Pre- and Post-Operative Nutrition Assessment in Patients with Colon Cancer Undergoing Ileostomy
Abstract
:1. Introduction
2. Method and Material
2.1. Study Population, Design, Setting, and Period of the Study
2.2. Sample: Inclusion and Exclusion Criteria
2.3. Data Collection and Procedure
2.4. Nutritional Assessment (Study Instrument)
- decrease in food intake due to loss of appetite, digestive problems, chewing or swallowing difficulties, during the last 3 months;
- involuntary weight loss, during the last 3 months;
- mobility;
- psychological stress or acute disease, during the last 3 months;
- neuropsychological problems;
- body mass index (BMI);
- independently living (not in a nursing home);
- more than 3 prescription drugs per day;
- pressure sores or skin ulcers;
- meals per day;
- consumption of two or more servings of fruits or vegetables per day;
- consumption of fluid (water, juice, coffee, tea, milk);
- mode of feeding;
- self view of nutritional status;
- self-perceived health status;
- mid-arm circumference and calf circumference.
2.5. Ethical Considerations
2.6. Statistical Analysis
3. Results
4. Discussion
5. Limitations of the Study
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Tonolini, M. A closer look at the stoma: Multimodal imaging of patients with ileostomies and colostomies. Insights Imaging 2019, 10, 41. [Google Scholar] [CrossRef]
- Nessar, G.; Wu, J.S. Evolution of continent ileostomy. World J. Gastroenterol. 2012, 18, 3479–3482. [Google Scholar] [CrossRef]
- Bafford, A.C.; Irani, J.L. Management and complications of stomas. Surg. Clin. N. Am. 2013, 93, 145–166. [Google Scholar] [CrossRef]
- Malik, T.; Lee, M.; Harikrishnan, A. The incidence of stoma related morbidity—A systematic review of randomised controlled trials. Ann. R. Coll. Surg. Engl. 2018, 100, 501–508. [Google Scholar] [CrossRef]
- Park, J.; Danielsen, A.K.; Angenete, E.; Bock, D.; Marinez, A.C.; Haglind, E.; Jansen, J.E.; Skullman, S.; Wedin, A.; Rosenberg, J. Quality of life in a randomized trial of early closure of temporary ileostomy after rectal resection for cancer (EASY trial). Br. J. Surg. 2018, 105, 244–251. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Villafranca, J.J.A.; Rodríguez, C.L.; Abilés, J.; Rivera, R.; Adán, N.G.; Utrilla, P. Protocol for the detection and nutritional management of high-output stomas. Nutr. J. 2015, 14, 45. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Berti-Hearn, L.; Elliott, B. Ileostomy Care: A Guide for Home Care Clinicians. Home Health Now 2019, 37, 136–144. [Google Scholar] [CrossRef] [PubMed]
- Hubbard, G.; Taylor, C.; Beeken, R.J.; Campbell, A.; Gracey, J.; Grimmett, C.; Fisher, A.; Ozakinci, G.; Slater, S.; Gorely, T. Research priorities about stoma-related quality of life from the perspective of people with a stoma: A pilot survey. Health Expect. 2017, 20, 1421–1427. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.J.; Kweon, M.; Park, M. Nutritional Management of a Patient with a High-Output Stoma after Extensive Small Bowel Resection to Treat Crohn’s Disease. Clin. Nutr. Res. 2019, 8, 247. [Google Scholar] [CrossRef]
- Medlin, S. Nutritional and fluid requirements: High-output stomas. Gastrointest. Nurs. 2012, 10, 42–49. [Google Scholar] [CrossRef]
- Buckman, S.A.; Heise, C.P. Nutrition considerations surrounding restorative proctocolectomy. Nutr. Clin. Pract. 2010, 25, 250–256. [Google Scholar] [CrossRef] [PubMed]
- Moraes, J.T.; Melo, A.F.F.; Araújo, C.; Faria, R.D.G.S.; Ferreira, N.R.; Belo, V.S. Anthropometric and dietetic evaluation of people with ileostomies. Arq. Gastroenterol. 2019, 56, 34–40. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nestle Nutrition Institute. Full Mini Nutritional Assessment. 2009. Available online: https://www.mna-elderly.com/forms/MNA_english.pdf (accessed on 1 July 2020).
