Access to an Electronic Health Record: A Polish National Survey
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Questionnaire
2.3. Data Analyses
3. Results
3.1. Characteristics of the Respondents
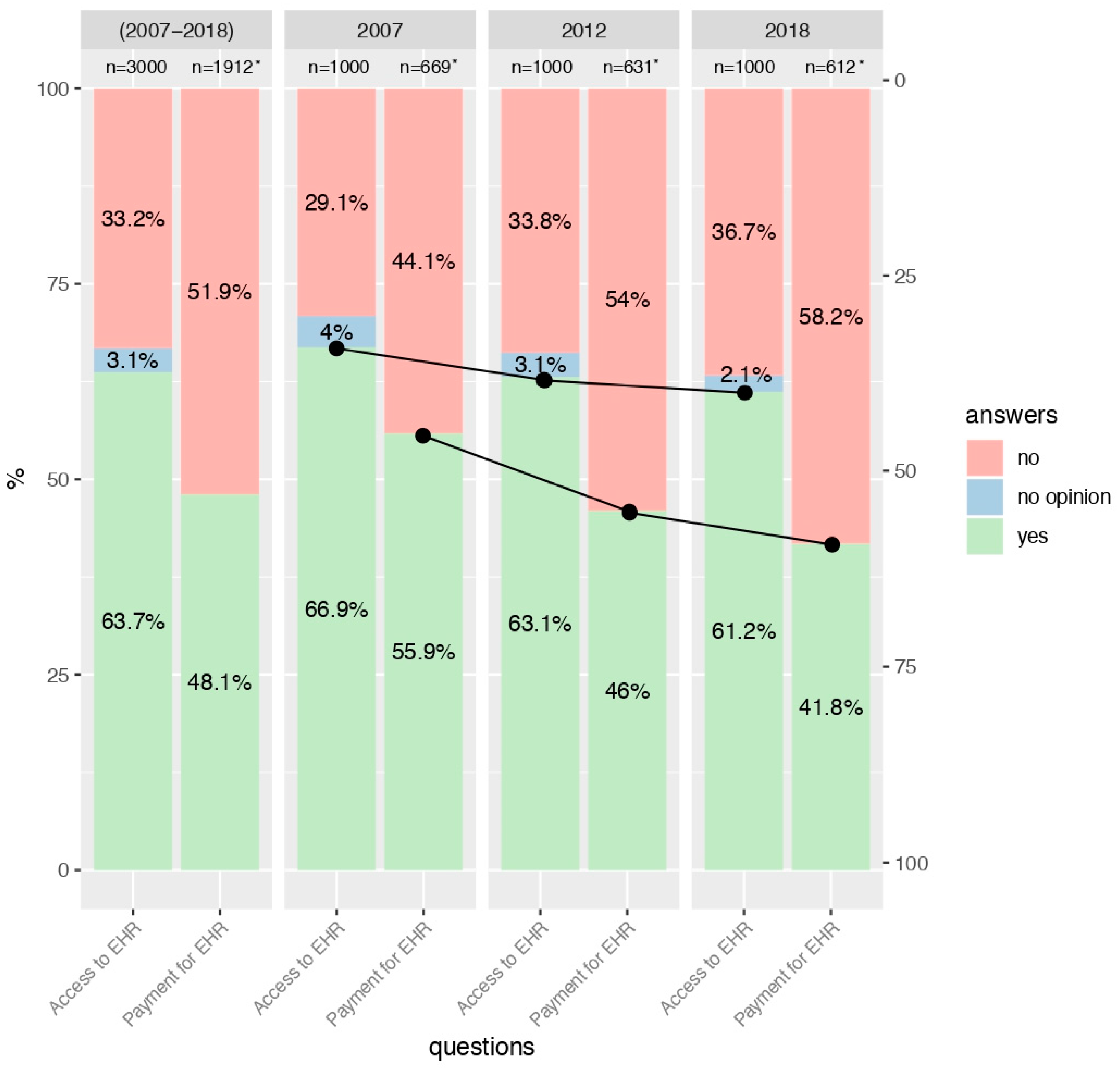
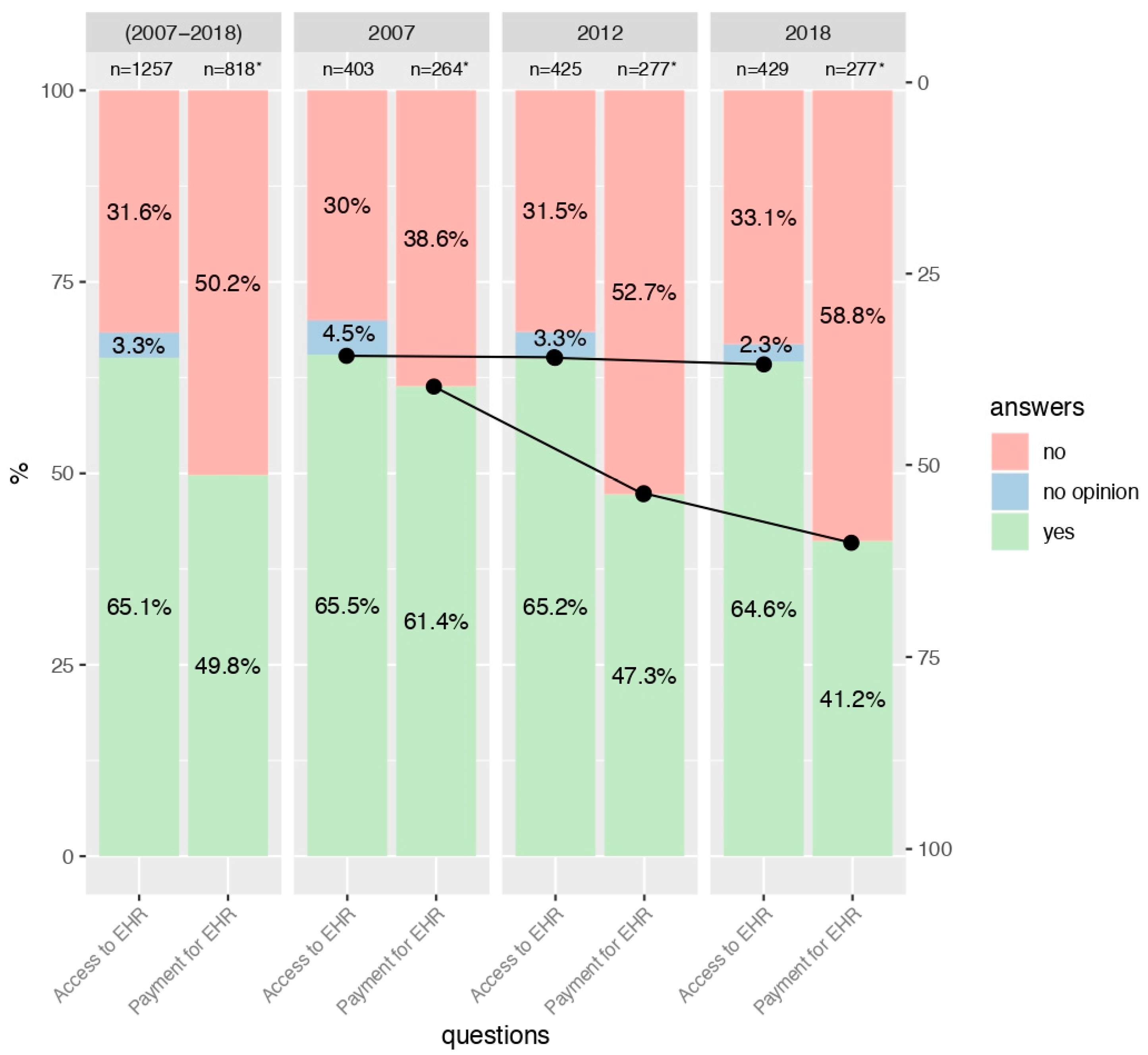
3.2. Interest in Access to EHRs
3.3. Consent to Payment for Access to EHRs
3.4. Impact of Sociodemographic Variables on Interest in Access to EHRs
3.5. Impact of Sociodemographic Variables on Consent to Payment for Access to EHRs
3.6. Profile of the Potential EHR User
4. Discussion
4.1. Trends Regarding Interest in Access to EHRs
4.2. Trends Regarding Consent to Payment for Access to EHRs
4.3. Impact of Sociodemographic Variables on Interest in Access and Consent to Pay for EHRs
4.4. Comparison with Other Countries and Implication for the Future
4.5. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Bujnowska-Fedak, M.M.; Węgierek, P. The impact of online health information on patient health behaviours and making decisions concerning health. Int. J. Environ. Res. Public Health 2020, 17, 880. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Novel Coronavirus Pneumonia Emergency Response Epidemiology Team. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. Zhonghua Liu Xing Bing Xue Za Zhi 2020, 41, 145–151. [Google Scholar] [CrossRef]
