Assessment in the Supine-To-Stand Task and Functional Health from Youth to Old Age: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
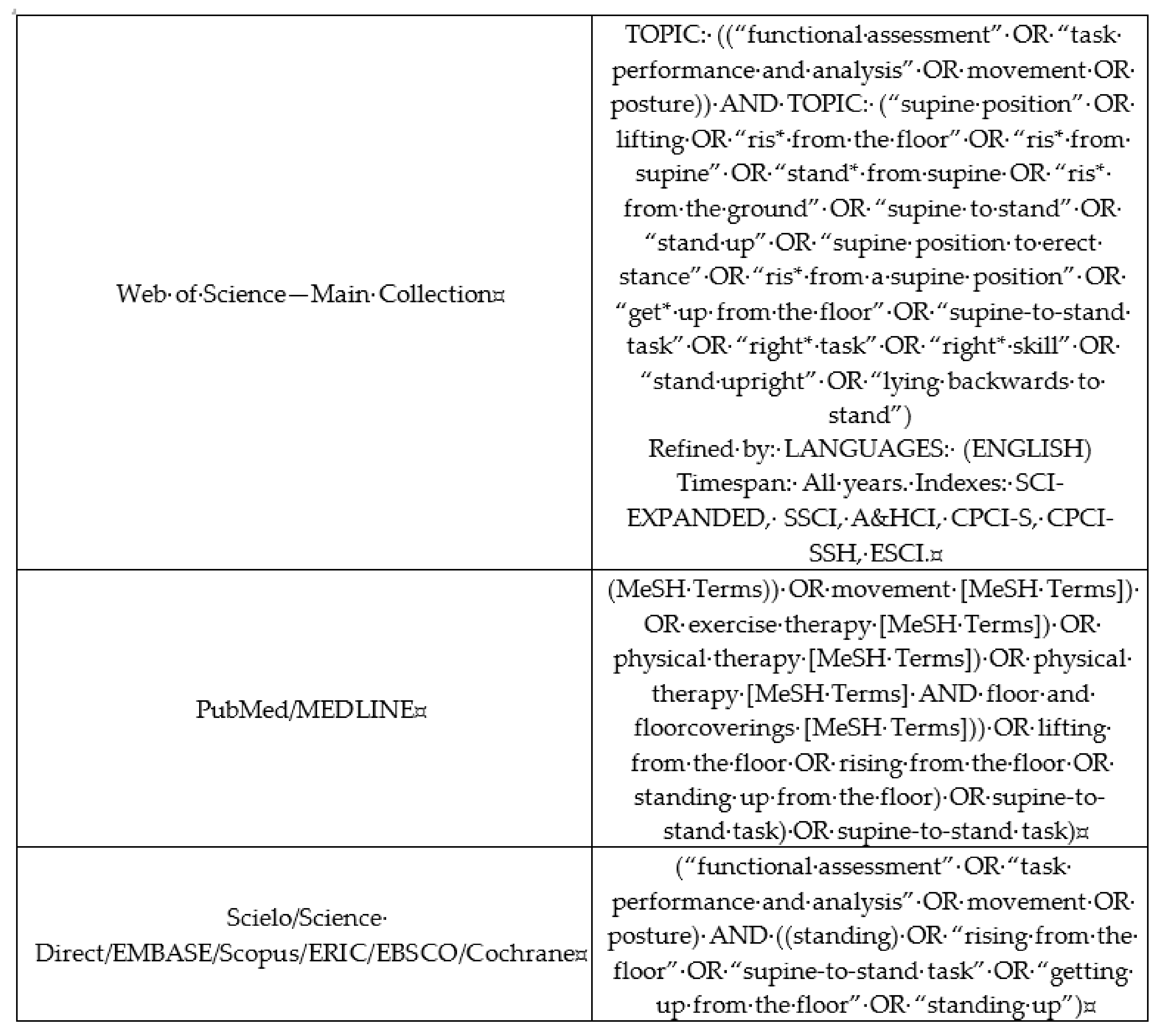
2.1. Data Sources and Searches Descriptors
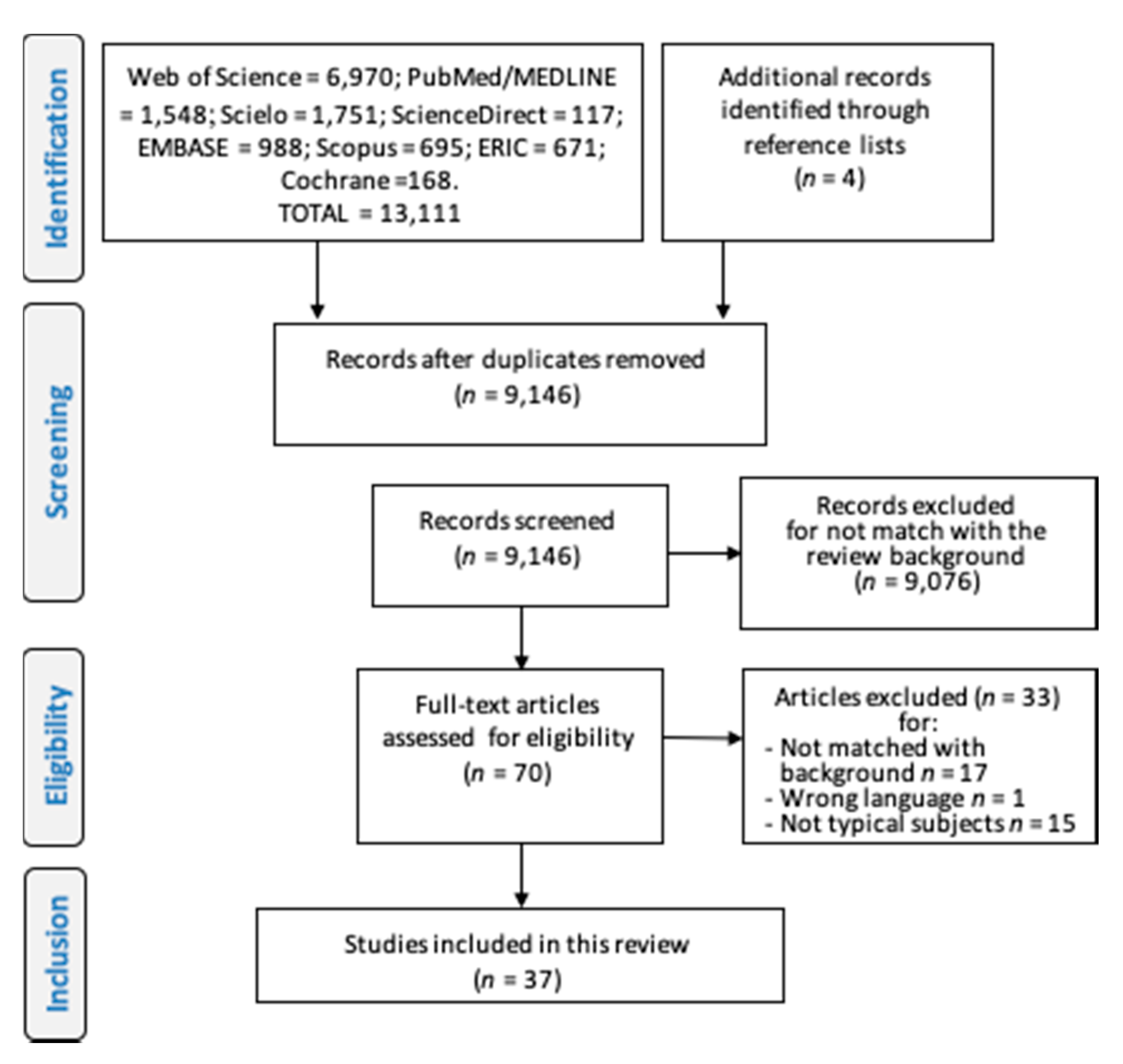
2.2. Study Selection
2.3. Data Extraction and Methodological Quality Assessment (Risk of Bias)
3. Results
The STS Task Performance and Body Weight Status, Musculoskeletal Fitness and Physical Activity
4. Discussion
4.1. Risk of Bias and Procedure Protocols
4.2. STS Performance and Body Weight Status, Musculoskeletal Fitness, and Physical Activity
4.3. Clinical Applications
4.4. Study Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
Appendix A
- ✓
- The participant’s feet must be bare, and it is suggested that participants wear light clothes, suitable for exercise;
- ✓
- The subject makes a trail test in order to train before performing valid attempts.
