Prognostic Factors for Staying at Work for Partially Sick-Listed Workers with Subjective Health Complaints: A Prospective Cohort Study.
Abstract
1. Introduction
2. Materials and Methods
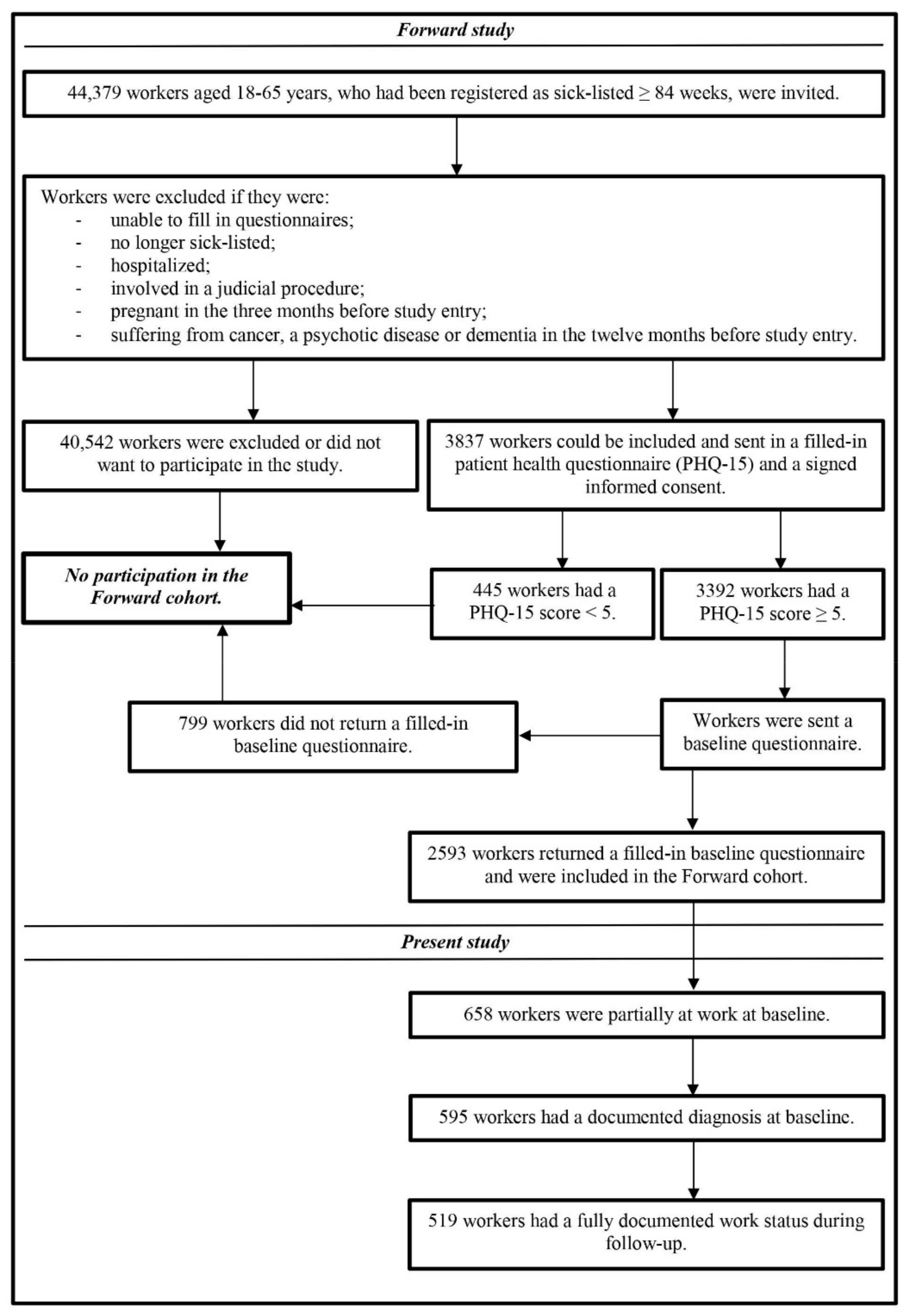
2.1. Study Design and Study Population
2.2. Informed Consent
2.3. Measures
2.3.1. Dependent Variable
2.3.2. Independent Variables
- 1.