- Deetjen, U. European E-Prescriptions: Benefits and Success Factors; Cyber Studies Programmme: Oxford, UK, 2016. [Google Scholar]
- Carnicero Giménez de Azcárate, J.; Rojas, D. Economic Commission for Latin America and the Caribbean. Social Development Division. In Application of Information and Communication Technologies for Health Systems in Belgium, Denmark, Spain, the United Kingdom and Sweden; Naciones Unidas, CEPAL: Santiago, Chile, 2010; ISBN 9789211217469. [Google Scholar]
- Hufstader, M.; Swain, M.; Furukawa, M.F. State Variation in E-Prescribing Trends in the United States—ONC Data Brief. No. 4 November 2012; ONC: Washington, DC, USA, 2012.
- Porterfield, A.; Engelbert, K.; Coustasse, A. Electronic prescribing: Improving the efficiency and accuracy of prescribing in the ambulatory care setting. Perspect. Health Inf. Manag. 2014, 11, 1g. [Google Scholar] [PubMed]
- The ePrescription System: Draft Amending the Act on Medicines is under Discussion in the Parliament of the Czech Republic—Lexology. Available online: https://www.lexology.com/library/detail.aspx?g=a82ee2c5-4bfc-46d4-bbf9-f83d04f452a8& (accessed on 1 April 2020).
