State of Mind Ireland-Higher Education: A Mixed-Methods Longitudinal Evaluation of a Positive Mental Health Intervention
Abstract
1. Introduction
1.1. The Purpose of This Study
1.2. The SOMI-HE Intervention Programme
2. Material and Methods
2.1. Participants and Setting
2.2. Ethical Considerations
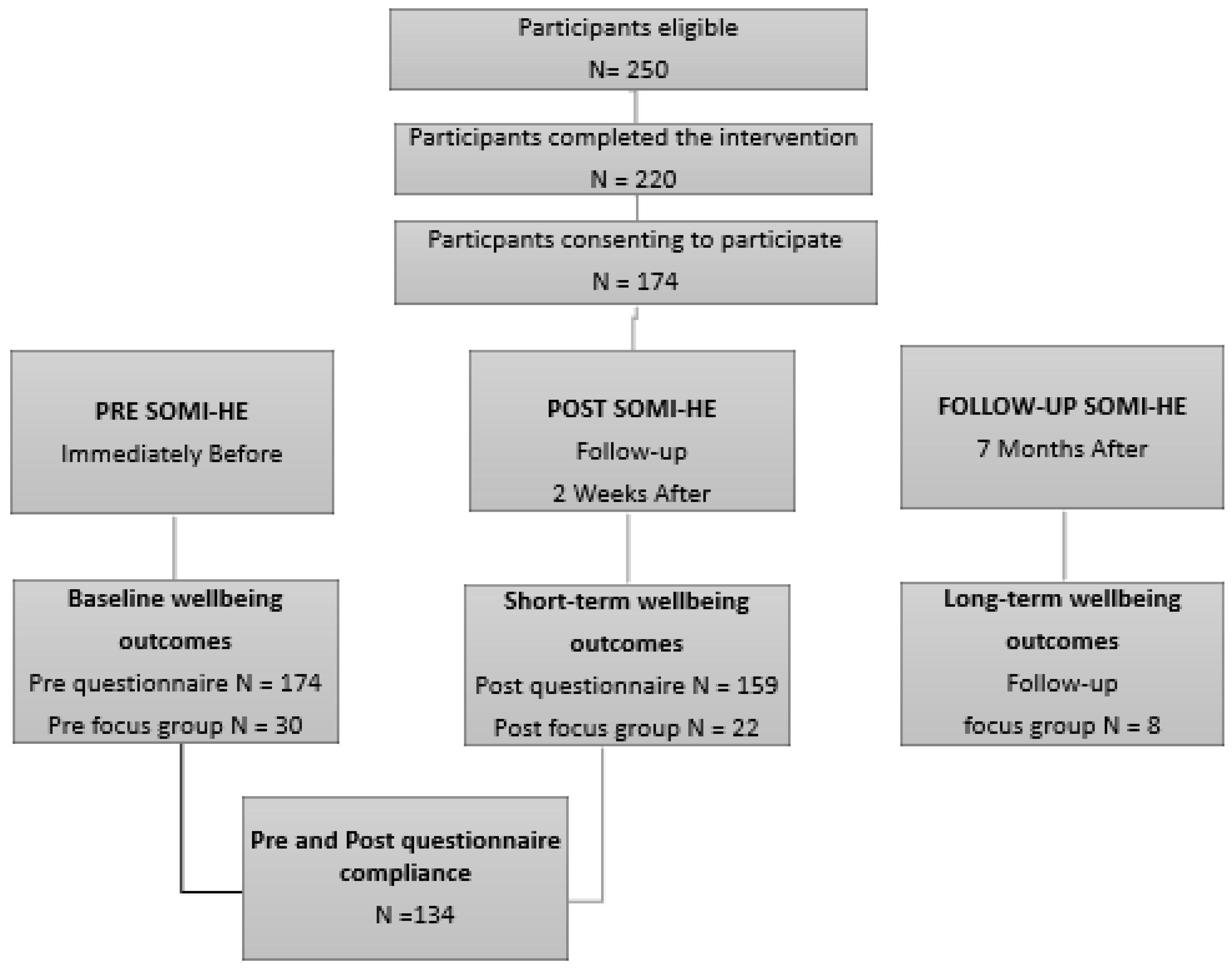
2.3. Study Design and Procedures
2.4. Quantitative Participants and Recruitment
2.5. Qualitative Participants and Recruitment
2.6. Measurements
2.6.1. The Warwick-Edinburgh Mental Wellbeing Scale (WEMWBS)
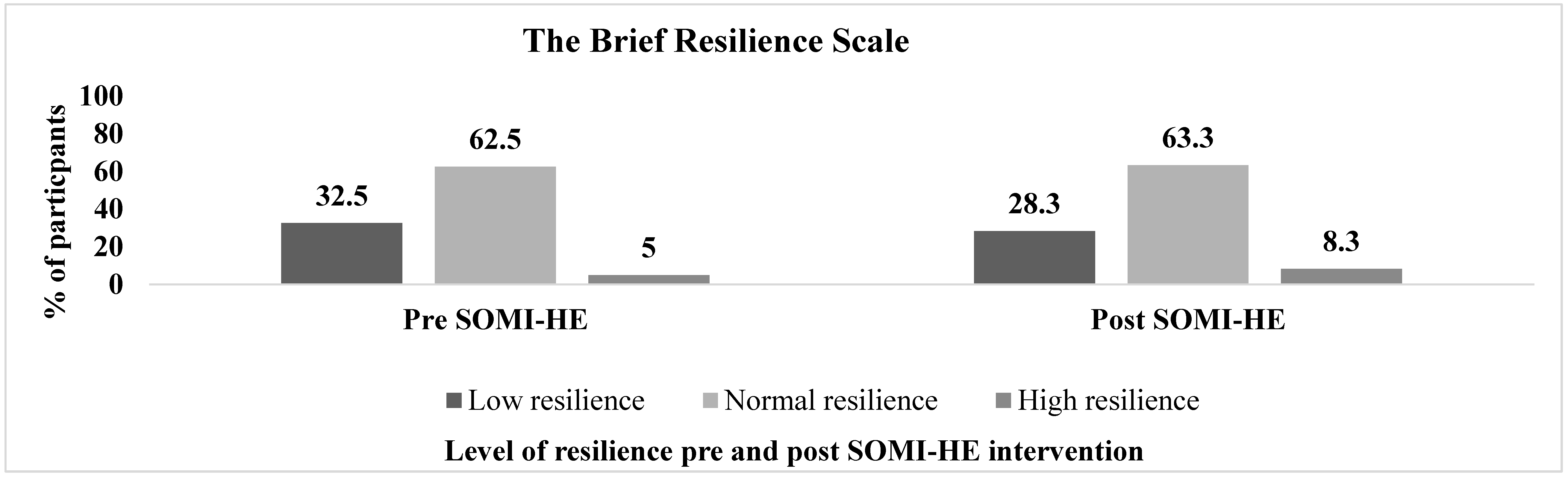
2.6.2. The Brief Resilience Scale (BRS)
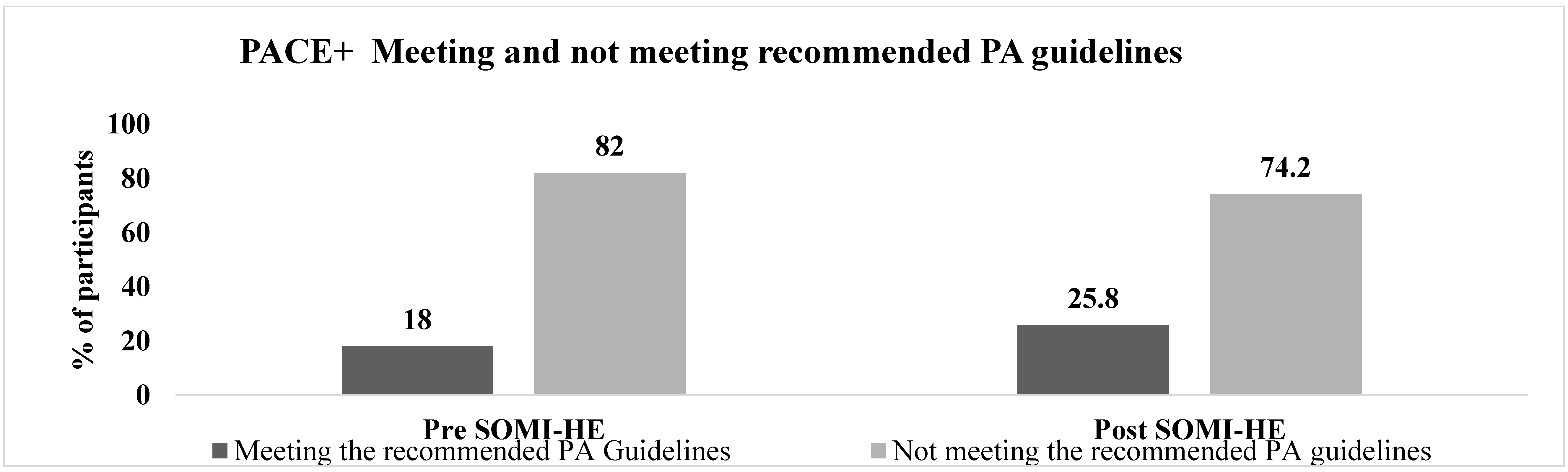
2.6.3. The Patient-Centred Assessment and Counselling for Exercise Plus Nutrition (PACE+ Physical Activity Measure)
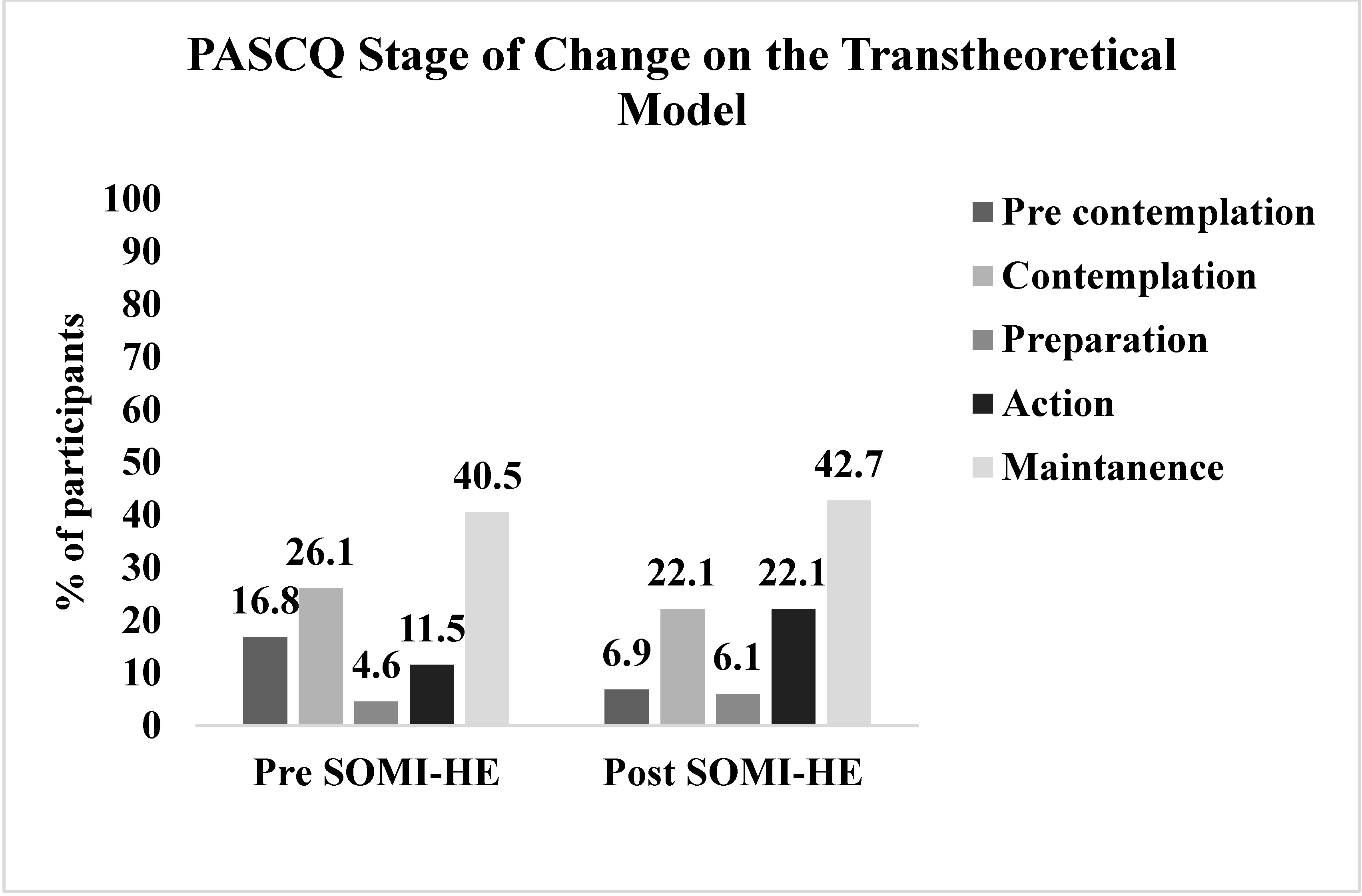
2.6.4. The Physical Activity Stages of Change Questionnaire (PASCQ) or Transtheoretical Model (TTM)
2.6.5. Focus Group Discussions
3. Data Analysis
3.1. Self-Report Questionnaire
3.2. Focus Groups
4. Results
4.1. Self-Report Questionnaire Findings
4.1.1. Descriptive Results
4.1.2. Wellbeing, Resilience, PA, and the SOMI-HE Intervention
4.1.3. Gender Differences Wellbeing, Resilience, and PA at Pre-Intervention
4.1.4. Demographic Determinants (Gender and Age Groups) of Changes in Wellbeing, Resilience Ad PA Over Time
4.2. Focus Group Findings
‘…mental health courses or wellbeing courses in today’s world, they’re all kind of focussed on speaking up and ignoring the stigma. I found this course actually gave you techniques of what you can actually do besides just talking out about it, and it actually showed you how to manage and what you should actually do besides just having the confidence to speak about it in the first place.’
