Evaluation of the Effectiveness of the Use of the Diode Laser in the Reduction of the Volume of the Edematous Gingival Tissue after Causal Therapy
Abstract
:1. Introduction
2. Materials and Methods
2.1. Sample Composition
2.2. Inclusion Criteria
- Inflammation caused by systemic factors; a typical example is represented by pregnancy or by hormonal upheavals such as puberty or menstruation.
- Phlogistic-hyperplastic alterations in conjunction with the intake of antiepileptics, calcium channel blockers, and cyclosporine.
- Gingivitis caused by the use of oral contraceptives.
- Gingivitis modified by systemic diseases.
- Gingivitis affecting patients with diabetes mellitus.
- Gingivitis associated with disorders of the blood picture (e.g., leukemia).
- Plaque gingivitis modified by malnutrition, such as chronic deficiency of vitamins A, C, and D (although they seem to occur rarely in Europe).
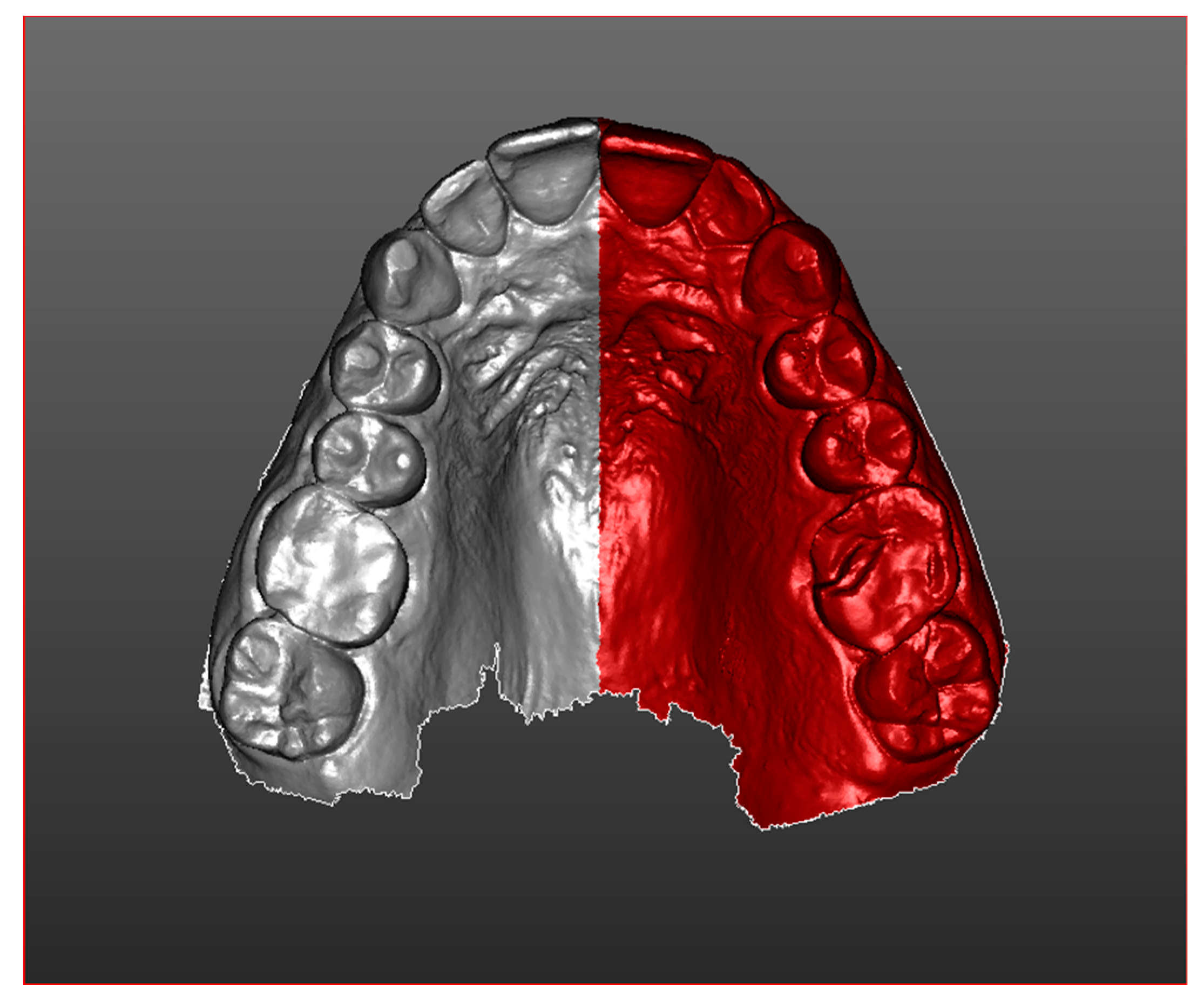
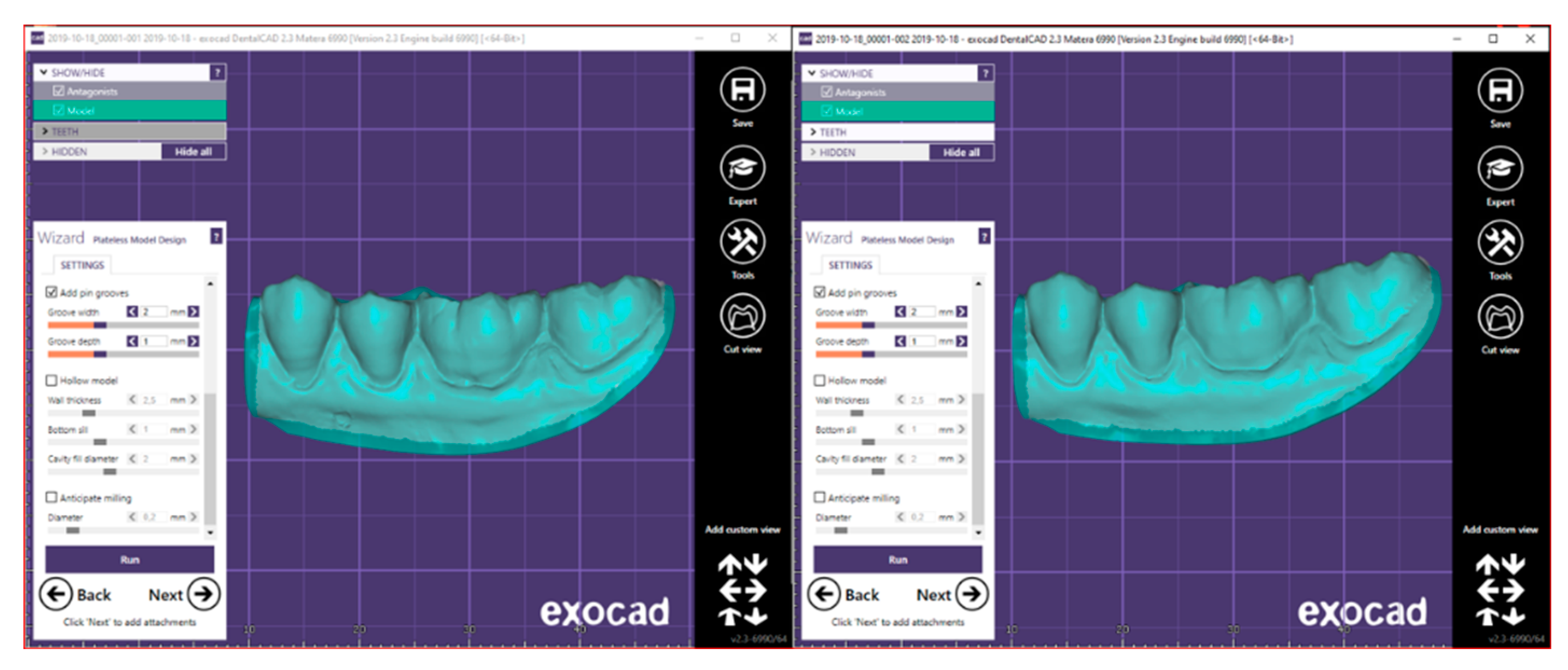
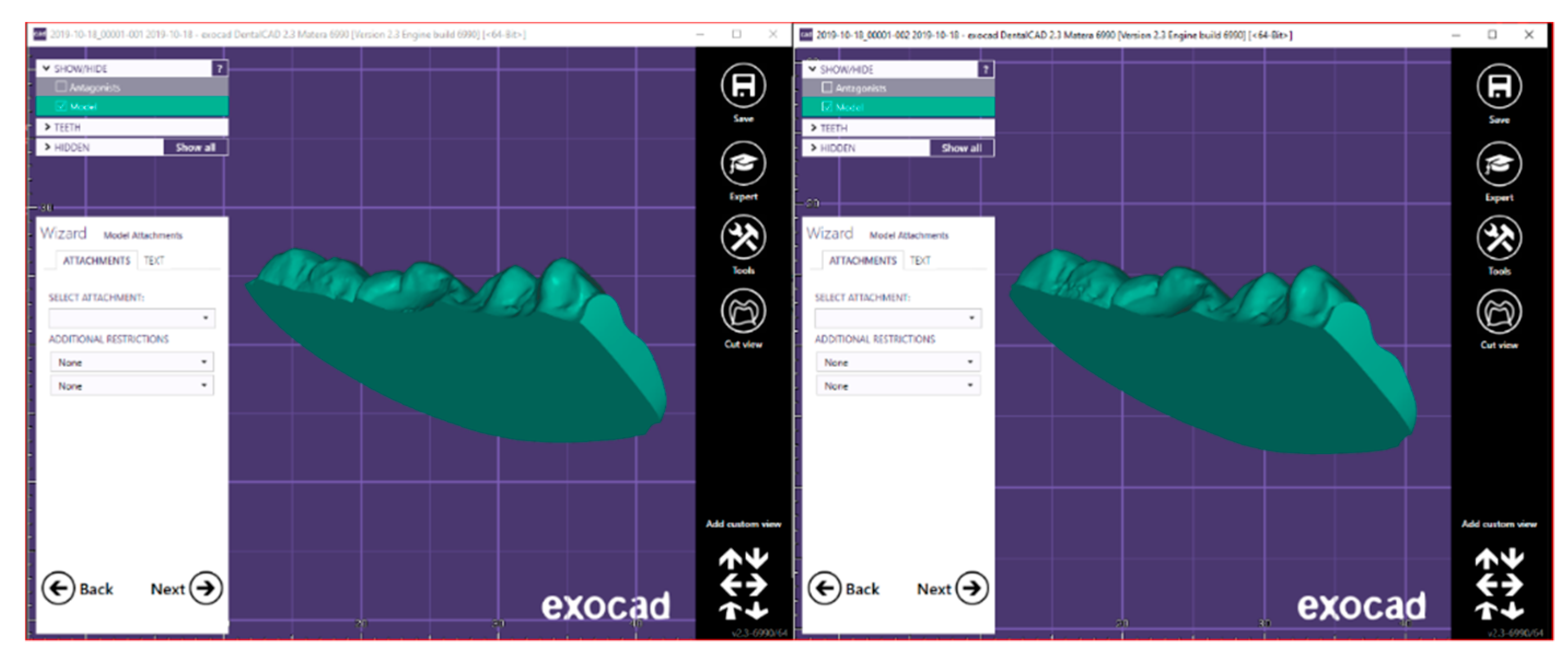
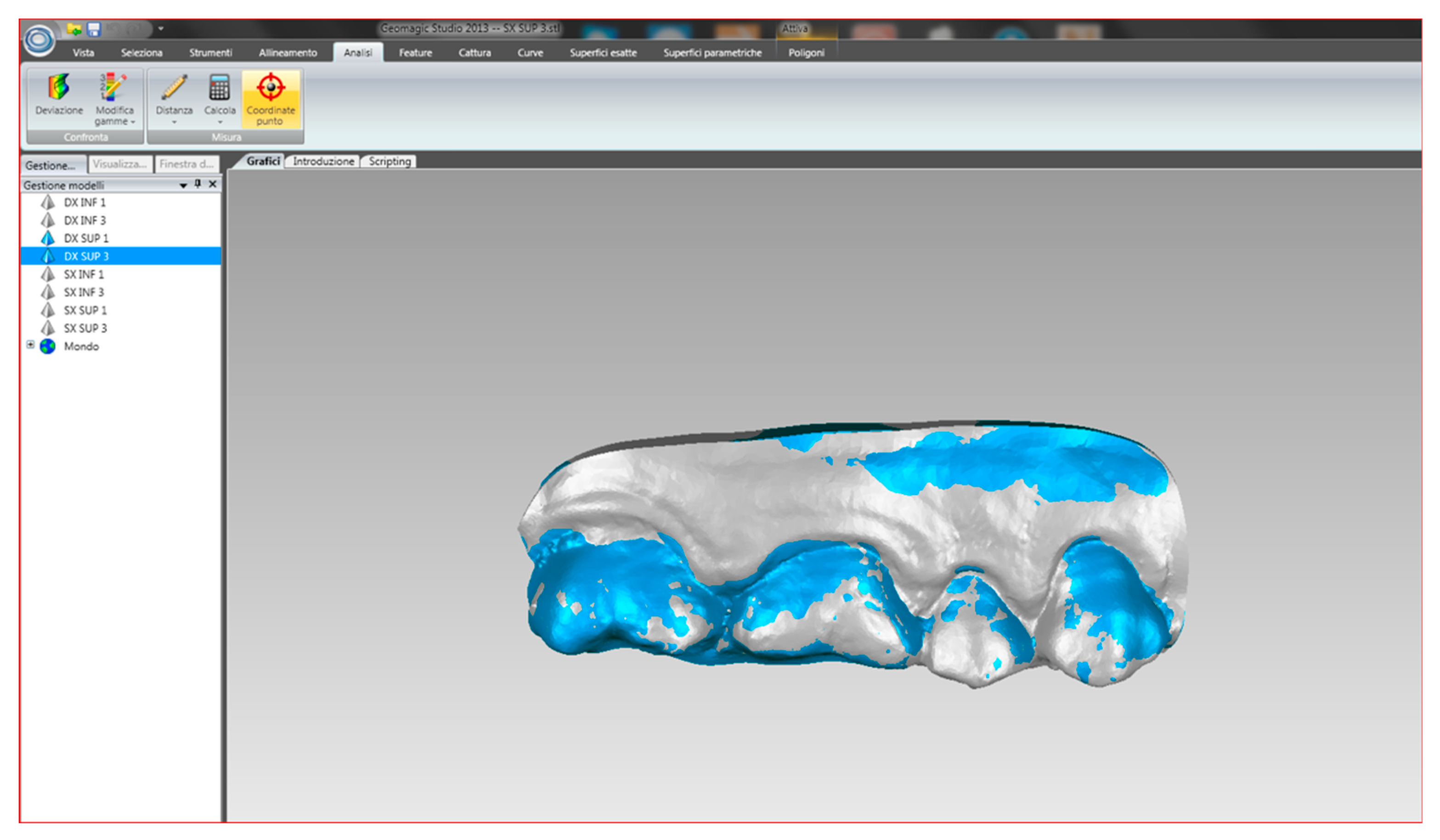
2.3. Procedure
- mandible
- maxilla
- buccal occlusal registration
- Partial scan of the arch: several teeth in the preparation area on the mandible and maxilla, and a buccal occlusal registration.
- Complete scan of the arch: maxilla, mandible and buccal occlusal registration.
2.4. Statistic Analysis
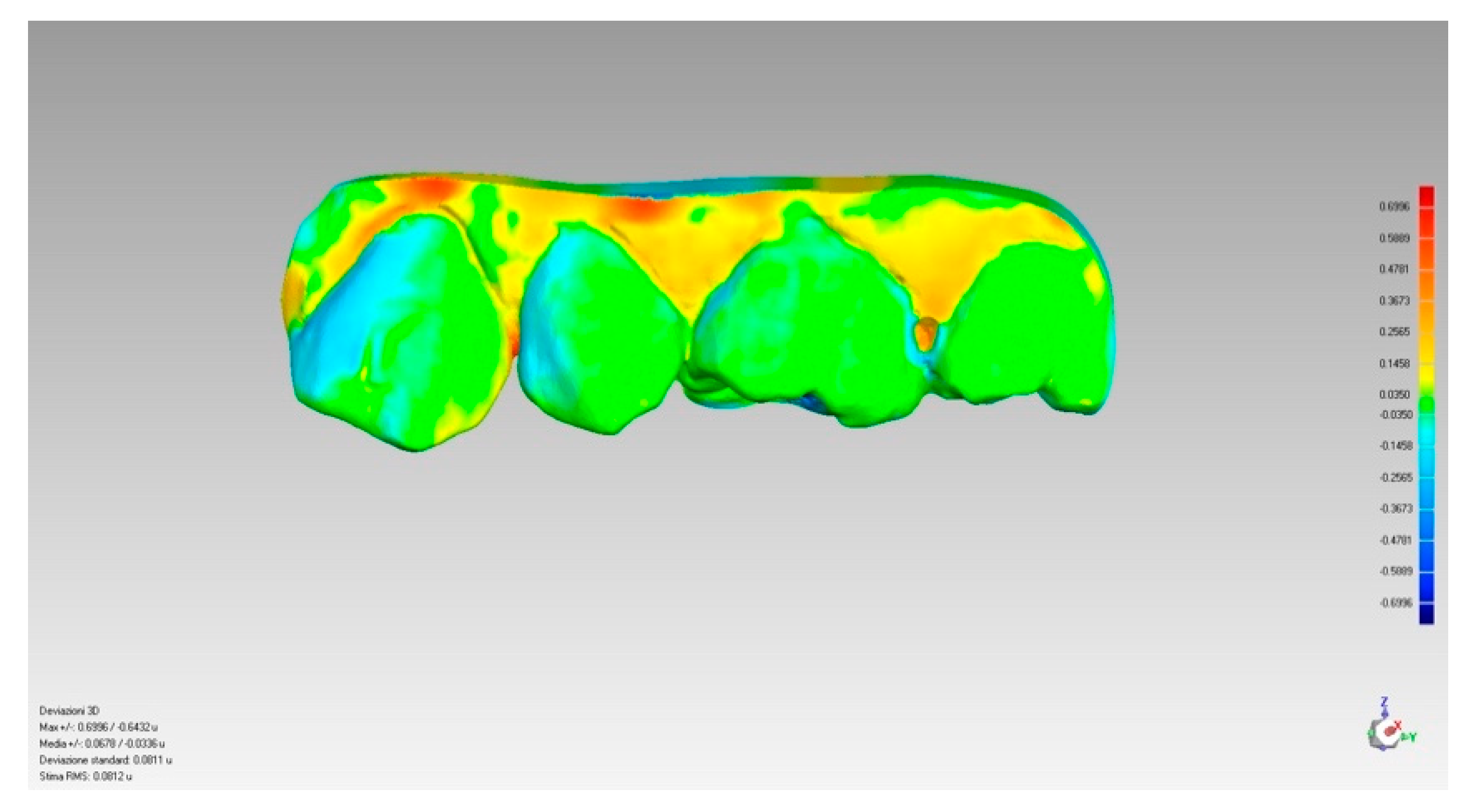
2.5. Treatment of the Collected Data
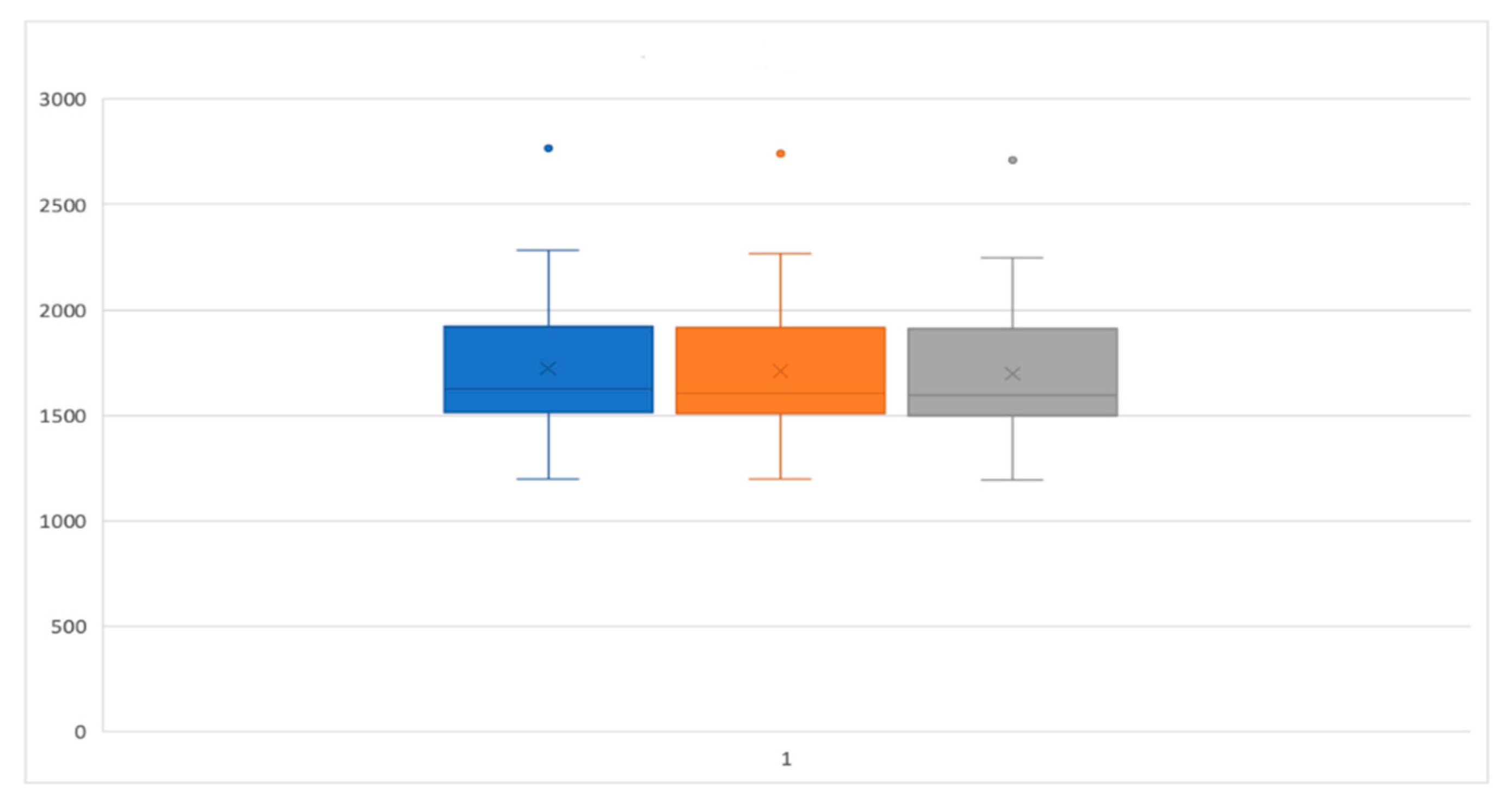
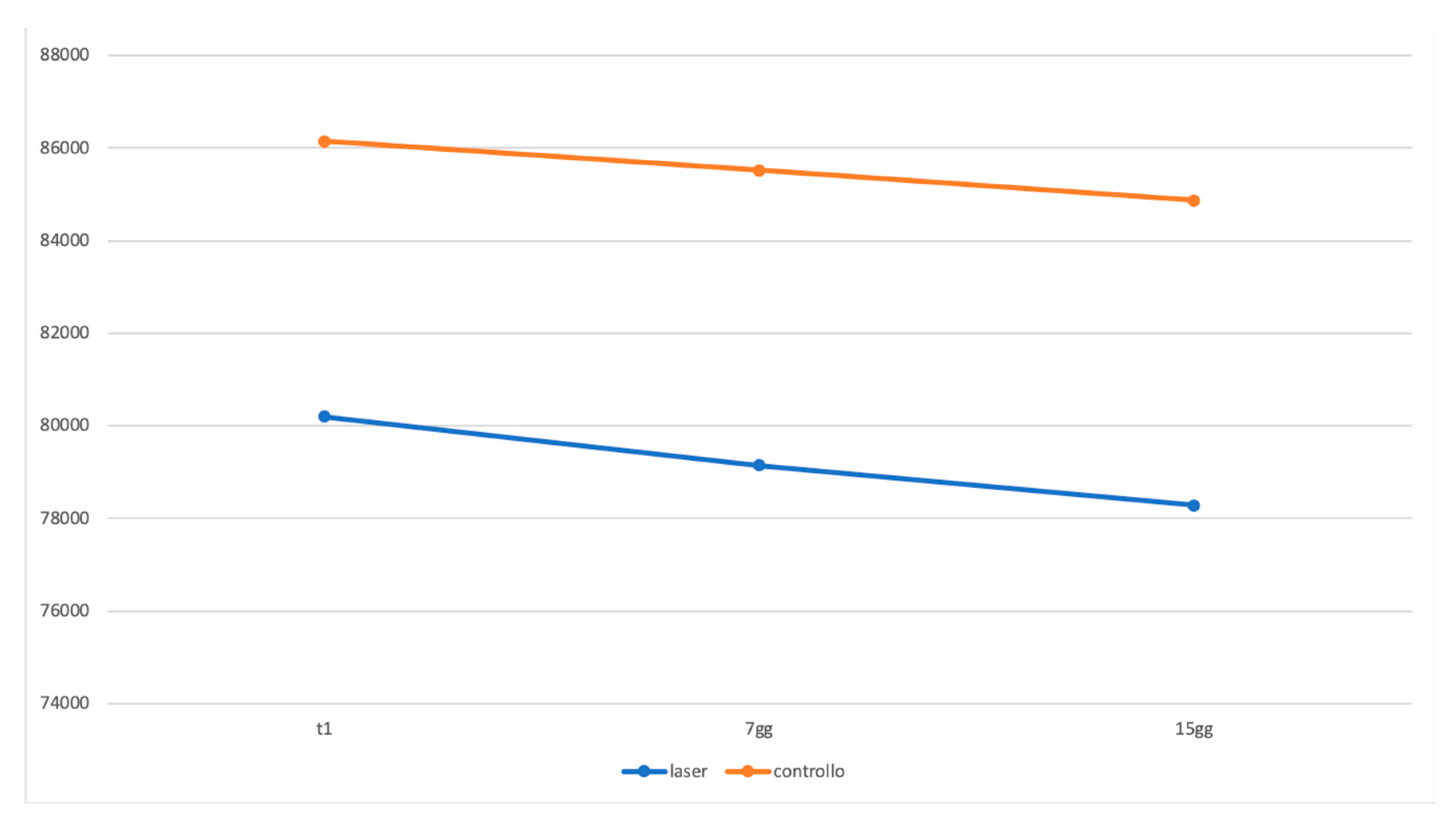
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Löe, H.; Theilade, E.; Jensen, S.B. Experimental gingivitis in man. J. Periodontol. 1965, 36, 177–187. [Google Scholar] [CrossRef] [PubMed]
- Theilade, E.; Wright, W.H.; Jensen, S.B.; Löe, H. Experimental gingivitis in man. II. A longitudinal clinical and bacteriological investigation. J. Periodontal Res. 1966, 1, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Trombelli, L.; Tatakis, D.N.; Scapoli, C.; Bottega, S.; Orlandini, E.; Tosi, M. Modulation of clinical expression of plaque-induced gingivitis. II. Identification of “high-responder” and “low-responder” subjects. J. Clin. Periodontol. 2004, 31, 239–252. [Google Scholar] [CrossRef] [PubMed]
