Thermotherapy Plus Neck Stabilization Exercise for Chronic Nonspecific Neck Pain in Elderly: A Single-Blinded Randomized Controlled Trial
Abstract
1. Introduction
2. Methods
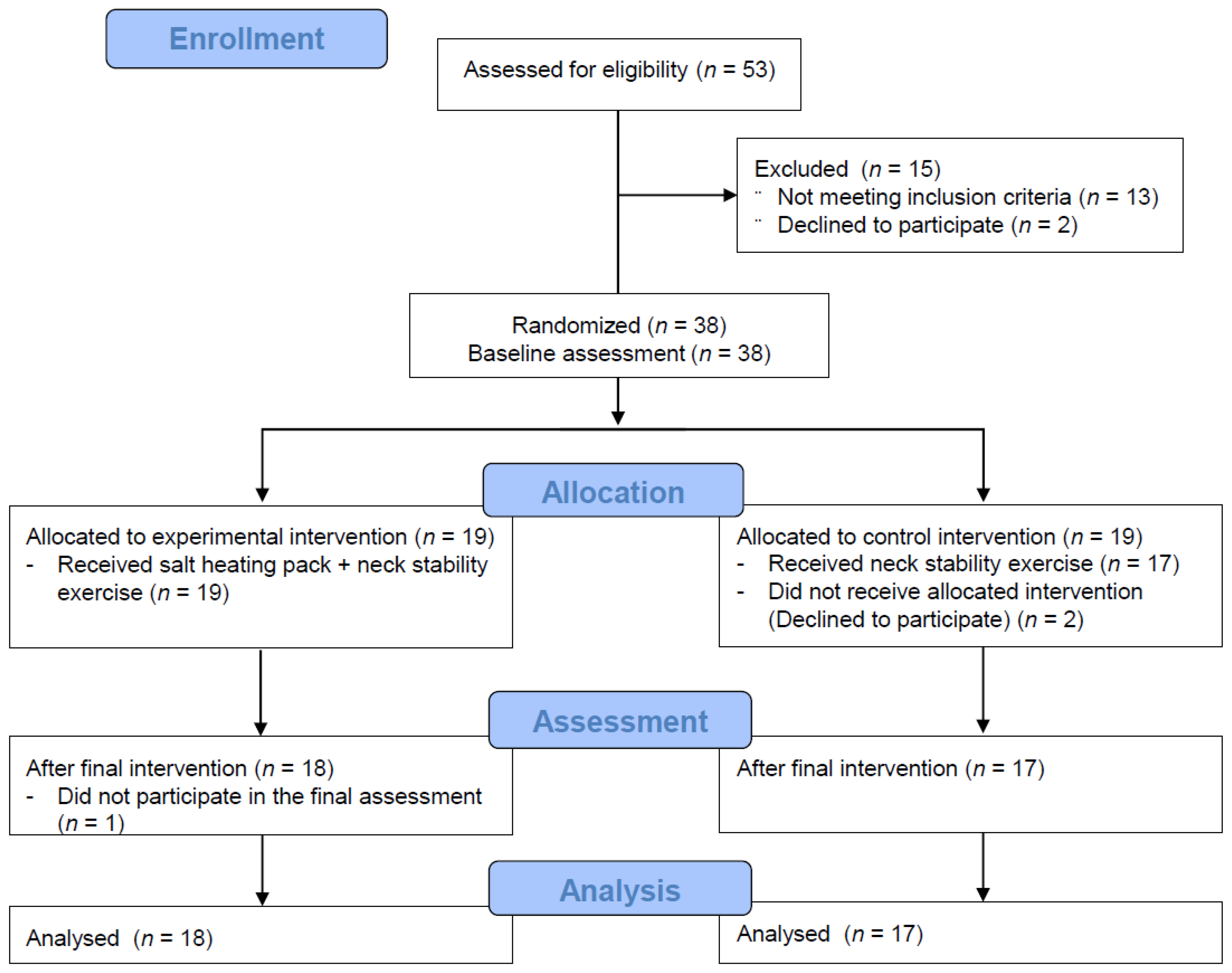
2.1. Study Design
2.2. Participants and Sample Size
2.3. Experimental Procedures and Interventions
2.4. Outcome Measures
2.4.1. Primary Variables
2.4.2. Secondary Variables
2.5. Statistical Analysis
3. Results
3.1. Participant Characteristics
3.2. Primary Outcomes
3.2.1. Pain Intensity
3.2.2. Pain Pressure Threshold
3.2.3. Neck Disability
3.3. Secondary Outcomes
3.3.1. Muscle Properties
3.3.2. Cervical and Shoulder Alignments
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A
| Emissivity (5~20 μm) | Emission Power (W/m2·μm) |
|---|---|
| 0.9000 | 3.89 × 102 |

References
- Fejer, R.; Kyvik, K.O.; Hartvigsen, J. The prevalence of neck pain in the world population: A systematic critical review of the literature. Eur. Spine J. 2006, 15, 834–848. [Google Scholar] [CrossRef] [PubMed]
- Son, K.M.; Cho, N.H.; Lim, S.H.; Kim, H.A. Prevalence and risk factor of neck pain in elderly Korean community residents. J. Korean Med. Sci. 2013, 28, 680–686. [Google Scholar] [CrossRef] [PubMed]
- Binder, A. The diagnosis and treatment of nonspecific neck pain and whiplash. Eur. Med. 2007, 43, 79–89. [Google Scholar]
- Tsakitzidis, G.; Remmen, R.; Peremans, L.; Van Royen, P.; Duchesnes, C.; Paulus, D.; Eyssen, M. Non-Specific neck pain: Diagnosis and treatment. Good Clin. Pract. 2009. KCE Reports 119C. D/2009/10.273/56. [Google Scholar]
- Gross, A.R.; Haines, T.; Goldsmith, C.H.; Santaguida, L.; McLaughlin, L.M.; Peloso, P.; Burnie, S.; Hoving, J. Knowledge to action: A challenge for neck pain treatment. J. Orthop. Sports Phys. Ther. 2009, 39, 351–363. [Google Scholar] [CrossRef] [PubMed]
- Graham, N.; Gross, A.R.; Carlesso, L.C.; Santaguida, P.L.; Macdermid, J.C.; Walton, D.; Ho, E. An ICON Overview on Physical Modalities for Neck Pain and Associated Disorders. Open Orthop. J. 2013, 7, 440–460. [Google Scholar] [CrossRef] [PubMed]
- O’Riordan, C.; Clifford, A.; Van De Ven, P.; Nelson, J. Chronic neck pain and exercise interventions: Frequency, intensity, time, and type principle. Arch. Phys. Med. Rehabil. 2014, 95, 770–783. [Google Scholar] [CrossRef]
- Celenay, S.T.; Kaya, D.O.; Akbayrak, T. Cervical and scapulothoracic stabilization exercises with and without connective tissue massage for chronic mechanical neck pain: A prospective, randomised controlled trial. Man. Ther. 2016, 21, 144–150. [Google Scholar] [CrossRef]
- Celenay, S.T.; Akbayrak, T.; Kaya, D.O. A Comparison of the Effects of Stabilization Exercises Plus Manual Therapy to Those of Stabilization Exercises Alone in Patients With Nonspecific Mechanical Neck Pain: A Randomized Clinical Trial. J. Orthop. Sports Phys. Ther. 2016, 46, 44–55. [Google Scholar] [CrossRef]
