What Happened to People with Non-Communicable Diseases during COVID-19: Implications of H-EDRM Policies
Abstract
1. Introduction
2. Materials and Methods
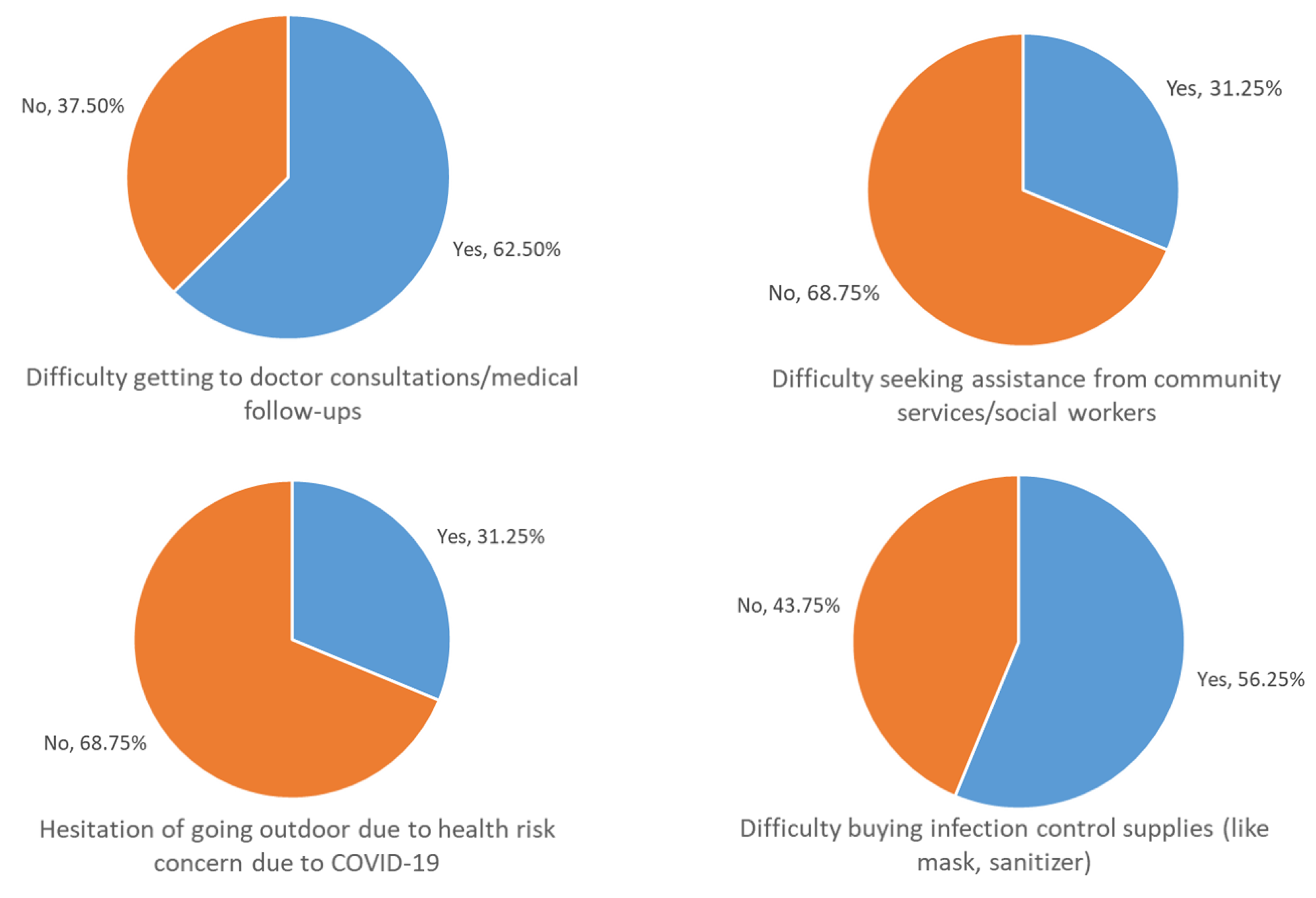
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Chan, E.Y.Y. Public Health Humanitarian Responses to Natural Disasters; Routledge: Abingdon, UK, 2017. [Google Scholar]
- World Health Organization. United Kingdom Health Protection Agency & Partners. Disaster Risk Management for Health: Non-Communicable Diseases. Available online: http://www.who.int/entity/hac/events/drm_fact_sheet_non_communicable_diseases.pdf?ua=1 (accessed on 18 June 2020).
