How the Lagged and Accumulated Effects of Stress, Coping, and Tasks Affect Mood and Fatigue during Nurses’ Shifts
Abstract
1. Introduction
1.1. Aim/Research Questions
- Accumulated effort will worsen mood and will increase fatigue, while reward will produce the opposite effect, as predicted by Siegrist’s model.
- 2.
- The use of problem-focused and seeking-support strategies will have a delayed and accumulated effect on mood and fatigue, producing an improvement in both; and
- 3.
- The use of emotion-focused and refusal strategies will have a delayed and accumulated effect on mood and fatigue, worsening them.
- 4.
- Accumulated direct care tasks improve mood and increase fatigue;
- 5.
- Administrative and organizational tasks will have a delayed and negative effect on mood, presumably due to tedium.
2. Materials and Methods
2.1. Design
2.2. Participants, Settings, and Procedure
2.3. Measures
2.3.1. Level 1 Measures (moment)
Ecological Momentary Assessment
2.3.2. Level 2 Measures (Person)
Questionnaires
2.4. Data Analyses
2.4.1. Multilevel Modelling (MLM)
2.4.2. Assumptions
2.4.3. Initial Models, Model Fit, and Fit Criteria
2.4.4. Mood and Fatigue from Lagged and Current Values of the Predictors
2.4.5. Mood and Fatigue from Accumulated Values of the Predictors
2.5. Ethics
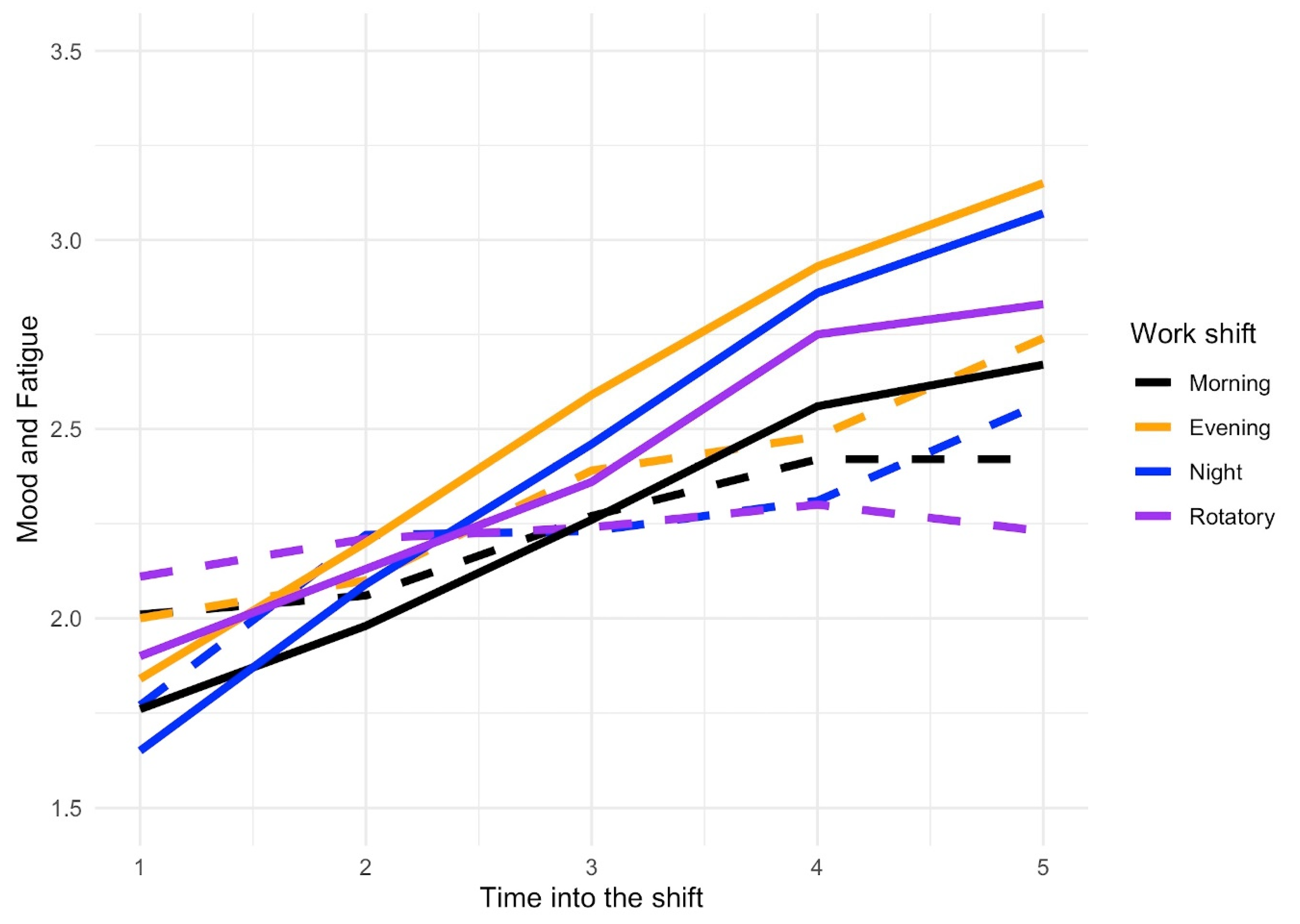
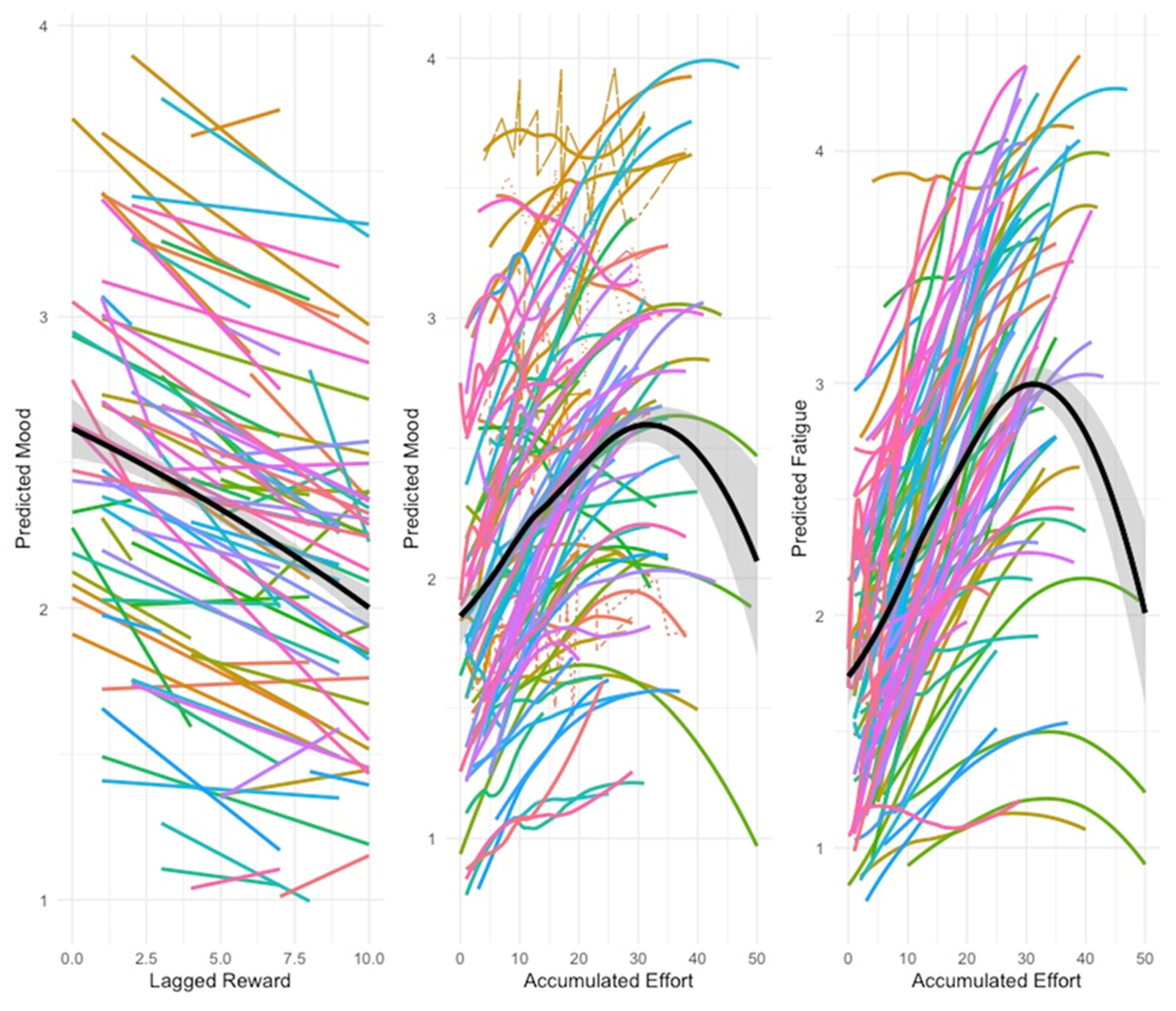
3. Results
3.1. Sample Description
3.2. Data Analyses
4. Discussion
4.1. The Effect of Stress on Mood and Fatigue
4.2. Effect of Coping on Mood and Fatigue
4.3. Effect of Nursing Task on their Mood and Fatigue
4.4. Limitations and Perspective for Future Studies
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Hasan, A.A. Work stress, coping strategies and levels of depression among nurses working in mental health hospital in Port-Said city. Int. Arch. Nurs. Health Care 2017, 3, 1–10. [Google Scholar] [CrossRef][Green Version]
- Martín-Del-Río, B.; Solanes-Puchol, Á.; Martínez-Zaragoza, F.; Benavides-Gil, G. Stress in nurses: The 100 top-cited papers published in nursing journals. J. Adv. Nurs. 2018, 74, 1488–1504. [Google Scholar] [CrossRef] [PubMed]
- Moustaka, Ε.; Constantinidis, T.C. Sources and effects of Work-related stress in nursing. Health Sci. J. 2010, 4, 210–216. [Google Scholar]
- Yau, S.Y.; Xiao, X.Y.; Lee, L.Y.; Tsang, A.Y.; Wong, S.L.; Wong, K.F. Job stress among nurses in China. Appl. Nurs. Res. 2012, 25, 60–64. [Google Scholar] [CrossRef]
