A Multi-Site Study of Traumatic Brain Injury in Mexico and Colombia: Longitudinal Mediational and Cross-Lagged Models of Family Dynamics, Coping, and Health-Related Quality of Life
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Measures
2.2.1. Short Form Health Survey (SF-36)
2.2.2. Sense of Coherence Scale (SOC-13)
2.2.3. Family Assessment Device (FAD)
2.3. Procedure
2.4. Data Analysis Plan
2.4.1. Preliminary Analyses
2.4.2. Primary Analyses
3. Results
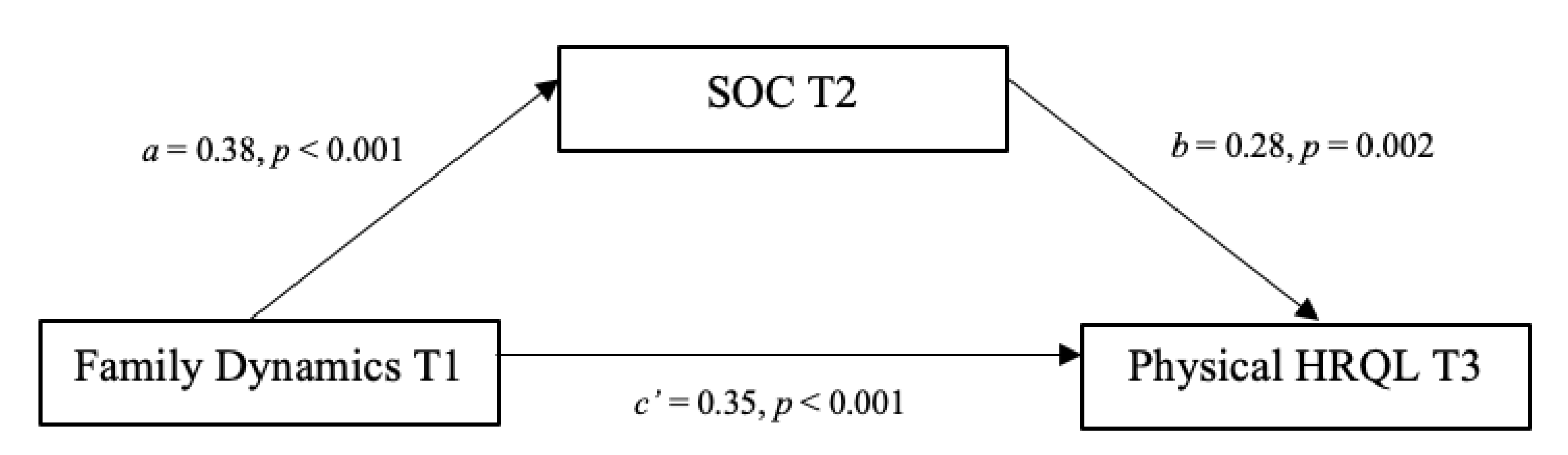
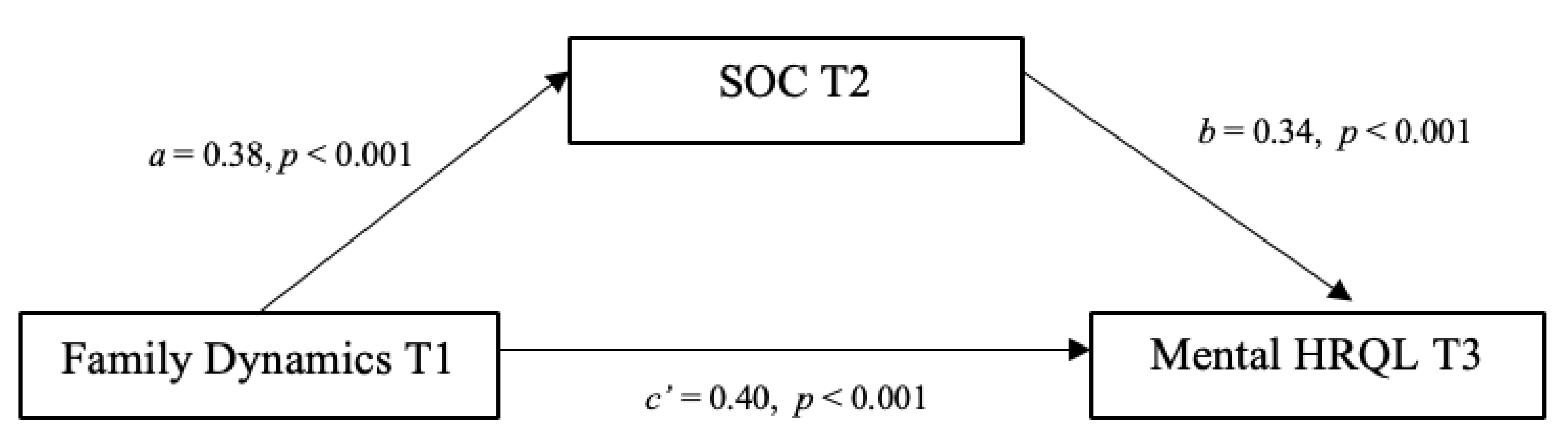
3.1. Mediations
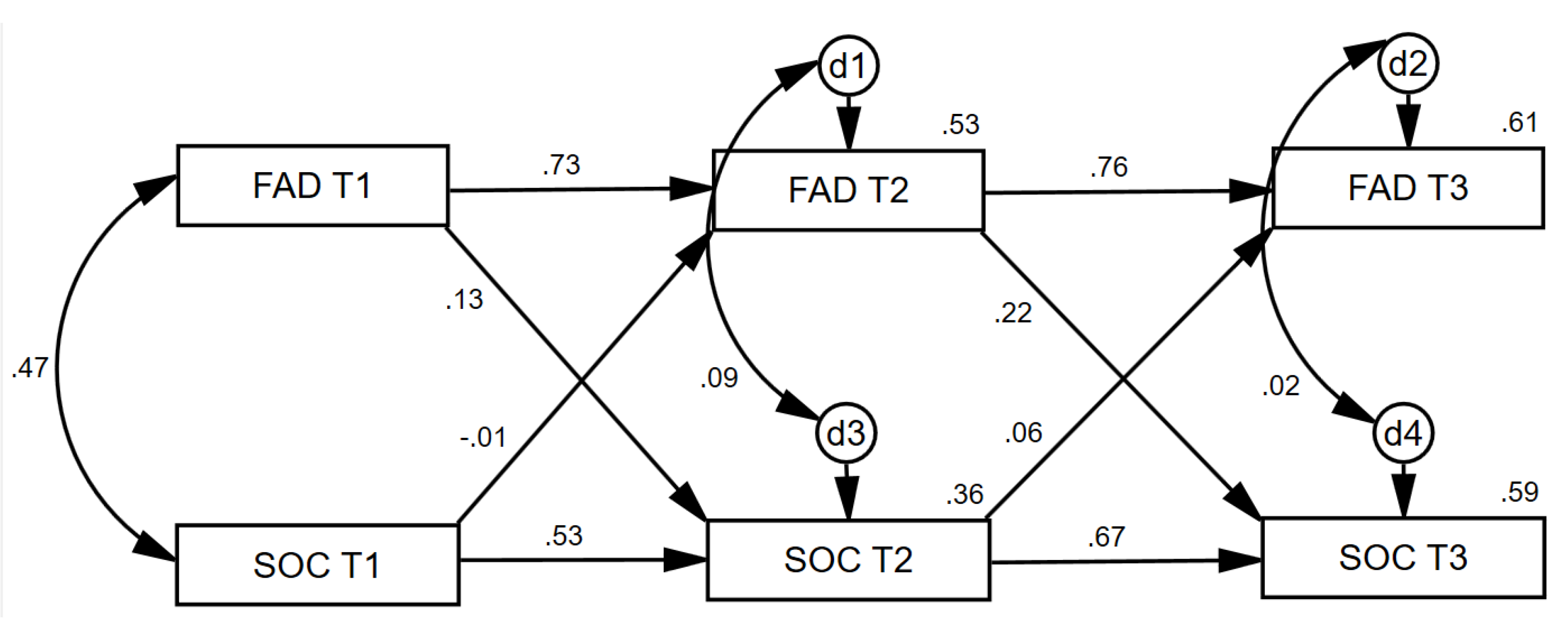
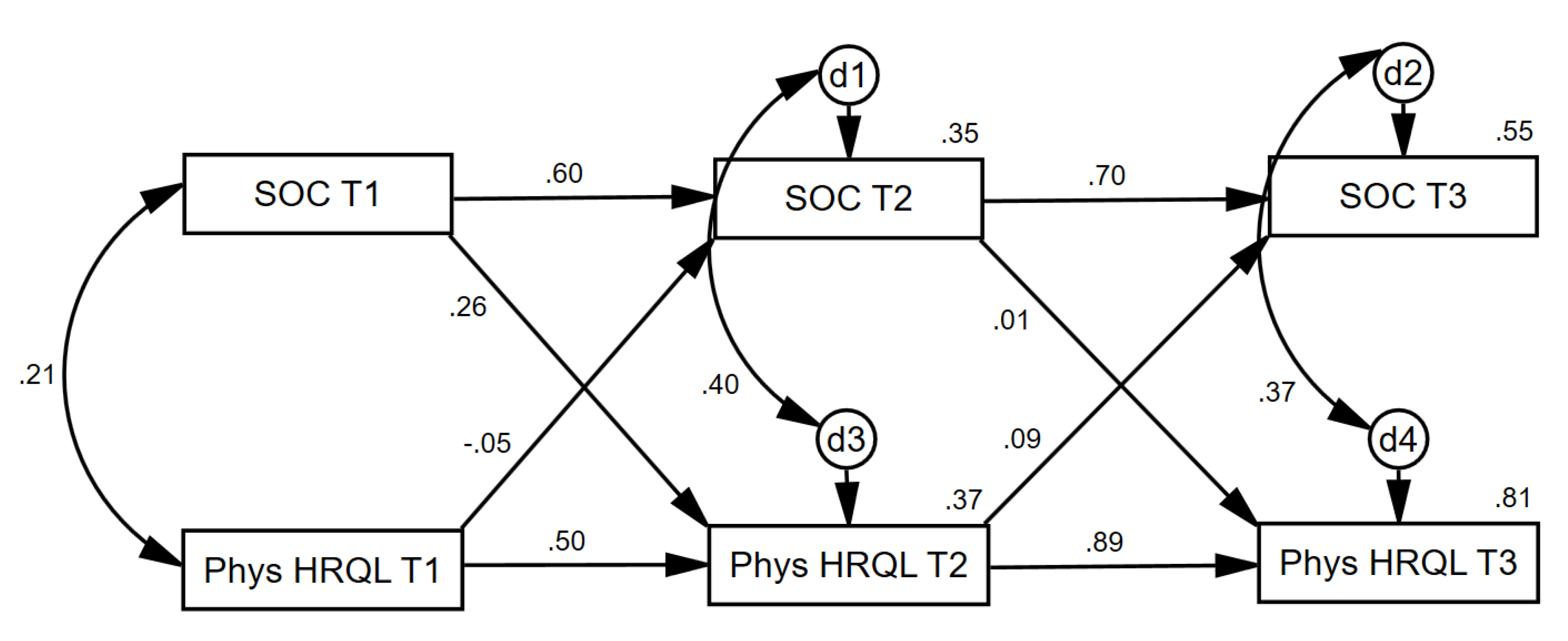
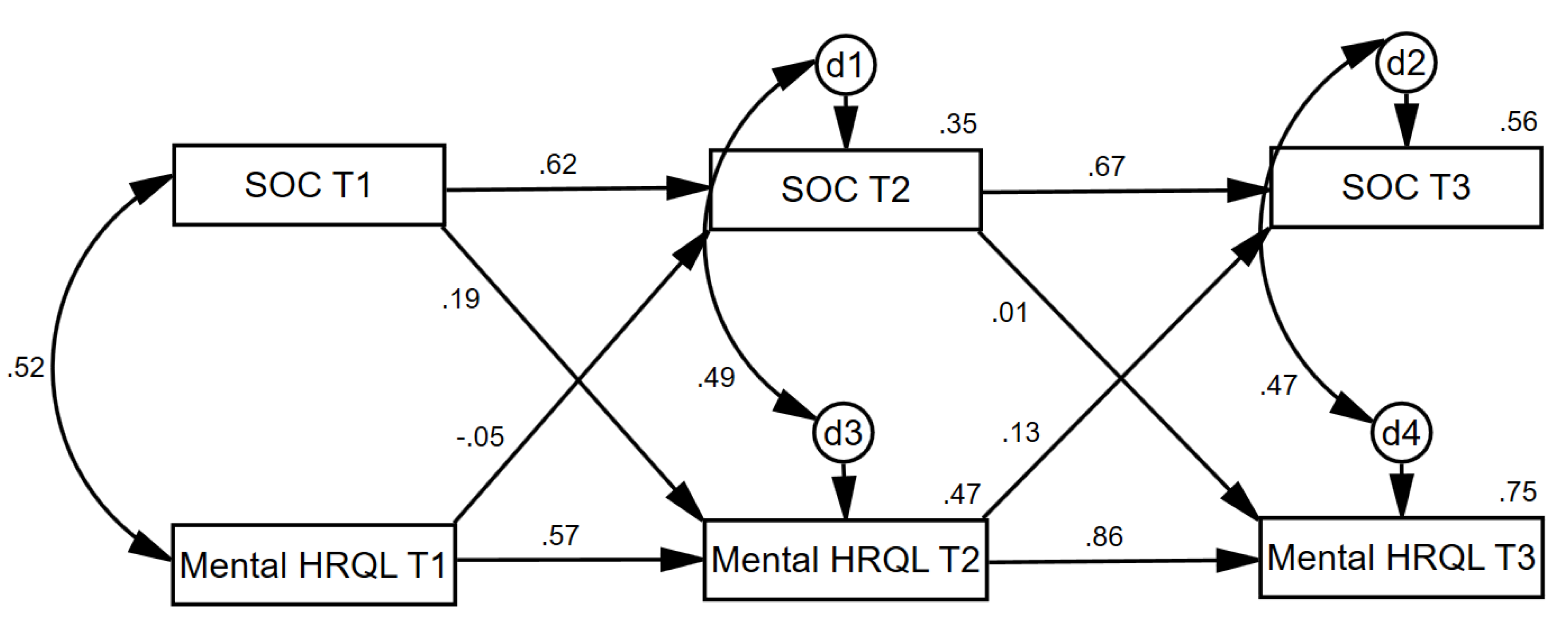
3.2. Cross-Lagged Effects
4. Discussion
4.1. Mediations
4.2. Cross-Lagged Effects
4.3. Implications
4.4. Limitations and Future Directions
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Vaishnavi, S.; Rao, V.; Fann, J.R. Neuropsychiatric problems after traumatic brain injury: Unraveling the silent epidemic. Psychosomatics 2009, 50, 198–205. [Google Scholar] [CrossRef]
- Briceño-León, R. Violence and the Right to Kill: Public Perceptions from Latin America. In Proceedings of the Workshop Rising Violence and the Criminal Justice Response in Latin America, Towards an Agenda for Collaborative Research in the 21st Century, Austin, TX, USA, 6–9 May 1999; pp. 6–9. [Google Scholar]
- Hyder, A.A.; Wunderlich, C.A.; Puvanachandra, P.; Gururaj, G.; Kobusingye, O.C. The impact of traumatic brain injuries: A global perspective. NeuroRehabilitation 2007, 22, 341–353. [Google Scholar] [CrossRef]
- Julio César, C.; Torres Norma, C.; Lozano, J.; Zúñiga Carrasco, I. Aspectos clínicos y epidemiológicos del trauma cráneo encefálico en México. Vigil. Epidemiol. 2008, 26, 1–4. [Google Scholar]
- Alvis-Miranda, H.R.; Navas, C.; Villa-Delgado, R.; Rubiano, A.M.; Alcala-Cerra, G.; Moscote-Salazar, L.R. Trends in Management of Traumatic Brain Injury by Emergency Physicians in Colombia. Panam. J. Trauma Crit. Care Emerg. Surg. 2013, 2, 134. [Google Scholar]
- Ramachandran, A.; Ranjit, A.; Zogg, C.K.; Herrera-Escobar, J.P.; Appelson, J.R.; Pino, L.F.; Aboutanous, M.B.; Haider, A.H.; Ordonez, C.A. Comparison of epidemiology of the injuries and outcomes in two first-level trauma centers in Colombia using the Pan-American Trauma Registry System. World J. Surg. 2017, 41, 2224–2230. [Google Scholar] [CrossRef] [PubMed]