- Lang, N.P.; Bartold, P.M. Periodontal health. J. Periodontol. 2018, 89 (Suppl. 1), S9–S16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kinane, D.F. Periodontitis modified by systemic factors. Ann. Periodontol. 1999, 4, 54–64. [Google Scholar] [CrossRef]
- Zmora, N.; Bashiardes, S.; Levy, M.; Elinav, E. The role of the immune system in metabolic health and disease. Cell Metab. 2017, 25, 506–521. [Google Scholar] [CrossRef] [Green Version]
- Capparé, P.; Teté, G.; Romanos, G.E.; Nagni, M.; Sannino, G.; Gherlone, E.F. The ‘All-on-four’ protocol in HIV-positive patients: A prospective, longitudinal 7-year clinical study. Int. J. Oral. Implantol. 2019, 12, 501–510. [Google Scholar]
- American Academy of Periodontology. Parameter on plaque-induced gingivitis. J. Periodontol. 2000, 71 (Suppl. 5), 851–852. [Google Scholar] [CrossRef]
- Löe, H.; Anerud, A.; Boysen, H.; Morrison, E. Natural history of periodontal disease in man. Rapid, moderate and no loss of attachment in Sri Lankan laborers 14 to 46 years of age. J. Clin. Periodontol. 1986, 13, 431–445. [Google Scholar]
- Ismail, A.I.; Morrison, E.C.; Burt, B.A.; Caffesse, R.G.; Kavanagh, M.T. Natural history of periodontal disease in adults: Findings from the Tecumseh Periodontal Disease Study, 1959–1987. J. Dent. Res. 1990, 69, 430–435. [Google Scholar] [CrossRef]
- Li, Y.; Lee, S.; Hujoel, P.; Su, M.; Zhang, W.; Kim, J.; Zhang, Y.P.; DeVizio, W. Prevalence and severity of gingivitis in American adults. Am. J. Dent. 2010, 23, 9–13. [Google Scholar] [PubMed]
- Murakami, S.; Mealey, B.L.; Mariotti, A.; Chapple, I.L.C. Dental plaque-induced gingival conditions. J. Periodontol. 2018, 89 (Suppl. 1), S17–S27. [Google Scholar] [CrossRef] [Green Version]
- Blicher, B.; Joshipura, K.; Eke, P. Validation of self-reported periodontal disease: A systematic review. J. Dent. Res. 2005, 84, 881–890. [Google Scholar] [CrossRef]
- Tecco, S.; Sciara, C.; Pantaleo, G.; Nota, A.; Visone, A.; Germani, S.; Polizzi, E.; Gherlone, E.F. The association between minor recurrent aphthous stomatitis (RAS), children’s poor oral condition, and underlying negative psychosocial habits and attitudes towards oral hygiene. BMC Pediatr. 2018, 18, 136. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- AlJehani, Y.A. Risk factors of periodontal disease: Review of the literature. Int. J. Dent. 2014, 2014, 182513. [Google Scholar] [CrossRef] [Green Version]