- ✓
- All commands given to participants must be communicated with kindness and firmness;
- ✓
- Do not give any feedback to participants between tests;
- ✓
- Do not give any visual instructions;
- ✓
- Repeat a minimum of three times and more if needed to address process-oriented mode sequences; the best performance (lowest movement time) is the primary measure for the analyses;
- ✓
- The interval between trials must last for as long as it takes for the participant to reposition himself/herself on the floor. It is not a problem if the participant takes more time between one attempt and another to return to the initial position: Individual comfort should be maintained;
- ✓
- In the case of elderly participants, at least one assistant must be behind the performer to provide any help during the action of rising from the ground.
References
- VanSant, A.F. Life-span development in functional tasks. Phys. Ther. 1990, 70, 788–798. [Google Scholar] [CrossRef] [PubMed]
- Leversen, J.S.R.; Haga, M.; Sigmundsson, H. From children to adults: Motor performance across the life-span. PLoS ONE 2012, 7, e38830. [Google Scholar] [CrossRef] [PubMed]
- VanSant, A.F. Age Differences in Movement Patterns Used by Children to Rise from a Supine Position to Erect Stance. Phys. Ther. 1988, 68, 1330–1338. [Google Scholar] [CrossRef] [PubMed]
- Alexander, N.B.; Ulbrich, J.; Raheja, A.; Channer, D. Rising from the floor in older adults. J. Am. Geriatr. Soc. 1997, 45, 564–569. [Google Scholar] [CrossRef] [PubMed]
- Cattuzzo, M.T.; dos Santos Henrique, R.; Ré, A.H.N.; de Oliveira, I.S.; Melo, B.M.; de Sousa Moura, M.; de Araújo, R.C.; Stodden, D. Motor competence and health related physical fitness in youth: A systematic review. J. Sci. Med. Sport 2016, 19, 123–129. [Google Scholar] [CrossRef] [PubMed]
- Robinson, L.E.; Stodden, D.F.; Barnett, L.M.; Lopes, V.P.; Logan, S.W.; Rodrigues, L.P.; D’Hondt, E. Motor Competence and its Effect on Positive Developmental Trajectories of Health. Sport. Med. 2015, 45, 1273–1284. [Google Scholar] [CrossRef]
- Stodden, D.F.; Langendorfer, S.J.; Goodway, J.D.; Roberton, M.A.; Rudisill, M.E.; Garcia, C.; Garcia, L.E. A developmental perspective on the role of motor skill competence in physical activity: An emergent relationship. Quest 2008, 60, 290–306. [Google Scholar] [CrossRef]
- Nesbitt, D.; Molina, S.L.; Sacko, R.; Robinson, L.E.; Brian, A.; Stodden, D. Examining the Feasibility of Supine-to-Stand as a Measure of Functional Motor Competence. J. Mot. Learn. Dev. 2018, 6, 267–286. [Google Scholar] [CrossRef]
- VanSant, A.F. Rising from a supine position to erect stance. Description of adult movement and a developmental hypothesis. Phys. Ther. 1988, 62, 185–192. [Google Scholar]
- Duncan, M.J.; Lawson, C.; Walker, L.J.; Stodden, D.; Eyre, E.L.J. The Utility of the Supine-to-Stand Test as a Measure of Functional Motor Competence in Children Aged 5-9 Years. Sports 2017, 5, 67. [Google Scholar] [CrossRef]
- Nesbitt, D.; Molina, S.L.; Cattuzzo, M.T.; Robinson, L.E.; Phillips, D.; Stodden, D. Assessment of a Supine-to-Stand (STS) Task in Early Childhood: A Measure of Functional Motor Competence. J. Mot. Learn. Dev. 2017, 5, 252–266. [Google Scholar] [CrossRef]
- Marsala, G.; VanSant, A.F. Age-related differences in movement patterns used by toddlers to rise from a suppine position to erect stance. Phys. Ther. 1998, 78, 149–159. [Google Scholar] [CrossRef] [PubMed]
- Green, L.N.; Williams, K. Differences in developmental movement patterns used by active versus sedentary middle-aged adults coming from a supine position to erect stance. Phys. Ther. 1992, 8, 560–568. [Google Scholar] [CrossRef]
- Bergland, A.; Jarnlo, G.B.; Laake, K. Validity of an index of self-reported walking for balance and falls in elderly women. Adv. Physiother. 2002, 4, 65–73. [Google Scholar] [CrossRef]
- Bergland, A.; Wyller, T.B. Risk factors for serious fall related injury in elderly women living at home. Inj. Prev. 2004, 10, 308–313. [Google Scholar] [CrossRef] [PubMed]
- Bergland, A.; Laake, K. Concurrent and predictive validity of “getting up from lying on the floor”. Aging Clin. Exp. Res. 2005, 17, 181–185. [Google Scholar] [CrossRef] [PubMed]
- Hands, B.P.; Hands, B. How Can We Best Measure Fundamental Movement Skills? Paper presented at the Australian Council for Health, Physical Education and Recreation Inc. (ACHPER) 23rd Biennial National/International Conference: Interactive Health & Physical Education, Launceston, TAS, Australia, 3–5 July 2002. [Google Scholar]
- Burton, A.W.; Miller, D.E. Movement Skill Assessment; Human Kinectis: Champaign, IL, USA, 1998. [Google Scholar]
- Hofmeyer, M.R.; Alexander, N.B.; Nyquist, L.V.; Medell, J.L.; Koreishi, A. Floor-rise strategy training in older adults. J. Am. Geriatr. Soc. 2002, 50, 1702–1706. [Google Scholar] [CrossRef] [PubMed]
- Hsue, B.J.; Chen, Y.J.; Wang, Y.E. The intra- and inter-rater reliability of component analysis of rise from supine in the children with typical development and developmental delay. Res. Dev. Disabil. 2014, 35, 162–170. [Google Scholar] [CrossRef]
- Hsue, B.J.; Wang, Y.E.; Chen, Y.J. The movement patterns used to rise from a supine position by children with developmental delay and age-related differences in these. Res. Dev. Disabil. 2014, 35, 2205–2214. [Google Scholar] [CrossRef]
- Schwickert, L.; Oberle, C.; Becker, C.; Lindemann, U.; Klenk, J.; Schwenk, M.; Bourke, A.; Zijlstra, W. Model development to study strategies of younger and older adults getting up from the floor. Aging Clin. Exp. Res. 2016, 28, 277–287. [Google Scholar] [CrossRef]
- Grant, M.J.; Booth, A. A typology of reviews: An analysis of 14 review types and associated methodologies. Health Info. Libr. J. 2009, 26, 91–108. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Altman, D.; Antes, G.; Atkins, D.; Barbour, V.; Barrowman, N.; Berlin, J.A.; et al. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan-a web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Law, M.; Stewart, D.; Letts, L.; Pollock, N.; Bosch, J.; Westmorland, M. Guidelines for Critical Review of Qualitative Studies; McMaster University Occupational Therapy Evidence-Based Practice Research Group: Hamilton, ON, Canada, 1998. [Google Scholar]
- Mewasingh, L.D.; Demil, A.; Christiaens, F.J.C.; Missa, A.M.; Cheron, G.; Dan, B. Motor strategies in standing up in leukomalacic spastic diplegia. Brain Dev. 2002, 24, 291–295. [Google Scholar] [CrossRef]
- Mewasingh, L.D.; Sékhara, T.; Pelc, K.; Missa, A.M.; Cheron, G.; Dan, B. Motor strategies in standing up in children with hemiplegia. Pediatr. Neurol. 2004, 30, 257–261. [Google Scholar] [CrossRef]
