Strategies for Referring Cancer Patients in a Smoking Cessation Program
Abstract
1. Introduction
1.1. Smoking Cessation in People with Cancer
1.2. Specialized Smoking Cessation Treatment for People with Cancer
1.3. Patient Engagement in Smoking Cessation Services
2. Materials and Methods
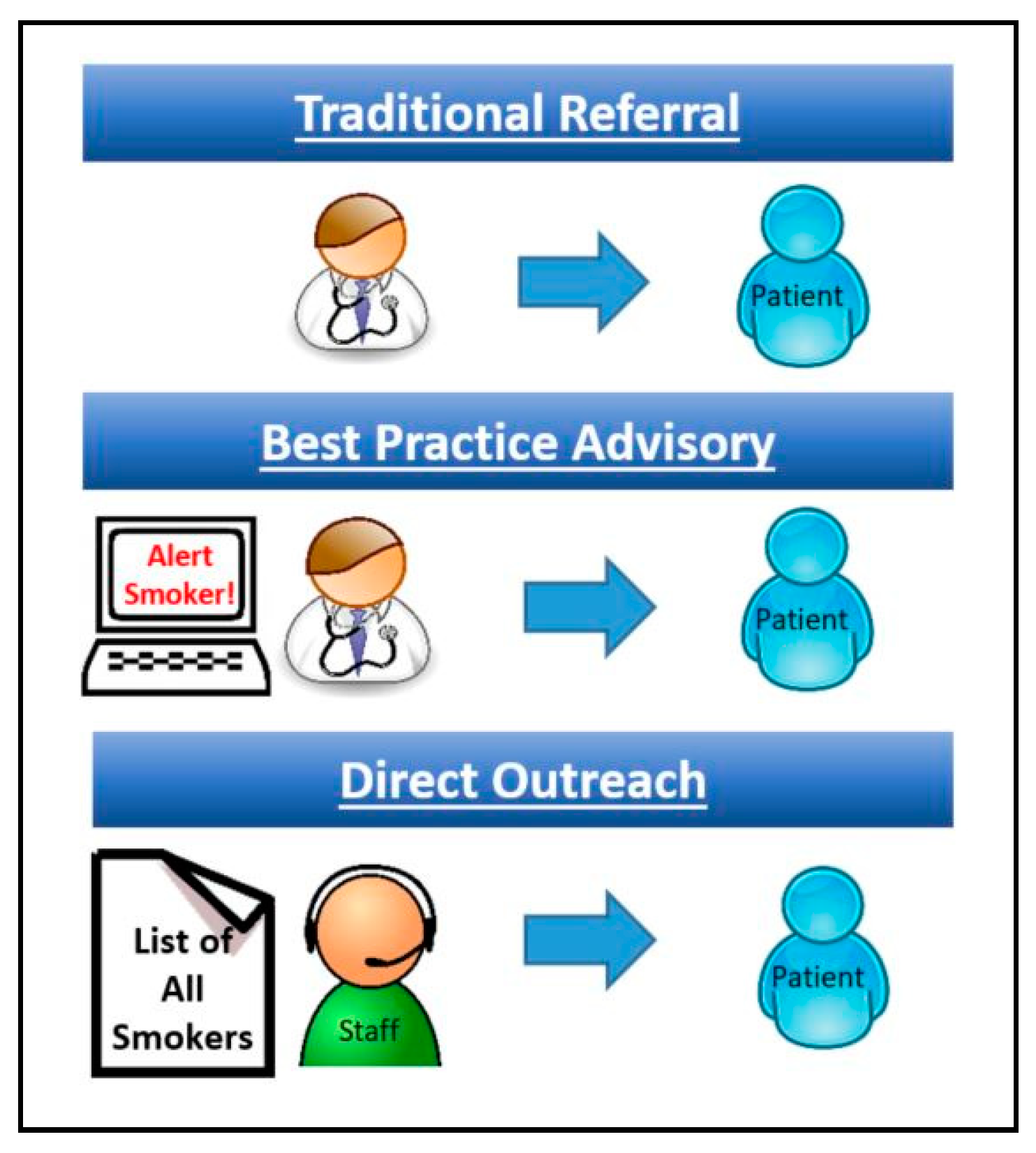
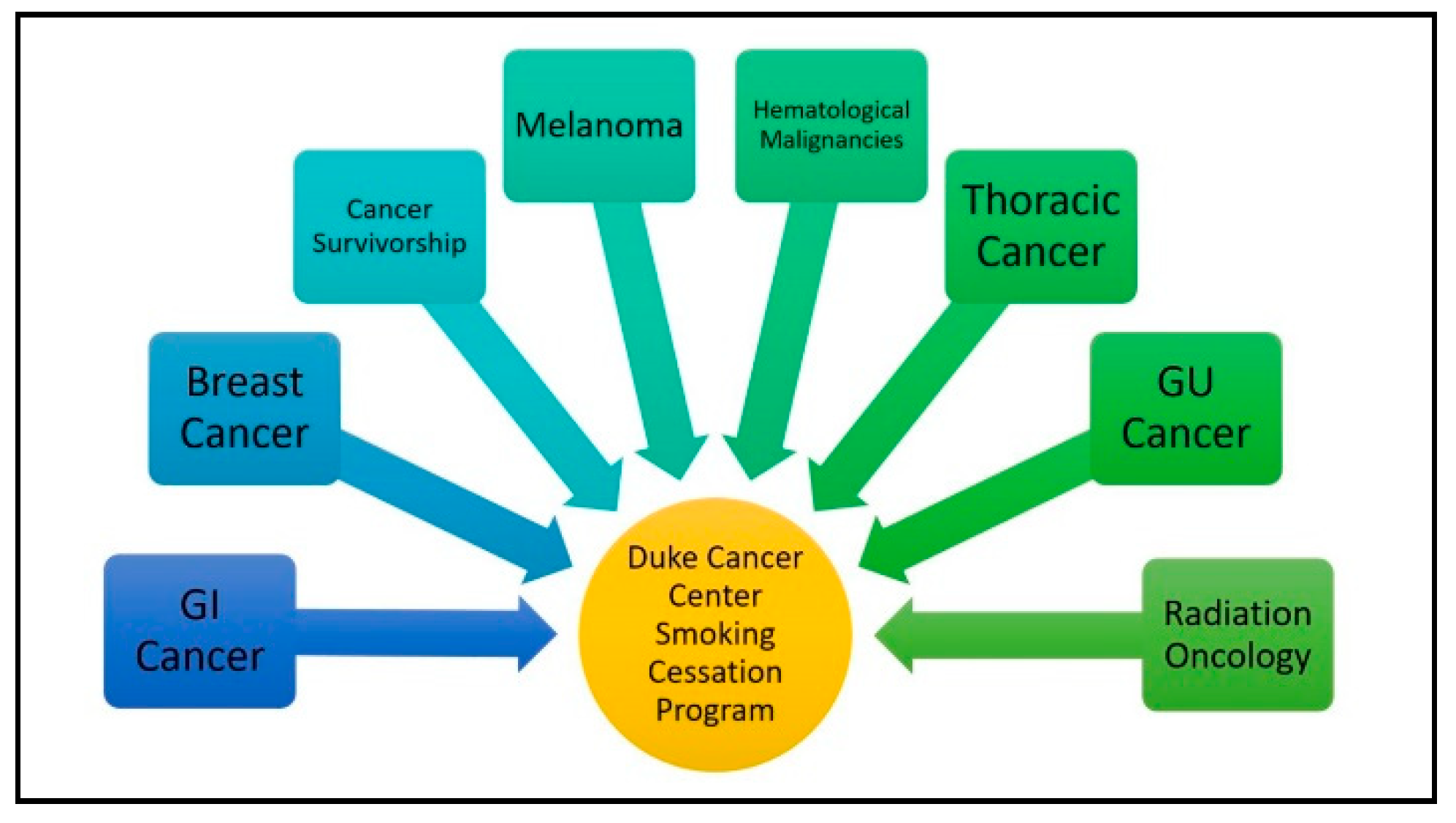
2.1. Program Referral
2.2. Program Utilization
2.3. Traditional Referral
2.4. Best Practice Advisory
2.5. Direct Outreach
2.6. Data Collection and Analysis
2.6.1. Population-Based Tobacco Use
2.6.2. Referral Database
3. Results
3.1. Demographics
3.2. 12-Month Program Referral and Utilization
3.3. 30-Day Pilot Test—Program Referral and Utilization
3.4. Smoking Outcomes
4. Discussion
4.1. Main Findings
4.2. Low Referral and Utilization Rates
4.3. Traditional Referral within a Cancer Center
4.4. Best Practice Advisory (BPA)
4.5. Direct Outreach
4.6. Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Lortet-Tieulent, J.; Sauer, A.G.; Siegel, R.L.; Miller, K.D.; Islami, F.; Fedewa, S.A.; Jacobs, E.J.; Jemal, A. State-Level Cancer Mortality Attributable to Cigarette Smoking in the United States. JAMA Intern. Med. 2016, 176, 1792–1798. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Smoking Cessation: A Report of the Surgeon General; US Department of Health and Human Services: Atlanta, GA, USA, 2020; p. 700.
