Adaptation and Integration of Psychosocial Stimulation, Maternal Mental Health and Nutritional Interventions for Pregnant and Lactating Women in Rural Bangladesh
Abstract
Key Messages
- Extending the scope of early child development intervention by including pregnancy and the post-childbirth periods, as well as maternal mental health is feasible in a low-resource setting;
- Development of such an integrated intervention requires a systematic process for the adaptation and feasibility testing;
- The three adaptation phases: situation analysis, intervention pilot, and identification of facilitators and barriers through participant feedback allow for productive curriculum revision;
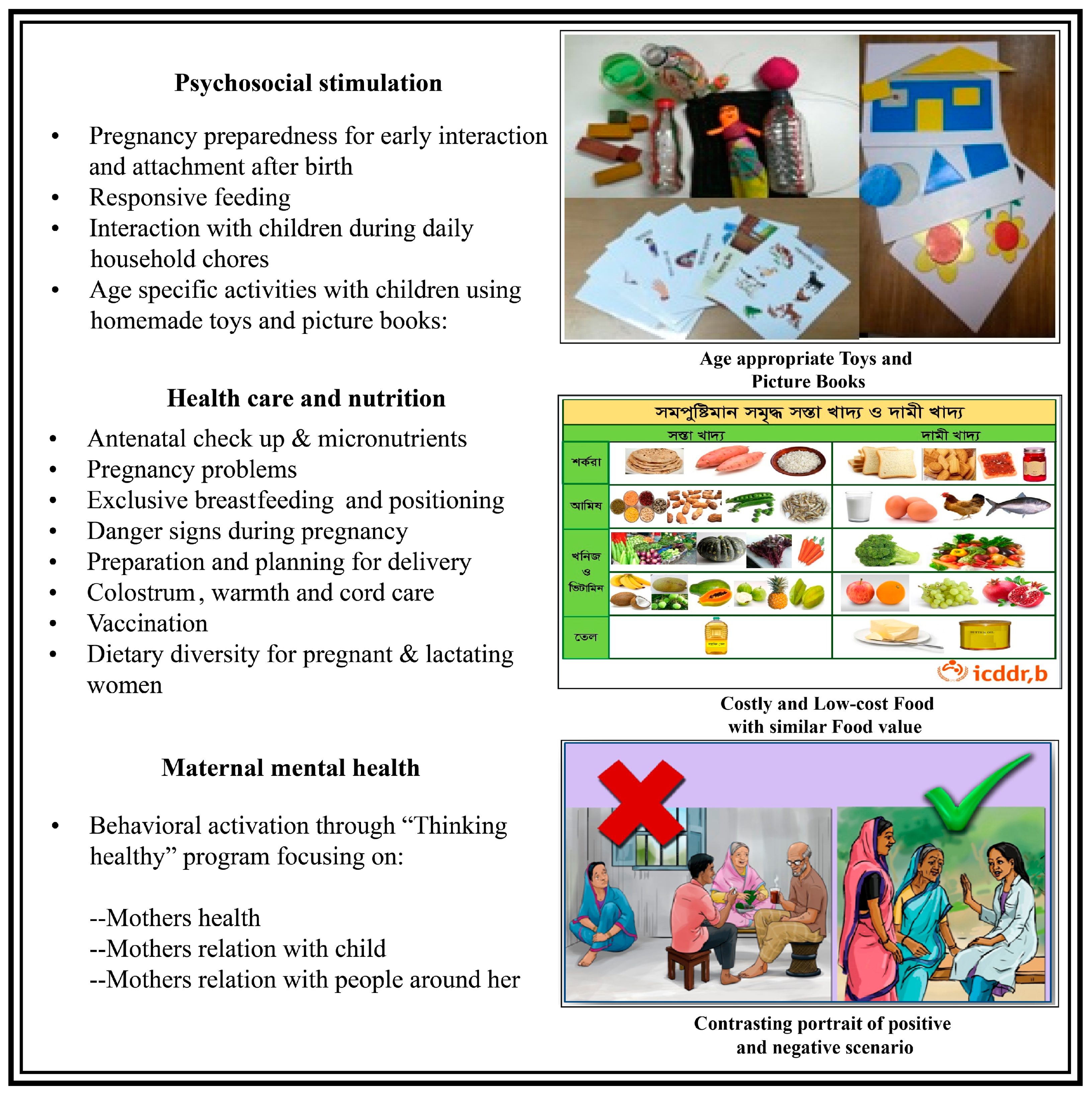
- Inclusion of a greater number of visual cues, interactive role-play activities, simplified mental health contents, motivational meetings with family members, and tailoring of intervention contents to the age groups present improved intervention acceptability and ease of delivery;
- A structured adaptation process may allow for rapid development of a feasible intervention in a new population.