- Kiljan, A.; Romaszewski, A.; Kopański, Z.; Liniarski, M.; Dyl, S.; Rowiński, J. The benefits of using an e-prescription. J. Public Health Nurs. Med. Rescue 2019, 289, 32–34. [Google Scholar]
- Czerska, I.; Trojanowska, A.; Korpak, T. Przyszłość Opieki Zdrowotnej w Polsce—Nowe Horyzonty [The Future of Healthcare in Poland—New Horizons.]. In E-Wydawnictwo. Prawnicza i Ekon. Bibl. Cyfrowa. Wydz. Prawa, Adm. i Ekon. Uniw. Wrocławskiego; E-Wydawnictwo: Portal, Poland, 2019; pp. 197–214. [Google Scholar] [CrossRef]
- National EHR System Exists—European Health Information Gateway. Available online: https://gateway.euro.who.int/en/indicators/ehealth_survey_84-has-a-national-ehr-system/ (accessed on 1 April 2020).
- Jha, A.K.; Doolan, D.; Grandt, D.; Scott, T.; Bates, D.W. The use of health information technology in seven nations. Int. J. Med. Inform. 2008, 77, 848–854. [Google Scholar] [CrossRef]
- Adler-Milstein, J.; DesRoches, C.M.; Kralovec, P.; Foster, G.; Worzala, C.; Charles, D.; Searcy, T.; Jha, A.K. Electronic health record adoption in us hospitals: Progress continues, but challenges persist. Health Aff. 2015, 34, 2174–2180. [Google Scholar] [CrossRef] [Green Version]
- Stroetmann, K.A.; Artmann, J.; Stroetmann, V.N.; Protti, D.; Dumortier, J.; Giest, S.; Walossek, U.; Whitehouse, D. eHealth Strategies—European Countries on their Journey towards National eHealth Infractructers—Final European Progress Report; European Commission: Luxembourg, 2011; pp. 1–60. Available online: http://ec.europa.eu/information_society/ehealth (accessed on 23 March 2020).
- Bonomi, S. The Electronic Health Record: A Comparison of Some European Countries. Inf. Commun. Technol. Organ. Soc. 2016, 15, 205–214. [Google Scholar] [CrossRef]
- Adler-Milstein, J.; DesRoches, C.M.; Furukawa, M.F.; Worzala, C.; Charles, D.; Kralovec, P.; Stalley, S.; Jha, A.K. More than half of US hospitals have at least a basic EHR, but stage 2 criteria remain challenging for most. Health Aff. 2014, 33, 1664–1671. [Google Scholar] [CrossRef] [Green Version]
- Hsiao, C.J.; Hing, E.; Ashman, J. Trends in Electronic Health Record System Use Among Office-based Physicians: United States, 2007–2012. Natl. Health Stat. Report. 2014, 75, 1–17. [Google Scholar]
- Zlabek, J.A.; Wickus, J.W.; Mathiason, M.A. Early cost and safety benefits of an inpatient electronic health record. J. Am. Med. Inform. Assoc. 2011, 18, 169–172. [Google Scholar] [CrossRef] [Green Version]
- Christensen, L. The Role of Web Interviews as Part of a National Travel Survey. In Transport Survey Methods: Best Practice for Decision Making; Emerald Group Publishing Limited: Bingley, UK, 2013; pp. 115–154. [Google Scholar]
- Bujnowska-Fedak, M.M.; Kurpas, D. The influence of online health information on the attitude and behavior of people aged 50+. Adv. Exp. Med. Biol. 2015, 861, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Santana, S.; Lausen, B.; Bujnowska-Fedak, M.; Chronaki, C.E.; Prokosch, H.U.; Wynn, R. Informed citizen and empowered citizen in health: Results from an European survey. BMC Fam. Pract. 2011, 12, 20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bujnowska-Fedak, M.M.; Mastalerz-Migas, A. Usage of Medical Internet and E-Health Services by the Elderly. In Advances in Experimental Medicine and Biology; Springer: New York, NY, USA, 2014; Volume 834, pp. 75–80. [Google Scholar]
- Bujnowska-Fedak, M.M.; Waligóra, J.; Mastalerz-Migas, A. The Internet as a Source of Health Information and Services. In Advances in Experimental Medicine and Biology; Springer: Singapore, 2019; Volume 1211, pp. 1–16. [Google Scholar]
- Waligóra, J.; Bujnowska–Fedak, M.M. Online Health Technologies and Mobile Devices: Attitudes, Needs, and Future. In Advances in Experimental Medicine and Biology; Springer: New York, NY, USA, 2019; Volume 1153, pp. 19–29. [Google Scholar]
- Andreassen, H.K.; Bujnowska-Fedak, M.M.; Chronaki, C.E.; Dumitru, R.C.; Pudule, I.; Santana, S.; Voss, H.; Wynn, R. European citizens’ use of E-health services: A study of seven countries. BMC Public Health 2007, 7, 53. [Google Scholar] [CrossRef] [Green Version]
- Bujnowska-Fedak, M.M. Trends in the use of the Internet for health purposes in Poland. BMC Public Health 2015, 15, 194. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kummervold, P.E.; Chronaki, C.E.; Lausen, B.; Prokosch, H.-U.; Rasmussen, J.; Santana, S.; Staniszewski, A.; Wangberg, S.C. eHealth trends in Europe 2005–2007: A population-based survey. J. Med. Internet Res. 2008, 10, e42. [Google Scholar] [CrossRef] [PubMed]