- Khuder, S.A.; Mutgi, A.B. Effect of smoking cessation on major histologic types of lung cancer. Chest 2001, 120, 1577–1583. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ferketich, A.K.; Niland, J.C.; Mamet, R.; Zornosa, C.; D’Amico, T.A.; Ettinger, D.S.; Kalemkerian, G.P.; Pisters, K.M.; Reid, M.E.; Otterson, G.A. Smoking status and survival in the national comprehensive cancer network non–small cell lung cancer cohort. Cancer 2013, 119, 847–853. [Google Scholar] [CrossRef] [PubMed]
- Gillison, M.L.; Zhang, Q.; Jordan, R.; Xiao, W.; Westra, W.H.; Trotti, A.; Spencer, S.; Harris, J.; Chung, C.H.; Ang, K.K. Tobacco Smoking and Increased Risk of Death and Progression for Patients With p16-Positive and p16-Negative Oropharyngeal Cancer. J. Clin. Oncol. 2012, 30, 2102–2111. [Google Scholar] [CrossRef]
- Tezel, Y.B.; Akyil, M.; Tezel, C.; Akyil, F.T.; Evman, S.; Gurer, D.; Baysungur, V.; Yalcinkaya, I. Impact of persistence of smoking on recurrence after early stage lung surgery. Eur. Respir. J. 2016, 48, PA4339. [Google Scholar] [CrossRef]
- Toll, B.A.; Brandon, T.H.; Gritz, E.R.; Warren, G.W.; Herbst, R.S. AACR Subcommittee on Tobacco and Cancer Assessing tobacco use by cancer patients and facilitating cessation: An American Association for Cancer Research policy statement. Clin. Cancer Res. 2013, 19, 1941–1948. [Google Scholar] [CrossRef]
- van Osch Frits, H.M.; Jochems Sylvia, H.J.; van Schooten Frederik, J.; Bryan Richard, T.; Zeegers Maurice, P. Significant Role of Lifetime Cigarette Smoking in Worsening Bladder Cancer and Upper Tract Urothelial Carcinoma Prognosis: A Meta-Analysis. J. Urol. 2016, 195, 872–879. [Google Scholar] [CrossRef]
- Praud, D.; Rota, M.; Pelucchi, C.; Bertuccio, P.; Rosso, T.; Galeone, C.; Zhang, Z.-F.; Matsuo, K.; Ito, H.; Hu, J.; et al. Cigarette smoking and gastric cancer in the Stomach Cancer Pooling (StoP) Project. Eur. J. Cancer Prev. 2018, 27, 124–133. [Google Scholar] [CrossRef]
- Sørensen, L.T. Wound healing and infection in surgery. The clinical impact of smoking and smoking cessation: A systematic review and meta-analysis. Arch. Surg. 2012, 147, 373–383. [Google Scholar] [CrossRef]
- Mills, E.; Eyawo, O.; Lockhart, I.; Kelly, S.; Wu, P.; Ebbert, J.O. Smoking cessation reduces postoperative complications: A systematic review and meta-analysis. Am. J. Med. 2011, 124, 144–154.e8. [Google Scholar] [CrossRef]
- Dresler, C.; Warren, G.W.; Arenberg, D.; Yang, P.; Steliga, M.A.; Cummings, K.M.; Stone, E.; Jassem, J. “Teachable Moment” Interventions in Lung Cancer: Why Action Matters. J. Thorac. Oncol. 2018, 13, 603–605. [Google Scholar] [CrossRef]