- Ng, J.; Conaway, M.R.; Rigby, A.S.; Priestman, A.; Baxter, P.S. Methods of standing from supine and percentiles for time to stand and to run 10 m in young children. J. Pediatr. 2013, 162, 552–556. [Google Scholar] [CrossRef]
- Kuwabara, C.; Shiba, Y.; Sakamoto, M.; Sato, H. The Relationship between the Movement Patterns of Rising from a Supine Position to an Erect Stance and Physical Functions in Healthy Children. Adv. Phys. Educ. 2013, 3, 92–97. [Google Scholar] [CrossRef][Green Version]
- Bohannon, R.W.; Lusardi, M.M. Getting up from the floor. Determinants and techniques among healthy older adults. Physiother. Theory Pract. 2004, 20, 233–241. [Google Scholar] [CrossRef]
- James, E.G. Body movement instructions facilitate synergy level motor learning, retention and transfer. Neurosci. Lett. 2012, 522, 162–166. [Google Scholar] [CrossRef]
- Santos De Oliveira, I.; Da, D.; Oliveira, S.; Cattuzzo, M.T. The Effect of Different Instructions in a General Motor Competence and Perceived Competence of Children. J. Phys. Educ. Sport. Manag. 2016, 3, 108–126. [Google Scholar]
- Beenakker, E.A.C.; Maurits, N.M.; Fock, J.M.; Brouwer, O.F.; van der Hoeven, J.H. Functional ability and muscle force in healthy children and ambulant Duchenne muscular dystrophy patients. Eur. J. Paediatr. Neurol. 2005, 9, 387–393. [Google Scholar] [CrossRef] [PubMed]
- Naugle, K.M.; Higgins, T.J.; Manini, T.M. Obesity and use of compensatory strategies to perform common daily activities in pre-clinically disabled older adults. Arch. Gerontol. Geriatr. 2012, 54, e134–e138. [Google Scholar] [CrossRef] [PubMed]
- Manckoundia, P.; Buatois, S.; Gueguen, R.; Perret-Guillaume, C.; Laurain, M.C.; Pfitzenmeyer, P.; Benetos, A. Clinical determinants of failure in balance tests in elderly subjects. Arch. Gerontol. Geriatr. 2008, 47, 217–228. [Google Scholar] [CrossRef] [PubMed]
- Klima, D.W.; Anderson, C.; Samrah, D.; Patel, D.; Chui, K.; Newton, R. Standing from the floor in community-dwelling older adults. J. Aging Phys. Act. 2016, 24, 207–213. [Google Scholar] [CrossRef]
- Manini, T.M.; Cook, S.B.; VanArnam, T.; Marko, M.; Ploutz-Snyder, L. Evaluating task modification as an objective measure of functional limitation: Repeatability and comparability. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2006, 61, 718–725. [Google Scholar] [CrossRef]
- King, L.A.; VanSant, A.F. The effect of solid ankle-foot orthoses on movement patterns used in a supine-to-stand rising task. Phys. Ther. 1995, 75, 952–964. [Google Scholar] [CrossRef]
- Belt, A.B.; Hertel, T.A.; Mante, J.R.; Marks, T.; Rockett, V.L.; Wade, C.; Clayton-Krasinski, D. Movement Characteristics of Persons with Prader-Willi Syndrome Rising from Supine. Pediatr. Phys. Ther. 2001, 13, 110–121. [Google Scholar] [CrossRef]
- Didier, J.P.; Mourey, F.; Brondel, L.; Marcer, I.; Milan, C.; Casillas, J.M.; Verges, B.; Winsland, J.K.D. The energetic cost of some daily activities: A comparison in a young and old population. Age Ageing 1993, 22, 90–96. [Google Scholar] [CrossRef]
- Ulbrich, J.; Raheja, A.; Alexander, N.B. Body positions used by healthy and frail older adults to rise from the floor. J. Am. Geriatr. Soc. 2000, 48, 1626–1632. [Google Scholar] [CrossRef]
- Schwickert, L.; Boos, R.; Klenk, J.; Bourke, A.; Becker, C.; Zijlstra, W. Inertial sensor based analysis of lie-to-stand transfers in younger and older adults. Sensors (Switz.) 2016, 16, 1277. [Google Scholar] [CrossRef]
- Schenkman, M.; Morey, M.; Kuchibhatla, M. Spinal flexibility and balance control among community-dwelling adults with and without Parkinson’s disease. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2000, 55, 441–445. [Google Scholar] [CrossRef] [PubMed]
- Henwood, T.R.; Taaffe, D.R. Improved physical performance in older adults undertaking a short-term programme of high-velocity resistance training. Gerontology 2005, 51, 108–115. [Google Scholar] [CrossRef] [PubMed]
- Manckoundia, P.; Gerbault, N.; Mourey, F.; d’Athis, P.; Nourdin, C.; Monin, M.P.; Camus, A.; Pfitzenmeyer, P. Multidisciplinary management in geriatric day-hospital is beneficial for elderly fallers: A prospective study of 28 cases. Arch. Gerontol. Geriatr. 2007, 44, 61–70. [Google Scholar] [CrossRef] [PubMed]
- Geraldes, A.A.R.; Albuquerque, R.B.; Soares, R.M.; Carvalho, J.; Farinatti, P.T.V. Association between flexibility of the glenohumeral and hip joints and functional performance in active elderly women. Rev. Bras. Fisioter. 2008, 12, 274–282. [Google Scholar]
- Raso, V.; Greve, J.M.D. Aerobic or resistance exercise improves performance in activities of daily living in elderly women. Rev. Bras. Med. Esporte 2012, 18, 87–90. [Google Scholar] [CrossRef][Green Version]
- Manckoundia, P.; Barthélémy, E.; Bonnot, R.; d’Athis, P. Impact of an ambulatory physical activity program on balance and motor abilities of retirees: A prospective study. Int. J. Clin. Pract. 2020, e13474. [Google Scholar]
- Moffett, M.A.; Avers, D.; Bohannon, R.W.; Shaw, K.L.; Merlo, A.R. Performance and Clinimetric Properties of the Timed Up From Floor Test Completed by Apparently Healthy Community-Dwelling Older Women. J. Geriatr. Phys. Ther. 2020. [Google Scholar] [CrossRef]
- Wulf, G.; McNevin, N.; Shea, C.H. The automaticity of complex motor skill learning as a function of attentional focus. Q. J. Exp. Psychol. A 2001, 54, 1143–1154. [Google Scholar] [CrossRef]
- Reid, K.F.; Fielding, R.A. Skeletal Muscle Power: A Critical Determinant of Physical. Exerc. Sport Sci. Rev. 2012, 40, 4–12. [Google Scholar] [CrossRef]
- Stodden, D.F.; True, L.K.; Langendorfer, S.J.; Gao, Z. Associations among selected motor skills and health-related fitness: Indirect evidence for Seefeldt’s proficiency barrier in young adults? Res. Q. Exerc. Sport 2013, 84, 397–403. [Google Scholar] [CrossRef]
- Utesch, T.; Bardid, F.; Strauss, B. The relationship between motor competence and physical fitness from early childhood to early adulthood: A meta-analysis. Sport. Med. 2019, 49, 541–551. [Google Scholar] [CrossRef] [PubMed]
- Robinson, L.E.; Goodway, J.D. Instructional climates in preschool children who are at-risk. Part I: Object-control skill development. Res. Q. Exerc. Sport 2009, 80, 533–542. [Google Scholar] [CrossRef] [PubMed]
- Barnett, L.M.; Morgan, P.J.; Van Beurden, E.; Ball, K.; Lubans, D.R. A reverse pathway? Actual and perceived skill proficiency and physical activity. Med. Sci. Sports Exerc. 2011, 43, 898–904. [Google Scholar] [CrossRef] [PubMed]
| Author (Year); Country | Objective | Study Design/Sample Characteristics | Main Outcome Measures | Main Results and Conclusions Related to STS Task | |
|---|---|---|---|---|---|