- The work and well-being inventory (WBI) questionnaire with 85 questions and five subscales [20]:
- The stressors subscale with a scoring range of 16–64 (higher scores indicate more stressors).
- The support subscale with a scoring range of 21–84 (higher scores indicate better support).
- The symptom subscale with a scoring range of 20–80 (higher scores indicate more symptoms).
- The coping strategies subscale with a scoring range of 17–68 (higher scores indicate better coping).
- The self-perceived disability subscale with a scoring range of 7–28 (higher scores indicate more self-perceived disability).
- 2.
- The hospital anxiety and depression scale (HADS) with 14 questions and two subscales [21]:
- The depressive disorder subscale with a scoring range of 0–21 (higher scores indicate a higher risk for a depressive disorder).
- The anxiety disorder subscale with a scoring range of 0–21 (higher scores indicate a higher risk for an anxiety disorder).
- 3.
- The patient health questionnaire (PHQ-15) with 15 questions and one scale [22]:
- The severity of complaints scale with a scoring range of 5–30 (higher scores indicate more severe complaints).
- 4.
- The physical health subscale (PCS) with a scoring range of 0–100 (higher scores indicate better levels of physical health and functioning).
- The mental health subscale (MCS) with a scoring range of 0–100 (higher scores indicate better levels of mental health and functioning).
- The health change subscale (SF-2), which was derived from the following question on the SF-36: “How is your health in general compared to a year ago?” We categorized the five answering options into two categories: ‘same or better’ and ‘worse’.
- 5.
- The Whitely index questionnaire (WI) with 14 questions and one scale [25]:
- The hypochondria scale with a scoring range of 0–14 (higher scores indicate a higher risk for hypochondria).
- 6.
- The work ability index (WAI) with three questions and two subscales [26]:
- The work ability in general subscale with a scoring range of 0–10 (higher scores indicate higher self-perceived work ability).
- The work ability in the context of work load subscale with a scoring range of 2–10 (higher scores indicate higher self-perceived work ability in the context of work load).
- 7.
- The obstacles to return to work questionnaire (ORQ) with six questions and one scale [27]:
- The perceived prognosis of work return scale with a scoring range of 0–36 (higher scores indicate higher self-perceived possibilities for returning to work).
2.4. Statistics
3. Results
3.1. Staying at Work Predictors for Participants with SHC
3.2. Staying at Work Predictors for Participants with Other Disorders (Reference group) than SHC
4. Discussion
4.1. Strengths and Limitations
4.2. Implications for Policy, Practice and Future Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Oganisation (WHO). Global Health Estimates 2016: Disease Burden by Cause, Age, Sex, by Country and by Region 2000–2016. Geneva: WHO. 2018. Available online: https://www.who.int/healthinfo/global_burden_disease/estimates/en/index1.html (accessed on 1 January 2000).