- Tseng, T.S.; Lin, H.Y.; Moody-Thomas, S.; Martin, M.; Chen, T. Who tended to continue smoking after cancer diagnosis: The national health and nutrition examination survey 1999–2008. BMC Public Health 2012, 12, 784. [Google Scholar] [CrossRef] [PubMed]
- Burke, L.; Miller, L.-A.; Saad, A.; Abraham, J. Smoking Behaviors Among Cancer Survivors: An Observational Clinical Study. J. Oncol Pract. 2009, 5, 6–9. [Google Scholar] [CrossRef] [PubMed]
- Warren, G.W.; Marshall, J.R.; Cummings, K.M.; Toll, B.A.; Gritz, E.R.; Hutson, A.; Dibaj, S.; Herbst, R.; Mulshine, J.L.; Hanna, N.; et al. Addressing tobacco use in patients with cancer: A survey of American Society of Clinical Oncology members. J. Oncol. Pract. 2013, 9, 258–262. [Google Scholar] [CrossRef] [PubMed]
- Wells, M.; Aitchison, P.; Harris, F.; Ozakinci, G.; Radley, A.; Bauld, L.; Entwistle, V.; Munro, A.; Haw, S.; Culbard, B.; et al. Barriers and facilitators to smoking cessation in a cancer context: A qualitative study of patient, family and professional views. BMC Cancer 2017, 17, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Cinciripini, P.M.; Karam-Hage, M.; Kypriotakis, G.; Robinson, J.D.; Rabius, V.; Beneventi, D.; Minnix, J.A.; Blalock, J.A. Association of a comprehensive smoking cessation program with smoking abstinence among patients with cancer. JAMA Netw. Open 2019, 2, e1912251. [Google Scholar] [CrossRef]
- Morgan, G.; Schnoll, R.A.; Alfano, C.M.; Evans, S.E.; Goldstein, A.; Ostroff, J.; Park, E.R.; Sarna, L.; Cox, L.S. National Cancer Institute conference on treating tobacco dependence at cancer centers. J. Oncol. Pract. 2011, 7, 178–182. [Google Scholar] [CrossRef]
- Cahill, K.; Stevens, S.; Perera, R.; Lancaster, T. Pharmacological interventions for smoking cessation: An overview and network meta-analysis. Cochrane Database Syst. Rev. 2013, 5. [Google Scholar] [CrossRef]
- Lancaster, T.; Stead, L. Does Individually-Delivered Counselling Help People to Stop Smoking? Available online: https://www.cochrane.org/CD001292/TOBACCO_does-individually-delivered-counselling-help-people-stop-smoking (accessed on 1 May 2019).
- Stead, C.A.; Lancaster, T. Do Group-based Smoking Cessation Programmes Help People to Stop Smoking? Available online: https://www.cochrane.org/CD001007/TOBACCO_do-group-based-smoking-cessation-programmes-help-people-stop-smoking (accessed on 1 May 2019).
- Center for Disease Control and Prevention. Best Practices for Comprehensive Tobacco Control Programs—2014; US Department of Health and Human Services: Atlanta, GA, USA, 2014.
