Risk Factors for Tooth Loss in Patients Undergoing Mid-Long-Term Maintenance: A Retrospective Study
Abstract
:1. Introduction
2. Materials and Methods
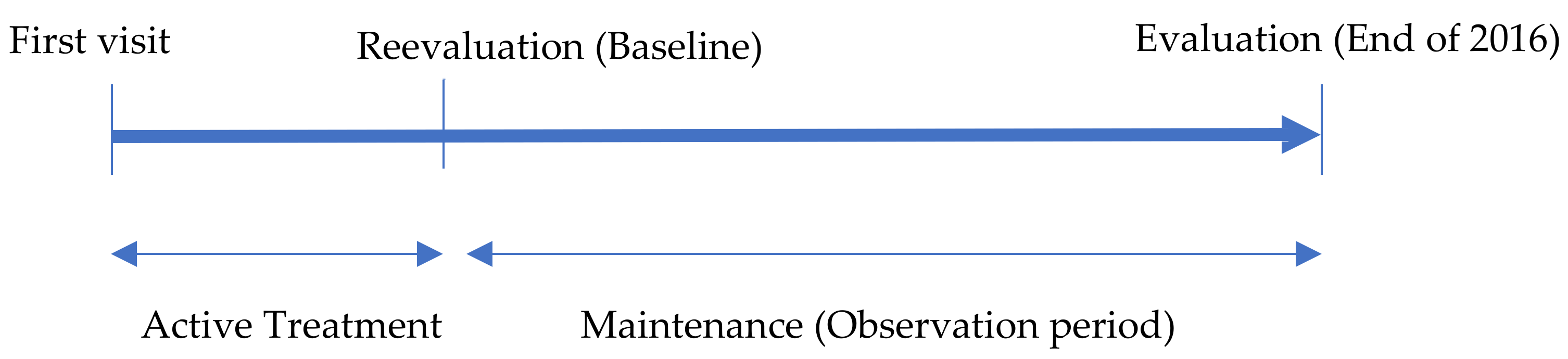
2.1. Study Design and Patient Sampling
2.2. Dental Treatment up to Maintenance
2.3. Baseline Status
2.4. Maintenance Criteria, Procedure, Interval, and Compliance
2.5. Cause and Status of Tooth Loss under Maintenance
2.6. Data Collection
2.7. Statistical Analysis
2.8. Ethics Approval and Consent to Participate
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Morita, M.; Kimura, T.; Kanegae, M.; Ishikawa, A.; Watanabe, T. Reasons for extraction of permanent teeth in Japan. Community Dent. Oral Epidemiol. 1994, 22, 303–306. [Google Scholar] [CrossRef] [PubMed]
- Stabholz, A.; Babayof, I.; Mersel, A.; Mann, J. The reasons for tooth loss in geriatric patients attending two surgical clinics in Jerusalem, Israel. Gerodontology 1997, 14, 83–88. [Google Scholar] [CrossRef] [PubMed]
- Sayegh, A.; Hilow, H.; Bedi, R. Pattern of tooth loss in recipients of free dental treatment at the University Hospital of Amman, Jordan. J. Oral Rehabil. 2004, 31, 124–130. [Google Scholar] [CrossRef] [PubMed]
- Al-Shammari, K.F.; Al-Ansari, J.M.; Al-Melh, M.A.; Al-Khabbaz, A.K. Reasons for tooth extraction in Kuwait. Med. Princ. Pract. 2006, 15, 417–422. [Google Scholar] [CrossRef]
- Montandon, A.A.B.; Zuza, E.P.; Toledo, B.E.C. Prevalence and reasons for tooth loss in a sample from a dental clinic in Brazil. Int. J. Dent. 2012, 2012, 719750. [Google Scholar] [CrossRef] [Green Version]
- Axelsson, P.; Lindhe, J. Effect of controlled oral hygiene procedures on caries and periodontal disease in adults. Results after 6 years. J. Clin. Periodontol. 1981, 8, 239–248. [Google Scholar] [CrossRef]
- Axelsson, P.; Nystrom, B.; Lindhe, J. The long-term effect of a plaque control program on tooth mortality, caries and periodontal disease in adults. Results after 30 years of maintenance. J. Clin. Periodontol. 2004, 31, 749–757. [Google Scholar] [CrossRef]
- Hirschfeld, L.; Wasserman, B. A long-term survey of tooth loss in 600 treated periodontal patients. J. Periodontol. 1978, 49, 225–237. [Google Scholar] [CrossRef] [Green Version]
- McFall, W.T., Jr. Tooth loss in 100 treated patients with periodontal disease. A long-term study. J. Periodontol. 1982, 53, 539–549. [Google Scholar] [CrossRef]
- Goldman, M.J.; Ross, I.F.; Goteiner, D. Effect of periodontal therapy on patients maintained for 15 years or longer. A retrospective study. J. Periodontol. 1986, 57, 347–353. [Google Scholar] [CrossRef]
- Wood, W.R.; Greco, G.W.; McFall, W.T., Jr. Tooth loss in patients with moderate periodontitis after treatment and long-term maintenance care. J. Periodontol. 1989, 60, 516–520. [Google Scholar] [CrossRef] [PubMed]