- World Health Organization. Health Emergency and Disaster Risk Management (Health-EDRM) Framework. Available online: https://www.who.int/hac/techguidance/preparedness/health-emergency-and-disaster-risk-management-framework-eng.pdf?ua=1 (accessed on 18 June 2020).
- Guan, W.-J.; Liang, W.-H.; Zhao, Y.; Liang, H.-R.; Chen, Z.-S.; Li, Y.-M.; Liu, X.-Q.; Chen, R.-C.; Tang, C.-L.; Wang, T.; et al. Comorbidity and its impact on 1590 patients with COVID-19 in China: A nationwide analysis. Eur. Respir. J. 2020, 55, 2000547. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Zheng, Y.; Gou, X.; Pu, K.; Chen, Z.; Guo, Q.; Ji, R.; Wang, H.; Wang, Y.; Zhou, Y. Prevalence of comorbidities and its effects in coronavirus disease 2019 patients: A systematic review and meta-analysis. Int. J. Infect. Dis. 2020, 94, 91–95. [Google Scholar] [CrossRef] [PubMed]
- Richardson, S.; Hirsch, J.S.; Narasimhan, M.; Crawford, J.M.; McGinn, T.; Davidson, K.W.; Barnaby, D.P.; Becker, L.B.; Chelico, J.D.; Cohen, S.L.; et al. Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area. JAMA 2020, 323, 2052. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. COVID-19 and NCD: Information note on COVID-19 and noncommunicable diseases. Available online: https://www.who.int/docs/default-source/inaugural-who-partners-forum/covid-19-and-ncds---final---corr7.pdf?sfvrsn=9b65e287_1&download=true (accessed on 18 June 2020).
- Kluge, H.H.P.; Wickramasinghe, K.; Rippin, H.L.; Mendes, R.; Peters, D.H.; Kontsevaya, A.; Breda, J. Prevention and control of non-communicable diseases in the COVID-19 response. Lancet 2020, 395, 1678–1680. [Google Scholar] [CrossRef]
- Chan, E.Y.Y.; Huang, Z.; Lo, E.S.K.; Hung, K.; Wong, E.L.-Y.; Wong, M.C. Sociodemographic Predictors of Health Risk Perception, Attitude and Behavior Practices Associated with Health-Emergency Disaster Risk Management for Biological Hazards: The Case of COVID-19 Pandemic in Hong Kong, SAR China. Int. J. Environ. Res. Public Health 2020, 17, 3869. [Google Scholar] [CrossRef] [PubMed]
- Ryan, D.H.; Ravussin, E.; Heymsfield, S. COVID 19 and the Patient with Obesity—The Editors Speak Out. Obesity 2020, 28, 847. [Google Scholar] [CrossRef] [PubMed]
- Chan, E.Y.Y.; Cheng, C.K.Y.; Tam, G.; Huang, Z.; Lee, P. Knowledge, attitudes, and practices of Hong Kong population towards human A/H7N9 influenza pandemic preparedness, China, 2014. BMC Public Health 2015, 15, 943. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Shortage of Personal Protective Equipment Endangering Health Workers Worldwide. Available online: https://www.who.int/news-room/detail/03-03-2020-shortage-of-personal-protective-equipment-endangering-health-workers-worldwide (accessed on 9 July 2020).