- Vellas, B.; Villars, H.; Abellan, G.; Soto, M.E.; Rolland, Y.; Guigoz, Y.; Morley, J.E.; Chumlea, W.; Salva, A.; Rubenstein, L.Z.; et al. Overview of the MNA®—Its history and challenges. J. Nutr. Health Aging 2006, 10, 456–463. [Google Scholar]
- Tsai, A.C.; Chang, M.-Z. Long-form but not short-form Mini-Nutritional Assessment is appropriate for grading nutritional risk of patients on hemodialysis—A cross-sectional study. Int. J. Nurs. Stud. 2011, 48, 1429–1435. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, A.; Perry, R.; England, C.; Searle, A.; Atkinson, C. Dietary management in people with an ileostomy: A scoping review protocol. JBI Database Syst. Rev. Implement Rep. 2019, 17, 129–136. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Torbahn, G.; Strauß, T.; Sieber, C.; Volkert, D.; Kiesswetter, E. Use of mini nutritional assessment (MNA) in oncological patients—An evidence map. Clin. Nutr. 2018, 37, S122. [Google Scholar] [CrossRef]
- Steele, S.R.; Park, G.E.; Johnson, E.K.; Martin, M.J.; Stojadinovic, A.; Maykel, J.A.; Causey, M.W. The impact of age on colorectal cancer incidence, treatment, and outcomes in an equal-access health care system. Dis. Colon Rectum 2014, 57, 303–310. [Google Scholar] [CrossRef]
- Rao, S.A.; Haleshappa, R.A.; Garg, S.; Kuntegowdanahalli, C.L.; Kanakasetty, G.B.; Dasappa, L. Is Colorectal Cancer in Young (<40 Years) Different from those in the Elderly (>40 Years): Experience from a Regional Care Center. Indian J. Med. Paediatr. Oncol. 2017, 38, 466–470. [Google Scholar] [CrossRef]
- Weinberg, B.A.; Marshall, J.L. Colon Cancer in Young Adults: Trends and Their Implications. Curr. Oncol. Rep. 2019, 21, 3. [Google Scholar] [CrossRef]
- Kim, M.S.; Kim, H.K.; Kim, D.Y.; Kim, H. The influence of nutritional assessment on the outcome of ostomy takedown. J. Korean Soc. Coloproctol. 2012, 28, 145–151. [Google Scholar] [CrossRef] [Green Version]
- Baker, M.L.; Williams, R.N.; Nightingale, J.M.D. Causes and management of a high-output stoma. Color. Dis. 2010, 13, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Hardiman, K.M.; Reames, C.D.; McLeod, M.C.; Regenbogen, S.E. Patient autonomy-centered self-care checklist reduces hospital readmissions after ileostomy creation. Surgery 2016, 160, 1302–1308. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Olieira, A.L.; Moreira, A.P.B.; Netto, M.P.; Leite, I.C.G. A Cross-sectional Study of Nutritional Status, Diet, and Dietary Restrictions among Persons With an Ileostomy or Colostomy. Ostomy Wound Manag. 2018, 64, 18–29. [Google Scholar] [CrossRef]