‘I think it spreads around, say like the community, even if I was talking to one of the lads it would be “are you alright?” or “do you need a hand with this?” or whatever. So, it definitely feeds into other people if you start doing it. It’s a knock-on effect basically.’
‘I made more of an effort during the summer. Knowing how it (PA) affects your mental health, knowing that it will benefit you and you won’t regret it…it’s that realisation I suppose that only good things can come from it.’
‘I think the whole exercise element really kind of hit me as well… I kind of realised that, no, I have to exercise to think clearly and all that… I thought I had to run away from my problems, I actually have to go for a run to actually face them.’
‘I find it extremely difficult to juggle everything together. If I was given the tools and maybe told maybe how I could do my work and then still have a social life and still be happy… I do get very, very stressed I must say. Before coming here, before this course, I used not to get stressed. I’d find myself getting very anxious I have to say.’
5. Discussion
6. Limitations
7. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Usher, W. Living in Quiet Desperation: The Mental Health Epidemic in Australia’s Higher Education. Health Educ. 2019, 79, 138–151. [Google Scholar] [CrossRef]
- Thorley, C. Not By Degrees: Improving Student Mental Health in the UK’s Universities. Available online: https://www.ippr.org/publications/not-by-degrees (accessed on 1 March 2018).
- Murphy, E. Responding to the Needs of Students with Mental Health Difficulties in Higher Education: An Irish Perspective. Eur. J. Spec. Needs Educ. 2017, 32, 110–124. [Google Scholar] [CrossRef]