- Pang, Z.; Yuan, H.; Zhang, Y.T.; Packirisamy, M. Guest Editorial Health Engineering Driven by the Industry 4.0 for Aging Society. IEEE J. Biomed. Health Inform. 2018, 22, 1709–1710. [Google Scholar] [CrossRef]
- Carbonaro, G.; Leanza, E.; McCann, P.; Medda, F. Demographic Decline, Population Aging, and Modern Financial Approaches to Urban Policy. Int. Reg. Sci. Rev. 2018, 41, 210–232. [Google Scholar] [CrossRef]
- Xuming, L.; Lina, C.; Peng, J.; Xiao, G.; Shuo, C. Current status and future prospects of data leakage prevention technology: A brief review. J. Phys. Conf. Ser. 2019, 1345, 22010. [Google Scholar] [CrossRef]
- Flynn, T.; Grispos, G.; Glisson, W.; Mahoney, W. Knock! Knock! Who Is There? Investigating Data Leakage from a Medical Internet of Things Hijacking Attack. In Proceedings of the 53rd Hawaii International Conference on System Sciences, Hawaii, HI, USA, 7–10 January 2020. [Google Scholar]
- Mou, J.; Shin, D.H.; Cohen, J.F. Trust and risk in consumer acceptance of e-services. Electron. Commer. Res. 2017, 17, 255–288. [Google Scholar] [CrossRef]
- Jara, A.J.; Bocchi, Y. GEO-Trust: Geo-aware security protocol for enabling cross-border trustable operations and data exchange in a global digital economy. In Proceedings of the 2019 IEEE 1st Sustainable Cities Latin America Conference, SCLA 2019, Arequpar, Peru, 26–29 August 2019. [Google Scholar]
- Massarczyk, P.; Winzer, E. Influence of the Perceived Data Security, Credibility, Trust and Confidence on the Usage Frequency of Internet Services and the Provision of Security Measures; IEEE: Piscataway Township, NJ, USA, 2019. [Google Scholar]
- Campanella, N.; Srl, N.; Benedetto del Tronto, S.; Piceno, A.; Pierpaolo Morosini, I.; Sampaolo, G.; Wright, H. Satisfaction of Medical Doctors in Handling the Citizen’s Electronic Health Record. Qual. Primaty Care 2017, 25, 267–272. [Google Scholar]
- Osop, H.; Sahama, T. Doctors’ perception of the potential of EHR: A Singapore insight. ACSW ’18 Proc. Australas. Comput. Sci. Week Multiconference 2017, 6, 1–6. [Google Scholar] [CrossRef]
- Frison, E.; Eggermont, S. “Harder, Better, Faster, Stronger”: Negative Comparison on Facebook and Adolescents’ Life Satisfaction Are Reciprocally Related. Cyberpsychol. Behav. Soc. Netw. 2016, 19, 158–164. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ruiz-Palomino, E.; Giménez-García, C.; Ballester-Arnal, R.; Gil-Llario, M.D. Health promotion in young people: Identifying the predisposing factors of self-care health habits. J. Health Psychol. 2018. [Google Scholar] [CrossRef] [PubMed]
- Bensing, J.M.; Verhaak, P.F.M. Somatisation: A joint responsibility of doctor and patient. Lancet 2006, 367, 452–454. [Google Scholar] [CrossRef] [Green Version]
- Sobczak, K.; Leoniuk, K.; Pawłowski, L.; Spolak, N. Clinical communication—A comparison of patients’ and doctors’ opinions. Pomeranian J. Life Sci. 2017, 62. [Google Scholar] [CrossRef] [Green Version]
- Currie, C.; Hurrlemann, K.; Settertobulte, W.; Smith, R.; Todd, J. Health and Health Behaviour Among Young People: International Report. In WHO Policy Series: Health Policy for Children and Adolescents; WHO Regional Office for Europe: Copenhagen, Danmark, 2000. [Google Scholar]
- Verhaeghe, R.; Mak, R.; Van Maele, G.; Kornitzer, M.; De Backer, G. Job stress among middle-aged health care workers and its relation to sickness absence. Stress Health 2003, 19, 265–274. [Google Scholar] [CrossRef]
- Luster, J.; Ratz, D.; Wei, M.Y. Predictors of social participation among middle-aged and older Americans: Data from the Health and Retirement Study. In Proceedings of the APHA’s 2019 Annual Meeting and Expo, Philadelphia, PA, USA, 2–6 November 2019. [Google Scholar]
- Zarina, I.; Circenis, K.; Erts, R. Measuring the technophobia among middle-aged and older adults in Latvia: A pilot study. SHS Web Conf. 2018, 51, 02003. [Google Scholar] [CrossRef] [Green Version]
- Chiu, C.-J.; Liu, C.-W. Understanding Older Adult’s Technology Adoption and Withdrawal for Elderly Care and Education: Mixed Method Analysis from National Survey. J. Med. Internet Res. 2017, 19, e374. [Google Scholar] [CrossRef] [Green Version]
- Benyamini, Y.; Leventhal, E.A.; Leventhal, H. Elderly people’s ratings of the importance of health-related factors to their self-assessments of health. Soc. Sci. Med. 2003, 56, 1661–1667. [Google Scholar] [CrossRef]
- Binelli, C. Employment and Earnings Expectations of Jobless Young Skilled: Evidence from Italy. Soc. Indic. Res. 2019, 145, 201–231. [Google Scholar] [CrossRef]
- Dotti Sani, G.M.; Acciai, C. Two hearts and a loan? Mortgages, employment insecurity and earnings among young couples in six European countries. Urban. Stud. 2018, 55, 2451–2469. [Google Scholar] [CrossRef]