- Dall’Ora, C.; Griffiths, P.; Hope, J.; Barker, H.; Smith, G.B. What is the nursing time and workload involved in taking and recording patients’ vital signs? A systematic review. J. Clin. Nurs. 2020, 29, 2053–2068. [Google Scholar] [CrossRef]
- Karasek, R. Demand/control model: A social, emotional and physiological approach to stress risk and active behavior development. In Encyclopedia of Occupational Health and Safety, International Labour Office; Stellman, J.M., Ed.; OIT: Geneva, Switzerland, 1998; pp. 34.6–34.14. [Google Scholar]
- Siegrist, J. Adverse health effects of high-effort/low-reward conditions. J. Occup. Health Psychol. 1996, 1, 27–41. [Google Scholar] [CrossRef]
- Baba, V.V.; Tourigny, L.; Wang, X.; Lituchy, T.; Monserrat, S.I. Stress among nurses: A multi-nation test of the demand-control-support model. Cross Cult. Manag. An Int. J. 2013, 20, 301–320. [Google Scholar] [CrossRef]
- Magnago, T.S.B.S.; Lisboa, M.T.L.; Griep, R.H.; Zeitoune, R.C.G.; Tavares, J.P. Working conditions of nurses: Evaluation based on the demand-control model. Acta Paul. Enfermagen 2010, 23, 811–817. [Google Scholar] [CrossRef]
- Negussie, N.; Kaur, G. The effect of job demand-control-social support model on nurses’ job satisfaction in specialized teaching hospitals, Ethiopia. Ethiop. J. Health Sci. 2016, 26, 311–320. [Google Scholar] [CrossRef]
- Caruso, C.C. Negative impacts of shiftwork and long work hours. Rehabil. Nurs. 2014, 39, 16–25. [Google Scholar] [CrossRef]
- Hasselhorn, H.M.; Tackenberg, P.; Peter, R. Effort-reward imbalance among nurses in stable countries and in countries in transition. Int. J. Occup. Environ. Health 2004, 10, 401–408. [Google Scholar] [CrossRef] [PubMed]
- Padilla, C.; Palmeiro-Silva, Y.K. Effort-reward imbalance and burnout among ICU nursing staff: A cross-sectional study. Nurs. Res. 2017, 66, 410–416. [Google Scholar] [CrossRef] [PubMed]
- Schreuder, J.A.H.; Roelen, C.A.M.; Koopmans, P.C.; Moen, B.E.; Groothoff, J.W. Effort-reward imbalance is associated with the frequency of sickness absence among female hospital nurses: A cross-sectional study. Int. J. Nurs. Stud. 2010, 47, 569–576. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Johnston, D.W.; Jones, M.C.; Charles, K.; McCann, S.K.; McKee, L. Stress in nurses: Stress-related affect and its determinants examined over the nursing day. Ann. Behav. Med. 2013, 45, 348–356. [Google Scholar] [CrossRef][Green Version]
- Hockey, R. The Psychology of Fatigue; Cambridge University Press: Cambridge, UK, 2013; ISBN 9781139015394. [Google Scholar]
- The Joint Commission. Health care worker fatigue and patient safety. Sentin. Event Alert 2011, 48, 1–4. [Google Scholar]