- Gore, F.M.; Bloem, P.J.; Patton, G.C.; Ferguson, J.; Joseph, V.; Coffey, C.; Sawyer, S.M.; Mathers, C.D. Global Burden of Disease in Young People Aged 10–24 Years: A Systematic Analysis. Lancet 2011, 377, 2093–2102. [Google Scholar] [CrossRef]
- Harding, T.; Lopez, V.; Klainin-Yobas, P. Predictors of Psychological Well-Being among Higher Education Students. Psychology 2019, 10, 578–594. [Google Scholar] [CrossRef][Green Version]
- Dalky, H.F.; Gharaibeh, A. Depression, Anxiety, and Stress among College Students in Jordan and Their Need for Mental Health Services. Nurs. Forum 2019, 54, 205–212. [Google Scholar] [CrossRef]
- Peer, J.W.; Hillman, S.B.; Van Hoet, E. The Effects of Stress on the Lives of Emerging Adult College Students: An Exploratory Analysis. Adultspan J. 2015, 14, 90–99. [Google Scholar] [CrossRef]
- Bewick, B.; Koutsopouloub, G.; Miles, J.; Slaad, E.; Barkham, M. Changes in Undergraduate Students’ Psychological Well-Being as They Progress through University. Stud. High. Educ. 2010, 35, 633–645. [Google Scholar] [CrossRef]
- Vidourek, R.A.; Burbage, M. Positive Mental Health and Mental Health Stigma: A Qualitative Study Assessing Student Attitudes. Ment. Health Prev. 2019, 13, 1–6. [Google Scholar] [CrossRef]
- Hunt, J.; Eisenberg, D. Mental Health Problems and Help-Seeking Behavior Among College Students. J. Adolesc. Health 2010, 46, 3–10. [Google Scholar] [CrossRef]
- Chan, M. Mental Health: Central to Human Development. Mental Health and Development: Targeting People with Mental Health Conditions as a Vulnerable Group. 2010, pp. 1–6. Available online: https://www.who.int/mental_health/policy/development/mh_devel_targeting_summary_2010_en.pdf (accessed on 6 May 2018).
