Independent and Combined Relationships of Perceived Neighborhood Social Cohesion and Physical Frailty on Functional Disability in Community-Dwelling Older Adults
Abstract
1. Introduction
2. Methods
2.1. Participants
2.2. Data Collection Procedure
2.3. Measures
2.3.1. Functional Disability
2.3.2. Physical Frailty
2.3.3. Perceived Neighborhood Social Cohesion
2.3.4. Covariates
2.4. Data Analysis
3. Results
3.1. Sample Characteristics
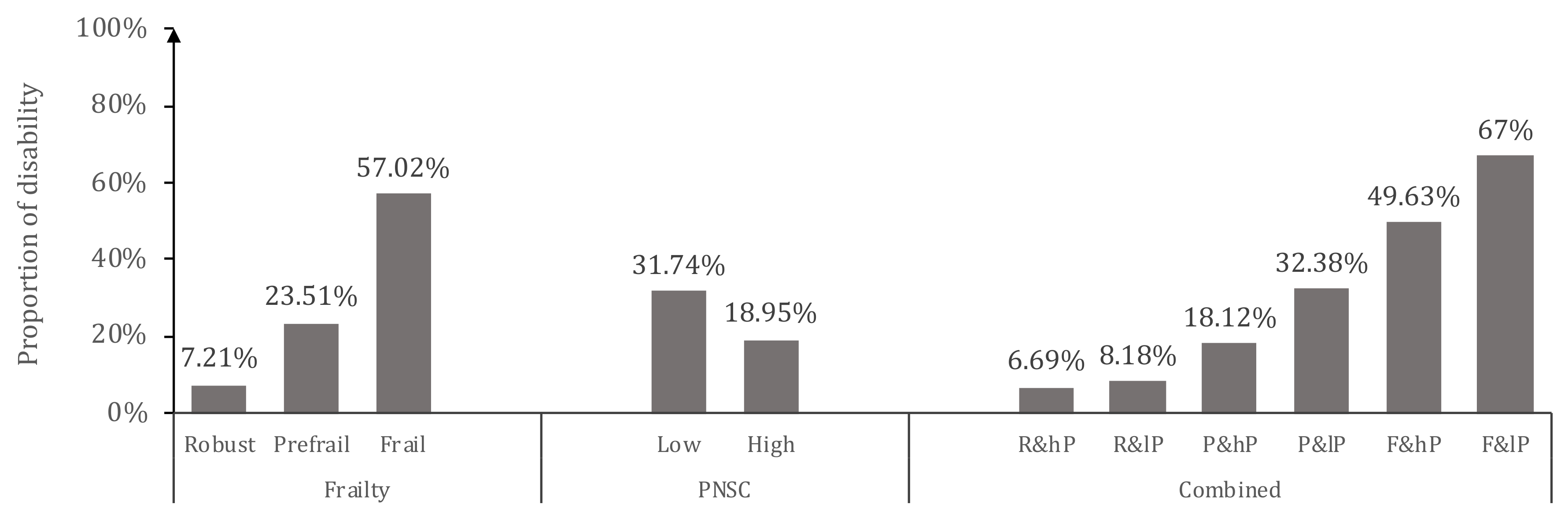
3.2. Rate of Functional Disability with Different Sample Characteristics
3.3. Physical Frailty and Perceived Neighborhood Social Cohesion According to Functional Disability
3.4. Independent Impact of Physical Frailty and Perceived Social Cohesion on Functional Disability
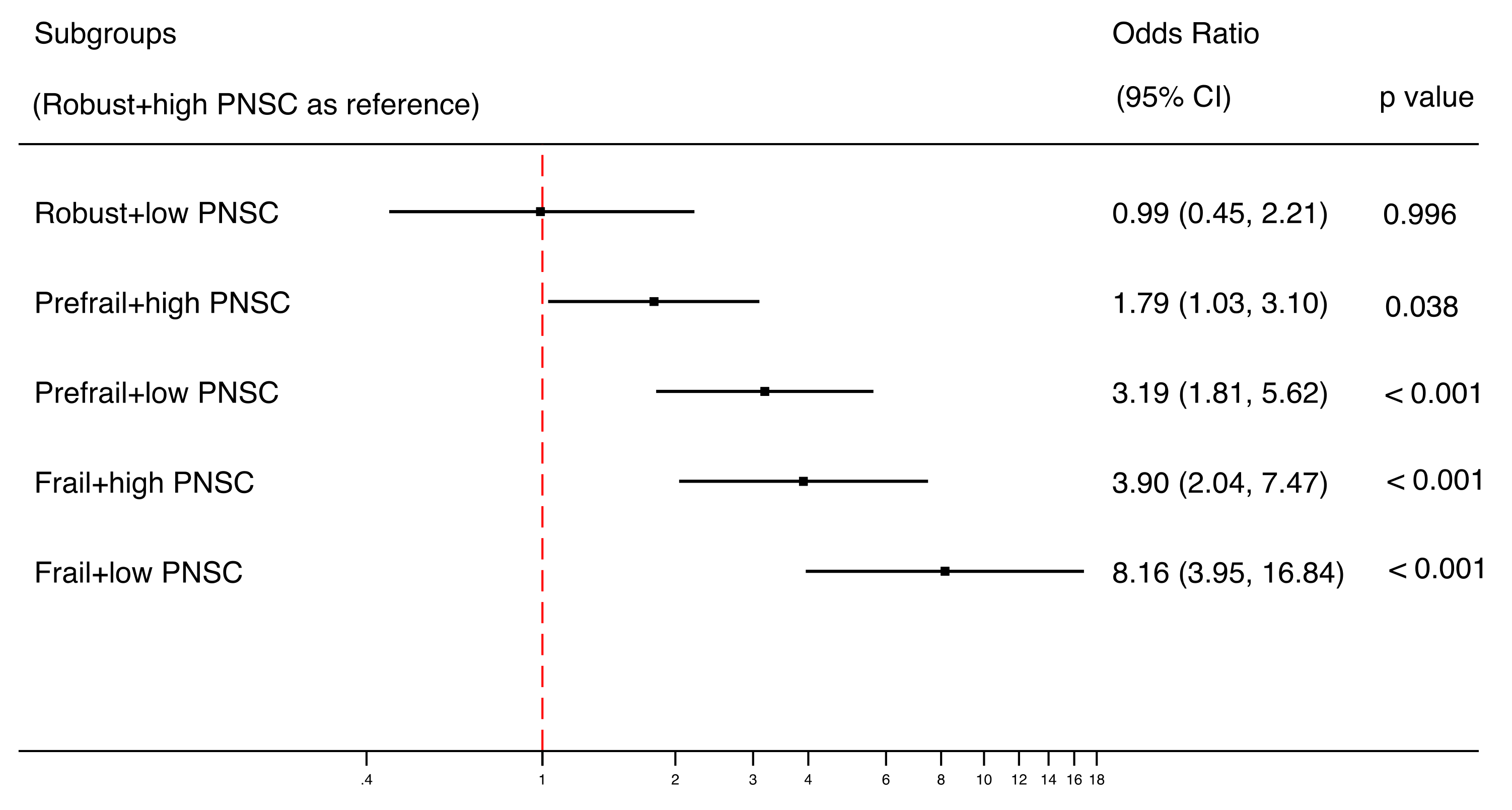
3.5. Combined Impact of Physical Frailty and Perceived Neighborhood Social Cohesion on Functional Disability
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Pope, A.; Tarlov, A.R. Disability in America:Toward a National Agenda for Prevention; National Academy Press: Washington, DC, USA, 1991. [Google Scholar]
- Rivera-Almaraz, A.; Manrique-Espinoza, B.; Ávila-Funes, J.A.; Chatterji, S.; Naidoo, N.; Kowal, P.; Salinas-Rodríguez, A. Disability, quality of life and all-cause mortality in older Mexican adults: Association with multimorbidity and frailty. BMC Geriatr. 2018, 18, 236. [Google Scholar] [CrossRef]
- Ng, W.L.; Shaw, J.E.; Peeters, A. The relationship between excessive daytime sleepiness, disability, and mortality, and implications for life expectancy. Sleep Med. 2018, 43, 83–89. [Google Scholar] [CrossRef]
- Jespersen, L.N.; Michelsen, S.I.; Tjørnhøj-Thomsen, T.; Svensson, M.K.; Holstein, B.E.; Due, P. Living with a disability: A qualitative study of associations between social relations, social participation and quality of life. Disabil. Rehabil. 2019, 41, 1275–1286. [Google Scholar] [CrossRef]
- Gill, T.M.; Han, L.; Gahbauer, E.A.; Leo-Summers, L.; Allore, H.G. Prognostic Effect of Changes in Physical Function Over Prior Year on Subsequent Mortality and Long-Term Nursing Home Admission. J. Am. Geriatr. Soc. 2018, 66, 1587–1591. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Dang, J. Blue Book of Aging: China Report of the Development on Aging Cause (2013); Social Sciences Academic Press: Beijing, China, 2013. [Google Scholar]
- World Health Organization. China Country Assessment Report on Ageing and Health; WHO: Geneva, Switzerland, 2015. [Google Scholar]