- Jurkovich, G.J.; Mock, C. Systematic review of trauma system effectiveness based on registry comparisons. J. Trauma Acute Care Surg. 1999, 47, S46–S55. [Google Scholar] [CrossRef] [PubMed]
- Arango-Lasprilla, J.C.; Krch, D.; Drew, A.; De los Reyes Aragon, C.J.; Stevens, L.F. Health-related quality of life of individuals with traumatic brain injury in Barranquilla, Colombia. Brain Inj. 2012, 26, 825–833. [Google Scholar] [CrossRef] [PubMed]
- Arango-Lasprilla, J.C.; Quijano, M.C.; Aponte, M.; Cuervo, M.T.; Nicholls, E.; Rogers, H.L.; Kreutzer, J. Family needs in caregivers of individuals with traumatic brain injury from Colombia, South America. Brain Inj. 2010, 24, 1017–1026. [Google Scholar] [CrossRef] [PubMed]
- Rassovsky, Y.; Levi, Y.; Agranov, E.; Sela-Kaufman, M.; Sverdlik, A.; Vakil, E. Predicting long-term outcome following traumatic brain injury (TBI). J. Clin. Exp. Neuropsychol. 2015, 37, 354–366. [Google Scholar] [CrossRef] [PubMed]
- Bullinger, M. Quality of life in patients with traumatic brain injury-basic issues, assessment and recommendations. Restor. Neurol. Neurosci. 2002, 20, 111–124. [Google Scholar]
- Petersen, C.; Bullinger, M. Assessing health-related quality of life after severe brain damage: Potentials and limitations. Prog. Brain Res. 2005, 150, 545–553. [Google Scholar] [PubMed]
- Andelic, N.; Hammergren, N.; Bautz-Holter, E.; Sveen, U.; Brunborg, C.; Røe, C. Functional outcome and health-related quality of life 10 years after moderate-to-severe traumatic brain injury. Acta Neurol. Scand. 2009, 120, 16–23. [Google Scholar] [CrossRef] [PubMed]
- Polinder, S.; Haagsma, J.A.; van Klaveren, D.; Steyerberg, E.W.; Van Beeck, E.F. Health-related quality of life after TBI: A systematic review of study design, instruments, measurement properties, and outcome. Popul. Health Metr. 2015, 13, 4. [Google Scholar] [CrossRef] [PubMed]
- Soberg, H.L.; Røe, C.; Anke, A.; Arango-Lasprilla, J.C.; Skandsen, T.; Sveen, U.; von Steinbüchel, N.; Andelic, N. Health-related quality of life 12 months after severe traumatic brain injury: A prospective nationwide cohort study. J. Rehabil. Med. 2013, 45, 785–791. [Google Scholar] [CrossRef]