- Aked, J.; Marks, N.A.; Cordon, C.; Thompson, S. Five Ways to Wellbeing: A Report Presented to the Foresight Project on Communicating the Evidence Base for Improving People’s Well-Being. In New Economics Foundation; Centre for wellbeing, New Economics Foundation: London, UK, 2008; pp. 1–23. [Google Scholar]
- Tennant, R.; Hiller, L.; Fishwick, R.; Platt, S.; Joseph, S.; Weich, S.; Parkinson, J.; Secker, J.; Stewart-Brown, S. The Warwick-Edinburgh Mental Well-Being Scale (WEMWBS): Development and UK Validation. Health Qual. Life Outcomes 2007, 5, 63. [Google Scholar] [CrossRef]
- Barry, M. Addressing the Determinants of Positive Mental Health: Concepts, Evidence and Practice. Int. J. Ment. Health Promot. 2009, 11, 4–17. [Google Scholar] [CrossRef]
- World Health Organization [WHO]. Promoting Mental Health.Concepts, Emerging Evidence, Practice; World Health Organization: Geneva, Switzerland, 2005. [Google Scholar]
- Vaillant, G.E. Positive Mental Health: Is There a Cross-Cultural Definition? World Psychiatry 2012, 11, 93–99. [Google Scholar] [CrossRef]
- Robinson, P.; Oades, L.G.; Caputi, P. Conceptualising and Measuring Mental Fitness: A Delphi Study. Int. J. Wellbeing 2016, 5, 53–73. [Google Scholar] [CrossRef]
- Smith, B.W.; Dalen, J.; Wiggins, K.; Tooley, E.; Christopher, P.; Bernard, J. The Brief Resilience Scale: Assessing the Ability to Bounce Back. Int. J. Behav. Med. 2008, 15, 194–200. [Google Scholar] [CrossRef] [PubMed]
- Oades, L.G.; Steger, M.; Delle Fave, A.; Passmore, J. The Wiley Blackwell Handbook of the Psychology of Positivity and Strengths-Based Approaches at Work; John Wiley & Sons: Chichester, UK, 2017. [Google Scholar]
- Greenwood, P.M.; Parasuraman, R. Neuronal and Cognitive Plasticity: A Neurocognitive Framework for Ameliorating Cognitive Aging. Front. Aging Neurosci. 2010, 2, 1–14. [Google Scholar] [CrossRef] [PubMed]
- May, A. Experience-Dependent Structural Plasticity in the Adult Human Brain. Trends Cogn. Sci. 2011, 15, 475–482. [Google Scholar] [CrossRef]
- Siegel, D. Mindsight; Random House Publishing Group: New York, NY, USA, 2010. [Google Scholar]
- Breslin, G.; Haughey, T.; O’Brien, W.; Caulfield, L.; Robertson, A.; Lawlor, M. Increasing Athlete Knowledge of Mental Health and Intentions to Seek Help: The State of Mind Ireland (SOMI) Pilot Program. J. Clin. Sport Psychol. 2018, 12, 39–56. [Google Scholar] [CrossRef]
- Keyes, C.L.M.; Simoes, E.J. To Flourish or Not: Positive Mental Health and All-Cause Mortality. Am. J. Public Health 2012, 102, 2164–2172. [Google Scholar] [CrossRef]
- Tugade, M.; Fredrickson, B.L. Resilient Individuals Use Positive Emotions to Bounce Back From Negative Emotional Experiences NIH Public Access. NIH Public Access 2004, 86, 320–333. [Google Scholar]
- Winzer, R.; Lindberg, L.; Guldbrandsson, K.; Sidorchuk, A. Effects of Mental Health Interventions for Students in Higher Education Are Sustainable over Time: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. PeerJ 2018, 2018. [Google Scholar] [CrossRef]
- Barrantes-Brais, K.; Sánchez-Ureña, B.; Ureña-Bonilla, P. The Effect of Psychological and Exercise Interventions on College Students’ Well-Being and Ill-Being: A Meta-Analysis of Randomized Controlled Trials. J. Sport Health Res. 2016, 8, 75–92. [Google Scholar]
- Conley, S.C.; Durlak, J.; Dickson, D. An Evaluative Review of Outcome Research on Universal Mental Health Promotion and Prevention Programs for Higher Education Students. J. Am. Coll. Health 2013, 61, 286–301. [Google Scholar] [CrossRef] [PubMed]
- Kok, G.; Schaalma, H.; Ruiter, R.A.C.; Van Empelen, P.; Brug, J. Intervention Mapping: A Protocol for Applying Health Psychology Theory to Prevention Programmes. J. Health Psychol. 2004, 9, 85–98. [Google Scholar] [CrossRef]
- Bjørnsen, H.N.; Espnes, G.A.; Ringdal, R.; Moksnes, U.K.; Eilertsen, M.-E.B. The Relationship Between Positive Mental Health Literacy and Mental Well-Being Among Adolescents. J. Sch. Nurs. 2017, 35. [Google Scholar] [CrossRef]
- Kutcher, S.; Wei, Y.; Costa, S.; Gusmão, R.; Skokauskas, N.; Sourander, A. Enhancing Mental Health Literacy in Young People. Eur. Child Adolesc. Psychiatry 2016, 25, 567–569. [Google Scholar] [CrossRef]
- Seligman, M.E.P.; Steen, T.A.; Park, N.; Peterson, C. Positive Psychology Progress: Empirical Validation of Interventions. Am. Psychol. 2005, 60, 410–421. [Google Scholar] [CrossRef]
- Galante, J.; Dufour, G.; Vainre, M.; Wagner, A.P.; Stochl, J.; Benton, A.; Lathia, N.; Howarth, E.; Jones, P.B. A Mindfulness-Based Intervention to Increase Resilience to Stress in University Students (the Mindful Student Study): A Pragmatic Randomised Controlled Trial. Lancet Public Health 2018, 3, e72–e81. [Google Scholar] [CrossRef]
- Ma, L.; Zhang, Y.; Cui, Z. Mindfulness-Based Interventions for Prevention of Depressive Symptoms in University Students: A Meta-Analytic Review. Mindfulness (N. Y.) 2019. [Google Scholar] [CrossRef]
- Kabat-Zinn, J. Mindfulness-Based Interventions in Context: Past, Present, and Future. Clin. Psychol. Sci. Pract. 2003, 10, 144–156. [Google Scholar] [CrossRef]
- Shoshani, A.; Steinmetz, S. Positive Psychology at School: A School-Based Intervention to Promote Adolescents’ Mental Health and Well-Being. J. Happiness Stud. 2014, 15, 1289–1311. [Google Scholar] [CrossRef]