- Poggenpoel, M.; Jacobs, F.E.; Myburgh, C.P.H.; Temane, A.M. Young families become mindful of their possibilities through the appreciation of their family life. Health SA Gesondheid 2017, 22, a948. [Google Scholar] [CrossRef] [Green Version]
- Jin, Y.; Hou, Z.; Zhang, D. Determinants of health insurance coverage among people aged 45 and over in China: Who buys public, private and multiple insurance. PLoS ONE 2016, 11, e0161774. [Google Scholar] [CrossRef] [Green Version]
- Phanie Baggio Id, S.; Dupuis, M.; Wolff, H.; Bodenmann, P. Associations of lack of voluntary private insurance and out-of-pocket expenditures with health inequalities. Evidence from an international longitudinal survey in countries with universal health coverage. PLoS ONE 2018, 13, e0204666. [Google Scholar] [CrossRef] [Green Version]
- Lewis, S.; Collyer, F.; Willis, K.; Harley, K.; Marcus, K.; Calnan, M.; Gabe, J. Healthcare in the news media: The privileging of private over public. J. Sociol. 2018, 54, 574–590. [Google Scholar] [CrossRef]
- Dolls, M.; Doerrenberg, P.; Peichl, A.; Stichnoth, H. Do retirement savings increase in response to information about retirement and expected pensions? J. Public Econ. 2018, 158, 168–179. [Google Scholar] [CrossRef] [Green Version]
- Giovanis, E.; Ozdamar, O. Health status, mental health and air quality: Evidence from pensioners in Europe. Environ. Sci. Pollut. Res. 2018, 25, 14206–14225. [Google Scholar] [CrossRef] [Green Version]
- Stafford, M.; Steventon, A.; Thorlby, R.; Fisher, R.; Turton, C.; Deeny, S. Briefing: Understanding the Health Care Needs of People with Multiple Health Conditions; The Health Foundation: London, UK, 2018. [Google Scholar]
- Zhang, Y.; Coello, P.A.; Brozek, J.; Wiercioch, W.; Etxeandia-Ikobaltzeta, I.; Akl, E.A.; Meerpohl, J.J.; Alhazzani, W.; Carrasco-Labra, A.; Morgan, R.L.; et al. Using patient values and preferences to inform the importance of health outcomes in practice guideline development following the GRADE approach. Health Qual. Life Outcomes 2017, 15, 1–10. [Google Scholar] [CrossRef]
- Lamu, A.N.; Olsen, J.A. The relative importance of health, income and social relations for subjective well-being: An integrative analysis. Soc. Sci. Med. 2016, 152, 176–185. [Google Scholar] [CrossRef] [Green Version]
- Yamashita, N.; Kuzuoka, H.; Kudo, T.; Hirata, K.; Aramaki, E.; Hattori, K. How Information Sharing About Care Recipients by Family Caregivers Impacts Family Communication. In Proceedings of the Conference on Human Factors in Computing Systems—Proceedings; Association for Computing Machinery: New York, NY, USA, 2018; pp. 1–13. [Google Scholar]
- Cortés, P.; Pan, J. When time binds: Substitutes for household production, returns to working long hours, and the skilled gender wage gap. J. Labor Econ. 2019, 37, 351–398. [Google Scholar] [CrossRef]
- Mulyaningsih, T.; Purwaningsih, Y.; Anggun, K. The Monetary Value of Market Replaceable Household Production: An Empirical Study of the Economic Significance of Housewives’ Roles. Makara Hubs-Asia 2018, 22, 43–55. [Google Scholar] [CrossRef]
- Verbakel, E. How to understand informal caregiving patterns in Europe? The role of formal long-term care provisions and family care norms. Scand. J. Public Health 2018, 46, 436–447. [Google Scholar] [CrossRef] [Green Version]
- Carroll, J.K.; Moorhead, A.; Bond, R.; LeBlanc, W.G.; Petrella, R.J.; Fiscella, K. Who uses mobile phone health apps and does use matter? A secondary data analytics approach. J. Med. Internet Res. 2017, 19, e125. [Google Scholar] [CrossRef] [Green Version]
- Fennell, C.; Barkley, J.E.; Lepp, A. The relationship between cell phone use, physical activity, and sedentary behavior in adults aged 18–80. Comput. Human Behav. 2019, 90, 53–59. [Google Scholar] [CrossRef]
- Zajacova, A.; Lawrence, E.M. The Relationship Between Education and Health: Reducing Disparities Through a Contextual Approach. Annu. Rev. Public Health 2018, 39, 273–289. [Google Scholar] [CrossRef] [Green Version]
- Yuan, J.; Lu, Y.; Ferrier, R.C.; Liu, Z.; Su, H.; Meng, J.; Song, S.; Jenkins, A. Urbanization, rural development and environmental health in China. Environ. Dev. 2018, 28, 101–110. [Google Scholar] [CrossRef]
- The Road to School: How Far Students Travel to School in the Choice-Rich Cities of Denver, Detroit, New Orleans, New York City, and Washington, DC | Greater DC. Available online: https://greaterdc.urban.org/publication/road-school-how-far-students-travel-school-choice-rich-cities-denver-detroit-new (accessed on 14 May 2020).