- Horneman, G.; Folkesson, P.; Sintonen, H.; von Wendt, L.; Emanuelson, I. Health-related quality of life of adolescents and young adults 10 years after serious traumatic brain injury. Int. J. Rehabil. Res. 2005, 28, 245–249. [Google Scholar] [CrossRef]
- Stalp, M.; Koch, C.; Ruchholtz, S.; Regel, G.; Panzica, M.; Krettek, C.; Pape, H.-C. Standardized outcome evaluation after blunt multiple injuries by scoring systems: A clinical follow-up investigation 2 years after injury. J. Trauma Acute Care Surg. 2002, 52, 1160–1168. [Google Scholar] [CrossRef]
- DeJong, G.; Batavia, A.I.; Williams, J.M. Who is responsible for the lifelong wellbeing of a person with a head injury? J. Head Trauma Rehabil. 1990, 5, 9–22. [Google Scholar] [CrossRef]
- Kitter, B.; Sharman, R. Caregivers’ support needs and factors promoting resiliency after brain injury. Brain Inj. 2015, 29, 1082–1093. [Google Scholar] [CrossRef]
- Kreutzer, J.S.; Stejskal, T.M.; Godwin, E.E.; Powell, V.D.; Arango-Lasprilla, J.C. A mixed methods evaluation of the Brain Injury Family Intervention. NeuroRehabilitation 2010, 27, 19–29. [Google Scholar] [CrossRef]
- Marin, G.; Marin, B.V. Research with Hispanic Populations; Sage Publications, Inc.: Newbury Park, CA, USA, 1991; ISBN 0-8039-3720-2. [Google Scholar]
- Niemann, Y.F. Stereotypes of Chicanas and Chicanos: Impact on family functioning, individual expectations, goals, and behavior. In The handbook of Chicana/o Psychology and Mental Health; Routledge: Abingdon, UK, 2004; pp. 79–100. [Google Scholar]
- Norup, A.; Perrin, P.B.; Cuberos-Urbano, G.; Anke, A.; Andelic, N.; Doyle, S.T.; Cristina Quijano, M.; Caracuel, A.; Mar, D.; Guadalupe Espinosa Jove, I. Family needs after brain injury: A cross cultural study. NeuroRehabilitation 2015, 36, 203–214. [Google Scholar] [CrossRef]
- Coy, A.E.; Perrin, P.B.; Stevens, L.F.; Hubbard, R.; Sosa, D.M.D.; Jove, I.G.E.; Arango-Lasprilla, J.C. Moderated mediation path analysis of Mexican traumatic brain injury patient social functioning, family functioning, and caregiver mental health. Arch. Phys. Med. Rehabil. 2013, 94, 362–368. [Google Scholar] [CrossRef] [PubMed]
- Gan, C.; Campbell, K.A.; Gemeinhardt, M.; McFadden, G.T. Predictors of family system functioning after brain injury. Brain Inj. 2006, 20, 587–600. [Google Scholar] [CrossRef] [PubMed]
