Effectiveness of Social Measures against COVID-19 Outbreaks in Selected Japanese Regions Analyzed by System Dynamic Modeling
Abstract
:1. Introduction
1.1. COVID-19 Pandemic and Reactions by Society
1.2. Previous Studies and Research Questions
1.3. Analytical Approach Applied in This Study
2. Materials and Methods
2.1. Data on COVID-19 Epidemic in Japan
2.2. Data on Societal Factors
2.3. Modeling and Software
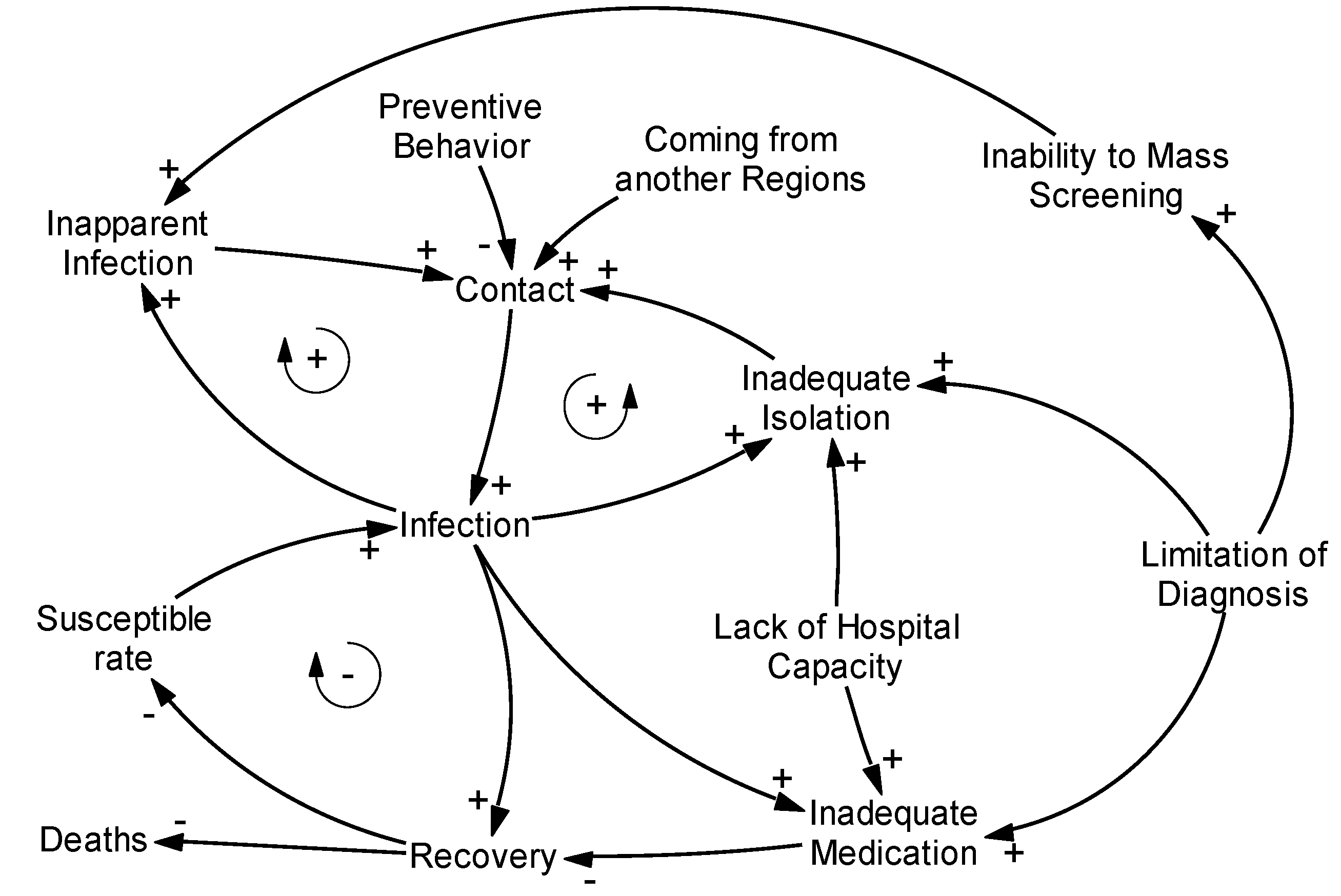
2.4. Causal Loop Model
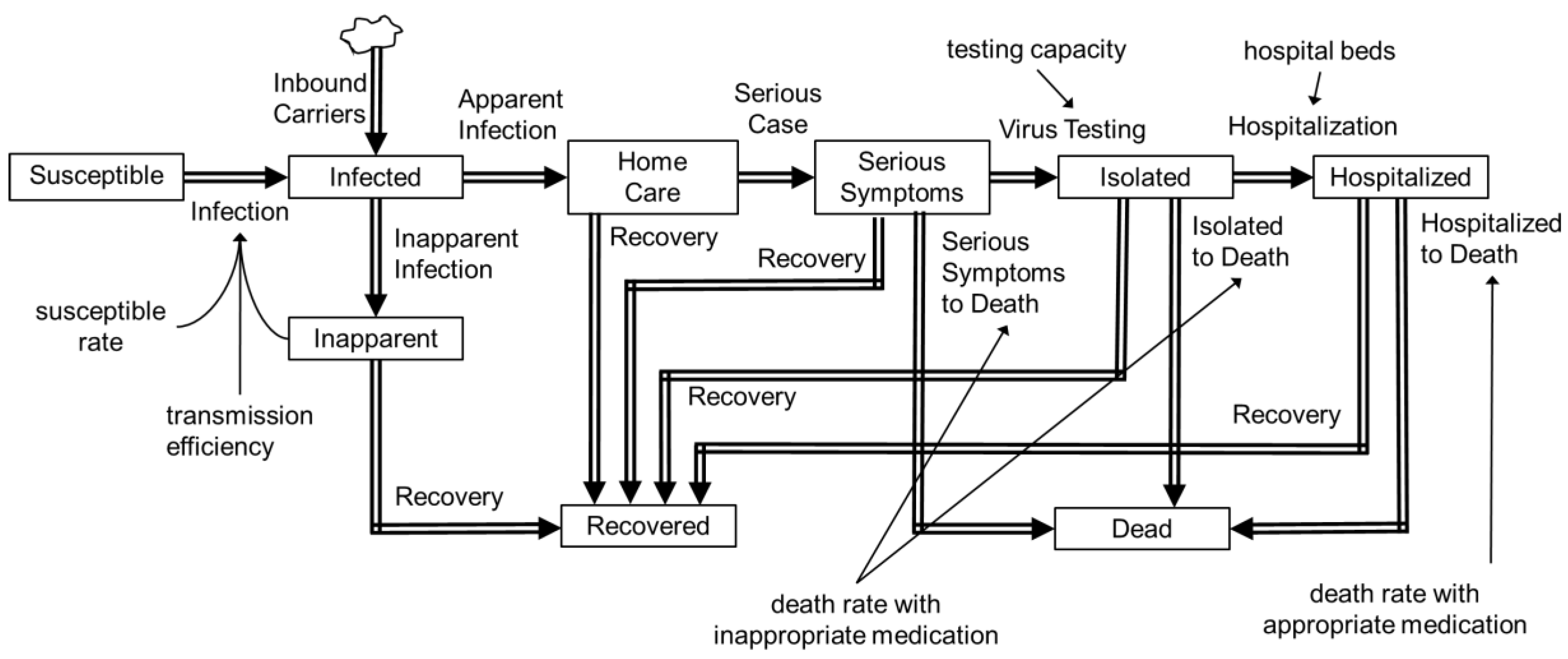
2.5. Stock Flow Model
3. Results
3.1. Causal Loop Analysis of Medical Systems
3.2. Quantitative Analysis by Stock-Flow Analysis
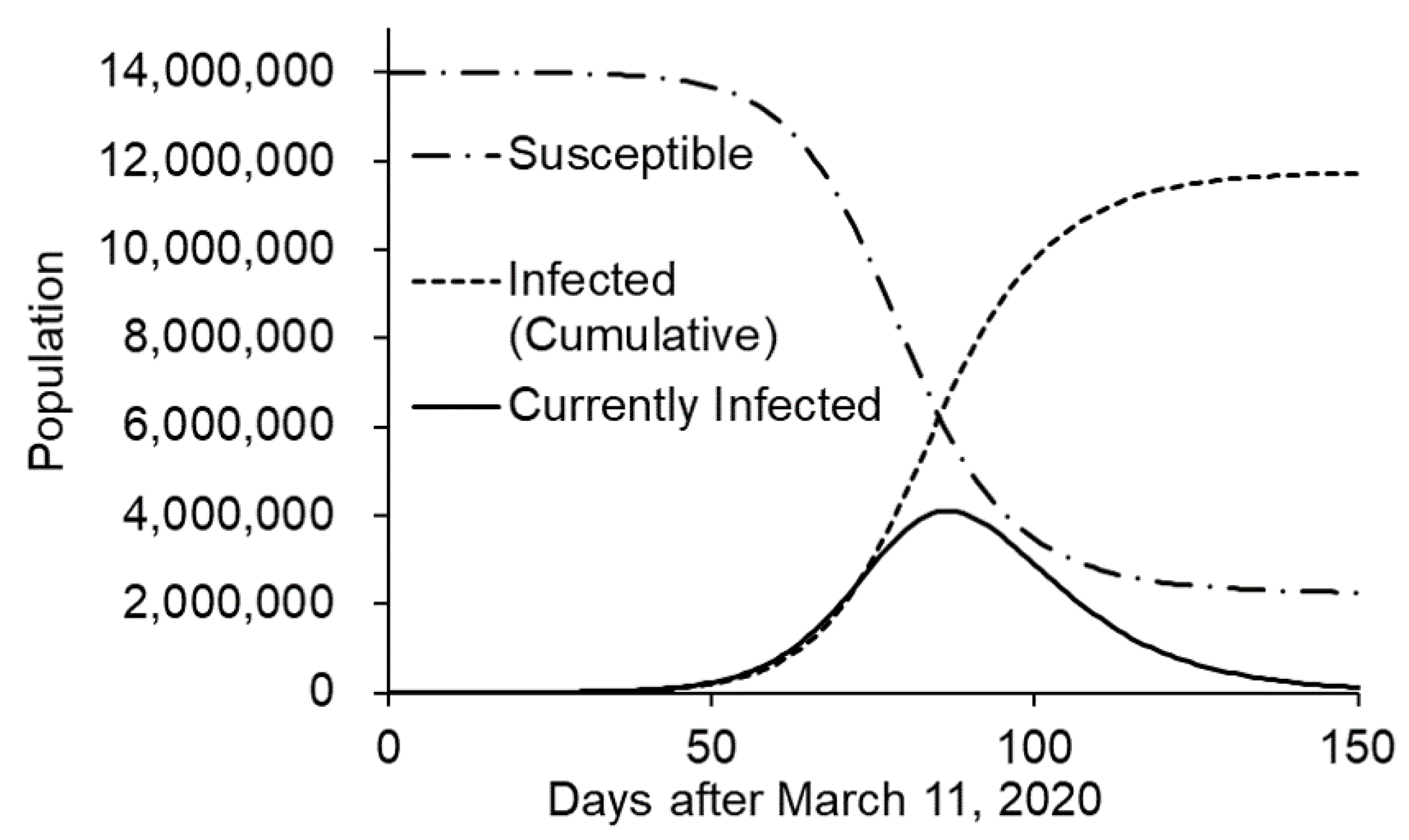
3.2.1. Prediction of Transmission without Intervention
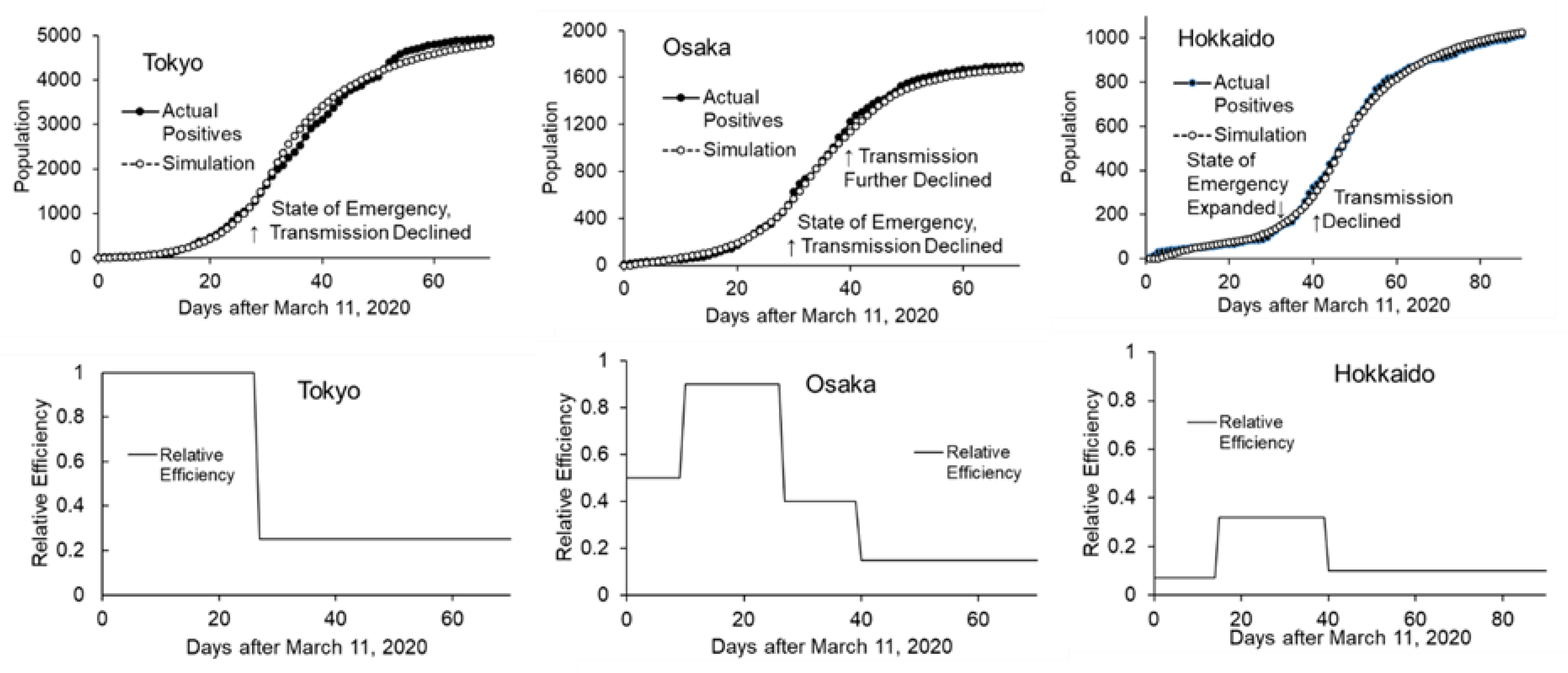