- Marks, E.M.; Hunter, M.S. Medically unexplained symptoms: An acceptable term? Br. J. Pain 2015, 9, 109–114. [Google Scholar] [CrossRef] [PubMed]
- Breivik, H.; Collett, B.; Ventafridda, V.; Cohen, R.; Gallacher, D. Survey of chronic pain in Europe: Prevalence, impact on daily life, and treatment. Eur. J. Pain 2006, 10, 287–333. [Google Scholar] [CrossRef] [PubMed]
- Lerner, D.; Allaire, S.H.; Reisine, S.T. Work disability resulting from chronic health conditions. J. Occup. Environ. Med. 2005, 47, 253–264. [Google Scholar] [CrossRef] [PubMed]
- Cochrane, A.; Higgins, N.M.; Rothwell, C.; Ashton, J.; Breen, R.; Corcoran, O. Work outcomes in patients who stay at work despite musculoskeletal pain. J. Occup. Rehabil. 2018, 28, 559–567. [Google Scholar] [CrossRef]
- Loengaard, K.; Bjorner, J.B.; Fink, P.K.; Burr, H.; Rugulies, R. Medically unexplained symptoms and the risk of loss of labor market participation: A prospective study in the Danish population. BMC Public Health 2015, 15, 844. [Google Scholar] [CrossRef]
- De Vries, H.J.; Reneman, M.F.; Groothoff, J.W.; Geertzen, J.H.; Brouwer, S. Factors promoting staying at work in people with chronic nonspecific musculoskeletal pain: A systematic review. Disabil. Rehabil. 2012, 34, 443–458. [Google Scholar] [CrossRef]
- Cancelliere, C.; Donovan, J.; Stochkendahl, M.J.; Biscardi, M.; Ammendolia, C.; Myburgh, C. Factors affecting return to work after injury or illness: Best evidence synthesis of systematic reviews. Chiropr. Man. Ther. 2016, 24, 32. [Google Scholar] [CrossRef]
- Weerdesteijn, K.H.N.; Schaafsma, F.; Bonefaas-Groenewoud, K.; Heymans, M.; Van der Beek, A.; Anema, J. Predicting return to work after long-term sickness absence with subjective health complaints: A prospective cohort study. BMC Public Health 2020, 20, 1095. [Google Scholar] [CrossRef]
- Van Duijn, M.; Burdorf, A. Influence of modified work on recurrence of sick leave due to musculoskeletal complaints. J. Rehabil. Med. 2008, 40, 576–581. [Google Scholar] [CrossRef][Green Version]
- Durand, M.J.; Corbiere, M.; Coutu, M.F.; Reinharz, D.; Albert, V. A review of best work-absence management and return-to-work practices for workers with musculoskeletal or common mental disorders. Work 2014, 48, 579–589. [Google Scholar] [CrossRef]
- Buck, R.; Wynne-Jones, G.; Varnava, A.; Main, C.J.; Phillips, C.J. Working with musculoskeletal pain. Rev. Pain 2009, 3, 6–10. [Google Scholar] [CrossRef] [PubMed]
- Van der Noordt, M.; IJzelenburg, H.; Droomers, M.; Proper, K.I. Health effects of employment: A systematic review of prospective studies. Occup. Environ. Med. 2014, 71, 730–736. [Google Scholar] [CrossRef]
- De Vries, G.; Koeter, M.W.; Nieuwenhuijsen, K.; Hees, H.L.; Schene, A.H. Predictors of impaired work functioning in employees with major depression in remission. J. Affect. Disord. 2015, 185, 180–187. [Google Scholar] [CrossRef] [PubMed]
- Noordik, E.; Nieuwenhuijsen, K.; Varekamp, I.; Van der Klink, J.J.; Van Dijk, F.J. Exploring the return-to-work process for workers partially returned to work and partially on long-term sick leave due to common mental disorders: A qualitative study. Disabil. Rehabil. 2011, 33, 1625–1635. [Google Scholar] [CrossRef] [PubMed]
- The Dutch Social Security Institute: The Institute for Employee Benefits Schemes. CAS: Classification of symptoms, diseases and causes for occupational and insurence physicians. Amsterdam: The Dutch Social Security Institute; 2002 [Updated 2010]. Available online: https://www.steungroep.nl/images/her_keuring_WIA_of_WAO/Wetten_en_regels_bij_her_keuring/CAS_Classificaties_voor_Arbo_en_SV_UWV_2002.pdf (accessed on 1 January 2002).
- World Health Organization (WHO). Manual of the International Statistical Classification of Diseases, Injuries, and Causes of Death. Geneva: WHO. 1977. Available online: https://apps.who.int/iris/handle/10665/40492 (accessed on 1 January 2010).