- Wylie, G.R.; Genova, H.M.; Deluca, J.; Dobryakova, E. The relationship between outcome prediction and cognitive fatigue: A convergence of paradigms. Cogn. Affect. Behav. Neurosci. 2017, 17, 838–849. [Google Scholar] [CrossRef]
- Rahman, H.A.; Abdul-Mumin, K.; Naing, L. A study into psychosocial factors as predictors of work-related fatigue. Br. J. Nurs. 2016, 25, 757–763. [Google Scholar] [CrossRef]
- Fernández-Castro, J.; Martínez-Zaragoza, F.; Rovira, T.; Edo, S.; Solanes-Puchol, Á.; Martín-del-Río, B.; García-Sierra, R.; Benavides-Gil, G.; Doval, E. How does emotional exhaustion influence work stress? Relationships between stressor appraisals, hedonic tone, and fatigue in nurses’ daily tasks: A longitudinal cohort study. Int. J. Nurs. Stud. 2017, 75, 43–50. [Google Scholar] [CrossRef]
- Allan, J.L.; Johnston, D.W.; Powell, D.J.H.; Farquharson, B.; Jones, M.C.; Leckie, G.; Johnston, M. Clinical decisions and time since rest break: An analysis of decision fatigue in nurses. Health Psychol. 2019, 38, 318–324. [Google Scholar] [CrossRef]
- Thompson, B.J. Does work-induced fatigue accumulate across three compressed 12 hour shifts in hospital nurses and aides? PLoS ONE 2019, 14, 1–15. [Google Scholar] [CrossRef]
- Smith-Miller, C.A.; Shaw-Kokot, J.; Curro, B.; Jones, C.B. An integrative review: Fatigue among nurses in acute care settings. J. Nurs. Adm. 2014, 44, 487–494. [Google Scholar] [CrossRef] [PubMed]
- Thompson, B.J.; Stock, M.S.; Banuelas, V.K. Effects of accumulating work shifts on performance-based fatigue using multiple strength measurements in day and night shift nurses and aides. Hum. Factors J. Hum. Factors Ergon. Soc. 2016, 59, 346–356. [Google Scholar] [CrossRef] [PubMed]
- Rogers, A.E. The Effects of Fatigue and Sleepiness on Nurse Performance and Patient Safety. In Patient Safety and Quality: An Evidence-Based Handbook for Nurses; Hughes, R.G., Ed.; Agency for Healthcare Research and Quality (US): Rockville, MD, USA, 2008; Volume 2, pp. 509–545. [Google Scholar]
- Bueno, J.L.; Figueiredo, M.N.; Figueiredo, T.H. Present mood states in Brazilian night nurses. Psychol. Rep. 2003, 93, 353–357. [Google Scholar] [CrossRef] [PubMed]
- De Martino, M.M.F.; Misko, M.D. Estados emocionais de enfermeiros no desempenho profissional em unidades críticas. Rev. Esc. Enferm. USP 2004, 38, 161–167. [Google Scholar] [CrossRef]
- Johnston, D.W.; Allan, J.L.; Powell, D.J.H.; Jones, M.C.; Farquharson, B.; Bell, C.; Johnston, M. Why does work cause fatigue? A real-time investigation of fatigue, and determinants of fatigue in nurses working 12-hour shifts. Ann. Behav. Med. 2019, 53, 551–562. [Google Scholar] [CrossRef]