- Fardal, O.; Johannessen, A.C.; Linden, G.J. Tooth loss during maintenance following periodontal treatment in a periodontal practice in Norway. J. Clin. Periodontol. 2004, 31, 550–555. [Google Scholar] [CrossRef] [PubMed]
- Costa, F.O.; Lages, E.J.; Cota, L.O.; Lorentz, T.C.; Soares, R.V.; Cortelli, J.R. Tooth loss in individuals under periodontal maintenance therapy: 5-year prospective study. J. Periodontal Res. 2014, 49, 121–128. [Google Scholar] [CrossRef] [PubMed]
- Stadler, A.F.; Mendez, M.; Oppermann, R.V.; Gomes, S.C. Tooth loss in patients under periodontal maintenance in a private practice: A retrospective study. Braz. Dent. J. 2017, 28, 440–446. [Google Scholar] [CrossRef] [Green Version]
- Ravald, N.; Johansson, C.S. Tooth loss in periodontally treated patients: A long-term study of periodontal disease and root caries. J. Clin. Periodontol. 2012, 39, 73–79. [Google Scholar] [CrossRef]
- Costa, F.O.; Santuchi, C.C.; Lages, E.J.; Cota, L.O.; Cortelli, S.C.; Cortelli, J.R.; Lorentz, T.C.; Costa, J.E. Prospective study in periodontal maintenance therapy: Comparative analysis between academic and private practices. J. Periodontol. 2012, 83, 301–311. [Google Scholar] [CrossRef]
- Pretzl, B.; Eickholz, P.; Saure, D.; Pfefferle, T.; Zeidler, A.; Dannewitz, B. Endodontic status and retention of molars in periodontally treated patients: Results after 10 or more years of supportive periodontal therapy. J. Clin. Periodontol. 2016, 43, 1116–1123. [Google Scholar] [CrossRef]
- Suzuki, S.; Yoshino, K.; Takayanagi, A.; Sugiyama, S.; Okamoto, M.; Tanaka, M.; Ishizuka, Y.; Satou, R.; Onose, Y.; Kamijo, H.; et al. Number of non-vital teeth as indicator of tooth loss during 10-year maintenance: A retrospective study. Bull. Tokyo Dent. Coll. 2017, 58, 223–230. [Google Scholar] [CrossRef] [Green Version]
- Marcus, S.E.; Drury, T.F.; Brown, L.J.; Zion, G.R. Tooth retention and tooth loss in the permanent dentition of adults: United States, 1988–1991. J. Dent. Res. 1996, 75, 684–695. [Google Scholar] [CrossRef]
- Downer, M.C. The improving dental health of United Kingdom adults and prospects for the future. Br. Dent. J. 1991, 170, 154–158. [Google Scholar] [CrossRef]
- Yoshino, K.; Ito, K.; Kuroda, M.; Sugihara, N. Tooth loss in problem-oriented, irregular, and regular attenders at dental offices. Bull. Tokyo Dent. Coll. 2016, 57, 11–19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saito, M.; Shimazaki, Y.; Fukai, K.; Furuta, M.; Aida, J.; Ando, Y.; Miyazaki, H.; Kambara, M. Risk factors for tooth loss in adult Japanese dental patients: 8020 promotion foundation study. J. Investig. Clin. Dent. 2019, 10, e12392. [Google Scholar] [CrossRef] [PubMed]