1. Background
2. Methods
2.1. Study Site and Design
2.2. Adaptation Phases of Integrated Intervention
2.2.1. Phase 1—Identify Core Components and Structure of Intervention
2.2.2. Phase 2—Pilot Initial Revisions of Intervention
2.2.3. Phase 3—Identify Feedback from Participants and CHWs
2.3. Ethical Approval
2.4. Data Analysis
3. Results
3.1. Phase 1: Identified Intervention Components and Structure
3.2. Phase 2: Feasibility of Implementing the Initial Revision of Intervention (Pilot Trial)
3.3. Phase 3: Participants’ Feedback after Intervention and Final Revision
3.4. Intervention Content
Before attending the session, I used to give toys to my baby, and she played alone… Now I have learned from the session… I followed this, and I have observed the benefit. Now my 5 month old daughter can make noise, pay attention to my sounds, and look at me when I call her by name (IDI-5).
I cannot eat between the afternoon (Asar) and evening (Maghrib) prayers, as my 27-day-old child died last year during this time period. People say that my dead son won’t get food if I take food during that time. So I will maintain this until my death (IDI-3).
Mothers can’t understand the thinking healthy story appropriately by the pictures only. It is difficult for us also (KII-1).
More visual things will help us to understand more. Videos are very helpful to memorize. Drama will be interesting (IDI-4).
3.5. Intervention Delivery and Participation
Some pregnant women felt uneasy to sit on the bed or floor. So, they sat on the chair. They also cannot sit for long. Then I allowed them to move for a while (KII-1).
Sometimes they didn’t want to share some feminine problems like danger signs if someone else was present in the session (KII-1).
It was hard to make them understand about the thinking healthy component and to identify their unhealthy thoughts. Who want to reveal own unproductive behavior in front of others? (KII-2)
If I could not finish my work, and the session is about to begin, my mother-in-law does the remaining work and let me go for the session (IDI-6).
3.6. Final Adaptation of Integrated Intervention
4. Discussion
5. Conclusions and Recommendations
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Lu, C.; Black, M.M.; Richter, L.M. Risk of poor development in young children in low-income and middle-income countries: An estimation and analysis at the global, regional, and country level. Lancet Glob. Health 2016, 4, e916–e922. [Google Scholar] [CrossRef]
- Black, M.M.; Walker, S.P.; Fernald, L.C.; Andersen, C.T.; DiGirolamo, A.M.; Lu, C.; McCoy, D.C.; Fink, G.; Shawar, Y.R.; Shiffman, J.; et al. Early childhood development coming of age: Science through the life course. Lancet 2017, 389, 77–90. [Google Scholar] [CrossRef]
- Jensen, S.K.; Tofail, F.; Haque, R.; Petri, W.A., Jr.; Nelson, C.A., III. Child development in the context of biological and psychosocial hazards among poor families in Bangladesh. PLoS ONE 2019, 14, e0215304. [Google Scholar] [CrossRef]
- Grantham-McGregor, S.; Cheung, Y.B.; Cueto, S.; Glewwe, P.; Richter, L.; Strupp, B.; International Child Development Steering Group. Developmental potential in the first 5 years for children in developing countries. Lancet 2007, 369, 60–70. [Google Scholar] [CrossRef]
- Lake, A.; Chan, M. Putting science into practice for early child development. Lancet 2015, 385, 1816–1817. [Google Scholar] [CrossRef]
- Borge, T.C.; Aase, H.; Brantsæter, A.L.; Biele, G. The importance of maternal diet quality during pregnancy on cognitive and behavioural outcomes in children: A systematic review and meta-analysis. BMJ Open 2017, 7, e016777. [Google Scholar] [CrossRef] [PubMed]