- Hart, T.C.; Gorry, M.C.; Hart, P.S.; Woodard, A.S.; Shihabi, Z.; Sandhu, J.; Shirts, B.; Xu, L.; Zhu, H.; Barmada, M.M.; et al. Mutations of the UMOD gene are responsible for medullary cystic kidney disease 2 and famil- ial juvenile hyperuricaemic nephropathy. J. Med. Genet. 2002, 39, 882–892. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Katz, J.; Guelmann, M.; Rudolph, M.; Ruskin, J. Acute streptococcal infection of the gingiva, lower lip, and pharynx—A case report. J. Periodontol. 2002, 73, 1392–1395. [Google Scholar] [CrossRef]
- Parisi, M.R.; Tecco, S.; Gastaldi, G.; Polizzi, E.; D’Amicantonio, T.; Negri, S.; Gardini, I.; Schlusnus, K.; Gherlone, E.; Capparè, P.; et al. Point-of-care testing for hepatitis C virus infection at alternative and high-risk sites: An Italian pilot study in a dental clinic. New Microbiol. 2017, 40, 242–245. [Google Scholar]
- Scully, C.; Epstein, J.; Porter, S.; Cox, M. Viruses and chronic disorders involving the human oral mucosa. Oral Surg. Oral Med. Oral Pathol. 1991, 72, 537–544. [Google Scholar] [CrossRef]
- Stone, S.J.; McCracken, G.I.; Heasman, P.A.; Staines, K.S.; Pennington, M. Cost-effectiveness of personalized plaque control for managing the gingival manifestations of oral lichen planus: A randomized controlled study. J. Clin. Periodontol. 2013, 40, 859–867. [Google Scholar] [CrossRef]
- Albandar, J.M.; Susin, C.; Hughes, F.J. Manifestations of systemic diseases and conditions that affect the periodontal attachment apparatus: Case definitions and diagnostic considerations. J. Periodontol. 2018, 89 (Suppl. 1), S183–S203. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Napier, S.S.; Speight, P.M. Natural history of potentially malignant oral lesions and conditions: An overview of the literature. J. Oral. Pathol. Med. 2008, 37, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Rawal, S.Y.; Claman, L.J.; Kalmar, J.R.; Tatakis, D.N. Traumatic lesions of the gingiva: A case series. J. Periodontol. 2004, 75, 762–769. [Google Scholar] [CrossRef] [PubMed]
