COVID-19 Global Risk: Expectation vs. Reality
Abstract
1. Introduction
2. Method
2.1. Data Collection
2.2. Modelling Techniques
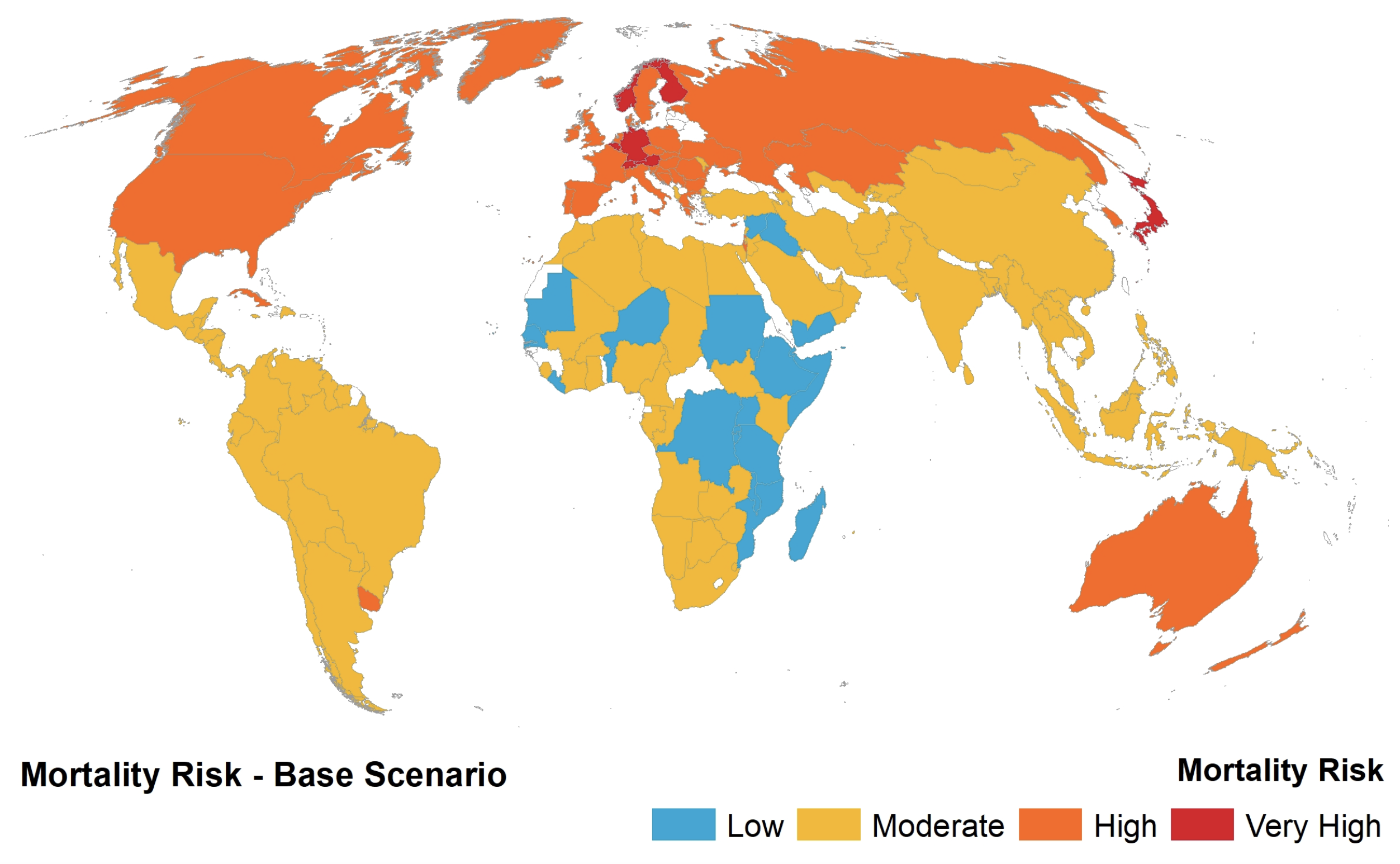
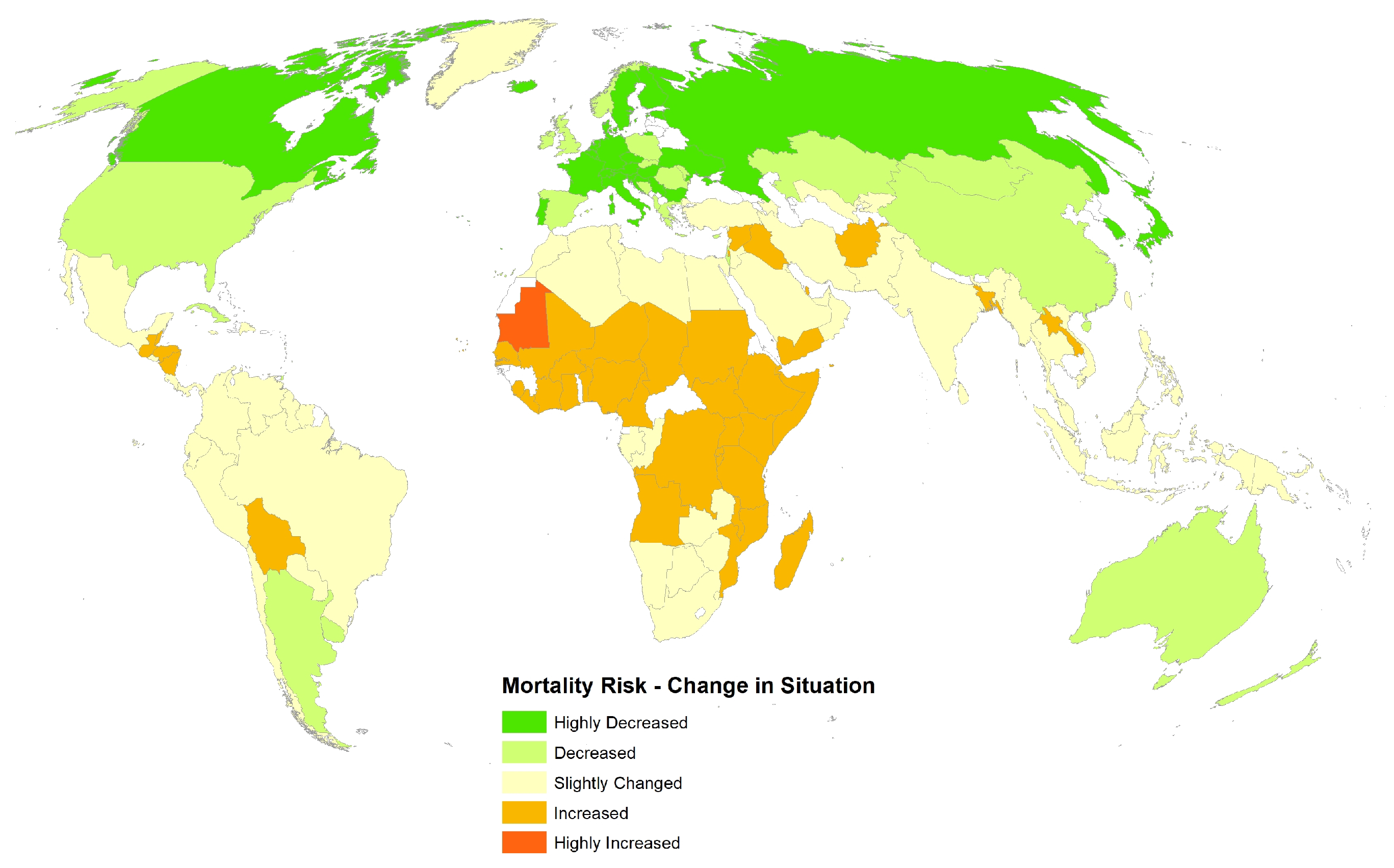
3. Results
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Pica, N.; Bouvier, N.M. Environmental factors affecting the transmission of respiratory viruses. Curr. Opin. Virol. 2012, 2, 90–95. [Google Scholar] [CrossRef] [PubMed]
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef] [PubMed]
- Hopkins, J. Coronavirus COVID-19 Global Cases by Johns Hopkins CSSE [Internet]. Available online: https://coronavirus.jhu.edu/data (accessed on 14 May 2020).