- Gelaye, B.; Rondon, M.B.; Araya, R.; Williams, M.A. Epidemiology of maternal depression, risk factors, and child outcomes in low-income and middle-income countries. Lancet Psychiatry 2016, 3, 973–982. [Google Scholar] [CrossRef]
- Lebel, C.; Walton, M.; Letourneau, N.; Giesbrecht, G.F.; Kaplan, B.J.; Dewey, D. Prepartum and postpartum maternal depressive symptoms are related to children’s brain structure in preschool. Biol. Psychiatry 2016, 80, 859–868. [Google Scholar] [CrossRef] [PubMed]
- Sandman, C.A.; Buss, C.; Head, K.; Davis, E.P. Fetal exposure to maternal depressive symptoms is associated with cortical thickness in late childhood. Biol. Psychiatry 2015, 77, 324–334. [Google Scholar] [CrossRef] [PubMed]
- MacLean, P.C.; Rynes, K.N.; Aragón, C.; Caprihan, A.; Phillips, J.P.; Lowe, J.R. Mother-Infant mutual eye gaze supports emotion regulation in infancy during the still-face paradigm. Infant Behav. Dev. 2014, 37, 512–522. [Google Scholar] [CrossRef]
- Magill-Evans, J.; Harrison, M.J.; Burke, S.O. Parent-Child interactions and development of toddlers born preterm. West. J. Nurs. Res. 1999, 21, 292–312. [Google Scholar] [CrossRef] [PubMed]
- Negayama, K.; Delafield-Butt, J.T.; Momose, K.; Ishijima, K.; Kawahara, N.; Lux, E.J.; Murphy, A.; Kaliarntas, K. Embodied intersubjective engagement in mother–infant tactile communication: A cross-cultural study of Japanese and Scottish mother-infant behaviors during infant pick-up. Front. Psychol. 2015, 6, 66. [Google Scholar] [CrossRef] [PubMed]
- Shannon, J.D.; Tamis-LeMonda, C.S.; London, K.; Cabrera, N. Beyond rough and tumble: Low-Income fathers’ interactions and children’s cognitive development at 24 months. Parent. Sci. Pract. 2002, 2, 77–104. [Google Scholar] [CrossRef]
- Slomian, J.; Honvo, G.; Emonts, P.; Reginster, J.Y.; Bruyère, O. Consequences of maternal postpartum depression: A systematic review of maternal and infant outcomes. Women’s Health 2019, 15, 1745506519844044. [Google Scholar] [CrossRef] [PubMed]
- Aboud, F.E.; Yousafzai, A.K. Global health and development in early childhood. Annu. Rev. Psychol. 2015, 66, 433–457. [Google Scholar] [CrossRef]
- Jeong, J.; Pitchik, H.O.; Yousafzai, A.K. Stimulation interventions and parenting in low-and middle-income countries: A meta-analysis. Pediatrics 2018, 141, e20173510. [Google Scholar] [CrossRef]
- Sharma, R.; Gaffey, M.F.; Alderman, H.; Bassani, D.G.; Bogard, K.; Darmstadt, G.L.; Das, J.K.; de Graft-Johnson, J.E.; Hamadani, J.D.; Horton, S.; et al. Prioritizing research for integrated implementation of early childhood development and maternal, newborn, child and adolescent health and nutrition platforms. J. Glob. Health 2017, 7, 011002. [Google Scholar] [CrossRef]
- Hamadani, J.D.; Huda, S.N.; Khatun, F.; Grantham-McGregor, S.M. Psychosocial stimulation improves the development of undernourished children in rural Bangladesh. J. Nutr. 2006, 136, 2645–2652. [Google Scholar] [CrossRef]
- Nahar, B.; Hamadani, J.D.; Ahmed, T.; Tofail, F.; Rahman, A.; Huda, S.N.; Grantham-McGregor, S.M. Effects of psychosocial stimulation on growth and development of severely malnourished children in a nutrition unit in Bangladesh. Eur. J. Clin. Nutr. 2009, 63, 725–731. [Google Scholar] [CrossRef] [PubMed]
- Tofail, F.; Hamadani, J.D.; Mehrin, F.; Ridout, D.A.; Huda, S.N.; Grantham-McGregor, S.M. Psychosocial stimulation benefits development in nonanemic children but not in anemic, iron-deficient children. J. Nutr. 2013, 143, 885–893. [Google Scholar] [CrossRef]