- Eberhard, J.; Grote, K.; Luchtefeld, M.; Heuer, W.; Schuett, H.; Divchev, D.; Scherer, R.; Schmitz-Streit, R.; Langfeldt, D.; Stumpp, N.; et al. Experimental gingivitis induced systemic inflammatory markers in young healthy individuals: A single-subject interventional study. PLoS ONE 2013, 8, e55265. [Google Scholar] [CrossRef] [PubMed]
- Badersten, A.; Nilveus, R.; Egelberg, J. Effect of nonsurgical periodontal therapy. II. Severely advanced periodontitis. J. Clin. Periodontol. 1984, 11, 63–76. [Google Scholar] [CrossRef]
- Badersten, A.; Nilvéus, R.; Egelberg, J. Effect of nonsurgical periodontal therapy. I. Moderately advanced periodontitis. J. Clin. Periodontol. 1981, 8, 57–72. [Google Scholar] [CrossRef]
- Kaldahl, W.B.; Kalkwarf, K.L.; Patil, K.D.; Molvar, M.P.; Dyer, J.K. Long-term evaluation of periodontal therapy: I. Response to 4 therapeutic modalities. J. Periodontol. 1996, 67, 93–102. [Google Scholar] [CrossRef]
- Chapple, I.L.; Van der Weijden, F.; Doerfer, C.; Herrera, D.; Shapira, L.; Polak, D.; Madianos, P.; Louropoulou, A.; Machtei, E.; Donos, N.; et al. Primary prevention of periodontitis: Managing gingivitis. J. Clin. Periodontol. 2015, 42 (Suppl. 16), S71–S76. [Google Scholar] [CrossRef] [Green Version]
- Agerbaek, N.; Melsen, B.; Lind, O.P.; Glavind, L.; Kristiansen, B. Effect of regular small group instruction per se on oral health status of Danish schoolchildren. Community Dent. Oral Epidemiol. 1979, 7, 17–20. [Google Scholar] [CrossRef]
- Ramseier, C.A.; Anerud, A.; Dulac, M.; Lulic, M.; Cullinan, M.P.; Seymour, G.J.; Faddy, M.J.; Bürgin, W.; Schätzle, M.; Lang, N.P. Natural history of periodontitis: Disease progression and tooth loss over 40 years. J. Clin. Periodontol. 2017, 44, 1182–1191. [Google Scholar] [CrossRef] [Green Version]
- Albandar, J.M.; Kingman, A.; Brown, L.J.; Löe, H. Gingival inflammation and subgingival calculus as determinants of disease progression in early-onset periodontitis. J. Clin. Periodontol. 1998, 25, 231–237. [Google Scholar] [CrossRef] [PubMed]