- Robbins, J.M.; Kirmayer, L.J.; Hemami, S. Latent variable models of functional somatic distress. J. Nerv. Ment. Dis. 1997, 185, 606–615. [Google Scholar] [CrossRef]
- Wade, D.T.; Halligan, P.W. The biopsychosocial model of illness: A model whose time has come. Clin. Rehabil. 2017, 31, 995–1004. [Google Scholar] [CrossRef]
- Vendrig, A.A.; Schaafsma, F.G. Reliability and validity of the work and well-being inventory (WBI) for employees. J. Occup. Rehabil. 2018, 28, 377–390. [Google Scholar] [CrossRef]
- Terluin, B.; Brouwers, E.P.; Van Marwijk, H.W.; Verhaak, P.; Van der Horst, H.E. Detecting depressive and anxiety disorders in distressed patients in primary care; comparative diagnostic accuracy of the Four-Dimensional Symptom Questionnaire (4DSQ) and the Hospital Anxiety and Depression Scale (HADS). BMC Fam. Pract. 2009, 10, 58. [Google Scholar] [CrossRef]
- De Vroege, L.; Hoedeman, R.; Nuyen, J.; Sijtsma, K.; Van der Feltz-Cornelis, C.M. Validation of the PHQ-15 for somatoform disorder in the occupational health care setting. J. Occup. Rehabil. 2012, 22, 51–58. [Google Scholar] [CrossRef]
- Aaronson, N.K.; Muller, M.; Cohen, P.D.; Essink-Bot, M.L.; Fekkes, M.; Sanderman, R. Translation, validation, and norming of the Dutch language version of the SF-36 Health Survey in community and chronic disease populations. J. Clin. Epidemiol. 1998, 51, 1055–1068. [Google Scholar] [CrossRef]
- Ware, J.; Kosinski, M.; Keller, S.D. SF-36 Physical and Mental Health Summary Scales: A User’s Manual, 5th ed.; Health Institute New England Medical Center: Boston, MA, USA, 1994; p. 191. [Google Scholar]
- Speckens, A.E.; Spinhoven, P.; Sloekers, P.P.; Bolk, J.H.; Van Hemert, A.M. A validation study of the Whitely Index, the Illness Attitude Scales, and the Somatosensory Amplification Scale in general medical and general practice patients. J. Psychosom. Res. 1996, 40, 95–104. [Google Scholar] [CrossRef]
- El Fassi, M.; Bocquet, V.; Majery, N.; Lair, M.L.; Couffignal, S.; Mairiaux, P. Work ability assessment in a worker population: Comparison and determinants of Work Ability Index and Work Ability score. BMC Public Health 2013, 13, 305. [Google Scholar] [CrossRef] [PubMed]
- Marhold, C.; Linton, S.J.; Melin, L. Identification of obstacles for chronic pain patients to return to work: Evaluation of a questionnaire. J. Occup. Rehabil. 2002, 12, 65–75. [Google Scholar] [CrossRef] [PubMed]
- Field, A. Discovering Statistics Using IBM SPSS Statistics, 4th ed.; Sage Publications Ltd.: London, UK, 2015. [Google Scholar]
- Moons, K.G.; Altman, D.G.; Reitsma, J.B.; Ioannidis, J.P.; Macaskill, P.; Steyerberg, E.W. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): Explanation and elaboration. Ann. Intern. Med. 2015, 162, W1–W73. [Google Scholar] [CrossRef] [PubMed]
- Steyerberg, E.W. Clinical Prediction Models: A Practical Approach to Development, Validation, and Updating, 1st ed.; Springer: New York, NY, USA, 2009. [Google Scholar]
- Murgatroyd, D.F.; Casey, P.P.; Cameron, I.D.; Harris, I.A. The effect of financial compensation on health outcomes following musculoskeletal injury: Systematic review. PLoS ONE 2015, 10, e0117597. [Google Scholar] [CrossRef] [PubMed]
- Cassidy, J.D.; Carroll, L.J.; Cote, P.; Lemstra, M.; Berglund, A.; Nygren, A. Effect of eliminating compensation for pain and suffering on the outcome of insurance claims for whiplash injury. New Engl. J. Med. 2000, 342, 1179–1186. [Google Scholar] [CrossRef]
- Organisation for Economic Co-operation and Development (OECD). Transforming Disability into Ability: Policies to Promote Work and Income Security for Disabled People. Paris: OECD. 2003. Available online: https://read.oecd-ilibrary.org/social-issues-migration-health/transforming-disability-into-ability_9789264158245-en#page1 (accessed on 1 January 2003).