- Dusunceli, Y.; Ozturk, C.; Atamaz, F.; Hepguler, S.; Durmaz, B. Efficacy of neck stabilization exercises for neck pain: A randomized controlled study. J. Rehabil. Med. 2009, 41, 626–631. [Google Scholar] [CrossRef]
- Hahm, S.C.; Shin, H.J.; Lee, M.G.; Lee, S.J.; Cho, H.Y. Mud Therapy Combined with Core Exercise for Chronic Nonspecific Low Back Pain: A Pilot, Single-Blind, Randomized Controlled Trial. Evid. Based Complement. Alternat. Med. 2020, 2020, 7547452. [Google Scholar] [CrossRef] [PubMed]
- Cramer, H.; Baumgarten, C.; Choi, K.E.; Lauche, R.; Saha, F.J.; Musial, F.; Dobos, G. Thermotherapy self-treatment for neck pain relief—A randomized controlled trial. Eur. J. Integr. Med. 2012, 4, e371–e378. [Google Scholar] [CrossRef]
- Nadler, S.F.; Weingand, K.; Kruse, R.J. The physiologic basis and clinical applications of cryotherapy and thermotherapy for the pain practitioner. Pain Physician 2004, 7, 395–399. [Google Scholar] [PubMed]
- Erasala, G.; Rubin, J.; Tuthill, T.; Fowlkes, J.; de Drue, S.; Hengehold, D.; Weingand, K.J. The effect of topical heat treatment on trapezius muscle blood flow using power Doppler ultrasound. Phys. Ther. 2001, 81, A5. [Google Scholar]
- Nadler, S.F.; Deprince, M.L.; Stitik, T.P.; Hendgehold, D.; Weingand, K. Experimentally induced trapezius fatigue and the effects of topical heat on the EMG power density spectrum. Am. J. Phys. Med. Rehab. 1999, 80, 1123. [Google Scholar]
- Mulkern, R.; McDannold, N.; Hynynen, K.; Fielding, J.; Panych, L.; Jolesz, F.; Weingand, K. Temperature Distribution Changes in Low Back Muscles during Applied Topical Heat: A Magnetic Resonance Thermometry Study. In Proceedings of the 7th Annual Meeting of the International Society of Magnetic Resonance, in Medicine, Philadelphia, PA, USA, 22–28 May 1999; p. 1054. [Google Scholar]
- Strickler, T.; Malone, T.; Garrett, W.E. The effects of passive warming on muscle injury. Am. J. Sports Med. 1990, 18, 141–145. [Google Scholar] [CrossRef] [PubMed]
- Petrofsky, J.; Laymon, M.; Lee, H. Local heating of trigger points reduces neck and plantar fascia pain. J. Back Musculoskelet. Rehabil. 2020, 33, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Petrofsky, J.S.; Laymon, M.; Alshammari, F.; Khowailed, I.A.; Lee, H. Use of low level of continuous heat and Ibuprofen as an adjunct to physical therapy improves pain relief, range of motion and the compliance for home exercise in patients with nonspecific neck pain: A randomized controlled trial. J. Back Musculoskelet. Rehabil. 2017, 30, 889–896. [Google Scholar] [CrossRef]