- Curry, S.J.; Keller, P.A.; Orleans, C.T.; Fiore, M.C. The role of health care systems in increased tobacco cessation. Annu. Rev. Public Health 2008, 29, 411–428. [Google Scholar] [CrossRef]
- Shields, P.G.; Herbst, R.S.; Arenberg, D.; Benowitz, N.L.; Bierut, L.; Luckart, J.B.; Cinciripini, P.; Collins, B.; David, S.; Davis, J.; et al. Smoking cessation, version 1.2016, NCCN clinical practice guidelines in oncology. J. Natl. Compr. Cancer Netw. 2016, 14, 1430–1468. [Google Scholar] [CrossRef]
- D’Angelo, H.; Rolland, B.; Adsit, R.; Baker, T.B.; Rosenblum, M.; Pauk, D.; Morgan, G.D.; Fiore, M.C. Tobacco Treatment Program Implementation at NCI Cancer Centers: Progress of the NCI Cancer Moonshot-Funded Cancer Center Cessation Initiative. Cancer Prev. Res. 2019, 12, 735–740. [Google Scholar] [CrossRef]
- Council for Tobacco Treatment Training Programs. Available online: https://ctttp.org/accredited-programs/ (accessed on 18 August 2020).
- Slattery, C.; Freund, M.; Gillham, K.; Knight, J.; Wolfenden, L.; Bisquera, A.; Wiggers, J. Increasing smoking cessation care across a network of hospitals: An implementation study. Implement Sci. 2016, 11, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Karam-Hage, M.; Oughli, H.A.; Rabius, V.; Beneventi, D.; Wippold, R.C.; Blalock, J.A.; Cinciripini, P.M. Tobacco cessation treatment pathways for cancer patients: 10 Years in the making models for smoking cessation practice. J. Natl. Compr. Cancer Netw. 2016, 14, 1469–1477. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hays, J.T.; Croghan, I.T.; Schroeder, D.R.; Burke, M.V.; Ebbert, J.O.; McFadden, D.D.; Hurt, R.D. Residential treatment compared with outpatient treatment for tobacco use and dependence. Mayo Clin. Proc. 2011, 86, 203–209. [Google Scholar] [CrossRef]
- Hughes, J.R.; Keely, J.; Naud, S. Shape of the relapse curve and long-term abstinence among untreated smokers. Addiction 2004, 99, 29–38. [Google Scholar] [CrossRef]
- Nett, L.M. The physician’s role in smoking cessation. A present and future agenda. Chest 1990, 97, 28S–32S. [Google Scholar] [CrossRef]
- Bains, M.; Britton, J.; Marsh, J.; Jayes, L.; Murray, R.L. Patients’ and healthcare professionals’ views on a specialist smoking cessation service delivered in a United Kingdom hospital: A qualitative study. Tob. Induc. Dis. 2014, 12, 2. [Google Scholar] [CrossRef]
- Lurio, J.; Morrison, F.P.; Pichardo, M.; Berg, R.; Buck, M.D.; Wu, W.; Kitson, K.; Mostashari, F.; Calman, N. Using electronic health record alerts to provide public health situational awareness to clinicians. J. Am. Med. Inf. Assoc. 2010, 17, 217–219. [Google Scholar] [CrossRef]
- Ancker, J.S.; Edwards, A.; Nosal, S.; Hauser, D.; Mauer, E.; Kaushal, R. Effects of workload, work complexity, and repeated alerts on alert fatigue in a clinical decision support system. BMC Med. Inf. Decis. Mak. 2017, 17, 36. [Google Scholar] [CrossRef]
- Faseru, B.; Ellerbeck, E.F.; Catley, D.; Gajewski, B.J.; Scheuermann, T.S.; Shireman, T.I.; Mussulman, L.M.; Nazir, N.; Bush, T.; Richter, K.P. Changing the default for tobacco-cessation treatment in an inpatient setting: Study protocol of a randomized controlled trial. Trials 2017, 18, 379. [Google Scholar] [CrossRef]
- Nolan, M.; Ridgeway, J.L.; Ghosh, K.; Martin, D.; Warner, D.O. Design, implementation, and evaluation of an intervention to improve referral to smoking cessation services in breast cancer patients. Support Care Cancer 2019, 27, 2153–2158. [Google Scholar] [CrossRef] [PubMed]
- Haas, J.S.; Linder, J.A.; Park, E.R.; Gonzalez, I.; Rigotti, N.A.; Klinger, E.V.; Kontos, E.Z.; Zaslavsky, A.M.; Brawarsky, P.; Marinacci, L.X.; et al. Proactive tobacco cessation outreach to smokers of low socioeconomic status: A randomized clinical trial. JAMA Intern. Med. 2015, 175, 218–226. [Google Scholar] [CrossRef] [PubMed]
- Giuliani, M.E.; Liu, G.; Xu, W.; Dirlea, M.; Selby, P.; Papadakos, J.; Abdelmutti, N.; Yang, D.; Eng, L.; Goldstein, D.P.; et al. Implementation of a Novel Electronic Patient-Directed Smoking Cessation Platform for Cancer Patients: Interrupted Time Series Analysis. J. Med. Internet Res. 2019, 21, e11735. [Google Scholar] [CrossRef] [PubMed]
- NC Department of Health and Human Services QuitlineNC.com. Available online: https://www.quitlinenc.com/ (accessed on 24 January 2020).