| Process or Product-Oriented Movement | Lifestyle/Motor Functions | ||||
| Childhood | |||||
| VanSant (1988) [3]; US | (1) To determine whether within the STS task MPs of different body regions vary with age, (2) describe movements used by children to perform this task. | OBS/pre-longitudinal/NP; 120 children divided into 4, 5, 6, and 7-year-old groups with 30 subjects each, matched by gender; G1 = 4.5 ± 0.27 yrs., G2 = 5.41 ± 0.28 yrs., G3 = 6.5 ± 0.27 yrs., G4 = 7.33 ± 0.24 yrs. | Process—MPs categories (UE, AX, and LE regions). | - | (1) Age differences in the incidence of MPs in each body region. (2) A trend toward increased symmetry of MPs as age increased. (3) The oldest subjects did not commonly use the symmetric form when rising. (4) Changes in the STS task likely to continue beyond early childhood. |
| Marsala and VanSant (1998) [24]; US | (1) To describe the MPs of toddlers on the STS task; (2) To determine whether toddlers’ MPs differ with age; (3) investigate whether MPs occur earliest in the development of this task prevail in toddlers. | OBS/pre-longitudinal/NP; 60 toddlers: 20 aged 15–25 months (mean age = 20.5 ± 2.9 mo.); 19 aged 26–36 months (mean age = 30.2 ± 2.6 mo.); 20 aged 37–47 months (mean age = 43.5 ± 2.6 mo.). | Process—MPs categories (UE, AX, and LE regions). | - | (1) Toddlers’ UE and AX movements confirmed previously developed MPs categories. (2) Age differences among toddlers regarding MPs. (3) MPs of UE and AX thought to occur earliest in the STS developmental sequence prevailed in this young group. |
| Mewasingh et al. (2002) [29]; Belgium | To analyze whether children with spastic diplegia use MPs as described for TD children and whether other MPs coexisted. | OBS/NP; 10 children with spastic diplegia associated with leukomalacia (♀ = 7; mean age = 7.5 ± 2 yrs.), CG: 14 age-matched TD children. | Process—MPs categories (UE, AX, and LE regions—adapted from Marsala and VanSant [12]. | - | Children with spastic diplegia use MPs described in healthy children, but with markedly reduced within- and inter-individual variability. |
| Mewasingh et al. (2004) [30]; Belgium | To describe MPs in the STS task used by children with hemiplegic cerebral palsy (HCP). | OBS/NP; 15 children (♀ = 8; mean age = 7.3 ± 2.8) with HCP who were able to walk unsupported 5 m or more and perform the STS task without assistance; CG = 14 age-matched TD children. | Process—MPs categories (UE, AX, and LE regions, adapted from Marsala and VanSant [12] | - | Children with HCP performed the STS task using general MPs, but with reduced inter-individual variability compared to CG, with more asymmetrical patterns with systematic support on the unaffected side. |
| Beenakker et al. (2005) [36]; Netherlands | To report typical values for timed functional tests in TD children; to determine which parameter changes most in ambulant children with DMD by comparing typical values for muscle force and functional ability with values obtained by these children. | OBS/NP; 16 ambulant children with DMD (mean age = 6.25 ± 0.93); TD children: ♂ = 66 (mean age = 7.4 ± 2.3) and ♀ = 57 (mean age = 7.4 ± 2.2 yrs.). | Product—STS time (s). | Running 9 m. | STS time in TD children: 4 yrs. (♀ = 1.52 s; ♂ = 1.56 s), 5 yrs. (♀ = 1.45 s; ♂ = 1.45 s), 6 yrs. (♀ = 1.17 s; ♂ = 1.42 s), 7 yrs. (♀ = 1.19 s; ♂ = 1.28 s), 8 yrs. (♀ = 1.03 s; ♂ = 1.24 s), 9 yrs. (♀ = 1.06 s; ♂ = 1.17 s), 10 yrs. (♀ = 1.42 s; ♂ = 1.08 s), and 11 yrs. (♀ = 1.13 s; ♂ = 0.99 s). The DMD children’s performance declined with age, while TD children improved it; DMD children (8 yrs.) took 7.5 times longer than DD ones; timed functional testing seemed to be more sensitive to determine disease progression and functional impairment changes than force measurement. |
| Ng et al. (2013) [31]; UK | To define typical values from the time to STS and the time to run 10 m, formulate charts for these tests, and assess their reproducibility. | OBS/pre-longitudinal screening/NP; n = 321 TD children; ♀ = 160; age range = 2–8 yrs. (mean age = 5.1 yrs.). | Product—STS Time (s); Process—the method used to stand from the supine position. | Age, sex, height, weight, BMI, and time to run 10 m. | STS time = 2.08 s (range 1.03–5.28 s); an association between the standing method and age; boys: Association between the standing method and STS time; large variability in the method used and STS time in youngers; strong negative correlation with age; height, weight, or BMI not affected the STS time; charts showed age-related values. |
| Kuwabara et al. (2013) [32]; Japan | To determine the relationship between the choices of movement patterns in STS task and physical functions in healthy children. O | 68 TD children (♀ = 42), age range = 3.4–6.4 yrs. | Process—MPs categories (UE, AX, and LE regions, from VanSant [3] | Age, sex, grip strength, trunk flexor, and extensor strength; balance in one-leg standing time(s) | Children who demonstrated symmetrical MPs had significantly higher grip and trunk muscle strength and better balance than children who showed asymmetrical MPs. The symmetrical MPs were explained by a positive relationship to grip strength and trunk flexor strength. Muscle strength seems to be related to symmetrical MPs of the STS task in healthy children. |
| Hsue (2014) [21]; Taiwan | To determine the within—and inter-rater reliability in classifying the MPs of STS task in TD children and children with mild to moderate DD. | OBS/NP; 68 TD children: 5–6 yrs. (n = 15), 4–5 yrs. (n = 19), 3–4 yrs. (n = 20), and 2–3 yrs. (n = 14); 20 children with DD: 5–6 yrs. (n = 4), 4–5 yrs. (n = 4), 3–4 yrs. (n = 6), and 2–3 yrs. (n = 5). | Process—MPs categories (UE, AX, and LE regions) | Developmental capability tested by Peabody Developmental Motor Scale-II. | Complexities and difficulties affecting the within- and inter-rater reliability in classifying the MPs of STS task were related to developmental capability, age, and body region. Extra training seems to be needed for children with DD, particularly for the UE and LE regions. |