- Wang, X.Q.; Chen, P.J. Population ageing challenges health care in China. Lancet 2014, 383, 870. [Google Scholar] [CrossRef]
- Xu, X.; Chen, L. Projection of Long-Term Care Costs in China, 2020–2050: Based on the Bayesian Quantile Regression Method. Sustainability 2019, 11, 3530. [Google Scholar] [CrossRef]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in older adults: Evidence for a phenotype. J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, 146–156. [Google Scholar] [CrossRef] [PubMed]
- Morley, J.E.; Vellas, B.; van Kan, G.A.; Anker, S.D.; Bauer, J.M.; Bernabei, R.; Cesari, M.; Chumlea, W.C.; Doehner, W.; Evans, J.; et al. Frailty consensus: A call to action. J. Am. Med. Dir. Assoc. 2013, 14, 392–397. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.X.; Ding, G.; Yu, W.J.; Liu, T.F.; Yan, A.Y.; Chen, H.Y.; Zhang, A.H. Association between frailty and incident risk of disability in community-dwelling elder people: Evidence from a meta-analysis. Public Health 2019, 175, 90–100. [Google Scholar] [CrossRef]
- Biritwum, R.B.; Minicuci, N.; Yawson, A.E.; Theou, O.; Mensah, G.P.; Naidoo, N.; Wu, F.; Guo, Y.; Zheng, Y.; Jiang, Y.; et al. Prevalence of and factors associated with frailty and disability in older adults from China, Ghana, India, Mexico, Russia and South Africa. Maturitas 2016, 91, 8–18. [Google Scholar]
- Vermeulen, J.; Neyens, J.C.; van Rossum, E.; Spreeuwenberg, M.D.; de Witte, L.P. Predicting ADL disability in community-dwelling elderly people using physical frailty indicators: A systematic review. BMC Geriatr. 2011, 11, 33. [Google Scholar] [CrossRef]
- Provencher, V.; Beland, F.; Demers, L.; Desrosiers, J.; Bier, N.; Avila-Funes, J.A.; Galand, C.; Julien, D.; Fletcher, J.D.; Trottier, L.; et al. Are frailty components associated with disability in specific activities of daily living in community-dwelling older adults? A multicenter Canadian study. Arch. Gerontol. Geriatr. 2017, 73, 187–194. [Google Scholar] [CrossRef] [PubMed]
- Gao, J.; Weaver, S.R.; Fu, H.; Jia, Y.; Li, J. Relationships between neighborhood attributes and subjective well-being among the Chinese elderly: Data from Shanghai. Biosci. Trends 2017, 11, 516–523. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.S.; Hawes, A.M.; Smith, J. Perceived neighbourhood social cohesion and myocardial infarction. J. Epidemiol. Community Health 2014, 68, 1020–1026. [Google Scholar] [CrossRef]
- Kim, E.S.; Park, N.; Peterson, C. Perceived neighborhood social cohesion and stroke. Soc. Sci. Med. 2013, 97, 49–55. [Google Scholar] [CrossRef]