- Cropsey, K.L.; Trent, L.R.; Clark, C.B.; Stevens, E.N.; Lahti, A.C.; Hendricks, P.S. How low should you go? Determining the optimal cutoff for exhaled carbon monoxide to confirm smoking abstinence when using cotinine as reference. Nicot. Tob. Res. 2014, 16, 1348–1355. [Google Scholar] [CrossRef] [PubMed]
- Prochaska, J.O. A stage paradigm for integrating clinical and public health approaches to smoking cessation. Addict. Behav. 1996, 21, 721–732. [Google Scholar] [CrossRef]
- Campbell, S.; Bohanna, I.; Swinbourne, A.; Cadet-James, Y.; McKeown, D.; McDermott, R. Stages of change, smoking behaviour and readiness to quit in a large sample of indigenous Australians living in eight remote north Queensland communities. Int. J. Environ. Res. Public Health 2013, 10, 1562–1571. [Google Scholar] [CrossRef] [PubMed]
- Glantz, S.; Kroon, L.; Prochaska, J.; Schroeder, S. Smoking Cessation: Theory and Practice of Behavior Change (Lecture). Available online: https://medschool.ucla.edu/workfiles/Site-System/Teaching-Materials/53-Smoking-Cessation-LEC-2007.pdf (accessed on 19 August 2020).
- Etter, J.-F.; Sutton, S. Assessing “stage of change” in current and former smokers. Addiction 2002, 97, 1171–1182. [Google Scholar] [CrossRef]
- Chaiton, M.; Diemert, L.; Cohen, J.E.; Bondy, S.J.; Selby, P.; Philipneri, A.; Schwartz, R. Estimating the number of quit attempts it takes to quit smoking successfully in a longitudinal cohort of smokers. BMJ Open 2016, 6, e011045. [Google Scholar] [CrossRef]
- Patel, K.K.; Jones, P.G.; Ellerbeck, E.F.; Buchanan, D.M.; Chan, P.S.; Pacheco, C.M.; Moneta, G.; Spertus, J.A.; Smolderen, K.G. Underutilization of evidence-based smoking cessation support strategies despite high smoking dddiction burden in peripheral artery disease specialty care: Insights from the International PORTRAIT registry. J. Am. Heart Assoc. 2018, 7, e010076. [Google Scholar] [CrossRef]
- Robinson, J.; McEwen, A.; Heah, R.; Papadakis, S. A ‘Cut-Down-To-Stop’ intervention for smokers who find it hard to quit: A qualitative evaluation. BMC Public Health 2019, 19, 403. [Google Scholar] [CrossRef]
- Keto, J.; Jokelainen, J.; Timonen, M.; Linden, K.; Ylisaukko-oja, T. Physicians discuss the risks of smoking with their patients, but seldom offer practical cessation support. Subst. Abus. Treat. Prev. Policy 2015, 10, 43. [Google Scholar] [CrossRef][Green Version]
- National Institute of Health Frequently Asked Questions–Smokefree Text. Available online: https://smokefree.gov/tools-tips/text-programs/faqs (accessed on 24 January 2020).