- Serrano, J.; Escribano, M.; Roldán, S.; Martín, C.; Herrera, D. Efficacy of adjunctive anti-plaque chemical agents in managing gingivitis: A systematic review and meta-analysis. J. Clin. Periodontol. 2015, 42 (Suppl. 16), S106–S138. [Google Scholar] [CrossRef] [PubMed]
- Calderini, A.; Pantaleo, G.; Rossi, A.; Gazzolo, D.; Polizzi, E. Adjunctive effect of chlorhexidine antiseptics in mechanical periodontal treatment: First results of a preliminary case series. Int. J. Dent. Hyg. 2013, 11, 180–185. [Google Scholar] [CrossRef] [PubMed]
- Caruso, U.; Nastri, L.; Piccolomini, R.; d’Ercole, S.; Mazza, C.; Guida, L. Use of diode laser 980 nm as adjunctive therapy in the treatment of chronic periodontitis. A randomized controlled clinical trial. New Microbiol. 2008, 31, 513–518. [Google Scholar] [PubMed]
- Harris, D.M.; Yessik, M. Therapeutic ratio quantifies laser antisepsis: Ablation of Porphyromonas gingivalis with dental lasers. Lasers Surg. Med. 2004, 35, 206–213. [Google Scholar] [CrossRef]
- Coluzzi, D.J. Fundamentals of lasers in dentistry: Basic science tissue interaction and instrumentation. J. Laser Dent. 2008, 16, 4–10. [Google Scholar]
- Gutknecht, N.; Apel, C.; Bradley, P.; de Paul Eduardo, C.; Featherstone, J. Proceedings of the 1st International Workshop of Evidence Based Dentistry on Lasers in Dentistry; Quintessence Pub. Co.: London, UK; Chicago, IL, USA, 2008; pp. 166–167, 207–210. [Google Scholar]
- Moritz, A.; Schoop, U.; Goharkhay, K.; Schauer, P.; Doertbudak, O.; Wernisch, J.; Sperr, W. Treatment of periodontal pockets with a diode laser. Lasers Surg. Med. 1998, 22, 302–311. [Google Scholar] [CrossRef]
- Cobb, C.M.; Low, S.B.; Coluzzi, D.J. Lasers and the treatment of chronic periodontitis. Dent. Clin. N. Am. 2010, 54, 35–53. [Google Scholar] [CrossRef]
- Ishikawa, I.; Aoki, A.; Takasaki, A.A.; Mizutani, K.; Sasaki, K.M.; Izumi, Y. Application of lasers in periodontics: True innovation or myth? Periodontology 2000 2009, 50, 90–126. [Google Scholar] [CrossRef]
- Linde, J.; Nikolaus, P.L. Parodontologia Clinica ed Implantologia Orale—Sesta Edizione, 2016; Edi.Ermes: Milano, Italy, 2016; pp. 34–39. [Google Scholar]
- Schroeder, H.E.; Listgarten, M.A. The gingival tissues: The architecture of periodontal protection. Periodontology 2000 1997, 13, 91–120. [Google Scholar] [CrossRef]