- Wu, C.; Liu, Y.; Ohannessian, R.; Duong, T.; Odone, A. Global Telemedicine Implementation and Integration Within Health Systems to Fight the COVID-19 Pandemic: A Call to Action. JMIR Public Health Surveill. 2020, 6, e18810. [Google Scholar] [CrossRef]
- Chan, E.Y.Y.; Hung, H. Key Public Health Challenges for Health-EDRM in the Twenty-First Century: Demographic and Epidemiological Transitions. In Disaster Risk Reduction; Springer Science and Business Media LLC: Berlin, Germany, 2020; pp. 19–38. [Google Scholar]
- Arrieta, M.I.; Foreman, R.D.; Crook, E.D.; Icenogle, M.L. Insuring Continuity of Care for Chronic Disease Patients After a Disaster: Key Preparedness Elements. Am. J. Med. Sci. 2008, 336, 128–133. [Google Scholar] [CrossRef] [PubMed]
- Ochi, S.; Hodgson, S.; Landeg, O.; Mayner, L.; Murray, V. Disaster-Driven Evacuation and Medication Loss: A Systematic Literature Review. PLoS Curr. 2014, 6. [Google Scholar] [CrossRef] [PubMed]
- Chan, E.Y.Y.; Sondorp, E. Medical Interventions following Natural Disasters: Missing out on Chronic Medical Needs. Asia Pac. J. Public Health 2007, 19, 45–51. [Google Scholar] [CrossRef] [PubMed]
| Perceived No Difficulty (n = 125) | Perceived Difficulty (n = 16) | p-Value | |
|---|---|---|---|
| Gender | 0.394 | ||
| Male | 48.8% | 37.5% | |
| Female | 51.2% | 62.5% | |
| Age a | 0.307 | ||
| 18–24 | 3.2% | 0.0% | |
| 25–44 | 7.2% | 18.8% | |
| 45–64 | 45.6% | 31.3% | |
| 65 or above | 44.0% | 50.0% | |
| Education attainment a | 0.087 | ||
| Primary level or below | 14.5% | 18.8% | |
| Secondary level | 54.0% | 75.0% | |
| Tertiary level | 31.5% | 6.3% | |
| Living alone a | 0.224 | ||
| Not living alone | 85.6% | 100.0% | |
| Living alone | 14.4% | 0.0% | |
| Employment group a | 0.289 | ||
| White collar | 24.2% | 6.3% | |
| Blue collar | 14.5% | 31.3% | |
| Housewives | 20.2% | 25.0% | |
| Students | 1.6% | 0.0% | |
| Unemployment or retired | 39.5% | 37.5% | |
| Housing type a | 0.012 * | ||
| Public housing | 32.0% | 18.8% | |
| Government subsidized housing | 10.4% | 31.3% | |
| Private housing | 57.6% | 43.8% | |
| Others | 0.0% | 6.3% | |
| Monthly h ousehold income (HK$) a,b | 0.018 * | ||
| < 8000 | 22.8% | 12.5% | |
| 8000–19999 | 25.4% | 62.5% | |
| 20000–39999 | 20.2% | 18.8% | |
| 40000 or more | 31.6% | 6.3% |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chan, E.Y.Y.; Kim, J.H.; Lo, E.S.K.; Huang, Z.; Hung, H.; Hung, K.K.C.; Wong, E.L.Y.; Lee, E.K.P.; Wong, M.C.S.; Wong, S.Y.S. What Happened to People with Non-Communicable Diseases during COVID-19: Implications of H-EDRM Policies. Int. J. Environ. Res. Public Health 2020, 17, 5588. https://doi.org/10.3390/ijerph17155588
Chan EYY, Kim JH, Lo ESK, Huang Z, Hung H, Hung KKC, Wong ELY, Lee EKP, Wong MCS, Wong SYS. What Happened to People with Non-Communicable Diseases during COVID-19: Implications of H-EDRM Policies. International Journal of Environmental Research and Public Health. 2020; 17(15):5588. https://doi.org/10.3390/ijerph17155588
Chicago/Turabian StyleChan, Emily Ying Yang, Jean Hee Kim, Eugene Siu Kai Lo, Zhe Huang, Heidi Hung, Kevin Kei Ching Hung, Eliza Lai Yi Wong, Eric Kam Pui Lee, Martin Chi Sang Wong, and Samuel Yeung Shan Wong. 2020. "What Happened to People with Non-Communicable Diseases during COVID-19: Implications of H-EDRM Policies" International Journal of Environmental Research and Public Health 17, no. 15: 5588. https://doi.org/10.3390/ijerph17155588
APA StyleChan, E. Y. Y., Kim, J. H., Lo, E. S. K., Huang, Z., Hung, H., Hung, K. K. C., Wong, E. L. Y., Lee, E. K. P., Wong, M. C. S., & Wong, S. Y. S. (2020). What Happened to People with Non-Communicable Diseases during COVID-19: Implications of H-EDRM Policies. International Journal of Environmental Research and Public Health, 17(15), 5588. https://doi.org/10.3390/ijerph17155588