- Vilardaga, R.; Rizo, J.; Zeng, E.; Kientz, J.A.; Ries, R.; Otis, C.; Hernandez, K. User-centered design of learn to quit, a smoking cessation smartphone app for people with serious mental illness. JMIR Serious Games 2018, 6, e2. [Google Scholar] [CrossRef] [PubMed]
- Davis, J.M.; Manley, A.R.; Goldberg, S.B.; Stankevitz, K.A.; Smith, S.S. Mindfulness training for smokers via web-based video instruction with phone support: A prospective observational study. BMC Complement. Altern. Med. 2015, 15, 95. [Google Scholar] [CrossRef] [PubMed]
- Kane-Gill, S.L.; O’Connor, M.F.; Rothschild, J.M.; Selby, N.M.; McLean, B.; Bonafide, C.P.; Cvach, M.M.; Hu, X.; Konkani, A.; Pelter, M.M. Technologic Distractions (Part 1): Summary of approaches to manage alert quantity with intent to reduce alert fatigue and suggestions for alert fatigue metrics. Crit. Care Med. 2017, 45, 1481–1488. [Google Scholar] [CrossRef] [PubMed]
- Drahnak, D.M. An observational study of the effects of a clinical nurse specialist quality improvement project for clinical reminders for sepsis on patient outcomes and nurse actions. J. Emerg. Crit. Care Med. 2018, 2, 99. [Google Scholar] [CrossRef]
- Schechter-Perkins, E.M.; Miller, N.S.; Hall, J.; Hartman, J.J.; Dorfman, D.H.; Andry, C.; Linas, B.P. Implementation and Preliminary Results of an Emergency Department Nontargeted, Opt-out Hepatitis C Virus Screening Program. Acad. Emerg. Med. 2018, 25, 1216–1226. [Google Scholar] [CrossRef]
- Rigotti, N.A.; Chang, Y.; Rosenfeld, L.C.; Japuntich, S.J.; Park, E.R.; Tindle, H.A.; Levy, D.E.; Reid, Z.Z.; Streck, J.; Gomperts, T.; et al. Interactive voice response calls to promote smoking cessation after hospital discharge: Pooled analysis of two randomized clinical trials. J. Gen. Intern. Med. 2017, 32, 1005–1013. [Google Scholar] [CrossRef]
- Scott-Sheldon, L.A.J.; Lantini, R.; Jennings, E.G.; Thind, H.; Rosen, R.K.; Salmoirago-Blotcher, E.; Bock, B.C. Text Messaging-Based Interventions for Smoking Cessation: A Systematic Review and Meta-Analysis. JMIR Mhealth Uhealth 2016, 4, e49. [Google Scholar] [CrossRef]
- Ralston, J.D.; Rutter, C.M.; Carrell, D.; Hecht, J.; Rubanowice, D.; Simon, G.E. Patient Use of Secure Electronic Messaging Within a Shared Medical Record: A Cross-sectional Study. J. Gen. Intern. Med. 2009, 24, 349–355. [Google Scholar] [CrossRef]

© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Davis, J.M.; Thomas, L.C.; Dirkes, J.E.H.; Swartzwelder, H.S. Strategies for Referring Cancer Patients in a Smoking Cessation Program. Int. J. Environ. Res. Public Health 2020, 17, 6089. https://doi.org/10.3390/ijerph17176089
Davis JM, Thomas LC, Dirkes JEH, Swartzwelder HS. Strategies for Referring Cancer Patients in a Smoking Cessation Program. International Journal of Environmental Research and Public Health. 2020; 17(17):6089. https://doi.org/10.3390/ijerph17176089
Chicago/Turabian StyleDavis, James M., Leah C. Thomas, Jillian E. H. Dirkes, and H. Scott Swartzwelder. 2020. "Strategies for Referring Cancer Patients in a Smoking Cessation Program" International Journal of Environmental Research and Public Health 17, no. 17: 6089. https://doi.org/10.3390/ijerph17176089
APA StyleDavis, J. M., Thomas, L. C., Dirkes, J. E. H., & Swartzwelder, H. S. (2020). Strategies for Referring Cancer Patients in a Smoking Cessation Program. International Journal of Environmental Research and Public Health, 17(17), 6089. https://doi.org/10.3390/ijerph17176089