- Zitzmann, N.U.; Berglundh, T. Definition and prevalence of peri-implant diseases. J. Clin. Periodontol. 2008, 35, 286–291. [Google Scholar] [CrossRef] [PubMed]
- Lang, N.P.; Schätzle, M.A.; Löe, H. Gingivitis as a risk factor in periodontal disease. J. Clin. Periodontol. 2009, 36 (Suppl. 10), 3–8. [Google Scholar] [CrossRef] [PubMed]
- Costa, F.O.; Takenaka Martinez, S.; Costa, L.O.; Ferreira, S.D.; Silva, G.L.; Costa, J.L. Peri-implant disease in patients with and without preventive maintenance: A 5-year follow-up. J. Clin. Periodontol. 2012, 39, 173–181. [Google Scholar] [CrossRef] [PubMed]
- Wilkins, E.M. La Pratica Clinica Dell’Igienista Dentale. II Edizione Italiana, a Cura di Nardi, G.M. (2011); Ediotre Piccin Nuova Libraria: Padova, Italy, 2011; pp. 3–17. [Google Scholar]
- Malchiodi, L.; Caricasulo, R.; Cucchi, A.; Vinci, R.; Agliardi, E.; Gherlone, E. Evaluation of Ultrashort and Longer Implants with Microrough Surfaces: Results of a 24- to 36-Month Prospective Study. Int. J. Oral Maxillofac. Implants 2017, 32, 171–179. [Google Scholar] [CrossRef]
- Vinci, R.; Teté, G.; Lucchetti, F.R.; Capparé, P.; Gherlone, E.F. Implant survival rate in calvarial bone grafts: A retrospective clinical study with 10 year follow-up. Clin. Implant. Dent. Relat. Res. 2019, 21, 662–668. [Google Scholar] [CrossRef]
- Agliardi, E.L.; Tetè, S.; Romeo, D.; Malchiodi, L.; Gherlone, E. Immediate function of partial fixed rehabilitation with axial and tilted implants having intrasinus insertion. J. Craniofac. Surg. 2014, 25, 851–855. [Google Scholar] [CrossRef]
- Maló, P.; Rigolizzo, M.; Nobre, M.; Lopes, A.; Agliardi, E. Clinical outcomes in the presence and absence of keratinized mucosa in mandibular guided implant surgeries: A pilot study with a proposal for the modification of the technique. Quintessence Int. 2013, 44, 149–157. [Google Scholar]
- Mühlemann, H.R.; Son, S. Gingival sulcus bleeding-a leading symptom in initial gingivitis. Helv. Odontol. Acta. 1971, 15, 107–113. [Google Scholar]
- Aykol, G.; Baser, U.; Maden, I.; Kazak, Z.; Onan, U.; Tanrikulu-Kucuk, S. The effect of low-level laser therapy as an adjunct to non-surgical periodontal treatment. J. Periodontol. 2011, 82, 481–488. [Google Scholar] [CrossRef]