- Hamadani, J.D.; Mehrin, S.F.; Tofail, F.; Hasan, M.I.; Huda, S.N.; Baker-Henningham, H.; Ridout, D.; Grantham-McGregor, S. Integrating an early childhood development programme into Bangladeshi primary health-care services: An open-label, cluster-randomised controlled trial. Lancet Glob. Health 2019, 7, e366–e375. [Google Scholar] [CrossRef]
- Aarons, G.A.; Green, A.E.; Palinkas, L.A.; Self-Brown, S.; Whitaker, D.J.; Lutzker, J.R.; Silovsky, J.F.; Hecht, D.B.; Chaffin, M.J. Dynamic adaptation process to implement an evidence-based child maltreatment intervention. Implement. Sci. 2012, 7, 32. [Google Scholar] [CrossRef] [PubMed]
- Cabassa, L.J.; Gomes, A.P.; Meyreles, Q.; Capitelli, L.; Younge, R.; Dragatsi, D.; Alvarez, J.; Manrique, Y.; Lewis-Fernández, R. Using the collaborative intervention planning framework to adapt a health-care manager intervention to a new population and provider group to improve the health of people with serious mental illness. Implement. Sci. 2014, 9, 178. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, N.E.; Kemp, K.A.; Leff, S.S.; Lochman, J.E. Guidelines for adapting manualized interventions for new target populations: A step-wise approach using anger management as a model. Clin. Psychol. Sci. Pract. 2012, 19, 385–401. [Google Scholar] [CrossRef]
- Grantham-McGregor, S.; Smith, J.A. Extending the Jamaican early childhood development intervention. J. Appl. Res. Child. Inf. Policy Child. Risk 2016, 7, 4. [Google Scholar]
- Smith, J.A.; Baker-Henningham, H.; Brentani, A.; Mugweni, R.; Walker, S.P. Implementation of reach up early childhood parenting program: Acceptability, appropriateness, and feasibility in Brazil and Zimbabwe. Ann. NY Acad. Sci. 2018, 1419, 120–140. [Google Scholar] [CrossRef]
- Rahman, A.; Malik, A.; Sikander, S.; Roberts, C.; Creed, F. Cognitive behaviour therapy-based intervention by community health workers for mothers with depression and their infants in rural Pakistan: A cluster-randomised controlled trial. Lancet 2008, 372, 902–909. [Google Scholar] [CrossRef]
- Yesmin, S.; Rahman, N.F.; Khatun, R.; Begum, T.; Tahmid, T.; Afrin, S.; Hamadani, J.D. Community based psychosocial intervention in reducing maternal depression and improving infant’s development in Bangladesh: A randomized control trial. IOSR J. Nurs. Health Sci. 2016, 5, 11–20. [Google Scholar]
- DGHS. Competency based training module on antenatal and postnatal care—Trainers’ module. Dhaka: Directorate General of Health Services (DGHS), and Obstetrical and Gynecological Society of Bangladesh (OGSB). Personal communication, 2017. [Google Scholar]
- Jannat, K.; Luby, S.P.; Unicomb, L.; Rahman, M.; Winch, P.J.; Parvez, S.M.; Das, K.K.; Leontsini, E.; Ram, P.K.; Stewart, C.P. Complementary feeding practices among rural Bangladeshi mothers: Results from WASH Benefits study. Matern. Child Nutr. 2019, 15, e12654. [Google Scholar] [CrossRef]
- Lee, J.; Lee, H.; Kim, S.; Choi, M.; Ko, I.S.; Bae, J.; Kim, S.H. Debriefing methods and learning outcomes in simulation nursing education: A systematic review and meta-analysis. Nurse Educ. Today 2020, 87, 104345. [Google Scholar] [CrossRef]
- McMahon, S.A.; Winch, P.J. Systematic debriefing after qualitative encounters: An essential analysis step in applied qualitative research. BMJ Glob. Health 2018, 3, e000837. [Google Scholar] [CrossRef] [PubMed]
- Cooper, J. Using Peer Debriefing in the Final Stage of Evaluation with Implications for Qualitative Research: Three Impressionist Tales. Annual Meeting of the American Educational Research Association 1997. Available online: https://eric.ed.gov/?id=ED410287 (accessed on 21 August 2020).