- Olamijuwon, E.O.; Odimegwu, C.O.; De Wet, N. Social cohesion and self-rated health among adults in South Africa: The moderating role of race. Health Place 2018, 51, 89–96. [Google Scholar] [CrossRef]
- Braveman, P.; Gottlieb, L. The social determinants of health: It’s time to consider the causes of the causes. Public Health Rep. 2014, 129, 19–31. [Google Scholar] [CrossRef]
- Gwon, J.G.; Choi, J.; Han, Y.J. Community-level socioeconomic inequality in the incidence of ischemic heart disease: A nationwide cohort study. BMC Cardiovasc. Disord. 2020, 20, 87. [Google Scholar] [CrossRef]
- McNeill, L.H.; Kreuter, M.W.; Subramanian, S.V. Social environment and physical activity: A review of concepts and evidence. Soc. Sci. Med. 2006, 63, 1011–1022. [Google Scholar] [CrossRef]
- Fone, D.; Dunstan, F.; Lloyd, K.; Williams, G.; Watkins, J.; Palmer, S. Does social cohesion modify the association between area income deprivation and mental health? A multilevel analysis. Int. J. Epidemiol. 2007, 36, 338–345. [Google Scholar] [CrossRef]
- Stafford, M.; Bartley, M.; Sacker, A.; Marmot, M.; Wilkinson, R.; Boreham, R.; Thomas, R. Measuring the social environment: Social cohesion and material deprivation in English and Scottish neighbourhoods. Environ. Plan. Econ. Space 2003, 35, 1459–1475. [Google Scholar] [CrossRef]
- Diez Roux, A.V.; Kershaw, K.; Lisabeth, L. Neighborhoods and cardiovascular risk: Beyond individual-level risk factors. Curr. Cardiovasc. Risk Rep. 2008, 2, 175. [Google Scholar] [CrossRef]
- Cagney, K.A.; Glass, T.A.; Skarupski, K.A.; Barnes, L.L.; Schwartz, B.S.; de Leon, C.F.M. Neighborhood-level cohesion and disorder: Measurement and validation in two older adult urban populations. J. Gerontol. B Psychol. Sci. Soc. Sci. 2009, 64, 415–424. [Google Scholar] [CrossRef] [PubMed]
- Rios, R.; Aiken, L.S.; Zautra, A.J. Neighborhood contexts and the mediating role of neighborhood social cohesion on health and psychological distress among Hispanic and non-Hispanic residents. Ann. Behav. Med. 2012, 43, 50–61. [Google Scholar] [CrossRef] [PubMed]
- Ruijsbroek, A.; Droomers, M.; Hardyns, W.; Groenewegen, P.P.; Stronks, K. The interplay between neighbourhood characteristics: The health impact of changes in social cohesion, disorder and unsafety feelings. Health Place 2016, 39, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Rahman, M.H.U.; Singh, A. Disability and social cohesion among older adults: A multi-country study. Int. J. Soc. Econ. 2019, 46, 485–502. [Google Scholar] [CrossRef]