- Steege, L.M.; Drake, D.A.; Olivas, M.; Mazza, G. Evaluation of physically and mentally fatiguing tasks and sources of fatigue as reported by registered nurses. J. Nurs. Manag. 2015, 23, 179–189. [Google Scholar] [CrossRef]
- Steege, L.M.; Dykstra, J.G. A macroergonomic perspective on fatigue and coping in the hospital nurse work system. Appl. Ergon. 2016, 54, 19–26. [Google Scholar] [CrossRef]
- Chang, E.M.; Bidewell, J.W.; Huntington, A.D.; Daly, J.; Johnson, A. A survey of role stress, coping and health in Australian and New Zealand hospital nurses. Int. J. Nurs. Stud. 2007, 44, 1354–1362. [Google Scholar] [CrossRef]
- Hätinen, M.; Mäkikangas, A.; Kinnunen, U.; Pekkonen, M. Recovery from burnout during a one-year rehabilitation intervention with six-month follow-up: Associations with coping strategies. Int. J. Stress Manag. 2013, 20, 364. [Google Scholar] [CrossRef]
- Lazarus, R.S.; Folkman, S. Stress, Appraisal, and Coping; Springer: New York, NY, USA, 1984. [Google Scholar]
- Rothbaum, F.; Weisz, J.R.; Snyder, S.S. Changing the world and changing the self: A two-process model of perceived control. J. Pers. Soc. Psychol. 1982, 42, 5–37. [Google Scholar] [CrossRef]
- Yoshizawa, K.; Sugawara, N.; Yasui-Furukori, N.; Danjo, K.; Furukori, H.; Sato, Y.; Tomita, T.; Fujii, A.; Nakagam, T.; Sasaki, M.; et al. Relationship between occupational stress and depression among psychiatric nurses in Japan. Arch. Environ. Occup. Health 2016, 71, 10–15. [Google Scholar] [CrossRef] [PubMed]
- Nayomi, W. Workplace stress in nursing: A literature review. J. Soc. Stat. 2016, 3, 47–53. [Google Scholar]
- Samaha, E.; Lal, S.; Samaha, N.; Wyndham, J. Psychological, lifestyle and coping contributors to chronic fatigue in shift-worker nurses. J. Adv. Nurs. 2007, 59, 221–232. [Google Scholar] [CrossRef] [PubMed]
- Healy, C.M.; McKay, M.F. Nursing stress: The effects of coping strategies and job satisfaction in a sample of Australian nurses. J. Adv. Nurs. 2000, 31, 681–688. [Google Scholar] [CrossRef] [PubMed]
- Segerstrom, S.C.; O’Connor, D.B. Stress, health and illness: Four challenges for the future. Psychol. Health 2012, 27, 128–140. [Google Scholar] [CrossRef] [PubMed]
- Al Barmawi, M.A.; Subih, M.; Salameh, O.; Sayyah Yousef Sayyah, N.; Shoqirat, N.; Abdel-Azeez Eid Abu Jebbeh, R. Coping strategies as moderating factors to compassion fatigue among critical care nurses. Brain Behav. 2019, 9, 1–8. [Google Scholar] [CrossRef]