- Saglam, M.; Kantarci, A.; Dundar, N.; Hakki, S.S. Clinical and biochemical effects of diode laser as an adjunct to nonsurgical treatment of chronic periodontitis: A randomized, controlled clinical trial. Lasers Med. Sci. 2014, 29, 37–46. [Google Scholar] [CrossRef]
- Kreisler, M.; Al Haj, H.; d’Hoedt, B. Clinical efficacy of semiconductor laser application as an adjunct to conventional scaling and root planing. Lasers Surg. Med. 2005, 37, 350–355. [Google Scholar] [CrossRef]
- Aoki, A.; Sasaki, K.M.; Watanabe, H.; Ishikawa, I. Lasers in nonsurgical periodontal therapy. Periodontology 2000 2004, 36, 59–97. [Google Scholar] [CrossRef] [PubMed]
- Ambrosini, P.; Miller, N.; Briancxon, S.; Gallina, S.; Penaud, J. Clinical and microbiological evaluation of the effectiveness of the Nd:Yap laser for the initial treatment of adult periodontitis. A randomized controlled study. J. Clin. Periodontol. 2005, 32, 670–676. [Google Scholar] [CrossRef] [PubMed]
- Assaf, M.; Yilmaz, S.; Kuru, B.; Ipci, S.D.; Noyun, U.; Kadir, T. Effect of the diode laser on bacteremia associated with dental ultrasonic scaling: A clinical and microbiological study. Photomed. Laser Surg. 2007, 25, 250–256. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Karlsson, M.R.; Diogo Löfgren, C.I.; Jansson, H.M. The effect of laser therapy as an adjunct to non-surgical periodontal treatment in subjects with chronic periodontitis: A systematic review. J. Periodontol. 2008, 79, 2021–2028. [Google Scholar] [CrossRef]
- Matys, J.; Grzech-Leśniak, K.; Flieger, R.; Dominiak, M. Assessment of an impact of a diode laser mode with wavelength of 980 nm on a temperature rise measured by means of k0−2 thermocouple: Preliminary results. Dent. Med. Probl. 2016, 53, 345–351. [Google Scholar] [CrossRef] [Green Version]





| Group 1 | Procedures | PI MEDIAN (IQR) | BOP MEDIAN (IQR) |
|---|---|---|---|
| T0 | LASER | 61 (50–82) | 33 (28–55) |
| CONTROL | 60 (48–83) | 35 (29–55) | |
| T1 | LASER | 10 (8–12) | 3 (0–6) |
| CONTROL | 10 (8–12) | 3 (1–6) | |
| T1–T0 | LASER | −53 (−70–39) | −33 (−50–27) |
| CONTROL | −51 (−70–36) | −31 (−49–28) | |