- Akbulut, G. Nutrition in stoma patients: A practical view of dietary therapy. Int. J. Hematol. Oncol. 2011, 21, 62–66. [Google Scholar] [CrossRef]
- Carli, F.; Zavorsky, G.S. Optimizing functional exercise capacity in the elderly surgical population. Curr. Opin. Clin. Nutr. Metab. Care 2005, 8, 23–32. [Google Scholar] [CrossRef] [PubMed]
- West, M.; Wischmeyer, P.E.; Grocott, M. Prehabilitation and Nutritional Support to Improve Perioperative Outcomes. Curr. Anesthesiol. Rep. 2017, 7, 340–349. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Messaris, E.; Sehgal, R.; Deiling, S.; Koltun, W.A.; Stewart, D.; McKenna, K.; Poritz, L.S. Dehydration is the most common indication for readmission after diverting ileostomy creation. Dis. Colon Rectum 2012, 55, 175–180. [Google Scholar] [CrossRef]
- Kulaylat, A.N.; Dillon, P.W.; Hollenbeak, C.S.; Stewart, D.B. Determinants of 30-d readmission after colectomy. J. Surg. Res. 2015, 193, 528–535. [Google Scholar] [CrossRef]
- Migdanis, A.; Koukoulis, G.; Mamaloudis, I.; Baloyiannis, I.; Migdanis, I.; Kanaki, M.; Malissiova, E.; Tzovaras, G. Administration of an oral hydration solution prevents electrolyte and fluid disturbances and reduces readmissions in patients with a diverting ileostomy after colorectal surgery: A prospective, randomized, controlled trial. Dis. Colon Rectum 2018, 61, 840–846. [Google Scholar] [CrossRef]
- Kandagatla, P.; Nikolian, V.C.; Matusko, N.; Mason, S.; Regenbogen, S.E.; Hardiman, K.M. Patient-Reported Outcomes and Readmission after Ileostomy Creation in Older Adults. Am. Surg. 2018, 84, 1814–1818. [Google Scholar] [CrossRef]
- Ang, S.G.M.; Chen, H.-C.; Siah, C.-J.R.; He, H.-G.; Klainin-Yobas, P. Stressors relating to patient psychological health following stoma surgery: An integrated literature review. Oncol. Nurs. Forum 2013, 40, 587–594. [Google Scholar] [CrossRef] [PubMed]
- Reinwalds, M.; Blixter, A.; Carlsson, E. A Descriptive, Qualitative Study to Assess Patient Experiences Following Stoma Reversal After Rectal Cancer Surgery. Ostomy Wound Manag. 2017, 63, 29–37. [Google Scholar]