- Ato, M.; López, J.J.; Benavente, A. Un sistema de clasificación de los diseños de investigación en Psicología [A classification system of research designs in Psychology]. An. Psicol. 2013, 29, 1038–1059. [Google Scholar] [CrossRef]
- Stone, A.A.; Shiffman, S. Ecological momentary assessment (EMA) in behavioural medicine. Ann. Behav. Med. 1994, 16, 199–202. [Google Scholar] [CrossRef]
- Bolger, N.; Davis, A.; Rafaeli, E. Capturing life as it is lived. Annu. Rev. Psychol. 2003, 54, 579–616. [Google Scholar] [CrossRef]
- Patrician, P.A. Single-Item Graphic Representational Scales. Nurs. Res. 2004, 53, 347–352. [Google Scholar] [CrossRef]
- Rovira, T.; Ferrer, I.; Edo, S.; Fernández-Castro, J.; Benavides, G.; Doval, E.; Martínez, F. Validity and feasibility of a nurses’ coping questionnaire for its use in Ecological Momentary Assessment. Eur. Health Psychol. 2016, 18, 758. [Google Scholar]
- Carver, C.; Scheier, M.; Weintraub, J. Assessing coping strategies: A theoretically based approach. J. Pers. Soc. Psychol. 1989, 56, 257–283. [Google Scholar] [CrossRef]
- Crespo, M.; Cruzado, J.A. La evaluación del afrontamiento: Adaptación española del cuestionario COPE con muestra de estudiantes universitarios. Análisis y Modif. Conduct. 1997, 23, 797–830. [Google Scholar]
- Ampt, A.; Westbrook, J.I.; Creswick, N.; Mallock, N. A comparison of self-reported and observational work sampling techniques for measuring time in nursing tasks. J. Health Serv. Res. Policy 2007, 12, 18–24. [Google Scholar] [CrossRef]
- Westbrook, J.I.; Ampt, A.; Kearney, L.; Rob, M.I. All in a day’s work: An observational study to quantify how and with whom doctors on hospital wards spend their time. Med. J. Aust. 2008, 118, 506–509. [Google Scholar] [CrossRef]
- Westbrook, J.I.; Ampt, A. Design, application and testing of the Work Observation Method by Activity Timing (WOMBAT) to measure clinicians’ patterns of work and communication. Int. J. Med. Inform. 2009, 78, S25–S33. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Viena, Austria, 2020; Available online: https://www.R-project.org/ (accessed on 1 September 2020).
- Fox, J.; Weisberg, S. An {R} Companion to Applied Regression, 2nd ed.; Sage: Thousand Oaks, CA, USA, 2011. [Google Scholar]
- Bliese, P.D.; Ployhart, R.E. Growth modeling using random coefficient models: Model building, testing and illustrations. Organ. Res. Methods 2002, 5, 362–387. [Google Scholar] [CrossRef]
- Bliese, P. Multilevel Modeling in R (2.6). An Introd. to R Notes R A Program. Environ. Data Anal. Graph. Smith, D.M.. 2016. Available online: http://www.statpower.net/Content/MLRM/Readings/Bliese_Multilevel.pdf (accessed on 1 September 2020).