- Bolier, L.; Haverman, M.; Westerhof, G.J.; Riper, H.; Smit, F.; Bohlmeijer, E. Positive Psychology Interventions: A Meta-Analysis of Randomized Controlled Studies. BMC Public Health 2013, 13, 1. [Google Scholar] [CrossRef] [PubMed]
- MacLeod, A.K.; Coates, E.; Hetherton, J. Increasing Well-Being through Teaching Goal-Setting and Planning Skills: Results of a Brief Intervention. J. Happiness Stud. 2008, 9, 185–196. [Google Scholar] [CrossRef]
- Biddle, S.J.H.; Ciaccioni, S.; Thomas, G.; Vergeer, I. Physical Activity and Mental Health in Children and Adolescents: An Updated Review of Reviews and an Analysis of Causality. Psychol. Sport Exerc. 2019, 42, 146–155. [Google Scholar] [CrossRef]
- Penedo, F.J.; Dahn, J.R. Exercise and Well-Being: A Review of Mental and Physical Health Benefits Associated with Physical Activity. Curr. Opin. Psychiatry 2005, 18, 189–193. [Google Scholar] [CrossRef]
- Gill, D.L.; Hammond, C.C.; Reifsteck, E.J.; Jehu, C.M.; Williams, R.A.; Adams, M.M.; Lange, E.H.; Becofsky, K.; Rodriguez, E.; Shang, Y.-T. Physical Activity and Quality of Life. J. Prev. Med. Public Health 2013, 46, S28–S34. [Google Scholar] [CrossRef]
- Humphreys, B.R.; McLeod, L.; Ruseski, J.E. Physical Actvity and Health Outcomes: Ecidence from Canada. Health Econ. 2014, 23, 33–54. [Google Scholar] [CrossRef]
- World Health Organization. Global Status Report on Noncommunicable Diseases; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Murphy, M.H.; Carlin, A.; Woods, C.; Nevill, A.; MacDonncha, C.; Ferguson, K.; Murphy, N. Active Students Are Healthier and Happier than Their Inactive Peers: The Results of a Large Representative Cross-Sectional Study of University Students in Ireland. J. Phys. Act. Health 2018, 15, 737–746. [Google Scholar] [CrossRef]
- Eime, R.M.; Young, J.A.; Harvey, J.T.; Charity, M.J.; Payne, W.R. A Systematic Review of the Psychological and Social Benefits of Participation in Sport for Adults: Informing Development of a Conceptual Model of Health through Sport. Int. J. Behav. Nutr. Phys. Act. 2013, 10, 135. [Google Scholar] [CrossRef]
- Malcolm, E.; Evans-Lacko, S.; Little, K.; Henderson, C.; Thornicroft, G. The Impact of Exercise Projects to Promote Mental Wellbeing. J. Ment. Health 2013, 22, 519–527. [Google Scholar] [CrossRef]
- Martin, P.; McCann, T.V. Exercise and Older Women’s Wellbeing. Contemp Nurse 2005, 20, 169–179. [Google Scholar] [CrossRef]
- Rodriguez-Ayllon, M.; Cadenas-Sánchez, C.; Estévez-López, F. Role of Physical Activity and Sedentary Behavior in the Mental Health of Preschoolers, Children and Adolescents: A Systematic Review and Meta-Analysis. Int. J. Sports Med. 2019, 49, 1383–1410. [Google Scholar] [CrossRef] [PubMed]
- Biddle, S.J.H.; Asare, M. Physical Activity and Mental Health in Children and Adolescents: A Review of Reviews. Br. J. Sports Med. 2011, 886–895. [Google Scholar] [CrossRef]
- Biddle, S.J.H.; Mutrie, N. Psychology of Physical Activity: Determinants, Well-Being and Interventions, 2nd ed.; Routledge: Abingdon, UK, 2008. [Google Scholar]
- O’ Brien, N.; Lawlor, M.; Chambers, F.; Breslin, G.; O’Brien, W. Levels of Wellbeing, Resilience, and Physical Activity amongst Irish Pre-Service Teachers: A Baseline Study. Irish Educ. Stud. 2019, 1–18. [Google Scholar] [CrossRef]
- Plotnikoff, R.C.; Costigan, S.A.; Williams, R.L.; Hutchesson, M.J.; Kennedy, S.G.; Robards, S.L.; Allen, J.; Collins, C.E.; Callister, R.; Germov, J. Effectiveness of Interventions Targeting Physical Activity, Nutrition and Healthy Weight for University and College Students: A Systematic Review and Meta-Analysis. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Kwan, M.Y.W.; Graham, J.D.; Bedard, C.; Bremer, E.; Healey, C.; Cairney, J. Examining the Effectiveness of a Pilot Physical Literacy–Based Intervention Targeting First-Year University Students: The PLUS Program. SAGE Open 2019, 9. [Google Scholar] [CrossRef]
- Woods, C.; Mutrie, N.; Scott, M. Physical Activity Intervention: A Transtheoretical Model-Based Intervention Designed to Help Sedentary Young Adults Become Active. Health Educ. Res. Theory Pract. Pages 2002, 17, 451–460. [Google Scholar] [CrossRef] [PubMed]
- O’ Brien, N.; Lawlor, M.; Chambers, F.; O’Brien, W. Mental Fitness in Higher Education: Intervention Mapping Programme Design. Health Educ. 2020, 120, 21–39. [Google Scholar] [CrossRef]
- Bartholomew Eldridge, L.K.; Markham, M.C.; Ruiter, A.C.R.; Gerjo, K.; Parcel, G.S. Planning Health Promotion Programs: An Intervention Mapping Approach, 4th ed.; John Wiley & Sons, Inc.: San Francisco, CA, USA, 2016. [Google Scholar]
- Barry, M.; Jenkins, R. Implementing Mental Health Promotion; Elsevier: Oxford, UK, 2007. [Google Scholar]
- Jané-Liopis, E.; Barry, M.; Hosman, C.; Patel, V. Mental Health Promtion Works. Promot. Educ. Suppl. 2005, 2, 9–25. [Google Scholar]
- Naidoo, J.; Wills, J. Foundations for Health Promotion; Elsevier: Edinburgh, Scotland, 2016. [Google Scholar]
- Institute for Futures Studies. Policies and Strategies to Promote Social Equity in Health. Background Document to WHO—Strategy Paper for Europe; Institute for Futures Studies: Stockholm, Sweden, 1991. [Google Scholar]
- Graham, H. Social Determinants and Their Unequal Distribution: Clarifying Policy Understandings. Milbank Q. 2004, 82, 101–124. [Google Scholar] [CrossRef]
