeneity across five countries in the WHO European Childhood Obesity Surveillance Initiative (COSI–2008). Int. J. Obes. (Lond.) 2016, 40, 796–802. [Google Scholar] [CrossRef]
- Pearce, A.; Dundas, R.; Whitehead, M.; Taylor-Robinson, D. Pathways to inequalities in child health. Arch. Dis. Child. 2019, 104, 998–1003. [Google Scholar] [CrossRef] [PubMed]
- Walsh, B.; Cullinan, J. Decomposing socioeconomic inequalities in childhood obesity: Evidence from Ireland. Econ. Hum. Biol. 2015, 16, 60–72. [Google Scholar] [CrossRef] [PubMed]
- Pearce, A.; Hope, S.; Griffiths, L.; Cortina-Borja, M.; Chittleborough, C.; Law, C. What if all children achieved WHO recommendations on physical activity? Estimating the impact on socioeconomic inequalities in childhood overweight in the UK Millennium Cohort Study. Int. J. Epidemiol. 2019, 48, 134–147. [Google Scholar] [CrossRef] [PubMed]
- Ip, P.; Ho, F.K.W.; So, H.-K.; Chan, D.F.; Ho, M.; Tso, W.; Nelson, E.A.S. Socioeconomic Gradient in Childhood Obesity and Hypertension: A Multilevel Population-Based Study in a Chinese Community. PLoS ONE 2016, 11, e0156945. [Google Scholar] [CrossRef]
- Magnusson, M.; Sørensen, T.I.A.; Olafsdottir, S.; Lehtinen-Jacks, S.; Holmen, T.L.; Heitmann, B.L.; Lissner, L. Social Inequalities in Obesity Persist in the Nordic Region Despite Its Relative Affluence and Equity. Curr. Obes. Rep. 2014, 3, 1–15. [Google Scholar] [CrossRef]
- Hamano, T.; Li, X.; Sundquist, J.; Sundquist, K. Association between Childhood Obesity and Neighbourhood Accessibility to Fast-Food Outlets: A Nationwide 6-Year Follow-Up Study of 944,487 Children. Obes. Facts 2018, 10, 559–568. [Google Scholar] [CrossRef]
- Nau, C.; Schwartz, B.S.; Bandeen-Roche, K.; Liu, A.; Pollak, J.; Hirsch, A.; Bailey-Davis, L.; Glass, T.A. Community socioeconomic deprivation and obesity trajectories in children using electronic health records. Obesity (Silver Spring) 2015, 23, 207–212. [Google Scholar] [CrossRef]
- Wilsher, S.H.; Harrison, F.; Yamoah, F.; Fearne, A.; Jones, A. The relationship between unhealthy food sales, socio-economic deprivation and childhood weight status: Results of a cross-sectional study in England. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 21. [Google Scholar] [CrossRef]
- Conrad, D.; Capewell, S. Associations between deprivation and rates of childhood overweight and obesity in England, 2007–2010: An ecological study. BMJ Open 2012, 2, e000463. [Google Scholar] [CrossRef]
- Li, X.; Memarian, E.; Sundquist, J.; Zöller, B.; Sundquist, K. Neighbourhood Deprivation, Individual-Level Familial and Socio-Demographic Factors and Diagnosed Childhood Obesity: A Nationwide Multilevel Study from Sweden. OFA 2014, 7, 253–263. [Google Scholar] [CrossRef]