- Bratthall, D.; Hansel Petersson, G. Cariogram—A multifactorial risk assessment model for a multifactorial disease. Community Dent. Oral Epidemiol. 2005, 33, 256–264. [Google Scholar] [CrossRef] [PubMed]
- Page, R.C.; Martin, J.A.; Loeb, C.F. The Oral Health Information Suite (OHIS): Its use in the management of periodontal disease. J. Dent. Educ. 2005, 69, 509–520. [Google Scholar] [CrossRef]
- Miyamoto, T.; Kumagai, T.; Jones, J.A.; Van Dyke, T.E.; Nunn, M.E. Compliance as a prognostic indicator: Retrospective study of 505 patients treated and maintained for 15 years. J. Periodontol. 2006, 77, 223–232. [Google Scholar] [CrossRef]
- Lee, C.T.; Huang, H.Y.; Sun, T.C.; Karimbux, N. Impact of patient compliance on tooth loss during supportive periodontal therapy: A systematic review and meta-analysis. J. Dent. Res. 2015, 94, 777–786. [Google Scholar] [CrossRef]
- Lorentz, T.C.; Cota, L.O.; Cortelli, J.R.; Vargas, A.M.; Costa, F.O. Tooth loss in individuals under periodontal maintenance therapy: Prospective study. Braz. Oral Res. 2010, 24, 231–237. [Google Scholar] [CrossRef]
- Tonetti, M.S.; Greenwell, H.; Kornman, K.S. Staging and grading of periodontitis: Framework and proposal of a new classification and case definition. J. Periodontol. 2018, 89 (Suppl. 1), S159–S172. [Google Scholar] [CrossRef] [Green Version]
- Al-Shammari, K.F.; Al-Khabbaz, A.K.; Al-Ansari, J.M.; Neiva, R.; Wang, H.L. Risk indicators for tooth loss due to periodontal disease. J. Periodontol. 2005, 76, 1910–1918. [Google Scholar] [CrossRef]
- Miranda-Rius, J.; Brunet-Llobet, L.; Lahor-Soler, E.; Farre, M. Salivary secretory disorders, inducing drugs, and clinical management. Int. J. Med. Sci. 2015, 12, 811–824. [Google Scholar] [CrossRef] [Green Version]
- Burt, B.A.; Ismail, A.I.; Morrison, E.C.; Beltran, E.D. Risk factors for tooth loss over a 28-year period. J. Dent. Res. 1990, 69, 1126–1130. [Google Scholar] [CrossRef]
- Eklund, S.A.; Burt, B.A. Risk factors for total tooth loss in the United States; longitudinal analysis of national data. J. Public Health Dent. 1994, 54, 5–14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pretzl, B.; Kaltschmitt, J.; Kim, T.S.; Reitmeir, P.; Eickholz, P. Tooth loss after active periodontal therapy 2: Tooth-related factors. J. Clin. Periodontol. 2008, 35, 175–182. [Google Scholar] [CrossRef] [PubMed]
- Muller, S.; Eickholz, P.; Reitmeir, P.; Eger, T. Long-term tooth loss in periodontally compromised but treated patients according to the type of prosthodontic treatment. A retrospective study. J. Oral Rehabil. 2013, 40, 358–367. [Google Scholar] [CrossRef] [PubMed]
- Ando, A.; Ohsawa, M.; Yaegashi, Y.; Sakata, K.; Tanno, K.; Onoda, T.; Itai, K.; Tanaka, F.; Makita, S.; Omama, S. Factors related to tooth loss among community-dwelling middle-aged and elderly Japanese men. J. Epidemiol. 2013, 23, 301–306. [Google Scholar] [CrossRef] [Green Version]