| T2 | LASER | 10 (9–13) | 0 (0–82) |
| CONTROL | 11 (10–13) | 3 (1–6) | |
| T2–T1 | LASER | 1(0–2) | 3 (0–6) |
| CONTROL | 1(0–1) | 0 (0–1) |
| Group 2 | Procedures | PI MEAN (SD) | BOP MEAN (SD) | p-Value |
|---|---|---|---|---|
| T0 | LASER | 67.32 (22) | 46.76 (29.14) | n.s. |
| CONTROL | 68.48 (22.39) | 46.96 (29.09) | ||
| T1 | LASER | 11.64 (6.68) | 4 (5.08) | n.s. |
| CONTROL | 12.16 (6.54) | 4.84 (5.26) | ||
| T1–T0 | LASER | −0.56 (0.18) | −0.43 (0.26) | n.s. |
| CONTROL | −0.54 (−0.19) | −0.42 (0.25) | ||
| T2 | LASER | 12.76 (7.57) | 67.32 (22) | n.s. |
| CONTROL | 13.16 (7.40) | 5.20 (5.35) | ||
| T2–T1 | LASER | 0.01 (0.02) | −0.43 (0.26) | n.s. |
| CONTROL | 0.01 (0.02) | 0.00 (0.01) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Polizzi, E.; Tetè, G.; Targa, C.; Salviato, B.; Ferrini, F.; Gastaldi, G. Evaluation of the Effectiveness of the Use of the Diode Laser in the Reduction of the Volume of the Edematous Gingival Tissue after Causal Therapy. Int. J. Environ. Res. Public Health 2020, 17, 6192. https://doi.org/10.3390/ijerph17176192
Polizzi E, Tetè G, Targa C, Salviato B, Ferrini F, Gastaldi G. Evaluation of the Effectiveness of the Use of the Diode Laser in the Reduction of the Volume of the Edematous Gingival Tissue after Causal Therapy. International Journal of Environmental Research and Public Health. 2020; 17(17):6192. https://doi.org/10.3390/ijerph17176192
Chicago/Turabian StylePolizzi, Elisabetta, Giulia Tetè, Claudia Targa, Barbara Salviato, Francesco Ferrini, and Giorgio Gastaldi. 2020. "Evaluation of the Effectiveness of the Use of the Diode Laser in the Reduction of the Volume of the Edematous Gingival Tissue after Causal Therapy" International Journal of Environmental Research and Public Health 17, no. 17: 6192. https://doi.org/10.3390/ijerph17176192
APA StylePolizzi, E., Tetè, G., Targa, C., Salviato, B., Ferrini, F., & Gastaldi, G. (2020). Evaluation of the Effectiveness of the Use of the Diode Laser in the Reduction of the Volume of the Edematous Gingival Tissue after Causal Therapy. International Journal of Environmental Research and Public Health, 17(17), 6192. https://doi.org/10.3390/ijerph17176192