- Akaike, H. A new look at the statistical model identification. IEEE Trans. Autom. Control 1974, AC-19, 716–723. [Google Scholar] [CrossRef]
- Bates, D.; Mächler, M.; Bolker, B.; Walker, S. Fitting linear mixed-effects models using lme4. J. Stat. Softw. 2015, 67, 1–48. [Google Scholar] [CrossRef]
- Kuznetsova, A.; Per Bruun Brockhoff, P.B.; Christensen, R.H.B. lmerTest: Tests in Linear Mixed Effects Models; R package version 2.0-32; 2016. Available online: https://cran.r-project.org/package=lmerTest (accessed on 1 September 2020).
- Lüdecke, D. Sjstats: Statistical Functions for Regression Models; R Package Version 0.14.1.; 2018. Available online: https://cran.r-project.org/package=sjstats (accessed on 1 September 2020).
- Wickham, H. Ggplot2: Elegant Graphics for Data Analysis, 2nd ed.; Springer: New York, NY, USA, 2016. [Google Scholar]
- Waugh, C.E.; Zarolia, P.; Mauss, I.B.; Lumian, D.S.; Ford, B.Q.; Davis, T.S.; Ciesielski, B.G.; Sams, K.V.; McRae, K. Emotion regulation changes the duration of the BOLD response to emotional stimuli. Soc. Cogn. Affect. Neurosci. 2016, 11, 1550–1559. [Google Scholar] [CrossRef][Green Version]
- Jiménez-Torres, M.G.; Pilar Martínez, M.; Miró, E.; Sánchez, A.I. Relación entre estrés percibido y estado de ánimo negativo: Diferencias según el estilo de afrontamiento. An. Psicol. 2012, 28, 28–36. [Google Scholar]
- Shin, H.; Park, Y.M.; Ying, J.Y.; Kim, B.; Noh, H.; Lee, S.M. Relationships between coping strategies and burnout symptoms: A meta-analytic approach. Prof. Psychol. Res. Pract. 2014, 45, 44–56. [Google Scholar] [CrossRef]
- Mardanian-Dehkordi, L.; Kahangi, L. The relationship between perception of social support and fatigue in patients with cancer. Iran. J. Nurs. Midwifery Res. 2018, 23, 261. [Google Scholar] [CrossRef] [PubMed]
- Aghaei, N.; Karbandi, S.; Gorji, M.H.; Golkhatmi, M.; Alizadeh, B. Social support in relation to fatigue symptoms among patients with multiple sclerosis. Indian J. Palliat. Care 2016, 22, 163. [Google Scholar] [CrossRef]
- Knupp, A.M.; Patterson, E.S.; Ford, J.L.; Zurmehly, J.; Patrick, T. Associations among nurse fatigue, individual nurse factors, and aspects of the nursing practice environment. J. Nurs. Adm. 2018, 48, 642–648. [Google Scholar] [CrossRef]
- American Organization for Nursing Leadership Elements of a Healthy Practice Environment. Available online: https://www.aonl.org/elements-healthy-practice-environment (accessed on 30 September 2020).