3.2.2. Effects of Interventions on Transmission Efficiency
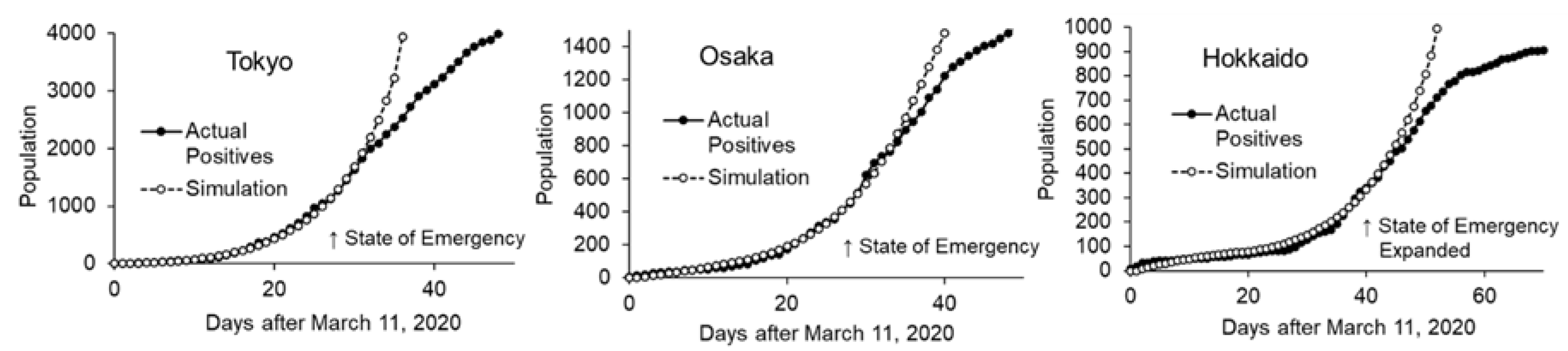
3.3. Simulation Using Stock-Flow Model
3.3.1. Quarantine at Airports
3.3.2. Effect of Timeliness of the State of Emergency
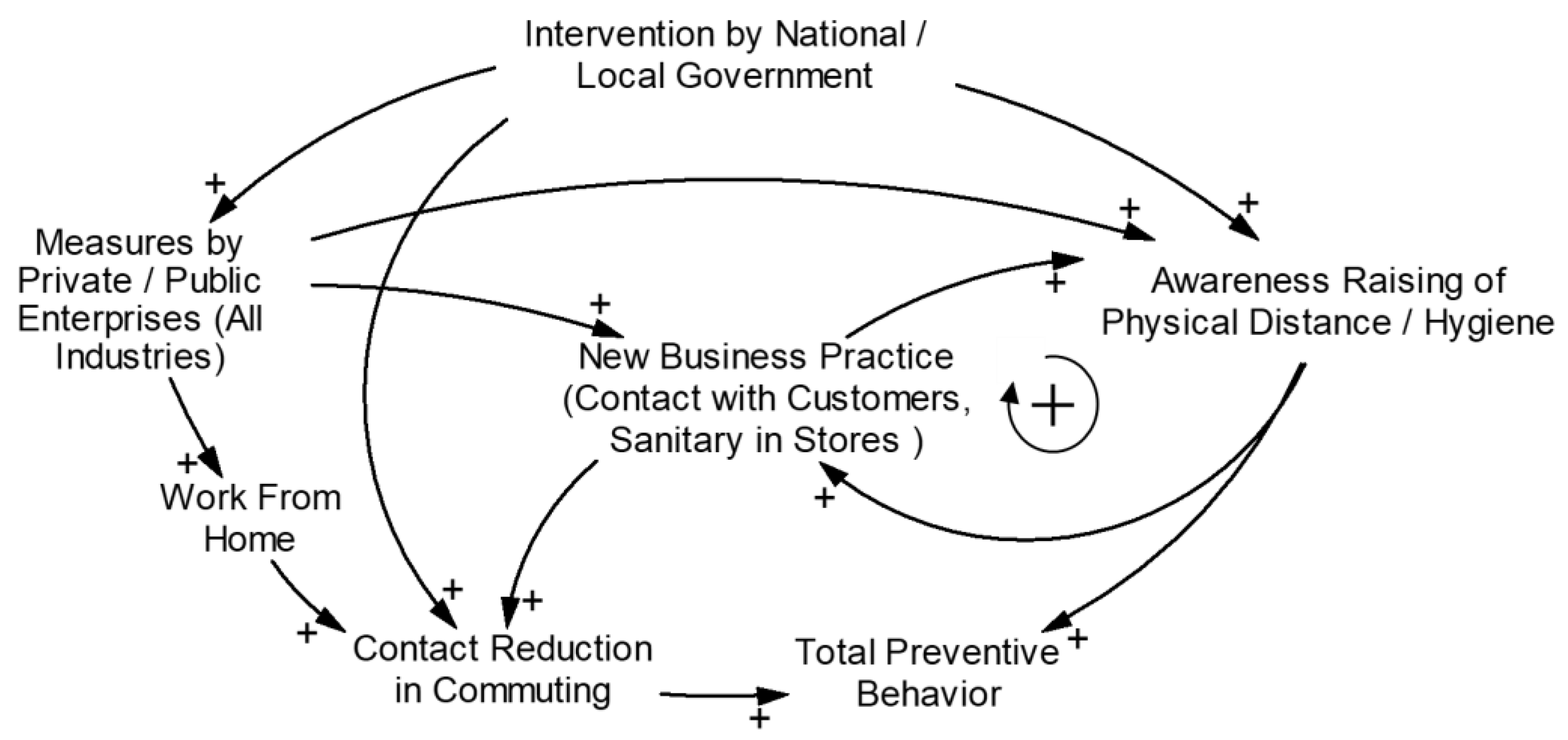
3.4. Effects of Societal Factors
3.5. Causal Loop Diagram for Societal Factors
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Yan, Y.; Shin, W.I.; Pang, Y.X.; Meng, Y.; Lai, J.; You, C.; Zhao, H.; Lester, E.; Wu, T.; Pang, C.H. The first 75 days of Novel Coronavirus (SARS-CoV-2) outbreak: Recent advances, prevention, and treatment. Int. J. Environ. Res. Public Health 2020, 17, 2323. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cilenti, D.; Issel, M.; Wells, R.; Link, S.; Lich, K.H. System dynamics approaches and collective action for community health: And integrative review. Am. J. Community Psycol. 