- Minuchin, S.; Baker, L.; Rosman, B.L.; Liebman, R.; Milman, L.; Todd, T.C. A conceptual model of psychosomatic illness in children: Family organization and family therapy. Arch. Gen. Psychiatry 1975, 32, 1031–1038. [Google Scholar] [CrossRef] [PubMed]
- Antonovsky, A. Unraveling the Mystery of Health: How People Manage Stress and Stay Well; Jossey-Bass: San Francisco, CA, USA, 1987; ISBN 1-55542-028-1. [Google Scholar]
- Feigin, R. The relationship between the sense of coherence and adjustment to disability studied in the context of marital interrelations. Marriage Fam. Rev. 1998, 27, 71–90. [Google Scholar] [CrossRef]
- Garcia-Moya, I.; Rivera, F.; Moreno, C.; Lindström, B.; Jiménez-Iglesias, A. Analysis of the importance of family in the development of sense of coherence during adolescence. Scand. J. Public Health 2012, 40, 333–339. [Google Scholar] [CrossRef]
- Jacobsson, L.; Westerberg, M.; Malec, J.; Lexell, J. Sense of coherence and disability and the relationship with life satisfaction 6–15 years after traumatic brain injury in northern Sweden. Neuropsychol. Rehabil. 2011, 21, 383–400. [Google Scholar] [CrossRef]
- Collicutt McGrath, J.; Linley, P.A. Post-traumatic growth in acquired brain injury: A preliminary small scale study. Brain Inj. 2006, 20, 767–773. [Google Scholar] [CrossRef]
- Rena, F.; Moshe, S.; Abraham, O. Couples’ adjustment to one partner’s disability: The relationship between sense of coherence and adjustment. Soc. Sci. Med. 1996, 43, 163–171. [Google Scholar] [CrossRef]
- Kenny, D.A. Longitudinal Models: Autoregressive Models. Available online: http://davidakenny.net/cm/ar.html (accessed on 15 February 2019).
- Findler, M.; Cantor, J.; Haddad, L.; Gordon, W.; Ashman, T. The reliability and validity of the SF-36 health survey questionnaire for use with individuals with traumatic brain injury. Brain Inj. 2001, 15, 715–723. [Google Scholar] [CrossRef]
- Ayuso-Mateos, J.; Lasa, L.; Vázquez-Barquero, J.; Oviedo, A.; Diez-Manrique, J. Measuring health status in psychiatric community surveys: Internal and external validity of the Spanish version of the SF-36. Acta Psychiatr. Scand. 1999, 99, 26–32. [Google Scholar] [CrossRef] [PubMed]