- Fernandes, N. Economic effects of coronavirus outbreak (COVID-19) on the world economy. Available SSRN 3557504 2020. [Google Scholar] [CrossRef]
- Anderson, R.M.; Heesterbeek, H.; Klinkenberg, D.; Hollingsworth, T.D. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet 2020, 395, 931–934. [Google Scholar] [CrossRef]
- Jones, K.E.; Patel, N.G.; Levy, M.A.; Storeygard, A.; Balk, D.; Gittleman, J.L.; Daszak, P. Global trends in emerging infectious diseases. Nature 2008, 451, 990–993. [Google Scholar] [CrossRef]
- Cox, N.J.; Trock, S.C.; Burke, S.A. Pandemic preparedness and the influenza risk assessment tool (IRAT). In Influenza Pathogenesis and Control-Volume I; Springer: Cham, Switzerland, 2014; pp. 119–136. [Google Scholar]
- Rocklöv, J.; Sjödin, H. High population densities catalyse the spread of COVID-19. J. Travel Med. 2020, 27, taaa038. [Google Scholar] [CrossRef]
- Duggal, A.; Pinto, R.; Rubenfeld, G.; Fowler, R.A. Global variability in reported mortality for critical illness during the 2009-10 influenza A (H1N1) pandemic: A systematic review and meta-regression to guide reporting of outcomes during disease outbreaks. PLoS ONE 2016, 11, e0155044. [Google Scholar] [CrossRef]
- Blumenshine, P.; Reingold, A.; Egerter, S.; Mockenhaupt, R.; Braveman, P.; Marks, J. Pandemic influenza planning in the United States from a health disparities perspective. Emerg. Infect. Dis. 2008, 14, 709. [Google Scholar] [CrossRef]
- Hu, W.; Williams, G.; Phung, H.; Birrell, F.; Tong, S.; Mengersen, K.; Huang, X.; Clements, A. Did socio-ecological factors drive the spatiotemporal patterns of pandemic influenza A (H1N1)? Environ. Int. 2012, 45, 39–43. [Google Scholar] [CrossRef]
- Summers, J.A.; Wilson, N.; Baker, M.G.; Shanks, G.D. Mortality risk factors for pandemic influenza on New Zealand troop ship, 1918. Emerg. Infect. Dis. 2010, 16, 1931. [Google Scholar] [CrossRef]
- Lönnroth, K.; Jaramillo, E.; Williams, B.G.; Dye, C.; Raviglione, M. Drivers of tuberculosis epidemics: The role of risk factors and social determinants. Soc. Sci. Med. 2009, 68, 2240–2246. [Google Scholar] [CrossRef] [PubMed]
- Pellowski, J.A.; Kalichman, S.C.; Matthews, K.A.; Adler, N. A pandemic of the poor: Social disadvantage and the US HIV epidemic. Am. Psychol. 2013, 68, 197. [Google Scholar] [CrossRef]
- Ajisegiri, W.S.; Chughtai, A.A.; MacIntyre, C.R. A risk analysis approach to prioritizing epidemics: Ebola virus disease in West Africa as a case study. Risk Anal. 2018, 38, 429–441. [Google Scholar] [CrossRef]
- Swinburn, B.A.; Sacks, G.; Hall, K.D.; McPherson, K.; Finegood, D.T.; Moodie, M.L.; Gortmaker, S.L. The global obesity pandemic: Shaped by global drivers and local environments. Lancet 2011, 378, 804–814. [Google Scholar] [CrossRef]
- The, L. Redefining vulnerability in the era of COVID-19. Lancet 2020, 395, 1089. [Google Scholar]
- Qiu, Y.; Chen, X.; Shi, W. Impacts of Social and Economic Factors on the Transmission of Coronavirus Disease 2019 (COVID-19) in China. Technical Report, GLO Discussion Paper. 2020. Available online: https://link.springer.com/article/10.1007/s00148-020-00778-2 (accessed on 31 July 2020).