2019, 63, 527–545. [Google Scholar] [CrossRef] [PubMed]
- Batchelder, A.W.; Gonzalez, J.S.; Palma, A.; Schoenbaum, E.; Lounsbury, D.W. A social ecological model of syndemic risk affecting women with and at-risk for HIV in impoverished urban communities. Am. J. Community Psycol. 2015, 56, 220–240. [Google Scholar] [CrossRef] [PubMed]
- Weeks, M.R.; Li, J.; Lounsbury, D.; Green, H.D.; Abbott, M.; Berman, M.; Rohena, L.; Gonzalez, R.; Lang, S.; Mosher, H. Using participatory system dynamics modeling to examine the local HIV test and treatment care continuum in order to reduce community viral load. Am. J. Community Psycol. 2017, 60, 584–598. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.-J.; Xue, H.; Liu, S.; Huang, T.T.K.; Wang, Y.C.; Wan, Y. Obesity trend in the United States and economic intervention options to change it: A simulation study linking ecological epidemiology and system dynamics modeling. Public Health 2018, 161, 20–28. [Google Scholar] [CrossRef] [PubMed]
- Horsch, A.; Khoshsima, D. Towards modeling and simulation of integrated social and health care services for elderly. Stud. Health Technol. Inform. 2007, 129, 38–42. [Google Scholar] [PubMed]
- Dickens, B.L.; Koo, J.R.; Wilder-Smith, A.; Cook, A.R. Institutional, not home-based, isolation could contain the COVID-19 outbreak. Lancet 2020, 395, 1541–1542. [Google Scholar] [CrossRef]
- Gerli, A.G.; Centanni, S.; Miozzo, M.; Virchow, J.C.; Sotgiu, G.; Canonica, G.W.; Soriano, J.B. COVID-19 mortality rates in the European