- Jorkjend, L.; Johansson, A.; Johansson, A.K.; Bergenholtz, A. Periodontitis, caries and salivary factors in Sjogren’s syndrome patients compared to sex- and age-matched controls. J. Oral Rehabil. 2003, 30, 369–378. [Google Scholar] [CrossRef]
| Sample Size | Age (Years) | Year (Years) | RT (Number of Teeth) | Total Number of Teeth Lost | Cause of Tooth Loss | Tooth Loss/Year Per Patient | |||
|---|---|---|---|---|---|---|---|---|---|
| Dental Caries | Periodontal Disease | Root Fracture | Other | ||||||
| N | Mean ± SD | Number of Teeth | |||||||
| 674 | 54.3 ± 8.0 | 9.3 ± 2.6 | 23.0 ± 5.5 | 572 | 127 | 66 | 355 | 24 | 0.09 |
| Observation Period (Years) | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Number of Patients | 75 | 84 | 63 | 102 | 112 | 68 | 43 | 46 | 42 | 39 | 674 |
| Cause of Tooth Loss | Number of Vital Teeth (%) | Number of Non-Vital Teeth (%) | Total Number of Teeth (%) |
|---|---|---|---|
| Dental caries | 2 (0.3%) | 125 (21.9%) | 127 (22.2%) |
| Periodontal disease | 31 (5.4%) | 35 (6.1%) | 66 (11.5%) |
| Root fracture | 3 (0.5%) | 352 (61.5%) | 355 (62.1%) |
| Other | 11 (2.0%) | 13 (2.3%) | 24 (4.2%) |
| Total (%) | 47 (8.2%) | 525 (91.7%) | 572 (100%) |
| Variables | Sample Size | Age (Years) | Year (Years) | RT (Number of Teeth) | Tooth Loss (Number of Teeth) | Tooth Loss /Patient/Year (Number of Teeth) | Logistic Regression Analyses | ||
|---|---|---|---|---|---|---|---|---|---|
| N | Mean ± SD | Mean ± SD | Mean ± SD | Odds Ratio (95% CI) | p-Value | ||||
| Compliance | Regular | 636 (94.4%) | 54.2 ± 7.9 | 9.3 ± 2.5 | 23.0 ± 5.4 | 528 (92.3%) | 0.09 | 1 | |
| Irregular | 38 (5.6%) | 54.7 ± 7.6 | 7.8 ± 2.0 | 22.2 ± 6.0 | 44 (7.7%) | 0.15 | 1.89 (0.97–3.66) | 0.06 | |
| Sex | Male | 265 (39.3%) | 54.6 ± 8.0 | 9.1 ± 2.6 | 22.8 ± 5.4 | 238 (41.6%) | 0.10 | 1 | |
| Female | 409 (60.7%) | 54.0 ± 7.9 | 9.3 ± 2.5 | 23.0 ± 5.4 | 334 (58.4%) | 0.09 | 0.82 (0.60–1.12) | 0.20 | |
| SM | No | 548 (75.5%) | 54.6 ± 7.8 | 9.2 ± 2.5 | 23.0 ± 5.5 | 478 (83.6%) | 0.09 | 1 | |
| Yes | 126 (18.7%) | 52.6 ± 8.1 | 8.7 ± 2.5 | 22.4 ± 5.5 | 94 (16.4%) | 0.09 | 0.92 (0.62–1.36) | 0.66 | |
| SSI | No | 509 (75.5%) | 52.9 ± 7.8 | 9.0 ± 2.5 | 23.2 ± 5.4 | 503 (88.0%) | 0.09 | 1 | |
| Yes | 165 (24.5%) | 58.2 ± 6.8 | 9.9 ± 2.5 | 22.2 ± 5.3 | 69 (12.0%) | 0.16 | 1.53 (1.07–2.17) | 0.02 | |
| DM | No | 628 (93.2%) | 53.9 ± 8.0 | 9.2 ± 2.5 | 23.0 ± 5.4 | 503 (88.0%) | 0.09 | 1 | |
| Yes | 46 (6.8%) | 58.2 ± 6.0 | 9.6 ± 2.6 | 21.5 ± 5.3 | 69 (12.0%) | 0.16 | 1.79 (0.98–3.28) | 0.06 | |
| AGE | 40–54 | 332 (49.3%) | 47.4 ± 4.4 | 9.2 ± 2.6 | 24.7 ± 4.2 | 197 (34.4%) | 0.06 | 1 | |