- May, C.; Finch, T. Implementing, embedding, and integrating practices: An outline of normalization process theory. Sociology 2009, 43, 535–554. [Google Scholar] [CrossRef]
- Holahan, C.J.; Moos, R.H.; Holahan, C.K.; Brennan, P.L.; Schutte, K.K. Stress Generation, Avoidance Coping, and Depressive Symptoms: A 10-Year Model. J. Consult. Clin. Psychol. 2005, 73, 658–666. [Google Scholar] [CrossRef]
- Gabriel, A.S.; Diefendorff, J.M.; Erickson, R.J. The relations of daily task accomplishment satisfaction with changes in affect: A multilevel study in nurses. J. Appl. Psychol. 2011, 96, 1095–1104. [Google Scholar] [CrossRef]
- Jones, T.; Willis, E.; Amorim-Lopes, M.; Drach-Zahavy, A. Advancing the science of unfinished nursing care: Exploring the benefits of cross-disciplinary knowledge exchange, knowledge integration and transdisciplinarity. J. Adv. Nurs. 2019, 75, 905–917. [Google Scholar] [CrossRef]
- Smallwood, J.; Davies, J.B.; Heim, D.; Finnigan, F.; Sudberry, M.; O’Connor, R.; Obonsawin, M. Subjective experience and the attentional lapse: Task engagement and disengagement during sustained attention. Conscious. Cogn. 2004, 13, 657–690. [Google Scholar] [CrossRef]

| Stress | ||||
|---|---|---|---|---|
| Mood | Fatigue | |||
| Parameter | Lagged | Accumulated | Lagged | Accumulated |
| Fixed effects | ||||
| Intercept | 1.53(9.67 × 10−2) *** | 2.44(0.10) *** | 1.35(1.11) *** | 1.95(9.74 × 10−2) *** |
| Level 1 (Moment) | ||||
| Time Demand Control Effort Reward | Time: 8.63 × 10−2(2.12 × 10−2) *** Effort: 9.40 × 10−2(8.57 × 10−3) *** Reward lag1 (quadratic): 2.68(1.00) ** | Time: −0.07(0.02) * Effort (quadratic): −3.92(0.95) *** | Time: 2.82 × 10−1(2.48 × 10−2) *** Effort lag1: 2.15 × 10−2(8.28 × 10−3) ** Effort: 4.95e−02(8.19 × 10−3) *** Reward lag1: −2.71 × 10−2(8.95 × 10−3) ** | Time: 2.41 × 10−1(3.61 × 10−2) *** Effort (quadratic): −2.35(8.54 × 10−1) ** Reward: −1.79 × 10−2(3.78 × 10−3) *** |
| Random effects | ||||
| Level 1 (Moment) | ||||
| Intercept SD | 0.59 | 0.73 | 0.61 | 0.72 |
| Time SD | 0.11 | 0.15 | 0.18 | 0.20 |
| ICC | 0.43 | 0.43 | 0.51 | 0.50 |
| AIC | − | 4641 | 3329 | 4169 |
| BIC | − | 4686 | 3376 | 4219 |
| Coping | ||||
| Fixed effects | ||||
| Intercept | 1.80(9.29 × 10−2) *** | 1.95(8.51 × 10−2) *** | 1.46(9.00 × 10−2) *** | 1.54(0.08) *** |
| Level 1 (Moment) | ||||
| Time Problem-focused Emotion-focused Seeking support Refusal | Time: 9.32 × 10−2(2.16 × 10−2) *** Problem: 3.46 × 10−1(5.75 × 10−2) *** Emotion: 2.24 × 10−1(5.47 × 10−2) *** | Time: 6.89 × 10−2(2.39 × 10−2) ** Emotion: 7.57 × 10−2(2.60 × 10−2) ** Refusal: 2.86 × 10−1(7.04 × 10−2) *** | Time: 2.80 × 10−1(2.50 × 10−2) *** Problem lag1: 9.90 × 10−2(5.05 × 10−2) * Emotion: 1.72 × 10−1(4.97 × 10−2 ) *** Refusal: 5.32 × 10−1(1.287 × 10−1) *** | Time: 0.24(0.02) *** Problem: 0.04(0.02) * Emotion: 0.08(0.02) *** Support: −0.11(0.03) ** Refusal: 0.27(0.06) *** |