- Antonovsky, A. The structure and properties of the sense of coherence scale. Soc. Sci. Med. 1993, 36, 725–733. [Google Scholar] [CrossRef]
- Virués-Ortega, J.; Martínez-Martín, P.; del Barrio, J.L.; Lozano, L.M. Validación transcultural de la Escala de Sentido de Coherencia de Antonovsky (OLQ-13) en ancianos mayores de 70 años. Med. Clínica 2007, 128, 486–492. [Google Scholar] [CrossRef] [PubMed]
- Aarons, G.A.; McDonald, E.J.; Connelly, C.D.; Newton, R.R. Assessment of family functioning in Caucasian and Hispanic Americans: Reliability, validity, and factor structure of the Family Assessment Device. Fam. Process 2007, 46, 557–569. [Google Scholar] [CrossRef] [PubMed]
- Elnasseh, A.G.; Trujillo, M.A.; Peralta, S.V.; Stolfi, M.E.; Morelli, E.; Perrin, P.B.; Arango-Lasprilla, J.C. Family dynamics and personal strengths among dementia caregivers in Argentina. Int. J. Alzheimer’s Dis. 2016, 2016, 2386728. [Google Scholar] [CrossRef]
- Andren, S.; Elmståhl, S. The relationship between caregiver burden, caregivers’ perceived health and their sense of coherence in caring for elders with dementia. J. Clin. Nurs. 2008, 17, 790–799. [Google Scholar] [CrossRef]
- Gison, A.; Rizza, F.; Bonassi, S.; Dall’Armi, V.; Lisi, S.; Giaquinto, S. The sense-of-coherence predicts health-related quality of life and emotional distress but not disability in Parkinson’s disease. BMC Neurol. 2014, 14, 193. [Google Scholar] [CrossRef]
- Sander, A.M.; Maestas, K.L.; Sherer, M.; Malec, J.F.; Nakase-Richardson, R. Relationship of caregiver and family functioning to participation outcomes after postacute rehabilitation for traumatic brain injury: A multicenter investigation. Arch. Phys. Med. Rehabil. 2012, 93, 842–848. [Google Scholar] [CrossRef]
- Kouneski, E. Circumplex model and FACES: Review of literature. Twin Cities MN Univ. Minn. 2002, 1, 1–60. [Google Scholar]
- Keenan, A.; Joseph, L. The needs of family members of severe traumatic brain injured patients during critical and acute care: A qualitative study. Can. J. Neurosci. Nurs. 2010, 32, 25–35. [Google Scholar]
- Bryant, R.A.; O’donnell, M.L.; Creamer, M.; McFarlane, A.C.; Clark, C.R.; Silove, D. The psychiatric sequelae of traumatic injury. Am. J. Psychiatry 2010, 167, 312–320. [Google Scholar] [CrossRef]