- Mody, M.; Gordon, S.; Lehto, X.; Adler, H. Study abroad and the development of college students’ travel venturesomeness. Tour. Manag. Perspect. 2017, 24, 126–138. [Google Scholar] [CrossRef] [Green Version]
- Wildenbos, G.A.; Peute, L.; Jaspers, M. Aging barriers influencing mobile health usability for older adults: A literature based framework (MOLD-US). Int. J. Med. Inform. 2018, 114, 66–75. [Google Scholar] [CrossRef]
- Zhang, S.; Grenhart, W.C.M.; McLaughlin, A.C.; Allaire, J.C. Predicting computer proficiency in older adults. Comput. Human Behav. 2017, 67, 106–112. [Google Scholar] [CrossRef]
- Kaplan, G.; Baron-Epel, O. What lies behind the subjective evaluation of health status? Soc. Sci. Med. 2003, 56, 1669–1676. [Google Scholar] [CrossRef]
- Pinquart, M. Correlates of subjective health in older adults: A meta-analysis. Psychol. Aging 2001, 16, 414–426. [Google Scholar] [CrossRef]
- Haugland, S.; Wold, B.; Stevenson, J.; Aaroe, L.E.; Woynarowska, B. Subjective health complaints in adolescence A cross-national comparison of prevalence and dimensionality. Eur. J. Public Health 2001, 11, 4–10. [Google Scholar] [CrossRef]
- Baker, L.; Wagner, T.H.; Singer, S.; Kate Bundorf, M. Use of the Internet and E-mail for Health Care Information: Results from a National Survey. J. Am. Med. Assoc. 2003, 289, 2400–2406. [Google Scholar] [CrossRef] [Green Version]
- Jiang, S.; Street, R.L. Pathway Linking Internet Health Information Seeking to Better Health: A Moderated Mediation Study. Health Commun. 2017, 32, 1024–1031. [Google Scholar] [CrossRef]
- Wald, H.S.; Dube, C.E.; Anthony, D.C. Untangling the Web-The impact of Internet use on health care and the physician-patient relationship. Patient Educ. Couns. 2007, 68, 218–224. [Google Scholar] [CrossRef]
- Paccoud, I.; Baumann, M.; Le Bihan, E.; Pétré, B.; Breinbauer, M.; Böhme, P.; Chauvel, L.; Leist, A.K. Socioeconomic and Behavioural Factors Associated with Access to and Use of Patient Electronic Health Records: A Cross-Sectional Analysis of Four European Countries. Health Policy 2020. [Google Scholar] [CrossRef]
- Liu, Y.; Zhang, Y.; Ling, J.; Liu, Z. Secure and fine-grained access control on e-healthcare records in mobile cloud computing. Futur. Gener. Comput. Syst. 2018, 78, 1020–1026. [Google Scholar] [CrossRef]
- Bushelle-Edghill, J.; Lee Brown, J.; Dong, S. An examination of EHR implementation impacts on patient-flow. Health Policy Technol. 2017, 6, 114–120. [Google Scholar] [CrossRef]
- Sarkar, U.; Lyles, C. Devil in the details: Understanding the effects of providing electronic health record access to patients and families. BMJ Qual. Saf. 2020, 1–3. [Google Scholar] [CrossRef]
- Payne, R.A. Polypharmacy and deprescribing. Medicine 2020, 48, 468–471. [Google Scholar] [CrossRef]



| Characteristics of Respondents | Overall | Year of the Study | |||||||
|---|---|---|---|---|---|---|---|---|---|
(n = 3000) | 2007 (n = 1000) | 2012 (n = 1000) | 2018 (n = 1000) | ||||||
| Characteristics | Categories | n | % | n | % | n | % | n | % |
| Age | (a) 15–35 years old | 1042 | 34.7 | 407 | 40.7 | 333 | 33.3 | 302 | 30.2 |
| (b) 36–59 years old | 1257 | 41.9 | 403 | 40.3 | 425 | 42.5 | 429 | 42.9 | |
| (c) 60+ years old | 701 | 23.4 | 190 | 19 | 242 | 24.2 | 269 | 26.9 | |
| Sex | (a) male | 1402 | 46.7 | 484 | 48.4 | 476 | 47.6 | 442 | 44.2 |
| (b) female | 1598 | 53.3 | 516 | 51.6 | 524 | 52.4 | 558 | 55.8 | |
| Education | (a) primary | 693 | 34.6 | 0 | NaN * | 354 | 35.4 | 339 | 33.9 |
| (b) secondary | 741 | 37.0 | 0 | NaN * | 368 | 36.8 | 373 | 37.3 | |
| (c) higher | 566 | 28.3 | 0 | NaN * | 278 | 27.8 | 288 | 28.8 | |