- Robertson, V.J.; Ward, A.R.; Jung, P. The effect of heat on tissue extensibility: A comparison of deep and superficial heating. Arch. Phys. Med. Rehabil. 2005, 86, 819–825. [Google Scholar] [CrossRef]
- Knight, C.A.; Rutledge, C.R.; Cox, M.E.; Acosta, M.; Hall, S.J. Effect of superficial heat, deep heat, and active exercise warm-up on the extensibility of the plantar flexors. Phys. Ther. 2001, 81, 1206–1214. [Google Scholar] [CrossRef]
- Oshima-Saeki, C.; Taniho, Y.; Arita, H.; Fujimoto, E. Lower-limb warming improves sleep quality in elderly people living in nursing homes. Sleep Sci. 2017, 10, 87–91. [Google Scholar] [CrossRef] [PubMed]
- Saeki, Y. Effect of local application of cold or heat for relief of pricking pain. Nurs. Health Sci. 2002, 4, 97–105. [Google Scholar] [CrossRef] [PubMed]
- Vakilinia, S.R.; Vaghasloo, M.A.; Aliasl, F.; Mohammadbeigi, A.; Bitarafan, B.; Etripoor, G.; Asghari, M. Evaluation of the efficacy of warm salt water foot-bath on patients with painful diabetic peripheral neuropathy: A randomized clinical trial. Complement. Ther. Med. 2020, 49, 102325. [Google Scholar] [CrossRef] [PubMed]
- Tishler, M.; Shoenfeld, Y. The medical and scientific aspects of spa therapy. Isr. J. Med. Sci. 1996, 32, S8–S10. [Google Scholar]
- Cerezo-Téllez, E.; Torres-Lacomba, M.; Fuentes-Gallardo, I.; Perez-Muñoz, M.; Mayoral-Del-Moral, O.; Lluch-Girbés, E.; Prieto-Valiente, L.; Falla, D. Effectiveness of dry needling for chronic nonspecific neck pain: A randomized, single-blinded, clinical trial. Pain 2016, 157, 1905–1917. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Academic Press: New York, NY, USA, 2013. [Google Scholar]
- Kim, J.; Shin, W. How to do random allocation (randomization). Clin. Orthop. Surg. 2014, 6, 103–109. [Google Scholar] [CrossRef]
- Garra, G.; Singer, A.J.; Leno, R.; Taira, B.R.; Gupta, N.; Mathaikutty, B.; Thode, H.J. Heat or cold packs for neck and back strain: A randomized controlled trial of efficacy. Acad. Emerg. Med. 2010, 17, 484–489. [Google Scholar] [CrossRef]
- Crichton, N. Visual analogue scale (VAS). J. Clin. Nurs. 2001, 10, 697–706. [Google Scholar]
- Lauche, R.; Cramer, H.; Langhorst, J.; Michalsen, A.; Dobos, G.J. Reliability and validity of the pain on movement questionnaire (POM) in chronic neck pain. Pain Med. 2014, 15, 1850–1856. [Google Scholar] [CrossRef]
- Hahm, S.-C.; Suh, H.R.; Cho, H.Y. The effect of transcutaneous electrical nerve stimulation on pain, muscle strength, balance, and gait in individuals with dementia: A double blind, pilot randomized controlled trial. Eur. J. Integr. Med. 2019, 29, 100932. [Google Scholar] [CrossRef]
- Cleland, J.A.; Fritz, J.M.; Whitman, J.M.; Palmer, J.A. The reliability and construct validity of the Neck Disability Index and patient specific functional scale in patients with cervical radiculopathy. Spine 2006, 31, 598–602. [Google Scholar] [CrossRef] [PubMed]