- Carroll, K.M.; Nuro, K.F. One size cannot fit all: A stage model for psychotherapy manual development. Clin. Psychol. Sci. Pract. 2002, 9, 396–406. [Google Scholar] [CrossRef]
- Goldstein, N.E.; Serico, J.M.; Romaine, C.L.R.; Zelechoski, A.D.; Kalbeitzer, R.; Kemp, K.; Lane, C. Development of the juvenile justice anger management treatment for girls. Cogn. Behav. Pract. 2013, 20, 171–188. [Google Scholar] [CrossRef] [PubMed]
- Willis, A.; Perle, J.G.; Schnur, L. Prolonged exposure in the treatment of PTSD following an apartment fire. Clin. Case Stud. 2015, 14, 449–465. [Google Scholar] [CrossRef]
- Pitchik, H.O.; Tofail, F.; Rahman, M.; Akter, F.; Sultana, J.; Shoab, A.K.; Huda, T.M.N.; Jahir, T.; Amin, M.R.; Hossain, M.K.; et al. Addressing risk factors for poor early child development: A randomized controlled trial of an integrated group-based responsive care giving, nutrition, sanitation, and mental health intervention. Manuscript in preparation.
| Study Phases | Goldstein et al.’s Manual Adaptation Process | Adaptation Stages of the Integrated Intervention in Parallel with the Process Developed by Goldstein et al. |
|---|---|---|
| Phase 1: Identify core components and structure of intervention | Stage-1: Choose a base manual for adaptation | The Reach-up curriculum for psychosocial stimulation was revised: contents for pregnancy and 0–5-month-old children were added. |
| Stage-2: Conduct a focus group with the new target population | Two small group discussions with nine pregnant women and nine lactating mothers were used to identify the core contents of the intervention. | |
| Stage-3: Make initial manual revisions | The integrated components of the intervention curriculum were revised based on the results of two small group discussions. | |
| Phase 2: Pilot initial revision of intervention | Stage-4: Pilot initial revisions of the manualized intervention | The adapted intervention package was piloted with 11 pregnant women and 29 mothers of children <24 months of age with two different delivery strategies. |
| Phase 3: Identify feedback from participants’ and CHWs | Stage-5: Conduct facilitator focus group | Interviews were conducted with the two facilitators and eight participants to identify areas for modification. |
| Stage-6: Acquire expert review of the revised manual | The qualitative data from the pilot were systematically analyzed and reviewed by child development specialists to identify the barriers and facilitators of intervention delivery and uptake. | |
| Stage-7: Incorporate staff and expert feedback | The curriculum was revised incorporating feedback from the facilitators, participants, and child development specialists. |
| Major Theme | Pregnant Women | Lactating Mothers |
|---|---|---|
| General perception of factors affecting early childhood development |
|
|
| Interaction with children |
|
|
| Maternal mental health |
|
|
| Pregnancy problems |
| NA |
| Negative thinking/Alternative beliefs |
| NA |
| Characteristics (n = 36) | n (%) |
|---|---|
| Types of participants | |
| Pregnant women | 9 (25) |
| Mothers of children <2 years old | 27 (75) |
| Mother’s education | |
| Below primary or no formal education | 6 (16.7) |
| Primary education | 26 (72.2) |
| Secondary education | 4 (11.1) |
| Father’s education | |
| Below primary or no formal education | 13 (36.1) |
| Primary education | 17 (47.2) |
| Secondary education | 6 (16.7) |
| Participants’ occupation | |
| Housewife | 36 (100) |
| Husbands’ occupation | |
| Irregular income (e.g., day labor, farming) | 18 (50) |
| Salaried work (e.g., government or private job with fixed monthly salary) | 6 (16.7) |
| Other (e.g., shopkeeper, retired, living abroad) | 12 (33.3) |