- Cramm, J.M.; Nieboer, A.P. Relationships between frailty, neighborhood security, social cohesion and sense of belonging among community-dwelling older people. Geriatr. Gerontol. Int. 2013, 13, 759–763. [Google Scholar] [CrossRef]
- Ye, B.; Gao, J.; Fu, H. Associations between lifestyle, physical and social environments and frailty among Chinese older people: A multilevel analysis. BMC Geriatr. 2018, 18, 314. [Google Scholar] [CrossRef]
- Zheng, X.; Chen, G.; Song, X.; Liu, J.; Yan, L.; Du, W.; Pang, L.; Zhang, L.; Wu, J.; Zhang, B.; et al. Twenty-year trends in the prevalence of disability in China. Bull. World Health Organ. 2011, 89, 788–797. [Google Scholar] [CrossRef]
- Huang, W.; Ge, X.; Hou, S.; Gao, G.; Zhang, X.; Yu, Y. Ability of daily living and its influencing factors among rural elderly in Dabieshan Mountain area. Chin. J. Public Health 2012, 7, 884–886. [Google Scholar]
- Robinson, T.N.; Wu, D.S.; Sauaia, A.; Dunn, C.L.; Stevens-Lapsley, J.E.; Moss, M.; Stiegmann, G.V.; Gajdos, C.; Cleveland, J.C., Jr.; Inouye, S.K. Slower walking speed forecasts increased postoperative morbidity and 1-year mortality across surgical specialties. Ann. Surg. 2013, 258, 582–588. [Google Scholar] [CrossRef] [PubMed]
- Savva, G.M.; Donoghue, O.A.; Horgan, F.; O’Regan, C.; Cronin, H.; Kenny, R.A. Using timed up-and-go to identify frail members of the older population. J. Gerontol. A Biol. Sci. Med. Sci. 2013, 68, 441–446. [Google Scholar] [CrossRef] [PubMed]
- Deng, Y.; Paul, D.R. The Relationships Between Depressive Symptoms, Functional Health Status, Physical Activity, and the Availability of Recreational Facilities: A Rural-Urban Comparison in Middle-Aged and Older Chinese Adults. Int. J. Behav. Med. 2018, 25, 322–330. [Google Scholar] [CrossRef] [PubMed]
- Ma, L.; Li, Z.; Tang, Z.; Sun, F.; Diao, L.; Li, J.; He, Y.; Dong, B.; Li, Y. Prevalence and socio-demographic characteristics of disability in older adults in China: Findings from China Comprehensive Geriatric Assessment Study. Arch. Gerontol. Geriatr. 2017, 73, 199–203. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Qin, J.; Li, Y.; Wei, Y.; Long, B.; Cai, J.; Tang, J.; Xu, X.; Yu, G.; Zhang, Z. Disability and Its Influencing Factors among the Elderly in a County, Guangxi Province, China. Int. J. Environ. Res. Public Health 2018, 15, 1967. [Google Scholar] [CrossRef] [PubMed]
- Masnoon, N.; Shakib, S.; Kalisch-Ellett, L.; Caughey, G.E. What is polypharmacy? A systematic review of definitions. BMC Geriatr. 2017, 17, 230. [Google Scholar] [CrossRef]