| Hsue (2014) [22]; Taiwan | (1) To determine MPs of children with DD used to STS task and how they differ from age-matched TD children, (2) to verify whether MPs differ with age in children with DD, and (3) To determine and compare the developmental sequences for the MPs for UE, AX, and LE in DD children and TD children. | OBS/NP; 66 TD children: 5–6 yrs. (n = 15), 4–5 yrs. (n = 19), 3–4 yrs. (n = 19), 2–3 yrs. (n = 13); 31 children with DD: 5–6 yrs. (n = 5), 4–5 yrs. (n = 6), 3–4 yrs. (n = 8), 2–3 yrs. (n = 12). | Process—MPs categories (UE, AX, and LE regions) from VanSant [3] revised by Marsala and VanSant [12], and Belt et al. [40] | Developmental capability tested by Peabody Developmental Motor Scale-II ( | The TD group followed the proposed developmental sequences, as well as the DD group, which showed different maturation speed and more variability, especially between the age of 3 and 5 yrs.; the most used MPs by children with DD were at least one developmental categorical pattern behind those used by the age-matched TD children before 5 yrs. Old, except for the LE region. In the DD group, children with better motor performance used more developmentally advanced patterns. |
| Duncan et al., (2017) [11]; UK | To examine how STS performance is related to process and product assessment of motor competence (MC) in children. | OBS/NP; 91 TD children (♀ = 44) aged 5–9 years (mean age = 6.8 ± 1.2 yrs.). | Product—STS Time (s) Process—MPs categories (UE, AX, and LE regions—VanSant [3]. | MC score comprised four skills: run, jump, catch, throw, 10 m running speed, and standing long jump distance. | Children who scored higher on STS process also scored higher on MC process and were faster in the 10 m running time; a significant association between STS time and BMI (r = −0.508), STS time and STS process (r = −0.463), standing long jump distance (cm) and STS time (r = −0.414), and 10 m running speed (s) and STS time (r = 0.539). STS test is a measure of functional MC in children. |
| Nesbitt et al. (2017) [12]; US | To examine the relationship between qualitative (developmental sequences) and quantitative (time) performance rising from a supine position in early childhood. | OBS/NP; 122 TD children (♀ = 56); age range = 3–5 years (mean age = 4.63 ± 0.5 yrs.). | Product—STS Time (s) Process—MPs categories (UE, AX, and LE regions—VanSant [3]. | BMI | The children’ STS task performance was quite variable in terms of qualitative MPs; STS mean time = 2.37 s, ± 0.60. The levels of the components of UE (r = -.383) and AX (r = −416) were correlated with time. Results indicated a strong association between trunk control development and UE (r = 0.791) movement levels, and together they demonstrated the strongest effect on STS performance. There was no association between BMI and time in the STS task. |
| Childhood and Adulthood | |||||
| Belt et al. (2001) [42]; US | To determine if previously published descriptors of the STS task in healthy individuals could be applied to the movements of persons with Prader-Willi Syndrome; and 2) assess UE, AX, LE region movements among subjects with PWS compared with TD controls. | OBS/NP; 9 subjects (children and adults) with PWS and nine matched TD controls; age range = seven –36 yrs. | Process—MPs categories (UE, AX, and LE regions) were classified using modified descriptors developed by Marsala and VanSant [12]; Product—STS time (s) | BMI | Subjects with PWS utilized less advanced asymmetrical rising patterns, took longer to rise (5.4 s for subjects with PWS and 2.86 s for controls), and demonstrated less within-subject variability than controls. Knowledge of successful rising patterns may use to assess and plan intervention strategies. Regardless of diagnosis, there was a weak correlation between body region movement score and BMI (rho = 0.01). There was no relationship between BMI and body region scores. |
| Nesbitt et al. (2018); [8]; US | To examine the validity of STS as a developmental measure of functional MC across childhood into young adulthood and examining associations between movement components. STS time also provided a secondary measure of developmental validity in addition to an examination of the concurrent validity of STS against developmentally valid measures of MC. | OBS/NP; 265 subjects ♂♀ (children and adults) distributed in 4 age groups: 3–6 (mean age 4.8 ± 0.9 years); 9–12 (mean age 10 ± 0.8 years); 13–17 (mean age 14.9 ± 0.9 years); 18–25 (mean age 20.9 ± 2 years) | Process—MPs categories (UE, AX, and LE regions) were classified using modified descriptors developed by Marsala and VanSant [12]; Product –STS time (s) | Developmentally valid measures of motor competence Throwing, kicking, jumping, hopping, and STS skills test | Results indicated that cross-sectional curves for the STS components generally fit Roberton’s (1980) hypothetical model curves. STS time demonstrated weak to moderate correlations to STS time across all age groups, indicating that it can be considered a valid and reliable measure of MC across childhood into young adulthood |
| Adulthood | |||||
| VanSant (1988b) [10]; US | (1) To describe MPs within specific body regions used to stand up from a supine position. (2) To identify motor developmental sequences for the UE, AX, and LE regions during this rising task. | OBS/NP; 32 healthy adults (♀ = 17); age range = 20–35 yrs. (mean age = 28.6 yrs.). | Process—MPs categories (UE, AX, and LE regions). | - | Subjects varied greatly in the MPs; 25% of subjects demonstrated a similar combination of MPs during rising, which involved the symmetrical use of the limbs and trunk while flexing forward from a supine position, moving through sitting to squatting, and then standing. An ordering of categories for each body region was proposed as a developmental sequence of STS MPs. |
| Green and Williams (1992) [14]; US | (1) To validate categories for the MPs of STS task in adults. (2) To evaluate the influence that physical activity might have on the MPs used for rising. | OBS/NP; 72 adults, age range = 30–39 years (mean age = 34.1 ± 2.8 yrs.) divided into three groups: group 1 (n = 25) reported daily physical activity, group 2 (n = 26) reported exercising once or twice a week, and group 3 (n = 21) reported did exercises less than once a week. | Process—MPs categories (UE, AX, and LE regions—VanSant, [3]. | Level of physical activity (questionnaire). | More active people used more advanced MP than the rarely active ones. The lifestyle patterns of regular, moderate physical activity may influence the STS task performance. This study provided support for the use of developmental sequences for the MP of the STS task. |
| Didier et al. (1993) [43]; France | To compare the energetic costs of daily activities in young and older adults, such as rising and sitting back down on a seat, getting up from and lying down on a bed, and getting up from the floor. | OBS/NP; 10 healthy men (mean age = 24.3 ± 2.8 yrs.), and 10 older men (mean age = 74.4 ± 2.2 yrs.). | Product—STS time (s). | Energy Cost | Getting up from and lying down on the floor or a standard hospital bed involved the same energy cost in the older and younger group, but performing these activities took significantly longer for the older people |