| Monthly Income | |
| <8000 BDT (<94 USD) | 4 (11.1) |
| 8000–20,000 BDT (94–235 USD) | 29 (80.6) |
| >20,000 BDT (>235 USD) | 3 (8.3) |
| Housing construction (Wall material) | |
| Cement | 7 (19.4) |
| Corrugated iron sheets | 28 (77.8) |
| Mud | 1 (2.8) |
| Study Activities | Challenges | Mitigation Strategies |
|---|---|---|
| Initial curriculum development |
|
|
| Selection and training of CHWs |
|
|
|
| |
|
| |
| Pilot intervention |
|
|
|
| |
|
| |
|
|
| Respondents Code | Type of Respondents | Age (Years) | Last Completed Grade in School | Occupation | Monthly Household Income (BDT) |
|---|---|---|---|---|---|
| IDI-1 | Pregnant woman (2nd trimester) | 20 | Grade 8 | Housewife | 6000/= |
| IDI-2 | Lactating mother (8-month old child) | 30 | Grade 2 | Housewife | 5000/= |
| IDI-3 | Pregnant woman (3rd trimester) | 22 | Grade 5 | Housewife | 6000/= |
| IDI-4 | Lactating mother (6-month old child) | 20 | Grade-5 | Housewife | 20,000/= |
| IDI-5 | Lactating mother (5-month old child) | 24 | Grade 6 | Housewife | 6500/= |
| IDI-6 | Lactating mother (7-month old child) | 20 | Grade 7 | Housewife | 25,000/= |
| IDI-7 | Pregnant woman (2nd trimester) | 26 | Grade 10 | Housewife | 6000/= |
| IDI-8 | Pregnant woman (2nd trimester) | 30 | Grade 6 | Housewife | 15,000/= |
| KII-1 | CHW | 25 | Higher secondary level | Bachelor’s degree student | ------- |
| KII-2 | CHW | 18 | Secondary level | Higher secondary school student | -------- |
| Theme | Sub-Theme | Core Findings |
|---|---|---|
| Intervention content | ||
| Facilitators to intervention success |
| |
| Obstacles to practice recommended behavior |
| |
| Suggestions for revision |
| |
| Intervention strategy and participation | ||
| Facilitators to intervention success |
| |
| Obstacles to session delivery and participation |
| |
| Suggestion for revision |
|
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Akter, F.; Rahman, M.; Pitchik, H.O.; Winch, P.J.; Fernald, L.C.H.; Nurul Huda, T.M.; Jahir, T.; Amin, R.; Das, J.B.; Hossain, K.; et al. Adaptation and Integration of Psychosocial Stimulation, Maternal Mental Health and Nutritional Interventions for Pregnant and Lactating Women in Rural Bangladesh. Int. J. Environ. Res. Public Health 2020, 17, 6233. https://doi.org/10.3390/ijerph17176233
Akter F, Rahman M, Pitchik HO, Winch PJ, Fernald LCH, Nurul Huda TM, Jahir T, Amin R, Das JB, Hossain K, et al. Adaptation and Integration of Psychosocial Stimulation, Maternal Mental Health and Nutritional Interventions for Pregnant and Lactating Women in Rural Bangladesh. International Journal of Environmental Research and Public Health. 2020; 17(17):6233. https://doi.org/10.3390/ijerph17176233
Chicago/Turabian StyleAkter, Fahmida, Mahbubur Rahman, Helen O. Pitchik, Peter J. Winch, Lia C. H. Fernald, Tarique Mohammad Nurul Huda, Tania Jahir, Ruhul Amin, Jyoti Bhushan Das, Khobair Hossain, and et al. 2020. "Adaptation and Integration of Psychosocial Stimulation, Maternal Mental Health and Nutritional Interventions for Pregnant and Lactating Women in Rural Bangladesh" International Journal of Environmental Research and Public Health 17, no. 17: 6233. https://doi.org/10.3390/ijerph17176233
APA StyleAkter, F., Rahman, M., Pitchik, H. O., Winch, P. J., Fernald, L. C. H., Nurul Huda, T. M., Jahir, T., Amin, R., Das, J. B., Hossain, K., Shoab, A. K., Khan, R., Yeasmin, F., Sultana, J., Luby, S. P., & Tofail, F. (2020). Adaptation and Integration of Psychosocial Stimulation, Maternal Mental Health and Nutritional Interventions for Pregnant and Lactating Women in Rural Bangladesh. International Journal of Environmental Research and Public Health, 17(17), 6233. https://doi.org/10.3390/ijerph17176233