- Lluch, E.; Arguisuelas, M.D.; Coloma, P.S.; Palma, F.; Rey, A.; Falla, D. Effects of deep cervical flexor training on pressure pain thresholds over myofascial trigger points in patients with chronic neck pain. J. Manip. Physiol. Ther. 2013, 36, 604–611. [Google Scholar] [CrossRef] [PubMed]
- Gapeyeva, H.; Vain, A. Methodical Guide: Principles of Applying Myoton in Physical Medicine and Rehabilitation; Muomeetria Ltd.: Tartu, Estonia, 2008. [Google Scholar]
- Singla, D.; Veqar, Z.; Hussain, M.E. Photogrammetric Assessment of Upper Body Posture Using Postural Angles: A Literature Review. J. Chiropr. Med. 2017, 16, 131–138. [Google Scholar] [CrossRef] [PubMed]
- Koyuncu, E.; Ökmen, B.M.; Özkuk, K.; Taşoğlu, Ö.; Özgirgin, N. The effectiveness of balneotherapy in chronic neck pain. Clin. Rheumatol. 2016, 35, 2549–2555. [Google Scholar] [CrossRef] [PubMed]
- Cramer, H.; Lauche, R.; Hohmann, C.; Lüdtke, R.; Haller, H.; Michalsen, A.; Langhorst, J.; Dobos, G. Randomized-controlled trial comparing yoga and home-based exercise for chronic neck pain. Clin. J. Pain 2013, 29, 216–223. [Google Scholar] [CrossRef] [PubMed]
- Lansinger, B.; Larsson, E.; Persson, L.C.; Carlsson, J.Y. Qigong and exercise therapy in patients with long-term neck pain: A prospective randomized trial. Spine 2007, 32, 2415–2422. [Google Scholar] [CrossRef]
- Vatansever, F.; Hamblin, M.R. Far infrared radiation (FIR): Its biological effects and medical applications. Photonics Lasers Med. 2012, 4, 255–266. [Google Scholar] [CrossRef]
- Lentell, G.; Hetherington, T.; Eagan, J.; Morgan, M. The use of thermal agents to influence the effectiveness of a low-load prolonged stretch. J. Orthop. Sports Phys. Ther. 1992, 16, 200–207. [Google Scholar] [CrossRef][Green Version]
- Hohmann, C.; Lauche, R.; Choi, K.E.; Saha, F.; Rampp, T.; Dobos, G.; Musial, F. Quantitative sensory testing in patients with chronic neck pain before and after the application of the acupressure pad—A randomized, controlled pilot study. Eur. J. Integr. Med. 2009, 1, 212–213. [Google Scholar] [CrossRef]
- Sterling, M. Testing for sensory hypersensitivity or central hyperexcitability associated with cervical spine pain. J. Manip. Physiol. Ther. 2008, 31, 534–539. [Google Scholar] [CrossRef]
- Nijs, J.; Lluch Girbés, E.; Lundberg, M.; Malfliet, A.; Sterling, M. Exercise therapy for chronic musculoskeletal pain: Innovation by altering pain memories. Man. Ther. 2015, 20, 216–220. [Google Scholar] [CrossRef] [PubMed]
- Yip, C.H.; Chiu, T.T.; Poon, A.T. The relationship between head posture and severity and disability of patients with neck pain. Man. Ther. 2008, 13, 148–154. [Google Scholar] [CrossRef] [PubMed]