- Mogi, R.; Spijker, J. The influence of social and economic ties to the spread of COVID-19 in Europe 2020. Available online: https://osf.io/preprints/socarxiv/sb8xn/ (accessed on 22 July 2020).
- Gilbert, M.; Pullano, G.; Pinotti, F.; Valdano, E.; Poletto, C.; Boëlle, P.Y.; d’Ortenzio, E.; Yazdanpanah, Y.; Eholie, S.P.; Altmann, M.; et al. Preparedness and vulnerability of African countries against importations of COVID-19: A modelling study. Lancet 2020, 395, 871–877. [Google Scholar] [CrossRef]
- Zanakis, S.H.; Alvarez, C.; Li, V. Socio-economic determinants of HIV/AIDS pandemic and nations efficiencies. Eur. J. Oper. Res. 2007, 176, 1811–1838. [Google Scholar] [CrossRef]
- The World Bank Development Indicators. 2020. Available online: https://databank.worldbank.org/source/world-development-indicators (accessed on 14 May 2020).
- Global Burden of Disease Collaborative Network. In Global Burden of Disease Study 2016 (GBD 2016) Results; Institute for Health Metrics and Evaluation: Seattle, WA, USA, 2017.
- Center for International Earth Science Information Network–CIESIN–Columbia University. Gridded Population of the World, Version 4 (GPWv4): Population Density; Columbia University: Palisades, NY, USA, 2016. [Google Scholar]
- Hale, T.; Webster, S.; Petherick, A.; Phillips, T.; Kira, B. Oxford COVID-19 Government Response Tracker. Available online: https://www.bsg.ox.ac.uk/research/research-projects/oxford-covid-19-government-response-tracker (accessed on 26 March 2020).
- Stojkoski, V.; Utkovski, Z.; Jolakoski, P.; Tevdovski, D.; Kocarev, L. The socio-economic determinants of the coronavirus disease (COVID-19) pandemic. arXiv 2020, arXiv:2004.07947. [Google Scholar]
- Esteve, A.; Permanyer, I.; Boertien, D.; Vaupel, J.W. National age and co-residence patterns shape covid-19 vulnerability. medRxiv 2020. [Google Scholar] [CrossRef]
- Guarini, M.R.; Battisti, F.; Chiovitti, A. A methodology for the selection of multi-criteria decision analysis methods in real estate and land management processes. Sustainability 2018, 10, 507. [Google Scholar] [CrossRef]
- Box, G.E.; Cox, D.R. An analysis of transformations. J. R. Stat. Soc. Ser. B (Methodol.) 1964, 26, 211–243. [Google Scholar] [CrossRef]
- Peterson, R.A.; Peterson, M.R.A. Package ‘bestNormalize’. 2017. Available online: https://github.com/petersonR/bestNormalize (accessed on 14 May 2020).