- Wright, C.M.; Parker, L.; Lamont, D.; Craft, A.W. Implications of childhood obesity for adult health: Findings from thousand families cohort study. BMJ 2001, 323, 1280–1284. [Google Scholar] [CrossRef] [PubMed]
- Norris, T.; Bann, D.; Hardy, R.; Johnson, W. Socioeconomic inequalities in childhood-to-adulthood BMI tracking in three British birth cohorts. Int. J. Obes. 2019, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Geserick, M.; Vogel, M.; Gausche, R.; Lipek, T.; Spielau, U.; Keller, E.; Pfäffle, R.; Kiess, W.; Körner, A. Acceleration of BMI in Early Childhood and Risk of Sustained Obesity. N. Engl. J. Med. 2018, 379, 1303–1312. [Google Scholar] [CrossRef] [PubMed]
- Kelly, Y.; Zilanawala, A.; Sacker, A.; Hiatt, R.; Viner, R. Early puberty in 11-year-old girls: Millennium Cohort Study findings. Arch. Dis. Child. 2017, 102, 232–237. [Google Scholar] [CrossRef]
- Public Health England. Childhood Obesity: Applying All Our Health; Public Health England: London, UK, 2019. [Google Scholar]
| Characteristics | Equivalised Family Income Quintiles | |||||
|---|---|---|---|---|---|---|
| Highest | Fourth | Third | Second | Lowest | p for Trend | |
| Sex | ||||||
| Boys | 51.6 | 54.0 | 51.9 | 51.1 | 53.4 | 0.467 |
| Girls | 48.4 | 46.0 | 48.1 | 48.9 | 46.6 | |
| Ethnicity 1 | ||||||
| White | 90.7 | 88.3 | 84.4 | 78.7 | 60.5 | <0.001 |
| Non-white | 9.3 | 11.7 | 15.6 | 21.3 | 39.5 | |
| Mother’s highest educational level 1 | ||||||
| <HE certificate | 23.4 | 50.3 | 61.9 | 75.7 | 89.6 | <0.001 |
| ≥HE certificate | 76.6 | 49.7 | 38.1 | 24.3 | 10.4 | |
| Moderate–vigorous PA 1 | ||||||
| <3 days per week | 21.7 | 27.1 | 32.4 | 30.6 | 34.3 | <0.001 |
| ≥3 days per week | 78.3 | 72.9 | 67.6 | 69.4 | 65.6 | |
| TV/video watching1 | ||||||
| ≥3 h per day | 36.1 | 43.8 | 45.5 | 47.5 | 48.6 | <0.001 |
| <3 h per day | 63.9 | 56.2 | 54.5 | 52.5 | 51.4 | |
| Obesity1 | ||||||
| Obese | 3.7 | 5.8 | 8.3 | 10.4 | 12.3 | <0.001 |
| Not obese | 96.3 | 94.2 | 91.7 | 89.7 | 87.7 | |
| Overweight 1 | ||||||
| Overweight/obese | 19.5 | 23.8 | 29.1 | 30.1 | 34.1 | <0.001 |
| Not overweight/obese | 80.5 | 76.2 | 70.9 | 69.9 | 65.9 | |
| Percentage body fat | 20.1 (0.2) | 21.0 (0.2) | 22.2 (0.2) | 22.7 (0.3) | 23.3 (0.4) | <0.001 |
| Characteristics | Geographic-Level Deprivation (IMD) Quintiles | |||||
|---|---|---|---|---|---|---|
| Least | Second | Third | Fourth | Most | p for Trend | |
| Sex | ||||||
| Boys | 53.1 | 51.4 | 53.1 | 53.1 | 52.1 | 0.921 |
| Girls | 46.9 | 48.6 | 46.9 | 46.9 | 47.9 | |
| Ethnicity 1 | ||||||
| White | 88.3 | 87.2 | 82.8 | 76.0 | 60.5 | <0.001 |