- Lammel, J.A. Relationship between Dimensions of Leisure Activity Experience, Sense of Coherence, and Psychological Well-Being for Traumatic Brain Injury Survivors. Ph.D. Thesis, Pennsylvania State University, State College, PA, USA, 2003. [Google Scholar]
- Lopez, R.A. Use of alternative folk medicine by Mexican American women. J. Immigr. Health 2005, 7, 23–31. [Google Scholar] [CrossRef] [PubMed]
- Kirchner, T.; Patino, C. Stress and depression in Latin American immigrants: The mediating role of religiosity. Eur. Psychiatry 2010, 25, 479–484. [Google Scholar] [CrossRef] [PubMed]
- Lehan, T.J.; Stevens, L.F.; Arango-Lasprilla, J.C.; Díaz Sosa, D.M.; Espinosa Jove, I.G. Balancing act: The influence of adaptability and cohesion on satisfaction and communication in families facing TBI in Mexico. NeuroRehabilitation 2012, 30, 75–86. [Google Scholar] [CrossRef] [PubMed]
- Snell, D.L.; Martin, R.; Surgenor, L.J.; Siegert, R.J.; Hay-Smith, E.J.C. What’s wrong with me? Seeking a coherent understanding of recovery after mild traumatic brain injury. Disabil. Rehabil. 2017, 39, 1968–1975. [Google Scholar] [CrossRef]
- Hsieh, M.-Y.; Ponsford, J.; Wong, D.; McKay, A. Exploring variables associated with change in cognitive behaviour therapy (CBT) for anxiety following traumatic brain injury. Disabil. Rehabil. 2012, 34, 408–415. [Google Scholar] [CrossRef]
- Ashman, T.; Cantor, J.B.; Tsaousides, T.; Spielman, L.; Gordon, W. Comparison of cognitive behavioral therapy and supportive psychotherapy for the treatment of depression following traumatic brain injury: A randomized controlled trial. J. Head Trauma Rehabil. 2014, 29, 467–478. [Google Scholar] [CrossRef]
- Yody, B.B.; Schaub, C.; Conway, J.; Peters, S.; Strauss, D.; Helsinger, S. Applied behavior management and acquired brain injury: Approaches and assessment. J. Head Trauma Rehabil. 2000, 15, 1041–1060. [Google Scholar] [CrossRef]
- Stejskal, T.M. Removing barriers to rehabilitation: Theory-based family intervention in community settings after brain injury. NeuroRehabilitation 2012, 31, 75–83. [Google Scholar] [CrossRef]
- Kreutzer, J.S.; Zasler, N.D.; Camplair, P.S.; Leininger, B.E. A practical guide to family intervention following adult traumatic brain injury. Community Integr. Trauma. Brain Inj. 1990, 249–273. [Google Scholar]