- Kim, E.S.; Kawachi, I. Perceived Neighborhood Social Cohesion and Preventive Healthcare Use. Am. J. Prev. Med. 2017, 53, 35–40. [Google Scholar] [CrossRef]
- Hoogerbrugge, M.M.; Burger, M.J. Neighborhood-Based social capital and life satisfaction: The case of Rotterdam, The Netherlands. Urban Geogr. 2018, 39, 1484–1509. [Google Scholar] [CrossRef]
- Fujihara, S.; Tsuji, T.; Miyaguni, Y.; Aida, J.; Saito, M.; Koyama, S.; Kondo, K. Does Community-Level Social Capital Predict Decline in Instrumental Activities of Daily Living? A JAGES Prospective Cohort Study. Int. J. Environ. Res. Public Health 2019, 16, 828. [Google Scholar] [CrossRef]
- Aida, J.; Kondo, K.; Kawachi, I.; Subramanian, S.V.; Ichida, Y.; Hirai, H.; Kondo, N.; Osaka, K.; Sheiham, A.; Tsakos, G.; et al. Does social capital affect the incidence of functional disability in older Japanese? A prospective population-based cohort study. J. Epidemiol. Community Health 2013, 67, 42–47. [Google Scholar] [CrossRef]
- Levasseur, M.; Généreux, M.; Bruneau, J.F.; Vanasse, A.; Chabot, É.; Beaulac, C.; Bédard, M.M. Importance of proximity to resources, social support, transportation and neighborhood security for mobility and social participation in older adults: Results from a scoping study. BMC Public Health 2015, 15, 503. [Google Scholar] [CrossRef] [PubMed]
- Sampson, R.J. Local Friendship Ties and Community Attachment in Mass Society—A Multilevel Systemic Model. Am. Sociol. Rev. 1988, 53, 766–779. [Google Scholar] [CrossRef]
- De Leon, C.F.M.; Cagney, K.A.; Bienias, J.L.; Barnes, L.L.; Skarupski, K.A.; Scherr, P.A.; Evans, D.A. Neighborhood Social Cohesion and Disorder in Relation to Walking in Community-Dwelling Older Adults A Multilevel Analysis. J. Aging Health 2009, 21, 155–171. [Google Scholar] [CrossRef] [PubMed]
- Lee, R.E.; O’Connor, D.P.; Smith-Ray, R.; Mama, S.K.; Medina, A.V.; Estabrooks, P.A. Effects and Mediators of a Social Cohesion Intervention to Increase Physical Activity and Improve Dietary Habits in Women of Color: Health Is Power. Ann. Behav. Med. 2011, 41, S35. [Google Scholar]
- Lozano, P.; Fleischer, N.L.; Moore, S.; Shigematsu, L.M.R.; Santillan, E.; Thrasher, J.F. Does neighborhood social cohesion modify the relationship between neighborhood social norms and smoking behaviors in Mexico? Health Place 2016, 40, 145–152. [Google Scholar] [CrossRef]
- Erdem, O.; Prins, R.G.; Voorham, T.; van Lenthe, F.J.; Burdorf, A. Structural neighbourhood conditions, social cohesion and psychological distress in the Netherlands. Eur. J. Public Health 2015, 25, 995–1001. [Google Scholar] [CrossRef]