- Danielsen, A.K.; Burcharth, J.; Rosenberg, J. Spouses of patients with a stoma lack information and support and are restricted in their social and sexual life: A systematic review. Int. J. Color. Dis. 2013, 28, 1603–1612. [Google Scholar] [CrossRef] [PubMed]
| Demographic characteristics | Median (IQR) |
|---|---|
| Age | 62 (52.5–71) |
| Height (cm) | 168.0 (164.5–173.0) |
| Weight | 75.0 (66.5–83.5) |
| Body Mass Index BMI (kg/m2) | 23.1 (16.7–29.9) |
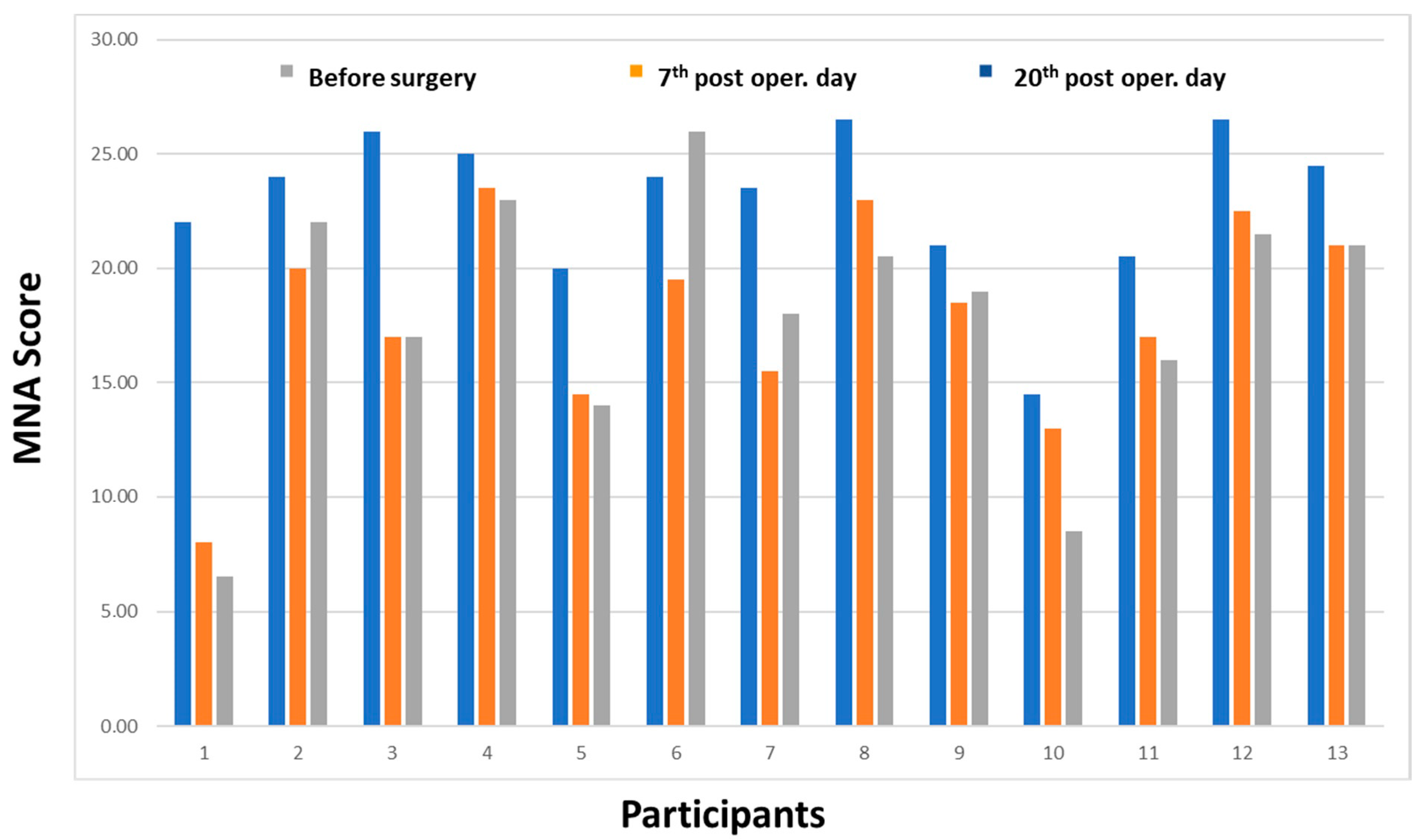
| MNA Score | Median (IQR) |
|---|---|
| Mini Nutritional Assessment, pre-surgery (time 0) | 24 (20.7–25.5) |
| Mini Nutritional Assessment, 7th post surgery (time 1) | 18.5 (15–21.7) |
| Mini Nutritional Assessment, 20th post surgery (time 2) | 19.0 (15.0–21.7) |
| Variables | MNA Pre-Operatively | MNA 7th Post-Operatively | MNA 20th Post-Operatively | p Value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Decrease in food intake | Severe | Moderate | No | Severe | Moderate | No | Severe | Moderate | No | |
| 7.7 | 46.2 | 46.2 | 7.7 | 46.2 | 46.2 | 15.4 | 38.5 | 46.2 | 0.250 | |
| Weight loss | >3 kg | 1–3 kg | No | >3 kg | 1–3 kg | No | >3 kg | 1–3 kg | No | |
| 38.5 | 23.1 | 38.5 | 46.2 | 15.4 | 38.5 | 53.8 | 15.4 | 30.8 | 0.012 | |
| Mobility | Bad | Able | Goes out | Bad | Able | Goes out | Bad | Able | Goes out | |
| 7.7 | 92.3 | 7.7 | 15.4 | 76.9 | 7.7 | 23.1 | 69.2 | 0.023 | ||
| Stress | Yes | No | Yes | No | Yes | No | ||||
| 38.5 | 61.5 | 46.2 | 53.8 | 46.2 | 53.8 | 0.366 | ||||
| Neuropsychological problems | Severe | Mild | No | Severe | Mild | No | Severe | Mild | No | |
| 7.7 | 92.3 | 7.7 | 92.3 | 7.7 | 92.3 | 0.224 | ||||
| BMI kg/m2 | <19 | 19–23 | >23 | <19 | 19–23 | >23 | <19 | 19–23 | >23 | |
| 15.4 | 84.6 | 38.5 | 61.5 | 7.7 | 61.5 | 30.8 | 0.011 | |||
| Independently life | Yes | No | Yes | No | Yes | No | ||||
| 23.1 | 76.9 | 100 | 38.5 | 61.5 | 0.123 | |||||
| >3 pills/per day | Yes | No | Yes | No | Yes | No | ||||
| 30.8 | 69.2 | 30.8 | 69.2 | 38.5 | 61.5 | 0.213 | ||||
| Pressure or skin ulcers | Yes | No | Yes | No | Yes | No | ||||
| 100 | 15.4 | 84.6 | 15.4 | 84.6 | 0.111 | |||||
| Full meals | 1 | 2 | 3 | 1 | 2 | 3 | 1 | 2 | 3 | |