| King and VanSant (1995) [41]; US | To verify if SAFOs affect the MPs used in the STS task, and to determine the mode and the incidence of MPs under each condition. | Interventional/NP convenience sample; 39 healthy adults, age range = 20–28 yrs. (mean age = 22.7 ± 1.87 yrs.). | Process—MPs categories (UE, AX, and LE regions). | - | Changes in the incidence of MPs occurred in all SAFO conditions, but not with the no SAFO condition. Changes resulted in more asymmetry in SAFOs condition, mainly in the axial region. |
| Adulthood and Elderly phase | |||||
| Alexander et al. (1997) [4]; US | (1) To determine the ability of older adults to rise from the floor; (2) explore how the ability to rise might differ based on the initial body position, with and without the use of an assistive device. | OBS/NP; 24 (♀ = 12) adults, age range = 19–30 years (mean age = 23 yrs.); 24 (♀ = 12) healthy older adults, age range = 66–87 yrs. (mean age = 73 yrs.); 38 (♀ = 32) older adults, living in congregate housings for the elderly, age range = 63–94 yrs. (mean age = 80 yrs.). | Product—STS time (s); Process—from five different initial positions, with and without external support: (1) supine; (2) on the side; (3) prone; (4) all fours; and (5) sitting. | Perceived level of difficulty. | Older adults had more difficulty performing STS task than young. Healthy older adults took two times longer than adults to rise; congregate older adults took 2–3 times more than healthy older adults. Adults and healthy older adults rose from every position; Congregate older adults were most likely rising successfully from a side-lying position using furniture for support. The most capable subjects rose more quickly and had fewer difficulties when rising from the all-fours position. |
| Ulbrich et al. (2000) [44]; US | To describe how older adults, particularly more physically impaired older adults, might differ from healthy young adults in the body positions used to rise from the floor. | OBS/NP; 22 (♀ = 11) young adult controls, age range = 19–30 yrs. (mean age = 23 ± 3; yrs.), 24 (♀ = 12) healthy older adults, age range = 66–87 yrs. (mean age = 73 ± 6 yrs.), and 29 (♀ = 29) congregate housing older adults, age range = 63–94 yrs. (mean age = 81 ± 7 yrs.) | Product—STS time(s); Process—Intermediate Position (IP): sit, crouch, side-lying, tuck, half-tuck, kneel, half-kneel, crouch-kneel, all fours, bear walk. | - | Congregate residents were slowest in rising (17.1 s) and used the most IP, followed by healthy older adults (5.5 s) and young controls (2.6 s). The most preferred rise strategy used by controls was sat and crouch, whereas congregate residents used tuck, crouch-kneel, all fours, and bear walk; healthy older adults used IPs common to young adults and congregates |
| Bohannon and Lusardi (2004) [33]; US | (1) To explore the relationship between STS performance and age, functional lower extremity strength, and balance; and (2) to describe movement strategies used by healthy older adults when getting up from the floor. | OBS/NP; 52 (♀ = 38) healthy and independent community-living volunteers, age range = 50–90 yrs. (mean age = 64.6 ± 9.5 yrs.). There was a relatively equal distribution of participants across decades of ages within the sample. | Product—STS time (s); Process—three distinct stages: Initiation, transitional weight transfer, and going to upright posture, and there were some strategies in each stage. | Muscle strength: Time to complete five sit-to-stand cycles. Balance: Timed (s) single limb stance with eyes open (up to 30 s) both sides. | STS time = 4.1 ± 1.1 s, ranging from 1.8 to 7.2 s; Correlations: STS time and age, r = 0.48; STS time and sit and stand test, r = 0.64; STS time and single right stance, r = −0.36; STS and left single stance, r = −0.42; STS performance may be enhanced by training that addresses impairments in lower extremity strength and balance. |
| Schwickert et al. (2015) [23]; Germany | (1) To develop a model of MP sequences for unassisted STS task from different lying positions; (2) to identify differences in the MPs and transfer times of healthy older adults compared to healthy young adults, and identify difficulties in the MPs of older adults; and (3) to verify the associations with executive function, power, and flexibility. | OBS/NP; 14 (♀ = 7) young adults, age range = 19–39 yrs., and 10 (♀ = 5) older adults, age range = 59–79 yrs. | Product—STS time (s); Process—type and number of components to perform the STS task in a naturalistic scenario and a standardized scenario. | Trail making test; maximum gait speed 4 m distance, 30 s chair rise, Romberg test, Nottingham power rig, chair sit-and-reach test, goniometry. | Seven task components were noted: Lying, initiation, positioning, supporting, and elevation stabilization followed by quiet stance or walking; older adults = 5.7 s vs. young adults = 3.7 s (p < 0.001). There was a reduction in STS performance in older subjects, which was associated with reduced power and flexibility. Executive function, leg and hip power, and knee flexibility were lower in the older adult group. The scenario type did not influence the number of STS task components. |
| Schwickert et al. (2016) [45]; Germany | To analyze different kinematic features of standing up from the floor in adults and healthy older adults using inertial sensors describing such transfer patterns. | OBS/NP; 14 (♂ = 7) adults, age range = 20–50 yrs., and 10 (♂ = 5) healthy older community dwellers aged ≥60 yrs. | Product—Transfer time (s); transfer angular velocity; vertical velocity and acceleration; jerk Process—smoothness, fluency, and complexity of movement strategies. | - | The motion sequences of the older adults were less fluent and smooth than in the younger group; older subjects used more indirect movement strategies, including more turns around the longitudinal axis to prepare for elevation. There was the feasibility of describing and discriminating the performance kinematics of younger and older subjects standing up from the floor from different lying postures, using inertial sensor signals at the trunk. |
| Elderly | |||||
| Schenkman et al. [46] (2000); US | To determine (a) the associations between spinal flexibility and functional limitations; (b) the relative contribution of spinal flexibility to specific functional limitations; and (c) how disease state (PD vs. no PD) modified these relationships | OBS/NP; n total = 251; 56 older adults with PD (♀ = 24,5%) (mean age = 70.7 ± 7.4 yrs.); 195 non-PD (mean age = 71.4 ± 5.0 yrs.) | Product—STS time (s); | Spinal flexibility; functional reach distance; 10-m walk time; number of steps to turn 360° | PD older adults, STS time = 7.2 ± 3.7; non-PD older adults, STS time = 5.2 ± 2.0. Spinal flexibility was a significant predictor of supine-to-stand time and the number of steps in the 360 degrees turn, but there was no clinical significance for these two variables |