- Sheehan, L.R.; Lane, T.J.; Collie, A. The impact of income sources on financial stress in workers’ compensation claimants. J. Occup. Rehabil. 2020. [Google Scholar] [CrossRef]
- Wynne-Jones, G.; Buck, R.; Varnava, A.; Phillips, C.J.; Main, C.J. Impacts on work performance; what matters 6 months on? Occup. Med. 2011, 61, 205–208. [Google Scholar] [CrossRef]
- Butterworth, P.; Leach, L.S.; Pirkis, J.; Kelaher, M. Poor mental health influences risk and duration of unemployment: A prospective study. Soc. Psychiatry Psychiatr. Epidemiol. 2012, 47, 1013–1021. [Google Scholar] [CrossRef]
- Arends, I.; Almansa, J.; Stansfeld, S.A.; Amick, B.C.; Van der Klink, J.J.L.; Bultmann, U. One-year trajectories of mental health and work outcomes post return to work in patients with common mental disorders. J. Affect. Disord. 2019, 257, 263–270. [Google Scholar] [CrossRef]
- Laisne, F.; Lecomte, C.; Corbiere, M. Biopsychosocial predictors of prognosis in musculoskeletal disorders: A systematic review of the literature (corrected and republished). Disabil. Rehabil. 2012, 34, 1912–1941. [Google Scholar] [CrossRef] [PubMed]
- Lofgren, M.; Ekholm, J.; Ohman, A. ‘A constant struggle’: Successful strategies of women in work despite fibromyalgia. Disabil. Rehabil. 2006, 28, 447–455. [Google Scholar] [CrossRef] [PubMed]
- Van Rhenen, W.; Schaufeli, W.B.; Van Dijk, F.J.; Blonk, R.W. Coping and sickness absence. Int. Arch. Occup. Environ. Health 2008, 81, 461–472. [Google Scholar] [CrossRef] [PubMed]
- Etuknwa, A.; Daniels, K.; Eib, C. Sustainable return to work: A systematic review focusing on personal and social factors. J. Occup. Rehabil. 2019, 29, 679–700. [Google Scholar] [CrossRef]
- Lazarus, R.S.; Folkman, S. Stress, Appraisal, and Coping, 1st ed.; Springer Publishing Company: New York, NY, USA, 1984. [Google Scholar]
- Varekamp, I.; Verbeek, J.H.; Van Dijk, F.J. How can we help employees with chronic diseases to stay at work? A review of interventions aimed at job retention and based on an empowerment perspective. Int. Arch. Occup. Environ. Health 2006, 80, 87–97. [Google Scholar] [CrossRef]
- Brenninkmeijer, V.; Lagerveld, S.E.; Blonk, R.W.B. Moeilijk objectiveerbare klachten in de praktijk van de bedrijfs- en verzekeringsarts [Symptoms difficult to objectify in occupational and insurance health care]. Tijdschr. Voor Bedr. Verzek. 2006, 14, 424–430. [Google Scholar] [CrossRef]
- Van Poppel, M.N.; De Vet, H.C.; Koes, B.W.; Smid, T.; Bouter, L.M. Measuring sick leave: A comparison of self-reported data on sick leave and data from company records. Occup. Med. 2002, 52, 485–490. [Google Scholar] [CrossRef]
- Kontopantelis, E.; White, I.R.; Sperrin, M.; Buchan, I. Outcome-sensitive multiple imputation: A simulation study. BMC Med Res. Methodol. 2017, 17, 2. [Google Scholar] [CrossRef]
| SHC 1 (No 2 = 86) | Other Disorders (No = 433) | ||||
|---|---|---|---|---|---|
| Domains | Categories/Ranges | Mean/No | SD 3/% | Mean/No | SD/% |
| Demographic | |||||
| Age in years | 18–65 | 47.12 | 10.46 | 50.90 | 9.21 |