- Fernández-de-Las-Peñas, C.; Cuadrado, M.L.; Pareja, J.A. Myofascial trigger points, neck mobility and forward head posture in unilateral migraine. Cephalalgia 2006, 26, 1061–1070. [Google Scholar] [CrossRef] [PubMed]
- Ijmker, S.; Huysmans, M.A.; Blatter, B.M.; van der Beek, A.J.; van Mechelen, W.; Bongers, P.M. Should office workers spend fewer hours at their computer? A systematic review of the literature. Occup. Environ. Med. 2007, 64, 211–222. [Google Scholar] [CrossRef] [PubMed]
- Wahlström, J. Ergonomics, musculoskeletal disorders and computer work. Occup. Med. 2005, 55, 168–176. [Google Scholar] [CrossRef]
| Variable | Intervention Group (n = 18) | Control Group (n = 17) | P |
|---|---|---|---|
| Age (years) | 68.06 ± 4.71 | 66.24 ± 4.71 | 0.261 |
| Height (m) | 1.54 ± 0.04 | 1.53 ± 0.03 | 0.299 |
| Weight (kg) | 58.92 ± 7.52 | 57.34 ± 4.68 | 0.457 |
| BMI (kg/m2) | 24.73 ± 2.93 | 24.5 ± 1.80 | 0.780 |
| VAS at rest (cm) | 4.78 ± 1.11 | 4.53 ± 1.37 | 0.560 |
| Onset duration (month) | 15.33 ± 7.76 | 14.29 ± 7.74 | 0.694 |
| Job context † | |||
| Working | 13 (72.22) | 11 (64.71) | 0.632 |
| Non-working | 5 (27.78) | 6 (35.29) |
| Outcome/Group | Baseline | Two Weeks Post-Treatment | P (Pairwise Comparison) | P (T * G) |
|---|---|---|---|---|
| VAS at rest(cm) | ||||
| Intervention group | 4.78 ± 1.11 | 1.17 ± 1.04 | <0.001 | <0.001 |
| Control group | 4.53 ± 1.37 | 3.41 ± 1.28 | 0.009 | |
| VAS during movement(cm) | ||||
| Intervention group | 6.75 ± 1.06 | 2.28 ± 1.41 | <0.001 | <0.001 |
| Control group | 6.06 ± 1.14 | 4.53 ± 1.37 | 0.001 | |
| PPT_Upper trapezius (kg) | ||||
| Intervention group | 2.41 ± 0.50 | 4.28 ± 1.38 | <0.001 | 0.002 |
| Control group | 2.56 ± 0.75 | 3.22 ± 0.87 | 0.014 | |
| PPT_Levator scapula (kg) | ||||
| Intervention group | 2.07 ± 0.51 | 4.12 ± 1.18 | <0.001 | <0.001 |
| Control group | 2.38 ± 0.89 | 2.99 ± 0.83 | 0.018 | |
| PPT_Splenius capitis (kg) | ||||
| Intervention group | 2.56 ± 0.93 | 4.52 ± 0.84 | <0.001 | 0.001 |
| Control group | 2.90 ± 0.87 | 3.55 ± 0.78 | 0.015 | |
| NDI (%) | ||||
| Intervention group | 36.11 ± 12.88 | 16.56 ± 10.56 | <0.001 | 0.005 |
| Control group | 33.65 ± 11.92 | 27.29 ± 10.79 | 0.052 | |
| Outcome/Group. | Baseline | Two Weeks Post-Treatment | P (Pairwise Comparison) | P (T * G) |
|---|---|---|---|---|
| Upper trapezius | ||||
| Tone (Hz) | ||||
| Intervention group | 13.71 ± 2.25 | 11.64 ± 0.91 | <0.001 | 0.021 |
| Control group | 14.19 ± 2.72 | 13.88 ± 3.43 | 0.552 | |
| Stiffness (N/m) | ||||
| Intervention group | 255.56 ± 19.25 | 229.83 ± 27.64 | <0.001 | 0.017 |
| Control group | 260.94 ± 11.33 | 254.88 ± 32.14 | 0.288 | |
| Elasticity (logarithm) | ||||
| Intervention group | 1.69 ± 0.26 | 1.97 ± 0.42 | 0.001 | 0.079 |