- Kok, G. A Practical Guide to Effective Behavior Change How to Apply Theory- and Evidence-Based Behavior Change Methods in an Intervention. Eur. Health Psychol. 2014, 16, 156–170. [Google Scholar]
- Ammendolia, C.; Côté, P.; Cancelliere, C.; Cassidy, J.D.; Hartvigsen, J.; Boyle, E.; Soklaridis, S.; Stern, P.; Iii, B.A. Healthy and Productive Workers: Using Intervention Mapping to Design a Workplace Health Promotion and Wellness Program to Improve Presenteeism. BMC Public Health 2016. [Google Scholar] [CrossRef]
- Koekkoek, B.; Van Meijel, B.; Schene, A.; Hutschemaekers, G. Development of an Intervention Program to Increase Effective Behaviours by Patients and Clinicians in Psychiatric Services: Intervention Mapping Study. BMC Health Serv. Res. 2010, 10. [Google Scholar] [CrossRef]
- Mceachan, R.R.C.; Lawton, R.J.; Jackson, C.; Conner, M.; Lunt, J. Evidence, Theory and Context: Using Intervention Mapping to Develop a Worksite Physical Activity Intervention. BMC Public Health 2008, 8, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Van Stralen, M.M.; Kok, G.; De Vries, H.; Mudde, A.N.; Bolman, C.; Lechner, L. The Active plus Protocol: Systematic Development of Two Theory- and Evidence-Based Tailored Physical Activity Interventions for the over-Fifties. BMC Public Health 2008, 8, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Michie, S.; West, R.; Sheals, K.; Godinho, C.A. Evaluating the Effectiveness of Behavior Change Techniques in Health-Related Behavior: A Scoping Review of Methods Used. Transl. Behav. Med. 2018, 8, 212–224. [Google Scholar] [CrossRef]
- Abraham, C.; Michie, S. A Taxonomy of Behavior Change Techniques Used in Interventions. Health Psychol. 2008, 27, 379–387. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W. Mixed Methods Application in Health Intervention Research: A Multiple Case Study. Int. J. Mult. Res. Approaches 2014, 8, 24–35. [Google Scholar] [CrossRef]
- Meissner, H.; Creswell, J.; Klassen, A.C.; Plano, V.; Smith, K.C. Best Practices for Mixed Methods Research in the Health Sciences. In The Need for Best Practices; Office of Behavioral and Social Sciences Research (OBSSR): Bethesda, MD, USA, 2011; pp. 1–39. [Google Scholar]
- Galdas, P. Revisiting Bias in Qualitative Research: Reflections on Its Relationship With Funding and Impact. Int. J. Qual. Methods 2017, 16, 1–2. [Google Scholar] [CrossRef]
- Creswell, J.W. Research Design:Qualitative, Quantitive and Mixed-Methods Approaches, 2nd ed.; Sage Publications: Thousand Oaks, CA, USA, 2003. [Google Scholar]
- Dezkin, N.K.; Lincoln, Y.S. The SAGE Handbook of Qualitative Research; Sage Publications: Thousand Oaks, CA, USA, 2011. [Google Scholar]
- Mertens, D.M.; Wilson, A.T. Program Evaluation Theory and Practice, 2nd ed.; The Guilford Press: New York, NY, USA, 2019. [Google Scholar]
- Stewart-brown, S.; Janmohamed, K. Warwick-Edinburgh Mental Well-Being Scale User Guide; NHS: Edinburgh, UK, 2008. [Google Scholar]
- Maheswaran, H.; Weich, S.; Powell, J.; Stewart-brown, S. Evaluating the Responsiveness of the Warwick Edinburgh Mental Well-Being Scale (WEMWBS): Group and Individual Level Analysis. Health Qual. Life Out. 2012, 1–8. Available online: https://doi.org/10.1186/1477-7525-10-156 (accessed on 6 August 2019). [CrossRef]
- Fellow, R.; Stewart-Brown, S.; Taggart, F. Warwick-Edinburgh Mental Well-Being Scale (WEMWBS). User Guide; Version 2. 2015. Available online: https://doi.org/http://www.healthscotland.com/documents/2702.aspx (accessed on 1 July 2019).
- Rodríguez-Rey, R.; Alonso-Tapia, J.; Hernansaiz-Garrido, H. Reliability and Validity of the Brief Resilience Scale (BRS) Spanish Version. Psychol. Assess. 2016, 28, 101–110. [Google Scholar] [CrossRef]
- Prochaska, J.J.; Sallis, J.F.; Long, B. A Physical Activity Screening Measure for Use with Adolescents in Primary Care. Arch. Pediatr. Adolesc. Med. 2001, 155, 554–559. [Google Scholar] [CrossRef] [PubMed]
- Murphy, J.J.; Murphy, M.H.; MacDonncha, C.; Murphy, N.; Woods, N.; Nevill, A.; Woods, C.B. Validity and Reliability of Three Self-Report Instruments for Assessing Attainment of Physical Activity Guidelines in University Students. Meas. Phys. Educ. Exerc. Sci. 2017, 21, 134–141. [Google Scholar] [CrossRef]
- Marcus, H.B.; Simkin, L.R. The Stages of Exercise Behavior. J. Sport. Med. Phys. Fit. 2003, 33, 83–88. [Google Scholar]
- Prochaska, J.O.; Velicer, W.F. The Transtheoretical Change Model of Health Behavior. Am. J. Health Promot. 1997, 12, 38–48. [Google Scholar] [CrossRef] [PubMed]
- Marcus, B.H.; Lewis, B.A. Physical Activity and the Stages of Motivational Readiness for Change Model. Pres. Counc. Phys. Fit. Sport. Res. Dig. 2003, 4, 1–6. [Google Scholar]
- Cardinal, B.J. Behavioral and Biometric Comparisons of the Preparation, Action, and Maintenance Stages of Exercise. Wellness Perspect. Res. Theory, Pract. 1995, 11, 36–43. [Google Scholar]
- Mettling, S.; Lee, J.-M.; Blount, A.; Dinkel, D. A Needs Assessment for Physical Activity Programming Based on the Transtheoretical Model. Recreat. Sport. J. 2018, 42. [Google Scholar] [CrossRef]
- Krueger, R.A.; Casey, M.A. Focus Group Interviewing, A Handbook of Practical Program Evaluation, 4th ed.; John Wiley & Sons, Inc.: New York, NY, USA, 2015. [Google Scholar]