- Webster, G.; Daisley, A.; King, N. Relationship and family breakdown following acquired brain injury: The role of the rehabilitation team. Brain Inj. 1999, 13, 593–603. [Google Scholar]
- Andelic, N.; Sigurdardottir, S.; Schanke, A.-K.; Sandvik, L.; Sveen, U.; Roe, C. Disability, physical health and mental health 1 year after traumatic brain injury. Disabil. Rehabil. 2010, 32, 1122–1131. [Google Scholar] [CrossRef] [PubMed]
| Variable | Category | (n = 109) |
|---|---|---|
| Age, M (SD) | 35.87 (14.08) | |
| Years of Education, M (SD) | 9.99 (3.55) | |
| Days in Hospital | 20.78 (28.95) | |
| Month Between Injury and Baseline Data Collection, M (SD) | 1.85 (3.06) | |
| Site, n (%) | Neiva, Colombia | 20 (18.3) |
| Cali, Colombia | 21 (19.3) | |
| Mexico City, Mexico | 68 (62.4) | |
| TBI Patient Sex, n (%) | Male | 90 (82.6) |
| Female | 19 (17.4) | |
| Marriage Status Post-Injury, n (%) | Single | 48 (44) |
| Married | 27 (24.8) | |
| Divorced | 2 (1.8) | |
| Separated | 2 (1.8) | |
| Widowed | 2 (1.8) | |
| Open Relationship | 27 (24.8) | |
| Other | 1 (0.9) | |
| TBI Cause, n (%) | Automobile Accident | 12 (11) |
| Motorcycle Accident | 41 (37.6) | |
| Bicycle Accident | 3 (2.8) | |
| Pedestrian accident | 7 (6.4) | |
| Gunshot Wound | 2 (1.8) | |
| Act of Violence | 17 (15.6) | |
| Sports Injury/Accident | 1 (0.9) | |
| Fall | 23 (21.1) | |
| Other | 3 (2.8) | |
| Pre-Injury Employment Status, n (%) | Full-Time Employment | 66 (60.6) |
| Part-Time Employment | 17 (15.6) | |
| Homemaker | 8 (7.3) | |
| Unemployed | 7 (6.4) | |
| Student | 9 (8.3) | |
| Pension | 1 (0.9) | |
| Retired | 1 (0.9) |
| Study Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Physical HRQL Time 1 | |||||||||||
| 2. Physical HRQL Time 2 | 0.552 ** | ||||||||||
| 3. Physical HRQL Time 3 | 0.537 ** | 0.898 ** | |||||||||
| 4. Mental HRQL Time 1 | 0.656 ** | 0.544 ** | 0.549 ** | ||||||||
| 5. Mental HRQL Time 2 | 0.360 ** | 0.755 ** | 0.696 ** | 0.669 ** | |||||||
| 6. Mental HRQL Time 3 | 0.399 ** | 0.733 ** | 0.793 ** | 0.637 ** | 0.867 ** | ||||||
| 7. SOC Time 1 | 0.213 * | 0.368 ** | 0.448 ** | 0.524 ** | 0.491 ** | 0.519 ** | |||||
| 8. SOC Time 2 | 0.08 | 0.453 ** | 0.412 ** | 0.273 ** | 0.557 ** | 0.490 ** | 0.591 ** | ||||
| 9. SOC Time 3 | 0.174 | 0.410 ** | 0.481 ** | 0.365 ** | 0.504 ** | 0.596 ** | 0.694 ** | 0.740 ** | |||