Union, Switzerland, and the UK: Effect of timeline, lockdown rigidity, and population density. Minerva Medica 2020. [Google Scholar] [CrossRef]
- Updates on COVID-19 in Tokyo. Available online: https://stopcovid19.metro.tokyo.lg.jp/ (accessed on 14 June 2020). (In Japanese).
- Latest Updates on COVID-19 in Osaka. Available online: https://covid19-osaka.info/ (accessed on 14 June 2020). (In Japanese).
- Hokkaido COVID-19 Information Site. Available online: https://stopcovid19.hokkaido.dev/ (accessed on 14 June 2020). (In Japanese).
- Portal Site of Official Statistics of Japan. Available online: https://www.e-stat.go.jp/ (accessed on 7 June 2020). (In Japanese).
- National Institute of Informatics Mizuno Laboratory. Available online: http://research.nii.ac.jp/~mizuno/ (accessed on 14 June 2020). (In Japanese).
- Maharaj, S.; Kleczkowski, A. Controlling epidemic spread by social distancing: Do it well or not at all. BMC Public Health 2012, 12, 679. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hatchett, R.J.; Mecher, C.E.; Lipsitch, M. Public health interventions and epidemic intensity during the 1918 influenza pandemic. Proc. Natl. Acad. Sci. USA 2007, 104, 7582–7587. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hattori, Y.; Okajima, Y.; Kanki, N.; Fujimoto, M.; Imagawa, T.; Otsuka, H.; Judo, H.; Koh, Y.; Sasaki, M.; Shionoya, G.; et al. An Urgent Survey of Japanese Companies’ Organizational Responses to COVID-19; A First Report. IIR Working Paper WP#20-10. Available online: http://pubs.iir.hit-u.ac.jp/admin/ja/pdfs/show/2390 (accessed on 7 June 2020). (In Japanese).