- Zijlstra, W.P.; van der Ark, L.A.; Sijtsma, K. Outliers in Questionnaire Data: Can They Be Detected and Should They Be Removed? J. Educ. Behav. Stat. 2011, 36, 186–212. [Google Scholar] [CrossRef]
- Abraham, W.T.; Russell, D.W. Statistical Power Analysis in Psychological Research. Soc. Personal. Psychol. Compass 2008, 2, 283–301. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Successful Qualitative Research: A Practical Guide for Beginners; SAGE Publications Ltd: Thousand Oaks, CA, USA, 2013; p. 400. [Google Scholar]
- Bree, R.; Gallagher, G. Using Microsoft Excel to Code and Thematically Analyse Qualitative Data: A Simple, Cost-Effective Approach. AISHE-J All Irel. J. Teach. Learn. High. Educ. 2016, 8, 2811–2824. [Google Scholar]
- Maguire, M.; Delahunt, B. Doing a Thematic Analysis: A Practical, Step-by-Step Guide for Learning and Teaching Scholars. All Irel. J. Teach. Learn. High. Educ. 2017, 8, 3351–3364. [Google Scholar]
- Fetters, M.D.; Curry, L.A.; Creswell, J.W. Achieving Integration in Mixed Methods Designs—Principles and Practices. Health Serv. Res. 2013, 48, 2134–2156. [Google Scholar] [CrossRef] [PubMed]
- Heale, R.; Forbes, D. Understanding Triangulation in Research. Evid. Based. Nurs. 2013, 16, 98. [Google Scholar] [CrossRef] [PubMed]
- Murphy, M.; MacDonncha, C.; Woods, C.; Murphy, N.; Byrne, N.; Ferguson, K.; Vevill, A. Student Actvity and Sports Study Ireland (SASSI); Irish Social Science Data Archive: Dublin, Ireland, 2016. [Google Scholar]
- Regehr, C.; Glancy, D.; Pitts, A. Interventions to Reduce Stress in University Students: A Review and Meta Analysis. Eur. Psychiatry 2013, 28, 1. [Google Scholar] [CrossRef]
- Barry, M.; Clarke, A.M.; Jenkins, R.; Patel, V. A Systematic Review of the Effectiveness of Mental Health Promotion Interventions for Young People in Low and Middle Income Countries. BMC Public Health 2013, 13, 1. [Google Scholar] [CrossRef]
- Reavley, N.J.; McCann, T.V.; Jorm, A.F. Mental Health Literacy in Higher Education Students. Early Interv. Psychiatry 2012, 6, 45–52. [Google Scholar] [CrossRef] [PubMed]
- Chambers, D.; Murphy, F.; Keeley, H.S. All of Us? An Exploration of the Concept of Mental Health Literacy Based on Young People’s Responses to Fictional Mental Health Vignettes. Ir. J. Psychol. Med. 2015, 32, 129–136. [Google Scholar] [CrossRef]
- WHO. MhGAP Community Toolkit Field Test Version; World Health Organisation: Geneva, Switzerland, 2019. [Google Scholar]
- Jorm, A.; Yap, M. The Future of Mental Health & Prevention. Ment. Health Prev. 2019, 14, 200168. [Google Scholar]
- Bauer Georg, F.; Hämmig, O. Bridging Occupational, Organizational and Public Health: A Transdisciplinary Approach; Springer: Berlin/Heidelberg, Germany, 2014; pp. 1–249. [Google Scholar] [CrossRef]
- Southwick, S.M.; Litz, B.T.; Charney, D.; Matthew, J. Resilience and Mental Health: Challenges across the Lifespan; Cambridge University Press: Cambridge, UK, 2012. [Google Scholar] [CrossRef]
- Dahlgren, G.; Whitehead, M. Levelling up (Part 1): A Discussion Paper on Concepts and Principles for Tackling Social Inequities in Health Margaret. Stud. Soc. Econ. Determ. Popul. Health 2006, 2, 1–105. [Google Scholar]
- González-Zamar, M.D.; Jiménez, L.O.; Ayala, A.S.; Abad-Segura, E. The Impact of the University Classroom on Managing the Socio-Educational Well-Being: A Global Study. Int. J. Environ. Res. Public Health 2020, 17, 931. [Google Scholar] [CrossRef] [PubMed]
- Thomas, L.; Hill, M.; O’Mahoney, J.; Yorke, M. Supporting Student Success: Strategies for Institutional Change; Higher Education Academy: York, UK, 2017; Available online: https://www.heacademy.ac.uk/download/what-works-2-summary-and-full-report (accessed on 5 July 2019).
- Joyce, S.; Shand, F.; Tighe, J.; Laurent, S.J.; Bryant, R.A.; Harvey, S.B. Road to Resilience: A Systematic Review and Meta-Analysis of Resilience Training Programmes and Interventions. BMJ Open 2018, 8, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Southwick, S.M.; Bonanno, G.A.; Masten, A.S.; Panter-Brick, C.; Yehuda, R. Resilience Definitions, Theory, and Challenges: Interdisciplinary Perspectives. Eur. J. Psychotraumatol. 2014, 5, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Martin-Breen, P.; Anderies, J. Resilience: A Literature Review; Bellagio Initiative: Brighton, UK, 2011. [Google Scholar]
- Jorm, A.F. Mental Health Literacy; Empowering the Community to Take Action for Better Mental Health. Am. Psychol. 2012, 67, 231–243. [Google Scholar] [CrossRef] [PubMed]
- Kelly, C.M.; Jorm, A.F.; Wright, A. Improving Mental Health Literacy as a Strategy to Facilitate Early Intervention for Mental Disorders. Med. J. Aust. 2007, 187, 26–30. [Google Scholar] [CrossRef]
- O’Reilly, A.; Illback, R.; Peiper, N.; O’Keeffe, L.; Clayton, R. Youth Engagement with an Emerging Irish Mental Health Early Intervention Programme (Jigsaw): Participant Characteristics and Implications for Service Delivery. J. Ment. Health 2015, 24, 283–288. [Google Scholar] [CrossRef]
- World Econmonic Forum. A Global Framework for Youth Mental Health: Investing in Future Mental Capital for Individuals, Communities and Economies: Geneva, Switzerland, 2020. Available online: http://www3.weforum.org/docs/WEF_Youth_Mental_Health_2020.pdf (accessed on 28 May 2020).