| Inhabitancy | (a) alone | 281 | 14.1 | 0 | NaN * | 138 | 13.8 | 143 | 14.3 |
| (b) with someone else | 1716 | 85.9 | 0 | NaN * | 860 | 86.2 | 856 | 85.7 | |
| Residence | (a) village/rural area | 1136 | 38.0 | 372 | 37.2 | 377 | 38 | 387 | 38.7 |
| (b) small town (<100.000 residents) | 926 | 30.9 | 299 | 29.9 | 300 | 30.2 | 327 | 32.7 | |
| (c) big city (>100.000 residents) | 931 | 31.1 | 329 | 32.9 | 316 | 31.8 | 286 | 28.6 | |
| Professional situation | (a) student | 291 | 9.7 | 172 | 17.2 | 75 | 7.5 | 44 | 4.4 |
| (b) working | 1662 | 55.5 | 504 | 50.5 | 564 | 56.6 | 594 | 59.4 | |
| (c) pensioner | 868 | 29.0 | 260 | 26 | 291 | 29.2 | 317 | 31.7 | |
| (d) unemployed | 175 | 5.8 | 63 | 6.3 | 67 | 6.7 | 45 | 4.5 | |
| Frequency of | (a) everyday | 1503 | 50.2 | 414 | 41.5 | 507 | 50.9 | 582 | 58.2 |
| internet usage | (b) at least once a month | 634 | 21.2 | 216 | 21.6 | 222 | 22.3 | 196 | 19.6 |
| (c) at least once a year | 69 | 2.3 | 37 | 3.7 | 15 | 1.5 | 17 | 1.7 | |
| (d) never | 788 | 26.3 | 331 | 33.2 | 252 | 25.3 | 205 | 20.5 | |
| Frequency of health internet usage | (a) everyday (b) at least once a month | 74 1240 | 3.2 54.1 | 24 345 | 3.6 52.1 | 17 452 | 2.3 61.1 | 33 443 | 3.7 49.8 |
| (c) at least once a month | 576 | 25.1 | 147 | 22.2 | 184 | 24.9 | 245 | 27.5 | |
| (d) less than once a year | 48 | 2.1 | 0 | 0 | 0 | 0 | 48 | 5.4 | |
| (e) never | 354 | 15.4 | 146 | 22.1 | 87 | 11.8 | 121 | 13.6 | |
| Subjective health | (a) good/very good | 1737 | 58.2 | 592 | 59.4 | 575 | 57.8 | 570 | 57.5 |
| assessment | (b) average | 1036 | 34.7 | 338 | 33.9 | 351 | 35.3 | 347 | 35 |
| (c) bad/very bad | 209 | 7.0 | 66 | 6.6 | 69 | 6.9 | 74 | 7.5 | |
| Interest in access to EHRs | (a) yes | 1912 | 63.7 | 669 | 66.9 | 631 | 63.1 | 612 | 61.2 |
| (b) no | 996 | 33.2 | 291 | 29.1 | 338 | 33.8 | 367 | 36.7 | |
| (c) I do not know | 92 | 3.1 | 40 | 4 | 31 | 3.1 | 21 | 2.1 | |
| Consent to payment for access to EHRs ** | (a) yes | 920 | 48.1 | 374 | 55.9 | 290 | 46 | 256 | 41.8 |
| (b) no | 992 | 51.9 | 295 | 44.1 | 341 | 54 | 356 | 58.2 | |
| Using a cell phone | (a) yes | 1848 | 92.4 | 0 | NaN * | 891 | 89.1 | 957 | 95.7 |
| (b) no | 152 | 7.6 | 0 | NaN * | 109 | 10.9 | 43 | 4.3 | |
| Characteristics of Respondents | Interest in Access to EHRs | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| (a) yes | (b) no | (c) I don’t know | p | ||||||
| Variable | Categories | n | % | n | % | n | % | 1 − | |
| Sex | (a) male | 925 | 66 | 440 | 31.4 | 37 | 2.6 | 0.044 | |
| (b) female | 987 | 61.8 | 556 | 34.8 | 55 | 3.4 | 0.604 | ||
| Education | (a) primary | 334 | 48.2 | 334 | 48.2 | 25 | 3.6 | 0 | * |
| (b) secondary | 481 | 64.9 | 239 | 32.3 | 21 | 2.8 | 1 | ||
| (c) higher | 428 | 75.6 | 132 | 23.3 | 6 | 1.1 | |||
| Inhabitancy | (a) alone | 142 | 50.5 | 125 | 44.5 | 14 | 5 | 0 | * |
| (b) with someone else | 1100 | 64.1 | 578 | 33.7 | 38 | 2.2 | 0.992 | ||
| Residence | (a) village/rural area | 650 | 57.2 | 447 | 39.3 | 39 | 3.4 | 0 | * |
| (b) small town (<100.000 residents) | 612 | 66.1 | 290 | 31.3 | 24 | 2.6 | 1 | ||
| (c) big city (>100.000 residents) | 648 | 69.6 | 254 | 27.3 | 29 | 3.1 | |||
| Professional situation | (a) student | 229 | 78.7 | 57 | 19.6 | 5 | 1.7 | 0 | * |
| (b) working | 1175 | 70.7 | 440 | 26.5 | 47 | 2.8 | 1 | ||
| (c) pensioner | 397 | 45.7 | 438 | 50.5 | 33 | 3.8 | |||
| (d) unemployed | 109 | 62.3 | 59 | 33.7 | 7 | 4 | |||
| Frequency of internet usage | (a) everyday | 1148 | 76.4 | 326 | 21.7 | 29 | 1.9 | 0 | * |
| (b) at least once a month | 376 | 59.3 | 236 | 37.2 | 22 | 3.5 | 1 | ||
| (c) at least once a year | 44 | 63.8 | 25 | 36.2 | 0 | 0 | |||