- Yuki, K.; Fujiogi, M.; Koutsogiannaki, S. COVID-19 pathophysiology: A review. Clin. Immunol. 2020, 215, 108427. [Google Scholar] [CrossRef] [PubMed]
- COVID-19: Guide on Home-Based Care, Screening & Isolation Ward Set up (April 2020). Available online: https://www.un.org/sites/un2.un.org/files/coronavirus_isolationwardguidance.pdf (accessed on 11 May 2020).
- Xie, M.; Chen, Q. Insight into 2019 novel coronavirus—An updated interim review and lessons from SARS-CoV and MERS-CoV. Int. J. Infect. Dis. 2020, 94, 119–124. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health, Labor and Welfare. Available online: https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/0000164708_00001.html (accessed on 7 June 2020). (In Japanese).
- Rocklöv, J.; Sjödin, H. High population densities catalyse the spread of COVID-19. J. Travel. Med. 2020, 27, taaa038. [Google Scholar] [CrossRef] [PubMed]
- Hattori, Y.; Okajima, Y.; Kanki, N.; Fujimoto, M.; Imagawa, T.; Otsuka, H.; Judo, H.; Koh, Y.; Sasaki, M.; Shionoya, G.; et al. An Urgent Survey of Japanese Companies’ Organizational Responses to COVID-19; A Second Report. IIR Working Paper WP#20-11. Available online: http://pubs.iir.hit-u.ac.jp/admin/ja/pdfs/show/2391 (accessed on 14 June 2020). (In Japanese).
- Moghadas, S.M.; Shoukat, A.; Fitzpatrik, M.C.; Wells, C.R.; Sah, P.; Pandey, A.; Sachs, J.D.; Wang, Z.; Meyers, L.A.; Singer, B.H.; et al. Projecting hospital utilization during the COVID-19 outbreaks in the United States. Proc. Natl. Acad. Sci. USA 2020, 117, 9122–9126. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Current Hospital Capacity Estimates—Snapshot. Available online: https://www.cdc.gov/nhsn/covid19/report-patient-impact.html (accessed on 11 May 2020).
- Halpern, N.A.; Tan, K.S. U.S. ICU Resource Availability for COVID-19. Available online: https://www.sccm.org/getattachment/Blog/March-2020/United-States-Resource-Availability-for-COVID-19/United-States-Resource-Availability-for-COVID-19.pdf (accessed on 11 May 2020).
- Running out of Beds and Gear, Tokyo Medical Staff say Japan’s ‘State of Emergency’ Already Here. Available online: https://www.japantimes.co.jp/news/2020/04/07/national/science-health/hospital-beds-gear-coronavirus/#.XrlM325uI5U (accessed on 11 May 2020).
- Japan Broadcasting Corporation. Available online: https://www3.nhk.or.jp/news/special/coronavirus/medical/ (accessed on 11 May 2020). (In Japanese).
- Ministry of Health, Labor and Welfare. Available online: https://www.mhlw.go.jp/content/10900000/000633020.pdf (accessed on 10 August 2020). (In Japanese).
- Basic Policies for Novel Coronavirus Disease Control (Revised on 7 April 2020). Available online: https://corona.go.jp/en/news/pdf/COVID19April7BasicAPolicies.pdf (accessed on 16 June 2020).