- Saaty, T.L. Decision making with the analytic hierarchy process. Int. J. Serv. Sci. 2008, 1, 83–98. [Google Scholar] [CrossRef]
- Topuz, E.; Talinli, I.; Aydin, E. Integration of environmental and human health risk assessment for industries using hazardous materials: A quantitative multi criteria approach for environmental decision makers. Environ. Int. 2011, 37, 393–403. [Google Scholar] [CrossRef] [PubMed]
- Kull, T.J.; Talluri, S. A supply risk reduction model using integrated multicriteria decision making. IEEE Trans. Eng. Manag. 2008, 55, 409–419. [Google Scholar] [CrossRef]
- Grömping, U. Relative importance for linear regression in R: The package relaimpo. J. Stat. Softw. 2006, 17, 1–27. [Google Scholar]
- Bharati, T.; Fakir, A. Pandemic Catch-22: How Effective Are Mobility Restrictions in Halting the Spread of COVID-19? Technical Report; The University of Western Australia: Perth, Australia, 2020. [Google Scholar]
- Dowd, J.B.; Andriano, L.; Brazel, D.M.; Rotondi, V.; Block, P.; Ding, X.; Liu, Y.; Mills, M.C. Demographic Science Aids in Understanding the Spread and Fatality Rates of COVID-19. Proc. Nat. Acad. Sci. USA 2020, 117, 9696–9698. [Google Scholar] [CrossRef] [PubMed]
- Barmparis, G.D.; Tsironis, G. Estimating the infection horizon of COVID-19 in eight countries with a data-driven approach. Chaos Solitons Fractals 2020, 135, 109842. [Google Scholar] [CrossRef]
- Miller, A.; Reandelar, M.J.; Fasciglione, K.; Roumenova, V.; Li, Y.; Otazu, G.H. Correlation between universal BCG vaccination policy and reduced morbidity and mortality for COVID-19: An epidemiological study. medRxiv 2020. [Google Scholar] [CrossRef]

| Variable | Weight |
|---|---|
| Average Population Density | 0.027 |
| Population | 0.039 |
| Health Expenditure | 0.058 |
| GDP | 0.09 |
| DALY | 0.157 |
| Nurses | 0.157 |
| Physicians | 0.157 |
| Hospital Beds | 0.157 |
| A65abp | 0.157 |
| Consistency Ratio < 0.01 |
| Regression Model | Significant p-Values | Top Weights | |
|---|---|---|---|
| Static factors | 0.69 | A65abp *** | A65abp (0.19), GDP (0.22) |
| Static and dynamic factors | 0.88 | A65abp ***, nurses *, susceptible *, active ***, mortality growth ** | active (0.20), susceptibles (0.15), mortality growth (0.11), A65abp (0.10) |
| Country Name | Mortality Rate (Actual) | Pre-COVID-19 Mortality Risk Rank (Predicted) | COVID-19 Mortality Risk Rank as at 13 May 2020 (Predicted) |
|---|---|---|---|
| San Marino | 1213.6 | 41 | 3 |
| Belgium | 774.2 | 7 | 8 |
| Andorra | 636.3 | 46 | 60 |
| Spain | 580.1 | 35 | 41 |
| Italy | 514.1 | 14 | 17 |
| United Kingdom | 499.1 | 25 | 16 |
| France | 403.5 | 11 | 13 |
| Sweden | 339.8 | 9 | 11 |
| Netherlands | 322.8 | 10 | 12 |
| Ireland | 308.4 | 27 | 33 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Arsalan, M.; Mubin, O.; Alnajjar, F.; Alsinglawi, B. COVID-19 Global Risk: Expectation vs. Reality. Int. J. Environ. Res. Public Health 2020, 17, 5592. https://doi.org/10.3390/ijerph17155592
Arsalan M, Mubin O, Alnajjar F, Alsinglawi B. COVID-19 Global Risk: Expectation vs. Reality. International Journal of Environmental Research and Public Health. 2020; 17(15):5592. https://doi.org/10.3390/ijerph17155592
Chicago/Turabian StyleArsalan, Mudassar, Omar Mubin, Fady Alnajjar, and Belal Alsinglawi. 2020. "COVID-19 Global Risk: Expectation vs. Reality" International Journal of Environmental Research and Public Health 17, no. 15: 5592. https://doi.org/10.3390/ijerph17155592
APA StyleArsalan, M., Mubin, O., Alnajjar, F., & Alsinglawi, B. (2020). COVID-19 Global Risk: Expectation vs. Reality. International Journal of Environmental Research and Public Health, 17(15), 5592. https://doi.org/10.3390/ijerph17155592