| Non-white | 11.7 | 12.8 | 17.2 | 24.0 | 39.5 | |
| Mother’s highest educational level 1 | ||||||
| <HE certificate | 40.1 | 45.5 | 60.6 | 65.0 | 72.4 | <0.001 |
| ≥HE certificate | 59.9 | 54.5 | 39.4 | 35.0 | 27.6 | |
| Moderate–vigorous PA 1 | ||||||
| <3 days per week | 22.2 | 28.2 | 31.3 | 35.7 | 32.0 | <0.001 |
| ≥3 days per week | 77.8 | 71.9 | 68.7 | 64.3 | 68.0 | |
| TV/video watching 1 | ||||||
| ≥3 h per day | 36.1 | 43.8 | 45.5 | 47.5 | 48.6 | <0.001 |
| <3 h per day | 60.2 | 58.4 | 54.3 | 50.1 | 53.5 | |
| Equivalised family income quintile | ||||||
| Highest | 45.2 | 31.3 | 18.0 | 9.6 | 1.8 | <0.001 |
| Fourth | 25.8 | 27.9 | 26.1 | 18.5 | 6.1 | |
| Third | 17.9 | 20.9 | 25.8 | 21.9 | 15.4 | |
| Second | 8.2 | 13.1 | 17.7 | 26.4 | 30.2 | |
| Lowest | 2.9 | 6.9 | 12.5 | 23.6 | 46.5 | |
| Obesity 1 | ||||||
| Obese | 4.4 | 6.0 | 7.6 | 9.8 | 10.7 | <0.001 |
| Not obese | 95.6 | 94.0 | 92.4 | 90.2 | 89.3 | |
| Overweight 1 | ||||||
| Overweight/obese | 21.1 | 22.9 | 26.6 | 30.3 | 32.5 | <0.001 |
| Not overweight/obese | 78.9 | 77.1 | 73.5 | 69.7 | 67.5 | |
| Percentage body fat | 20.1 (0.3) | 20.9 (0.3) | 21.6 (0.3) | 22.5 (0.3) | 23.1 (0.4) | <0.001 |
| Obesity | Overweight | Percentage Body Fat | ||||
|---|---|---|---|---|---|---|
| Income Quintiles | RR (95% CI) 1 | RR (95% CI) 3 | RR (95% CI) 1 | RR (95% CI) 3 | MD (95% CI) 2 | MD (95% CI) 4 |
| A. Analysis in entire UK cohort | ||||||
| Highest 5 | 1.0 | 1.0 | 1.0 | 1.0 | 0.0 | 0.0 |
| Fourth | 1.4 (1.0–1.8) * | 1.3 (1.0–1.8) * | 1.2 (1.1–1.4) # | 1.2 (1.0–1.3) * | 0.9 (0.4–1.4) ≠ | 0.7 (0.2–1.2) # |
| Third | 1.8 (1.3–2.4) ≠ | 1.7 (1.2–2.3) # | 1.4 (1.2–1.6) ≠ | 1.3 (1.1–1.5) ≠ | 1.5 (0.9–2.0) ≠ | 1.2 (0.7–1.8) ≠ |
| Second | 2.1 (1.5–2.8) ≠ | 1.9 (1.4–2.7) ≠ | 1.5 (1.3–1.7) ≠ | 1.4 (1.2–1.6) ≠ | 2.1 (1.4–2.7) ≠ | 1.8 (1.2–2.4) ≠ |
| Lowest | 2.7 (1.9–3.7) ≠ | 2.4 (1.7–3.4) ≠ | 1.6 (1.4–1.9) ≠ | 1.5 (1.3–1.8) ≠ | 3.0 (2.2–3.9) ≠ | 2.7 (1.8–3.6) ≠ |
| B. Analysis in England sub-cohort | ||||||
| Highest 5 | 1.0 | 1.0 | 1.0 | 1.0 | 0.0 | 0.0 |
| Fourth | 1.2 (0.9–1.7) | 1.1 (0.8–1.6) | 1.2 (1.0–1.4) * | 1.1 (1.0–1.3) | 0.8 (0.3–1.4) # | 0.6 (0.1–1.2) * |
| Third | 1.8 (1.3–2.6) ≠ | 1.7 (1.2–2.4) # | 1.4 (1.2–1.7) ≠ | 1.4 (1.2–1.6) ≠ | 1.6 (1.0–2.2) ≠ | 1.4 (0.8–2.0) ≠ |
| Second | 2.1 (1.4–3.0) ≠ | 1.9 (1.3–2.8) # | 1.5 (1.3–1.8) ≠ | 1.4 (1.2–1.7) ≠ | 2.2 (1.5–2.9) ≠ | 1.9 (1.2–2.6) ≠ |
| Lowest | 2.5 (1.7–3.8) ≠ | 2.2 (1.5–3.3) ≠ | 1.6 (1.4–1.9) ≠ | 1.5 (1.3–1.8) ≠ | 3.1 (2.1–4.1) ≠ | 2.7 (1.7–3.7) ≠ |
| Family Income Quintiles | Geographic-Level Deprivation Quintiles | ||||
|---|---|---|---|---|---|
| Least | Second | Third | Fourth | Most | |