- Graham, H.; White, P.C. Social determinants and lifestyles: Integrating environmental and public health perspectives. Public Health 2016, 141, 270–278. [Google Scholar] [CrossRef]
- Rethorn, Z.D.; Cook, C.; Reneker, J.C. Social Determinants of Health: If You Aren’t Measuring Them, You Aren’t Seeing the Big Picture. J. Orthop. Sports Phys. Ther. 2019, 49, 872–874. [Google Scholar] [CrossRef]
- Gill, T.M.; Gahbauer, E.A.; Allore, H.G.; Han, L. Transitions between frailty states among community-living older persons. Arch. Intern. Med. 2006, 166, 418–423. [Google Scholar] [CrossRef]
- Sacha, J.; Sacha, M.; Soboń, J.; Borysiuk, Z.; Feusette, P. Is It Time to Begin a Public Campaign Concerning Frailty and Pre-frailty? A Review Article. Front. Physiol. 2017, 8, 484. [Google Scholar] [CrossRef]
- Su, P.; Ding, H.; Zhang, W.; Duan, G.; Yang, Y.; Chen, R.; Duan, Z.; Du, L.; Xie, C.; Jin, C.; et al. The association of multimorbidity and disability in a community-based sample of elderly aged 80 or older in Shanghai, China. BMC Geriatr. 2016, 16, 178. [Google Scholar] [CrossRef] [PubMed]
- Gao, M.; Sa, Z.; Li, Y.; Zhang, W.; Tian, D.; Zhang, S.; Gu, L. Does social participation reduce the risk of functional disability among older adults in China? A survival analysis using the 2005–2011 waves of the CLHLS data. BMC Geriatr. 2018, 18, 224. [Google Scholar] [CrossRef] [PubMed]
| Total n (%) | Normal n (%) | Disability n (%) | p Value † | ||
|---|---|---|---|---|---|
| Gender | Male | 666 (41.3) | 513 (41.7) | 153 (40.1) | 0.558 |
| Female | 945 (58.7) | 716 (58.3) | 229 (59.9) | - | |
| Age | 75–80 years | 811 (50.2) | 718 (58.3) | 93 (24.2) | <0.001 ** |
| 81–85 years | 453(28.0) | 333 (27.0) | 120 (31.3) | - | |
| 86 years and older | 352 (21.8) | 181 (14.7) | 171 (44.5) | - | |
| Educated Years | ≤9 years | 794 (49.5) | 575 (47.0) | 219 (57.3) | <0.001 ** |
| >9 years | 811 (50.5) | 648 (53.0) | 163 (42.7) | - | |
| Marriage Status | Married | 1060 (65.7) | 846 (68.7) | 214 (56.0) | <0.001 ** |
| Unmarried | 553 (34.3) | 385 (31.3) | 168 (44.0) | - | |
| Family Income Monthly | <5000 Yuan | 1070 (66.3) | 800 (65.0) | 270 (70.5) | 0.046 * |
| ≥5000 Yuan | 544 (33.7) | 431 (35.0) | 113 (29.5) | - | |
| Hypertension | Yes | 1062 (65.7) | 785 (63.7) | 277 (72.1) | 0.002 ** |
| Stroke | Yes | 107 (6.63) | 65 (5.28) | 42 (11.0) | <0.001 ** |
| Heart Diseases | Yes | 631 (39.1) | 438 (35.6) | 193 (50.3) | <0.001 ** |
| Diabetes Mellitus | Yes | 357 (22.1) | 268 (21.8) | 89 (23.2) | 0.557 |