| Control group | 1.59 ± 0.23 | 1.67 ± 0.31 | 0.328 | |
| Levator scapula | ||||
| Tone (Hz) | ||||
| Intervention group | 19.03 ± 1.89 | 17.04 ± 2.23 | 0.003 | 0.129 |
| Control group | 20.11 ± 2.66 | 19.48 ± 3.10 | 0.331 | |
| Stiffness (N/m) | ||||
| Intervention group | 335.78 ± 48.50 | 280.06 ± 53.92 | <0.001 | 0.025 |
| Control group | 345.00 ± 48.90 | 333.35 ± 54.75 | 0.393 | |
| Elasticity (logarithm) | ||||
| Intervention group | 1.42 ± 0.17 | 1.65 ± 0.23 | <0.001 | 0.035 |
| Control group | 1.38 ± 0.14 | 1.44 ± 0.25 | 0.325 | |
| Splenius capitis | ||||
| Tone (Hz) | ||||
| Intervention group | 21.01 ± 1.65 | 19.07 ± 2.69 | 0.006 | 0.094 |
| Control group | 21.18 ± 2.47 | 20.88 ± 3.5 | 0.655 | |
| Stiffness (N/m) | ||||
| Intervention group | 388.56 ± 48.13 | 332.22 ± 52.88 | <0.001 | 0.012 |
| Control group | 395.24 ± 51.39 | 385.59 ± 59.32 | 0.449 | |
| Elasticity (logarithm) | ||||
| Intervention group | 1.49 ± 0.15 | 1.64 ± 0.23 | 0.001 | 0.101 |
| Control group | 1.48 ± 0.15 | 1.53 ± 0.24 | 0.296 | |
| Outcome/Group | Baseline | Two Weeks Post-Treatment | P (Pairwise comparison) | P (T * G) |
|---|---|---|---|---|
| Cervical angle (degree) | ||||
| Intervention group | 48.06 ± 6.31 | 50.26 ± 6.22 | <0.001 | 0.016 |
| Control group | 50.12 ± 4.62 | 50.59 ± 5.43 | 0.352 | |
| Shoulder angle (degree) | ||||
| Intervention group | 60.49 ± 4.57 | 65.86 ± 4.64 | <0.001 | <0.001 |
| Control group | 62.18 ± 5.49 | 62.97 ± 6.30 | 0.293 | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shin, H.-J.; Kim, S.-H.; Hahm, S.-C.; Cho, H.-Y. Thermotherapy Plus Neck Stabilization Exercise for Chronic Nonspecific Neck Pain in Elderly: A Single-Blinded Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2020, 17, 5572. https://doi.org/10.3390/ijerph17155572
Shin H-J, Kim S-H, Hahm S-C, Cho H-Y. Thermotherapy Plus Neck Stabilization Exercise for Chronic Nonspecific Neck Pain in Elderly: A Single-Blinded Randomized Controlled Trial. International Journal of Environmental Research and Public Health. 2020; 17(15):5572. https://doi.org/10.3390/ijerph17155572
Chicago/Turabian StyleShin, Ho-Jin, Sung-Hyeon Kim, Suk-Chan Hahm, and Hwi-Young Cho. 2020. "Thermotherapy Plus Neck Stabilization Exercise for Chronic Nonspecific Neck Pain in Elderly: A Single-Blinded Randomized Controlled Trial" International Journal of Environmental Research and Public Health 17, no. 15: 5572. https://doi.org/10.3390/ijerph17155572
APA StyleShin, H.-J., Kim, S.-H., Hahm, S.-C., & Cho, H.-Y. (2020). Thermotherapy Plus Neck Stabilization Exercise for Chronic Nonspecific Neck Pain in Elderly: A Single-Blinded Randomized Controlled Trial. International Journal of Environmental Research and Public Health, 17(15), 5572. https://doi.org/10.3390/ijerph17155572