- Rubin, D.; Huang, J.; Fisher, B.T.; Gasparrini, A.G.; Tam, V.T.; Song, L.; Wang, X.; Kaufman, J.; Fitzpatrick, K.; Jain, A.; et al. Association of social distancing, population density, and temperature with the instantaneous reproduction number of SARS-CoV-2 in counties across the United States. JAMA Network Open 2020, 3, e2016099. [Google Scholar] [CrossRef] [PubMed]
| Parameters | Value | Basis |
|---|---|---|
| Susceptible People | Start with 14,000,000 (Tokyo), 8,800,000 (Osaka), and 5,300,000 (Hokkaido) | Whole population, 1 October 2019 [12] |
| Incubation period | 5 days | From the literature [17] |
| Inbound virus carrier | 8 (Tokyo), 5 (Osaka), and 3 (Hokkaido) daily before 3 April 2020 | All foreign arrivals multiplied by assumed positive rate (0.003) were divided in proportion to the population |
| Baseline positives per day before epidemic | 5 (Tokyo), 7 (Osaka), and 7 (Hokkaido) | Assumed from average from 11 March 2020 to 15 March 2020 |
| Initial value, incubation period, related to inbound | 24 (Tokyo), 15 (Osaka), and 9 (Hokkaido) | Inbound carrier assuming 3 days of incubation period remaining |
| Initial value, incubation period, domestic | 125 (Tokyo), 175 (Osaka), and 175 (Hokkaido) | Baseline positives divided by serious symptoms rate (0.2) and multiplied by incubation days (5) |
| Initial value, mild symptoms | 140 (Tokyo), 175 (Osaka), and 175 (Hokkaido) | Baseline positives divided by serious symptoms rate (0.2), multiplied by recovery days (14) and inapparent rate (0.4) |
| Initial value, moderate or developing symptoms | 30 (Tokyo), 42 (Osaka), and 42 (Hokkaido) | Baseline positives divided by serious symptoms rate (0.2), multiplied by development days (2) and apparent rate (0.6) |
| Initial value, serious symptoms | 5 (Tokyo), 7 (Osaka), and 7 (Hokkaido) | Baseline positives multiplied by assumed diagnosis day 1 |
| Days to be isolated | 14 days | From the literature [18] |
| Time to disease development from initial symptoms | 2 days | From the literature [18] |
| Recovery time | 14 days | From the literature [19] |
| Ratio: Serious symptoms/All symptoms | 20% | From the literature [18] |
| Ratio: Mild symptoms/All symptoms | 40% | From the literature [18] |
| Diagnosis (polymeric chain reaction virus test) efficiency | 500 (Tokyo), 110 (Osaka), and 100 (Hokkaido) subjects per day | Peak test numbers collected from MHLW website [20] |
| Hospital beds | 2000 (Tokyo), 1100 (Osaka), and 500 (Hokkaido) | Survey by the Ministry of Health, Labor and Welfare on 1 May 2020 [20] |
| Infection per day per virus carrier | 0.25 | Reproduction number 3.3 was divided by average exposure by carrier (5 days incubation and 60% probability for 14 days inapparent infection results in 13.4 days) |
| Tokyo | Osaka | Hokkaido | |
|---|---|---|---|
| Disease Transmission Parameters | |||
| Baseline relative transmission efficiency | 1.00 | 0.90 | 0.32 |
| Maximum intervention Effect | 0.75 | 0.83 | 0.69 |
| Intervention effect before holiday season | 0.75 | 0.40 | 0.32 |
| Demographics | |||
| Total Population *1 | 1.39 × 107 | 8.81 × 106 | 5.25 × 106 |
| Population density in densely inhabited district *2 | 1.23 × 104 | 9.32 × 103 | 5.09 × 103 |
| Proportion of population in densely inhabited district *2 | 0.984 | 0.957 | 0.752 |
| Behavior-related data | |||
| Maximum Reduction in Outings *3 | 0.56 | 0.46 | 0.34 |
| Maximum Reduction in Outings before holiday season *3 | 0.55 | 0.43 | 0.29 |
| Worker population | 7.44 × 106 | 4.71 × 106 | 2.66 × 106 |
| Located companies | 2.02 × 105 | 1.05 × 105 | 6.97 × 104 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Niwa, M.; Hara, Y.; Sengoku, S.; Kodama, K. Effectiveness of Social Measures against COVID-19 Outbreaks in Selected Japanese Regions Analyzed by System Dynamic Modeling. Int. J. Environ. Res. Public Health 2020, 17, 6238. https://doi.org/10.3390/ijerph17176238
Niwa M, Hara Y, Sengoku S, Kodama K. Effectiveness of Social Measures against COVID-19 Outbreaks in Selected Japanese Regions Analyzed by System Dynamic Modeling. International Journal of Environmental Research and Public Health. 2020; 17(17):6238. https://doi.org/10.3390/ijerph17176238
Chicago/Turabian StyleNiwa, Makoto, Yasushi Hara, Shintaro Sengoku, and Kota Kodama. 2020. "Effectiveness of Social Measures against COVID-19 Outbreaks in Selected Japanese Regions Analyzed by System Dynamic Modeling" International Journal of Environmental Research and Public Health 17, no. 17: 6238. https://doi.org/10.3390/ijerph17176238