| Gender | Male | 29 | 34% | 206 | 48% |
| Married or partner | Yes | 69 | 80% | 321 | 74% |
| Breadwinner of the family | Yes | 49 | 57% | 296 | 68% |
| Land of birth | The Netherlands | 78 | 91% | 393 | 91% |
| Educational level | Primary/Secondary school | 33 | 38% | 170 | 39% |
| High school | 27 | 32% | 145 | 34% | |
| Bachelor’s/Master’s degree | 26 | 30% | 118 | 27% | |
| Socio-economic and work-related | |||||
| Collar job | Blue | 14 | 16% | 105 | 24% |
| White | 31 | 36% | 158 | 37% | |
| Pink | 41 | 48% | 170 | 39% | |
| Employed | Yes | 75 | 87% | 378 | 87% |
| Usual working time in hours | 4–60 | 30.84 | 8.31 | 33.20 | 8.69 |
| Regular work schedule | Yes | 59 | 69% | 309 | 71% |
| Managerial position | Yes | 15 | 17% | 62 | 14% |
| Job demands | Psychological | 20 | 23% | 154 | 36% |
| Physical | 36 | 42% | 132 | 30% | |
| Combination of both | 30 | 35% | 147 | 34% | |
| Stressors4 | 16–64 | 35.84 | 9.11 | 35.64 | 8.39 |
| Support4 | 21–84 | 60.79 | 10.49 | 61.41 | 11.38 |
| Previous absenteeism for the same health complaint | Yes | 39 | 45% | 230 | 53% |
| Work disability benefits | No/Partial | 73 | 85% | 301 | 70% |
| Adjustments at work | Yes | 70 | 81% | 360 | 83% |
| Interventions at work (e.g., job coaching) | Yes | 77 | 89% | 392 | 91% |
| Health-related | |||||
| Use of specialist care in the last 2 years | Yes | 73 | 85% | 363 | 84% |
| Use of psychiatric care in the last 2 years | Yes | 52 | 61% | 213 | 49% |
| Use of medication | Yes | 61 | 71% | 368 | 85% |
| Depressive disorder5 | 0–21 | 7.60 | 4.10 | 7.66 | 4.62 |
| Anxiety disorder5 | 0–21 | 7.40 | 4.06 | 8.07 | 4.17 |
| Severity of complaints6 | 5–30 | 11.83 | 5.04 | 10.91 | 4.37 |
| Physical health7 | 0–100 | 31.96 | 8.58 | 34.29 | 9.59 |
| Mental health7 | 0–100 | 40.78 | 12.48 | 38.63 | 13.07 |
| Health compared to a year ago7 | Worse | 28 | 33% | 163 | 38% |
| Hypochondria8 | 0–14 | 5.28 | 2.93 | 5.38 | 2.98 |
| Symptom scale4 | 20–80 | 41.01 | 9.20 | 41.37 | 10.39 |
| Coping strategies4 | 17–68 | 40.68 | 9.37 | 41.17 | 9.51 |
| Self-perceived ability | |||||
| Positive expectations for staying at work | Yes/Inconclusive | 43 | 50% | 271 | 63% |
| Disability4 | 7–28 | 21.70 | 4.65 | 20.54 | 4.90 |
| Work ability in general9 | 0–10 | 4.14 | 2.04 | 4.64 | 1.96 |
| Work ability in the context of work load9 | 2–10 | 5.82 | 1.52 | 6.15 | 1.50 |
| Possibilities for returning to work10 | 0–36 | 15.00 | 8.85 | 14.77 | 9.54 |
| Domains | Categories/Ranges | OR 1 | 95% CI 2 | p |
|---|---|---|---|---|
| Demographic | ||||
| Age in years | 18–65 | 0.99 | 0.95–1.03 | 0.51 |
| Gender | Male | Reference | - | |
| Female | 0.97 | 0.40–2.37 | 0.94 | |
| Married or partner | No | Reference | - | |
| Yes | 0.92 | 0.32–2.65 | 0.87 | |
| Breadwinner of the family | No | Reference | - | |
| Yes | 1.19 | 0.51–2.81 | 0.69 | |
| Land of birth | The Netherlands | Reference | - | |
| Other country | 0.29 | 0.05–1.50 | 0.14 | |
| Educational level | Primary/Secondary school | Reference | - | |