| Urine Incontinence | Yes | 342 (21.3) | 216 (17.7) | 126 (33.0) | <0.001 ** |
| Chronic Pain | Yes | 788 (48.8) | 553 (45.0) | 235 (61.2) | <0.001 ** |
| Visional Impairment | Yes | 1257 (77.8) | 941 (76.4) | 316 (82.3) | 0.015 * |
| Hearing Impairment | Yes | 887 (55) | 629 (51.1) | 258 (67.4) | <0.001 ** |
| Polypharmacy | ≥5 Medications | 155 (9.6) | 105 (8.5) | 50 (13.1) | 0.008 ** |
| Hospitalization in Past Year | Yes | 270 (16.7) | 165 (13.4) | 105 (27.3) | <0.001 ** |
| Falls in Past Year | Yes | 169 (10.5) | 115 (9.4) | 54 (14.1) | 0.008 ** |
| Cognitive Function | Intact | 1043 (65.9) | 866 (71.4) | 177 (47.8) | <0.001 ** |
| Impaired | 540 (34.1) | 347 (28.6) | 193 (52.2) | - | |
| Depression | Normal | 1250 (78.4) | 1017 (83.6) | 233 (61.6) | <0.001 ** |
| Depressed | 345 (21.6) | 200 (16.4) | 145 (38.4) | - |
| Unadjusted Model | Adjusted Model † | ||||
|---|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | ||
| PF | Robust | 1.00 | 1.00 | ||
| Pre-frail | 3.95 (2.68, 5.82) | <0.001 | 2.30 (1.49, 3.55) | <0.001 | |
| Frail | 17.14 (11.02, 26,68) | <0.001 | 5.33 (3.17, 8.96) | <0.001 | |
| PNSC | High Level | 1.00 | 1.00 | ||
| Low Level | 2.00 (1.56, 2.57) | <0.001 | 1.71 (1.28, 2.27) | <0.001 | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xie, B.; Ma, C.; Wang, J. Independent and Combined Relationships of Perceived Neighborhood Social Cohesion and Physical Frailty on Functional Disability in Community-Dwelling Older Adults. Int. J. Environ. Res. Public Health 2020, 17, 5912. https://doi.org/10.3390/ijerph17165912
Xie B, Ma C, Wang J. Independent and Combined Relationships of Perceived Neighborhood Social Cohesion and Physical Frailty on Functional Disability in Community-Dwelling Older Adults. International Journal of Environmental Research and Public Health. 2020; 17(16):5912. https://doi.org/10.3390/ijerph17165912
Chicago/Turabian StyleXie, Boqin, Chenjuan Ma, and Junqiao Wang. 2020. "Independent and Combined Relationships of Perceived Neighborhood Social Cohesion and Physical Frailty on Functional Disability in Community-Dwelling Older Adults" International Journal of Environmental Research and Public Health 17, no. 16: 5912. https://doi.org/10.3390/ijerph17165912
APA StyleXie, B., Ma, C., & Wang, J. (2020). Independent and Combined Relationships of Perceived Neighborhood Social Cohesion and Physical Frailty on Functional Disability in Community-Dwelling Older Adults. International Journal of Environmental Research and Public Health, 17(16), 5912. https://doi.org/10.3390/ijerph17165912