| (a) Partially adjusted model | |||||
| Highest 1 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Fourth | 1.4 (0.7–2.8) | 0.7 (0.3–1.5) | 0.9 (0.4–2.2) | 1.6 (0.7–3.9) | 3.1 (0.6–17.3) |
| Third | 2.2 (1.1–4.3) | 0.7 (0.3–1.6) | 2.2 (1.0–4.8) * | 2.2 (0.9–5.2) | 2.4 (0.4–13.0) |
| Second | 4.3 (1.8–10.4) # | 1.4 (0.6–3.1) | 1.1 (0.4–3.5) | 1.7 (0.8–3.9) | 4.1 (0.8–21.1) |
| Lowest | 5.5 (1.8–17.2) * | 0.2 (0.0–1.6) | 2.7 (1.0–7.2) | 2.4 (1.0–5.8) * | 4.4 (0.9–22.3) |
| p for trend | <0.001 | 0.990 | 0.052 | 0.133 | 0.040 |
| (b) Fully adjusted model | |||||
| Highest 1 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Fourth | 1.3 (0.6–2.6) | 0.7 (0.3–1.5) | 0.8 (0.4–1.9) | 1.5 (0.6–3.7) | 3.1 (0.6–17.3) |
| Third | 1.9 (1.0–3.8) | 0.7 (0.3–1.6) | 1.9 (0.9–4.2) | 2.1 (0.9–4.7) | 2.4 (0.4–13.1) |
| Second | 3.9 (1.6–9.4) # | 1.5 (0.7–3.2) | 1.0 (0.3–2.9) | 1.6 (0.7–3.7) | 4.1 (0.8–21.3) |
| Lowest | 4.8 (1.4–16.8) * | 0.2 (0.0–1.4) | 2.1 (0.8–5.4) | 2.0 (0.8–5.0) | 4.4 (0.9–22.4) |
| p for trend | <0.001 | 0.956 | 0.096 | 0.336 | 0.039 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mireku, M.O.; Rodriguez, A. Family Income Gradients in Adolescent Obesity, Overweight and Adiposity Persist in Extremely Deprived and Extremely Affluent Neighbourhoods but Not in Middle-Class Neighbourhoods: Evidence from the UK Millennium Cohort Study. Int. J. Environ. Res. Public Health 2020, 17, 418. https://doi.org/10.3390/ijerph17020418
Mireku MO, Rodriguez A. Family Income Gradients in Adolescent Obesity, Overweight and Adiposity Persist in Extremely Deprived and Extremely Affluent Neighbourhoods but Not in Middle-Class Neighbourhoods: Evidence from the UK Millennium Cohort Study. International Journal of Environmental Research and Public Health. 2020; 17(2):418. https://doi.org/10.3390/ijerph17020418
Chicago/Turabian StyleMireku, Michael Osei, and Alina Rodriguez. 2020. "Family Income Gradients in Adolescent Obesity, Overweight and Adiposity Persist in Extremely Deprived and Extremely Affluent Neighbourhoods but Not in Middle-Class Neighbourhoods: Evidence from the UK Millennium Cohort Study" International Journal of Environmental Research and Public Health 17, no. 2: 418. https://doi.org/10.3390/ijerph17020418
APA StyleMireku, M. O., & Rodriguez, A. (2020). Family Income Gradients in Adolescent Obesity, Overweight and Adiposity Persist in Extremely Deprived and Extremely Affluent Neighbourhoods but Not in Middle-Class Neighbourhoods: Evidence from the UK Millennium Cohort Study. International Journal of Environmental Research and Public Health, 17(2), 418. https://doi.org/10.3390/ijerph17020418