| 55–69 | 342 (50.7%) | 61.0 ± 3.9 | 9.3 ± 2.6 | 21.3 ± 5.9 | 375 (65.6%) | 0.18 | 1.58 (1.17–2.15) | 0.003 | |
| RT | 28–25 | 366 (54.3%) | 51.7 ± 7.9 | 9.2 ± 2.6 | 26.7 ± 1.1 | 195 (34.1%) | 0.06 | 1 | |
| ≤24 | 308 (45.7%) | 57.4 ± 6.8 | 9.4 ± 2.6 | 18.5 ± 5.2 | 377 (65.9%) | 0.13 | 2.33 (1.71–3.20) | ≤0.001 | |
| BL | Class 0–1 | 410 (60.8%) | 52.7 ± 8.2 | 9.2 ± 2.6 | 24.3 ± 4.6 | 315 (55.1%) | 0.08 | 1 | |
| Class 2–3 | 264 (39.2%) | 56.7 ± 7.0 | 9.4 ± 2.6 | 20.9 ± 6.0 | 257 (44.9%) | 0.10 | 1.17 (0.86–1.61) | 0.31 | |
| RD | No | 486 (69.4%) | 52.5 ± 8.0 | 9.2 ± 2.6 | 26.0 ± 1.7 | 290 (50.7%) | 0.07 | 1 | |
| Yes | 206 (30.6%) | 58.2 ± 6.3 | 9.4 ± 2.6 | 16.1 ± 4.8 | 283 (49.3%) | 0.15 | 2.18 (1.56–3.03) | ≤0.001 | |
| Variables | Coefficient | Standard Error | χ2 | Odds Ratio (95% CI) | p-Value | |
|---|---|---|---|---|---|---|
| Compliance | Regular | 1 | 0.09 | |||
| Irregular | 0.29 | 0.17 | 2.85 | 1.80 (0.91–3.57) | ||
| Sex | Men | 1 | 0.13 | |||
| Women | −0.14 | 0.09 | 2.25 | 0.76 (0.52–1.09) | ||
| SM | No | 1 | 0.23 | |||
| Yes | −0.14 | 0.12 | 1.42 | 0.75 (0.48–1.20) | ||
| SSI | No | 1 | 0.23 | |||
| Yes | 0.12 | 0.09 | 1.43 | 1.26 (0.86–1.85) | ||
| DM | No | 1 | 0.40 | |||
| Yes | 0.14 | 0.16 | 0.71 | 1.32 (0.69–2.52) | ||
| AGE | 40–54 | 1 | ||||
| 55–69 | 0.12 | 0.18 | 0.15 | 1.13 (0.80–1.60) | 0.47 | |
| RT | 28–25 | 1 | ||||
| ≤24 | 0.68 | 0.23 | 8.73 | 1.99 (1.26–3.14) | 0.003 | |
| BL | Class 0–1 | 1 | ||||
| Class 2–3 | 0.15 | 0.17 | 0.80 | 0.85 (0.60–1.21) | 0.37 | |
| RD | No | 1 | ||||
| Yes | 0.11 | 0.12 | 0.79 | 1.25 (0.76–2.03) | 0.37 | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kawahara, H.; Inoue, M.; Okura, K.; Oshima, M.; Matsuka, Y. Risk Factors for Tooth Loss in Patients Undergoing Mid-Long-Term Maintenance: A Retrospective Study. Int. J. Environ. Res. Public Health 2020, 17, 6258. https://doi.org/10.3390/ijerph17176258
Kawahara H, Inoue M, Okura K, Oshima M, Matsuka Y. Risk Factors for Tooth Loss in Patients Undergoing Mid-Long-Term Maintenance: A Retrospective Study. International Journal of Environmental Research and Public Health. 2020; 17(17):6258. https://doi.org/10.3390/ijerph17176258
Chicago/Turabian StyleKawahara, Hiroo, Miho Inoue, Kazuo Okura, Masamitsu Oshima, and Yoshizo Matsuka. 2020. "Risk Factors for Tooth Loss in Patients Undergoing Mid-Long-Term Maintenance: A Retrospective Study" International Journal of Environmental Research and Public Health 17, no. 17: 6258. https://doi.org/10.3390/ijerph17176258
APA StyleKawahara, H., Inoue, M., Okura, K., Oshima, M., & Matsuka, Y. (2020). Risk Factors for Tooth Loss in Patients Undergoing Mid-Long-Term Maintenance: A Retrospective Study. International Journal of Environmental Research and Public Health, 17(17), 6258. https://doi.org/10.3390/ijerph17176258