| High school | 2.55 | 0.90–7.24 | 0.08 | |
| Bachelor’s/Master’s degree | 2.80 | 0.97–8.10 | 0.06 | |
| Socio-economic and work-related | ||||
| Collar job | Blue | Reference | - | |
| White | 1.62 | 0.45–5.78 | 0.46 | |
| Pink | 1.40 | 0.41–4.76 | 0.59 | |
| Employed | No | Reference | - | |
| Yes | 0.56 | 0.15–2.06 | 0.38 | |
| Usual working time in hours | 4–60 | 1.03 | 0.98–1.08 | 0.30 |
| Regular work schedule | No | Reference | - | |
| Yes | 0.77 | 0.31–1.93 | 0.58 | |
| Managerial position | No | Reference | - | |
| Yes | 1.11 | 0.36–3.39 | 0.85 | |
| Job demands | Psychological | Reference | - | |
| Physical | 1.02 | 0.34–3.07 | 0.97 | |
| Combination of both | 0.63 | 0.20–1.96 | 0.42 | |
| Stressors3 | 16–64 | 0.98 | 0.94–1.03 | 0.41 |
| Support3 | 21–84 | 1.03 | 0.99–1.08 | 0.14 |
| Previous absenteeism for the same health complaint | No | Reference | - | |
| Yes | 0.32 | 0.13–0.77 | 0.01 | |
| Work disability benefits | No/Partial | Reference | - | |
| Full | 0.06 | 0.01–0.47 | 0.01 | |
| Adjustments at work | No | Reference | - | |
| Yes | 1.44 | 0.48–4.30 | 0.51 | |
| Interventions at work (e.g., job coaching) | No | Reference | - | |
| Yes | 0.82 | 0.21–3.29 | 0.78 | |
| Health-related | ||||
| Use of specialist care for the last 2 years | No | Reference | - | |
| Yes | 0.88 | 0.27–2.88 | 0.83 | |
| Use of psychiatric care for the last 2 years | No | Reference | - | |
| Yes | 0.89 | 0.37–2.11 | 0.79 | |
| Use of medication | No | Reference | - | |
| Yes | 0.22 | 0.08–0.63 | 0.01 | |
| Depressive disorder4 | 0–21 | 0.89 | 0.80–0.99 | 0.05 |
| Anxiety disorder4 | 0–21 | 0.94 | 0.85–1.05 | 0.28 |
| Severity of complaints5 | 5–30 | 0.85 | 0.77–0.94 | 0.002 |
| Physical health6 | 0–100 | 1.03 | 0.98–1.09 | 0.21 |
| Mental health6 | 0–100 | 1.04 | 1.00–1.07 | 0.05 |
| Health compared to a year ago6 | Worse | Reference | - | |
| Same/Better | 3.21 | 1.24–8.32 | 0.02 | |
| Hypochondria7 | 0–14 | 0.82 | 0.70–0.97 | 0.02 |
| Symptom scale3 | 20–80 | 0.96 | 0.91–1.00 | 0.07 |
| Coping strategies3 | 17–68 | 1.05 | 1.00–1.10 | 0.06 |
| Self-perceived ability | ||||
| Positive expectations for staying at work | No | Reference | - | |
| Yes/Inconclusive | 3.87 | 1.58–9.46 | 0.003 | |
| Disability3 | 7–28 | 0.92 | 0.83–1.01 | 0.08 |
| Work ability in general8 | 0–10 | 1.25 | 1.00–1.56 | 0.05 |
| Work ability in the context of work load8 | 2–10 | 1.36 | 1.00–1.85 | 0.05 |
| Possibilities for returning to work9 | 0–36 | 1.02 | 0.97–1.07 | 0.54 |
| Domains | Categories/Ranges | OR 1 | 95% CI 2 | p |
|---|---|---|---|---|
| Demographic | ||||
| Educational level | Primary/Secondary school | Reference | - | |
| High school | 2.55 | 0.90–7.24 | 0.08 | |
| Bachelor’s/Master’s degree | 2.80 | 0.97–8.10 | 0.06 | |
| Socio-economic and work-related | ||||
| Support3 | 21–84 | 1.04 | 0.99–1.09 | 0.11 |
| Previous absenteeism for the same health complaint | No | Reference | - | |
| Yes | 0.33 | 0.13–0.87 | 0.03 | |
| Work disability benefits | No/Partial | Reference | - | |