| Random effects | ||||
| Level 1 (Moment) | ||||
| Intercept SD | 0.59 | 0.73 | 0.63 | 0.72 |
| Time SD | 0.11 | 0.17 | 0.18 | 0.21 |
| ICC | 0.41 | 0.42 | 0.52 | 0.52 |
| AIC | 3572 | 4693 | 3352 | 4208 |
| BIC | 3615 | 4738 | 3400 | 4263 |
| Task | ||||
| Fixed effects | ||||
| Intercept | 1.96(9.17 × 10−2) *** | 1.94(0.08) *** | 1.48(0.08) *** | 1.51(8.15e−02) *** |
| Level 1 (Moment) | ||||
| Time Direct Care Indirect Care Medication Documentation Communication Social/resting | Time: 8.54 × 10−2(2.16 × 10−2) *** Direct Care lag1: 1.30 × 10−1(4.53 × 10−2) ** | Time: 0.11(0.02) *** Documentation:−0.09(0.03) ** | Time: 0.29(0.02) *** Direct Care: 0.20(0.04) *** Documentation lag1: −0.12(0.05) * Communication lag1: −0.22(0.08) ** | Time: 2.15e−01(2.54 × 10−2) *** Direct Care: 1.76 × 10−1(2.34 × 10−2) *** Medication: 1.25 × 10−1(2.92 × 10−2) *** |
| Random effects | ||||
| Level 1 (Moment) | ||||
| Intercept SD | 0.62 | 0.73 | 0.64 | 0.71 |
| Time SD | 0.11 | 0.16 | 0.18 | 0.20 |
| ICC | 0.42 | 0.42 | 0.52 | 0.52 |
| AIC | 3607 | − | 3349 | 4182 |
| BIC | 3644 | − | 3397 | 4227 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martínez-Zaragoza, F.; Fernández-Castro, J.; Benavides-Gil, G.; García-Sierra, R. How the Lagged and Accumulated Effects of Stress, Coping, and Tasks Affect Mood and Fatigue during Nurses’ Shifts. Int. J. Environ. Res. Public Health 2020, 17, 7277. https://doi.org/10.3390/ijerph17197277
Martínez-Zaragoza F, Fernández-Castro J, Benavides-Gil G, García-Sierra R. How the Lagged and Accumulated Effects of Stress, Coping, and Tasks Affect Mood and Fatigue during Nurses’ Shifts. International Journal of Environmental Research and Public Health. 2020; 17(19):7277. https://doi.org/10.3390/ijerph17197277
Chicago/Turabian StyleMartínez-Zaragoza, Fermín, Jordi Fernández-Castro, Gemma Benavides-Gil, and Rosa García-Sierra. 2020. "How the Lagged and Accumulated Effects of Stress, Coping, and Tasks Affect Mood and Fatigue during Nurses’ Shifts" International Journal of Environmental Research and Public Health 17, no. 19: 7277. https://doi.org/10.3390/ijerph17197277
APA StyleMartínez-Zaragoza, F., Fernández-Castro, J., Benavides-Gil, G., & García-Sierra, R. (2020). How the Lagged and Accumulated Effects of Stress, Coping, and Tasks Affect Mood and Fatigue during Nurses’ Shifts. International Journal of Environmental Research and Public Health, 17(19), 7277. https://doi.org/10.3390/ijerph17197277