| 10. Healthy Family Dynamics Time 1 | 0.153 | 0.357 ** | 0.455 ** | 0.356 ** | 0.432 ** | 0.532 ** | 0.466 ** | 0.377 ** | 0.441 ** | ||
| 11. Healthy Family Dynamics Time 2 | 0.151 | 0.334 ** | 0.371 ** | 0.214 * | 0.351 ** | 0.389 ** | 0.333 ** | 0.321 ** | 0.439 ** | 0.730 ** | |
| 12. Healthy Family Dynamics Time 3 | 0.156 | 0.317 ** | 0.367 ** | 0.169 | 0.332 ** | 0.411 ** | 0.212 * | 0.302 ** | 0.387 ** | 0.612 ** | 0.782 ** |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cariello, A.N.; Perrin, P.B.; Rodríguez-Agudelo, Y.; Olivera Plaza, S.L.; Quijano-Martinez, M.C.; Arango-Lasprilla, J.C. A Multi-Site Study of Traumatic Brain Injury in Mexico and Colombia: Longitudinal Mediational and Cross-Lagged Models of Family Dynamics, Coping, and Health-Related Quality of Life. Int. J. Environ. Res. Public Health 2020, 17, 6045. https://doi.org/10.3390/ijerph17176045
Cariello AN, Perrin PB, Rodríguez-Agudelo Y, Olivera Plaza SL, Quijano-Martinez MC, Arango-Lasprilla JC. A Multi-Site Study of Traumatic Brain Injury in Mexico and Colombia: Longitudinal Mediational and Cross-Lagged Models of Family Dynamics, Coping, and Health-Related Quality of Life. International Journal of Environmental Research and Public Health. 2020; 17(17):6045. https://doi.org/10.3390/ijerph17176045
Chicago/Turabian StyleCariello, Annahir N., Paul B. Perrin, Yaneth Rodríguez-Agudelo, Silvia Leonor Olivera Plaza, Maria Cristina Quijano-Martinez, and Juan Carlos Arango-Lasprilla. 2020. "A Multi-Site Study of Traumatic Brain Injury in Mexico and Colombia: Longitudinal Mediational and Cross-Lagged Models of Family Dynamics, Coping, and Health-Related Quality of Life" International Journal of Environmental Research and Public Health 17, no. 17: 6045. https://doi.org/10.3390/ijerph17176045
APA StyleCariello, A. N., Perrin, P. B., Rodríguez-Agudelo, Y., Olivera Plaza, S. L., Quijano-Martinez, M. C., & Arango-Lasprilla, J. C. (2020). A Multi-Site Study of Traumatic Brain Injury in Mexico and Colombia: Longitudinal Mediational and Cross-Lagged Models of Family Dynamics, Coping, and Health-Related Quality of Life. International Journal of Environmental Research and Public Health, 17(17), 6045. https://doi.org/10.3390/ijerph17176045