| Full | 0.06 | 0.01–0.48 | 0.01 | |
| Health-related | ||||
| Use of medication | No | Reference | - | |
| Yes | 0.40 | 0.12–1.31 | 0.13 | |
| Severity of complaints4 | 5–30 | 0.90 | 0.79–1.03 | 0.12 |
| Mental Health5 | 0–100 | 1.05 | 1.00–1.11 | 0.07 |
| Health compared to a year ago5 | Worse | Reference | - | |
| Same/Better | 2.77 | 0.87–8.80 | 0.08 | |
| Coping strategies3 | 17–68 | 1.08 | 1.01–1.15 | 0.02 |
| Self-perceived ability | ||||
| Positive expectations for staying at work | No | Reference | - | |
| Yes/Inconclusive | 3.44 | 1.38–8.58 | 0.01 | |
| Work ability in the context of work load6 | 2–10 | 1.27 | 0.92–1.74 | 0.14 |
| SHC (No 1 = 86) | Other Disorders (No = 433) | ||||||
|---|---|---|---|---|---|---|---|
| Domains | Categories/Ranges | OR 2 | 95% CI 3 | p | OR | 95% CI | p |
| Socio-economic and work-related | |||||||
| Previous absenteeism for the same health complaint | No | Reference | Reference | ||||
| Yes | 0.31 | 0.10–0.96 | 0.04 | 0.72 | 0.46–1.13 | 0.16 | |
| Work disability benefits | No/Partial | Reference | Reference | ||||
| Full | 0.07 | 0.01–0.64 | 0.02 | 0.13 | 0.08–0.21 | 0.000 | |
| Health-related | |||||||
| Mental Health4 | 0–100 | 1.08 | 1.02–1.14 | 0.01 | 1.03 | 1.01–1.05 | 0.002 |
| Coping strategies5 | 17–68 | 1.13 | 1.04–1.23 | 0.004 | 1.02 | 1.00–1.04 | 0.23 |
| Self-perceived ability | |||||||
| Positive expectations for staying at work | No | Reference | Reference | ||||
| Yes/Inconclusive | 6.49 | 2.00–21.09 | 0.002 | 3.15 | 2.00–4.97 | 0.000 | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Weerdesteijn, K.; Schaafsma, F.; Bonefaas-Groenewoud, K.; Heymans, M.; Van der Beek, A.; Anema, J. Prognostic Factors for Staying at Work for Partially Sick-Listed Workers with Subjective Health Complaints: A Prospective Cohort Study. Int. J. Environ. Res. Public Health 2020, 17, 7184. https://doi.org/10.3390/ijerph17197184
Weerdesteijn K, Schaafsma F, Bonefaas-Groenewoud K, Heymans M, Van der Beek A, Anema J. Prognostic Factors for Staying at Work for Partially Sick-Listed Workers with Subjective Health Complaints: A Prospective Cohort Study. International Journal of Environmental Research and Public Health. 2020; 17(19):7184. https://doi.org/10.3390/ijerph17197184
Chicago/Turabian StyleWeerdesteijn, Kristel, Frederieke Schaafsma, Karin Bonefaas-Groenewoud, Martijn Heymans, Allard Van der Beek, and Johannes Anema. 2020. "Prognostic Factors for Staying at Work for Partially Sick-Listed Workers with Subjective Health Complaints: A Prospective Cohort Study." International Journal of Environmental Research and Public Health 17, no. 19: 7184. https://doi.org/10.3390/ijerph17197184
APA StyleWeerdesteijn, K., Schaafsma, F., Bonefaas-Groenewoud, K., Heymans, M., Van der Beek, A., & Anema, J. (2020). Prognostic Factors for Staying at Work for Partially Sick-Listed Workers with Subjective Health Complaints: A Prospective Cohort Study. International Journal of Environmental Research and Public Health, 17(19), 7184. https://doi.org/10.3390/ijerph17197184