| Bergland et al. (2002) [15]; Norway | To evaluate the concurrent and prospective validity of self-reported items concerning walking and balance. | OBS/Probabilistic, longitudinal, and predictive; 307 elderly women, living at home, age range = 75–93 yrs. (mean age = 80.8 yrs.). | Product—scored according to whether the subject managed to perform the STS task without assistance (1 point) or not (0 points). | Tandem stance/eyes open; functional reach; one-legged stance/eyes open; walking in figure-eight; climbing stairs; self-reported walking difficulties. | About 80% of the women managed to perform the STS task and could cope with steps higher than 30 cm; younger subjects performed better than those in the higher age bands in all tests; all clinical tests correlated significantly with each other (range = 0.25–0.85) and also with the self-reported walking index (range = 0.32–0.62). |
| Hofmeyer et al. (2002) [20]; US | To determine the effect of a 2-week training intervention to improve disabled older adults’ ability to rise from the floor. | Interventional/Random allocation; healthy older adults. Training group (n = 17, ♀ = 13; mean age = 81 ± 6 yrs.) submitted to an individual training in strategies to rise from the floor using key body positions; control group (n = 18, ♀ = 13; mean age = 80 ± 7 yrs.) submitted to an chair-based flexibility intervention. | Product 1—able or not able to perform the STS task in eight different conditions; Product 2—STS time. | The Perceived Scale of Symptoms and Difficulties. | The training group showed a significant improvement in the post-test mean number of rising tasks completed; regarding the supine position, the mean rise time varied from 21–25 s at baseline to 20–27 s post-intervention, but such improvement was not significant. The training group showed a significant improvement in the level of difficulties and symptoms. |
| Bergland et al. (2004) [16]; Norway | To verify whether balance, function, and other health status indicators can predict serious fall-related injuries or fall-induced fractures in older women. | OBS/Probabilistic, longitudinal, and predictive; 307 women, age range = 75–93 yrs. (mean age = 80.8 yrs.) who were living at home. | Product—scored whether the subject managed to perform the tasks without assistance (1 point) or not (0 points). | Other measures: Serious fall injuries over a year, health records, function, and walking and balance | Rheumatic disorders and the inability to perform STS task were the most substantial independent risk factors for fall-related severe injuries. |
| Henwood et al. (2005) [47]; Australia | To investigate the effects of a short-term high-velocity varied resistance training program on physical performance in healthy community-dwelling older adults aged 60 to 80 years. | Interventional/NP; 25 healthy community-dwelling men and women, age range = 60–80 yrs.; they were divided in two groups: Experimental (n = 14; 69.9 ± 6.5 yrs.) and control group (n = 10; 71.3 ± 5.6 yrs.). | Product—STS time (s). | Muscle power and strength measures: Chair rise to standing, 6-m walk, lift and reach; BMI and percentage of body fat. | In Baseline, Experimental group STS time = 4.5 ± 0.8 s; control group STS time = 3.8 ± 0.9 s; after training there was 10.4% reduction in time in the experimental group from the baseline (p = 0.006). There was a group X time interaction for floor rise to standing (experimental group). There was no change in body composition during the study. |
| Bergland et al. (2005) [17]; Norway | To assess the concurrent and predictive validity of older women’s ability to get up from lying on the floor. | OBS/Probabilistic; predictive; 307 elderly women, age range = 75–93 yrs. (mean age = 80.8 yrs.) who were living at home. | Product—scored whether the subject managed to perform the tasks without assistance (1 point) or not (0 points). | Falls and falls-related injuries, function measures, and health and social resources. | The STS task is a valid marker of failing health and function in older adults and a significant predictor of serious fall-related injuries. |
| Manini et al. (2006) [40]; US | Develop a task modification scale to examine its reliability and comparability to timed performance and standard measures of physical function and impairment in older adults | OBS/NP; 82 (♀ = 21) older adults (mean age = 74.4 ± 8.2 yrs.) | Product—STS timeProcess—MOD Score | Gait speed (fast and regular), five chair rises, self-reported physical function, knee extensor strength, and single-leg balance. | The MOD score is reliable across raters and repeatable within participants; also, it showed higher correlations with muscle strength and balance impairment than did other measures as gait speed, time to complete five chair stands, and self-reported physical function. |
| Mankoundia et al. (2007) [48]; France | To determine whether the management, including medical, psychological and physiotherapeutic approaches may be beneficial in the short and medium-term, for elderly fallers with psychomotor disadaptation syndrome. | Interventional/NP; longitudinal; 28 (♀ = 25) elderly fallers (mean age = 81.43 ± 6.7 yrs.). | Product—STS time (s) | Functional Independence Measure, Mini Mental State Examination, Tinetti test, Mini Motor test, Dual Task test, Beck Depression Inventory-II, Covi Scale, Modified-Falls Efficacy Scale | The multidisciplinary intervention had an overall positive impact on motor abilities as shown by the increase in the mini-motor test scores, the rate of success in rising from the floor and decrease of time for the dual task. |
| Manckoundia et al. (2008) [38]; France | Identifying the demographic and clinical parameters, assessed during a standard health examination, affects balance control in older adults. | OBS/NP; 2368 (♀ = 1215) older adults (mean age = 70.0 ± 4.5 yrs.). | Product—able or unable to perform the STS task. | Age, gender, BMI, cognitive status, self-perception of health, and use of psychotropic drugs | Women (8%) failed more than men (2.7%) in the STS task. Women who failed in the STS task had higher diastolic blood pressure and glycemia; BMI and health scores determined errors in the STS task in both genders. The BMI was a significant determinant of performance in all balance tests. |