| (d) never | 342 | 43.4 | 405 | 51.4 | 41 | 5.2 | |||
| Frequency of | (a) everyday | 58 | 78.4 | 14 | 18.9 | 2 | 2.7 | 0 | * |
| health internet usage | (b) at least once a month | 918 | 74 | 296 | 23.9 | 26 | 2.1 | 1 | |
| (c) at least once a year | 411 | 71.4 | 155 | 26.9 | 10 | 1.7 | |||
| (d) less than one a year | 30 | 62.5 | 17 | 35.4 | 1 | 2.1 | |||
| (e) never | 184 | 52 | 155 | 43.8 | 15 | 4.2 | |||
| Subjective health assessment | (a) good/very good | 1221 | 70.3 | 465 | 26.8 | 51 | 2.9 | 0 | * |
| (b) average | 585 | 56.5 | 421 | 40.6 | 30 | 2.9 | 1 | ||
| (c) bad/very bad | 97 | 46.4 | 101 | 48.3 | 11 | 5.3 | |||
| Using a cell phone | (a) yes | 1193 | 64.6 | 613 | 33.2 | 42 | 2.3 | 0 | * |
| (b) no | 50 | 32.9 | 92 | 60.5 | 10 | 6.6 | 1 | ||
| Characteristics of Respondents | Consent to Payment for Access to EHRs * | |||||
|---|---|---|---|---|---|---|
| (a) yes | (b) no | p | ||||
| Variable | Categories | n | % | n | % | 1 − |
| Sex | (a) male | 450 | 48.6 | 475 | 51.4 | 0.686 |
| (b) female | 470 | 47.6 | 517 | 52.4 | 0.069 | |
| Education | (a) primary | 148 | 44.3 | 186 | 55.7 | 0.985 |
| (b) secondary | 211 | 43.9 | 270 | 56.1 | 0.053 | |
| (c) higher | 187 | 43.7 | 241 | 56.3 | ||
| Inhabitancy | (a) alone | 55 | 38.7 | 87 | 61.3 | 0.213 |
| (b) with someone else | 491 | 44.6 | 609 | 55.4 | 0.238 | |
| Residence | (a) village/rural area | 330 | 50.8 | 320 | 49.2 | 0.15 |
| (b) small town (<100.000 residents) | 294 | 48 | 318 | 52 | 0.396 | |
| (c) big city (>100.000 residents) | 294 | 45.4 | 354 | 54.6 | ||
| Professional situation | (a) student | 100 | 43.7 | 129 | 56.3 | 0.528 |
| (b) working | 575 | 48.9 | 600 | 51.1 | 0.210 | |
| (c) pensioner | 191 | 48.1 | 206 | 51.9 | ||
| (d) unemployed | 54 | 49.5 | 55 | 50.5 | ||
| Frequency of internet usage | (a) everyday | 537 | 46.8 | 611 | 53.2 | 0.521 |
| (b) at least once a month | 191 | 50.8 | 185 | 49.2 | 0.213 | |
| (c) at least once a year | 21 | 47.7 | 23 | 52.3 | ||
| (d) never | 170 | 49.7 | 172 | 50.3 | ||
| Frequency of | (a) everyday | 30 | 51.7 | 28 | 48.3 | 0.048 |
| health internet usage | (b) at least once a month | 461 | 50.2 | 457 | 49.8 | 0.694 |
| (c) at least once a year | 174 | 42.3 | 237 | 57.7 | ||
| (d) less than one a year | 11 | 36.7 | 19 | 63.3 | ||
| (e) never | 82 | 44.6 | 102 | 55.4 | ||
| Subjective health assessment | (a) good/very good | 576 | 47.2 | 645 | 52.8 | 0.548 |
| (b) average | 292 | 49.9 | 293 | 50.1 | 0.151 | |
| (c) bad/very bad | 46 | 47.4 | 51 | 52.6 | ||
| Using a cell phone | (a) yes | 529 | 44.3 | 664 | 55.7 | 0.194 |
| (b) no | 17 | 34 | 33 | 66 | 0.196 | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bujnowska-Fedak, M.M.; Wysoczański, Ł. Access to an Electronic Health Record: A Polish National Survey. Int. J. Environ. Res. Public Health 2020, 17, 6165. https://doi.org/10.3390/ijerph17176165
Bujnowska-Fedak MM, Wysoczański Ł. Access to an Electronic Health Record: A Polish National Survey. International Journal of Environmental Research and Public Health. 2020; 17(17):6165. https://doi.org/10.3390/ijerph17176165
Chicago/Turabian StyleBujnowska-Fedak, Maria Magdalena, and Łukasz Wysoczański. 2020. "Access to an Electronic Health Record: A Polish National Survey" International Journal of Environmental Research and Public Health 17, no. 17: 6165. https://doi.org/10.3390/ijerph17176165
APA StyleBujnowska-Fedak, M. M., & Wysoczański, Ł. (2020). Access to an Electronic Health Record: A Polish National Survey. International Journal of Environmental Research and Public Health, 17(17), 6165. https://doi.org/10.3390/ijerph17176165