| 7.7 | 84.6 | 7.7 | 38.5 | 46.2 | 15.4 | 30.8 | 69.2 | 0.023 | ||
| >2 consumption fruit -vegetables | Yes | No | Yes | No | Yes | No | ||||
| 30.8 | 69.2. | 100 | 100 | 0.007 | ||||||
| Fluid consumption | >5 | 3–5 | <3 | >5 | 3–5 | <3 | >5 | 3–5 | <3 | |
| 69.2 | 30.8 | 15.4 | 46.2 | 38.5 | 53.8 | 38.5 | 7.7 | 0.024 | ||
| Mode of feeding | Unable | Difficulty | No | Unable | Difficulty | No | Unable | Difficulty | No | |
| 100 | 7.7 | 38.5 | 53.8 | 7.7 | 92.3 | |||||
| Arm circumference | <21 | 21–22 | >22 | <21 | 21–22 | >22 | <21 | 21–22 | >22 | |
| 100 | 7.7 | 7.7 | 84.6 | 23.1 | 38.5 | 38.5 | 0.002 | |||
| Calf circumference | <31 cm | >31 cm | <31 cm | >31 cm | <31 cm | >31 cm | ||||
| 100 | 7.7 | 92.3 | 30.8 | 69.2 | 0.003 | |||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vasilopoulos, G.; Makrigianni, P.; Polikandrioti, M.; Tsiampouris, I.; Karayiannis, D.; Margari, N.; Avramopoulou, L.; Toulia, G.; Fasoi, G. Pre- and Post-Operative Nutrition Assessment in Patients with Colon Cancer Undergoing Ileostomy. Int. J. Environ. Res. Public Health 2020, 17, 6124. https://doi.org/10.3390/ijerph17176124
Vasilopoulos G, Makrigianni P, Polikandrioti M, Tsiampouris I, Karayiannis D, Margari N, Avramopoulou L, Toulia G, Fasoi G. Pre- and Post-Operative Nutrition Assessment in Patients with Colon Cancer Undergoing Ileostomy. International Journal of Environmental Research and Public Health. 2020; 17(17):6124. https://doi.org/10.3390/ijerph17176124
Chicago/Turabian StyleVasilopoulos, Georgios, Panagiota Makrigianni, Maria Polikandrioti, Ilias Tsiampouris, Dimitrios Karayiannis, Nikoletta Margari, Lamprini Avramopoulou, Georgia Toulia, and Georgia Fasoi. 2020. "Pre- and Post-Operative Nutrition Assessment in Patients with Colon Cancer Undergoing Ileostomy" International Journal of Environmental Research and Public Health 17, no. 17: 6124. https://doi.org/10.3390/ijerph17176124
APA StyleVasilopoulos, G., Makrigianni, P., Polikandrioti, M., Tsiampouris, I., Karayiannis, D., Margari, N., Avramopoulou, L., Toulia, G., & Fasoi, G. (2020). Pre- and Post-Operative Nutrition Assessment in Patients with Colon Cancer Undergoing Ileostomy. International Journal of Environmental Research and Public Health, 17(17), 6124. https://doi.org/10.3390/ijerph17176124