| Geraldes et al. (2008) [49]; Brazil | To investigate the relationship between flexibility of flexion and extension of the glenohumeral and coxofemoral joints and functional performance among physically active and functionally independent elderly women. | OBS/NP/22 functionally independent elderly women mean (age 70 ± 6 yrs) | Product-STS time (s). | Flexibility of the glenohumeral and hip joints | There was a significant association between assisted-active flexibility and STS performance. |
| Naugle et al. (2012) [37]; US | To examine the association between compensatory strategies to successfully daily activities and body mass in pre-clinically disabled older adults. | OBS/NP; 259 (♀ = 116) older adults (mean age = 67.6 ± 7.0 yrs). | Process—MOD Score evaluated (0 to 5 points) participants’ performance on each task according to the severity of the compensatory strategy to complete the task. | Chair rise from three heights (43, 38, and 30 cm), kneel to stand, stair ascent, stair descent, and lift and carry a basket filled with 10% of the subject’s BMI. | The obese class II group had a higher likelihood of using one or more compensatory strategies while performing the STS task compared to all other groups. Individuals categorized as overweight and obese Class-I were more likely to use compensatory strategies while performing the STS task than the healthy weight group. |
| Raso and Greve (2012) [50]; Brazil | To determine the effect of an aerobic or resistance exercise protocol on the performance of daily living activities in older women. | Interventional/NP/random allocation; 41 healthy elderly women, age range = 60–85 yrs. (mean age = 65.1 ± 7.9 yrs.) randomly assigned to resistance (n = 22) or aerobic exercise (n = 19). | Product—STS velocity (s). | Performance in these tasks was measured while subjects were wearing sneakers: Sitting to standing position, STS task, and climbing stairs. | Subjects of the aerobic exercise protocol improved speed significantly when wearing sneakers, while subjects of the resistance exercise protocol improved their performance in the STS task and climbing stairs when using these shoes. |
| Klima et al. (2016) [39]; US | To examine physical performance correlates of timed supine to standing performance, Furthermore, to identify the predominant motor pattern used to complete rising from the floor. | OBS/NP; 53 (♀ = 36) older adults (mean age = 78.5 ± 8.5 yrs.). | Product—STS time (s); Process (symmetrical rise and squat sequence or symmetrical rise and asymmetrical squat sequence or roll and push maneuver). | Handgrip, balance, 9-m walk test, TUG test; Physical Activity Scale for Elderly | STS time was associated with age (r = 0.57), gait velocity (r = −0.61), ABC scores (r = −0.51); there were correlations with physical activity (Rho = −0.29), grip strength (r = −0.30); and with the TUG test (r = 0.71). Hierarchical regression demonstrated that TUG performance predicted 48% of the variance in STS time (p < 0.001). This significance remained after adjusting for age and BMI covariates. |
| Manckoundia et al. (2020) [51]; France | To investigate the impact of an ambulatory physical activity program on the motor skills of retirees | Interventional, not controlled study/NP. N total = 200 living home healthy older adults (♀ = 172), age range = 60–100 yrs. (mean age = 73.8 ± 7.4 yrs.). They were divided into two groups for STS task: Robust subjects vs. frail or very frail subjects. The program included strengthening muscular and joint flexibility exercises, balance work, one-leg-balance test, stimulation of the foot arch, STS task, TUG, gait speed, one-leg-balance | Product—able or unable to perform the STS task. | One-leg-balance test, TUG, gait speed, one-leg-balance test duration | For STS, 81% of participants did not change groups after training program, 18.5% changed from (very) frail to robust, and 0.5% of subjects changed from robust to (very) frail. |
| Moffett et al. (2020) [52]; US | To describe the performance and clinimetric properties STS completed by apparently healthy community-dwelling older women | OBS/methodological quality study; 52 ♀ (mean age = 66.4 ± 8.1 yrs) | Product—STS time (s) | 36-Short Form Health Survey, Gait Speed test, Sit-To-Stand test, Johns Hopkins Fall Risk Assessment | STS test appears to be informative, valid, and reliable, at least for older independent women. |
| N | f (%) | ||
|---|---|---|---|
| Quality of study | Superior–Low risk of bias (≥ 12) | 18 | 64.9 |
| Medium–Moderate risk of bias (8 to 11) | 13 | 35.1 | |
| Inferior–High risk of bias (≤ 7) | 0 | 0.00 | |
| Number of trials * | Only one trial | 7 | 18.9 |
| 2 to 5 trials | 12 | 32.4 | |
| 6 to 10 trials | 10 | 27.0 | |
| Above 10 trials | 2 | 5.4 | |
| Instruction for performance speed | “As fast as possible” | 18 | 48.6 |
| Comfortable speed | 14 | 37.8 | |
| Not informed | 4 | 10.8 | |
| Participant’s caring * | Use of the test trail | 32 | 86.5 |
| Rest interval | 11 | 29.7 | |
| Demonstration | 6 | 16.2 | |
| Use of the assistants | 6 | 16.2 | |
| Motivational strategies * | Feedbacks | 3 | 8.1 |
| Rewards | 1 | 2.7 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cattuzzo, M.T.; de Santana, F.S.; Safons, M.P.; Ré, A.H.N.; Nesbitt, D.R.; Santos, A.B.D.; Feitoza, A.H.P.; Stodden, D.F. Assessment in the Supine-To-Stand Task and Functional Health from Youth to Old Age: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 5794. https://doi.org/10.3390/ijerph17165794
Cattuzzo MT, de Santana FS, Safons MP, Ré AHN, Nesbitt DR, Santos ABD, Feitoza AHP, Stodden DF. Assessment in the Supine-To-Stand Task and Functional Health from Youth to Old Age: A Systematic Review. International Journal of Environmental Research and Public Health. 2020; 17(16):5794. https://doi.org/10.3390/ijerph17165794
Chicago/Turabian StyleCattuzzo, Maria Teresa, Frederico Santos de Santana, Marisete Peralta Safons, Alessandro Hervaldo Nicolai Ré, Danielle Rene Nesbitt, Ariane Brito Diniz Santos, Anderson Henry Pereira Feitoza, and David Franklin Stodden. 2020. "Assessment in the Supine-To-Stand Task and Functional Health from Youth to Old Age: A Systematic Review" International Journal of Environmental Research and Public Health 17, no. 16: 5794. https://doi.org/10.3390/ijerph17165794
APA StyleCattuzzo, M. T., de Santana, F. S., Safons, M. P., Ré, A. H. N., Nesbitt, D. R., Santos, A. B. D., Feitoza, A. H. P., & Stodden, D. F. (2020). Assessment in the Supine-To-Stand Task and Functional Health from Youth to Old Age: A Systematic Review. International Journal of Environmental Research and Public Health, 17(16), 5794. https://doi.org/10.3390/ijerph17165794