- McMahon, J.; Ryan, F.; Cannon, M.; O’Brien, G.; O’Callaghan, M.; Flanagan, R.; O’Connor, K.; Chambers, D.; Byrne, S.; McGorry, P. Where next for Youth Mental Health Services in Ireland? Ir. J. Psychol. Med. 2019, 36, 163–167. [Google Scholar] [CrossRef]
- Rhodes, R.E.; Janssen, I.; Bredin, S.S.D.; Warburton, D.E.R.; Bauman, A. Physical Activity: Health Impact, Prevalence, Correlates and Interventions. Psychol. Health 2017, 32, 942–975. [Google Scholar] [CrossRef]
- Buchan, D.S.; Ollis, S.; Thomas, N.E.; Baker, J.S. Physical Activity Behaviour: An Overview of Current and Emergent Theoretical Practices. J. Obes. 2012, 2012. [Google Scholar] [CrossRef]
- Jeon, D.J.; Kim, K.J.; Heo, M. Factors Related to Stages of Exercise Behavior Change among University Students Based on the Transtheoretical Model. J. Phys. Ther. Sci. 2014, 26, 1929–1932. [Google Scholar] [CrossRef][Green Version]
- Dooley, B.; O’Connor, C.; Fitzgerald, A.; O’Reilly, A. My World Survey 2: The National Study of Youth Mental Health in Ireland; University College Dublin School of Psychology and Jigsaw, the National Centre for Youth Mental Health: Dublin, Ireland, 2019. [Google Scholar]
- Linton, M.-J.; Dieppe, P.; Medina-Lara, A.; Watson, L.; Crathorne, L. Review of 99 self-report measures for assessing well-being in adults: Exploring dimensions of well-being and developments over time. BMJ Open 2016, 6, e010641. [Google Scholar] [CrossRef]
- Sylvia, L.G.; Bernstein, E.E.; Hubbard, J.L.; Keating, L.; Anderson, E.J. Practical Guide to Measuring Physical activity. J. Acad. Nutr. Diet. 2014, 114, 199–208. [Google Scholar] [CrossRef] [PubMed]
- Alessandri, G.; Zuffianò, A.; Perinelli, E. Evaluating Intervention Programs with a Pretest-Posttest Design: A Structural Equation Modeling Approach. Front. Psychol. 2017, 8, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Paulus, J.K.; Dahabreh, I.J.; Balk, E.M.; Avendano, E.E.; Lau, J.; Ip, S. Opportunities and Challenges in Using Studies without a Control Group in Comparative Effectiveness Reviews. Res. Synth. Methods 2014, 5, 152–161. [Google Scholar] [CrossRef] [PubMed]
- Glasgow, R.E.; Harden, S.M.; Gaglio, B.; Rabin, B.; Smith, M.L.; Porter, G.C.; Ory, M.G.; Estabrooks, P.A. RE-AIM Planning and Evaluation Framework: Adapting to New Science and Practice with a 20-Year Review. Front. Public Health 2019, 7. [Google Scholar] [CrossRef] [PubMed]
| Day 1 Workshop A—Positive Mental Health |
| PART 1 Understanding positive mental health—Everyone has mental health Mental fitness: stress, resilience, and vulnerability Mental health, emerging adults, and ‘one good adult’ Neuroplasticity—mindfulness and positive affirmations |
| PART 2 Exercise has been known to cause health and happiness The five ways to wellbeing The transtheoretical model of change SMART—don’t find the time, make time |
| Day 2 Workshop B—Mental Health First |
| PART 1 Everyone has mental health—let’s talk stigma Mental health literacy and responding to mental health issues The stress-vulnerability bucket analogy Alcohol consumption and mental health |
| PART 2 Maintaining wellbeing strategies—mindfulness Mental health literacy SMART—Resetting physical activity goals The Mental Fitness toolkit |
| Gender | Count | Percentage (%) |
|---|---|---|
| Male | 39 | 29.1 |
| Female | 95 | 70.9 |
| Age | ||
| 18–25 years | 100 | 74.6 |
| 26–29 years | 19 | 14.2 |
| 30 years + | 15 | 11.2 |
| Level of Education | ||
| Undergraduate | 19 | 14.2 |
| Postgraduate | 115 | 85.8 |
| Year of study | ||
| First-year | 113 | 84.3 |
| Second-year | 17 | 12.7 |
| Third-year | 4 | 3 |
| Type of course | ||
| Education | 100 | 74.6 |
| Engineering | 19 | 14.2 |
| Science | 13 | 9.7 |
| Business | 2 | 1.5 |
| N | Pre SOMI-HE Mean Score (SD) | Post SOMI-HE Mean Score (SD) | t | df | Sig (2-Tailed) | |
|---|---|---|---|---|---|---|
| WEMWBS Male Female | 124 37 87 | 44.52 ± 7.53 47.20 ± 7.21 43.47 ± 7.43 | 48.28 ± 7.52 49.23 ± 6.72 47.91 ± 7.82 | −5.27 | 120 | 0.000 ** |
| BRS Male Female | 120 35 85 | 3.17 ± 0.68 3.47 ± 0.58 3.05 ± 0.69 | 3.25 ± 0.61 3.40 ± 0.60 3.19 ± 0.62 | −1.75 | 119 | 0.083 |
| PACE+ Male Female | 126 37 89 | 2.96 ± 1.6 3.26 ± 1.54 2.84 ± 1.6 | 3.5 ± 1.70 4.08 ± 1.49 3.29 ± 1.73 | −3.91 | 125 | 0.000 ** |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
O’Brien, N.; Lawlor, M.; Chambers, F.; O’Brien, W. State of Mind Ireland-Higher Education: A Mixed-Methods Longitudinal Evaluation of a Positive Mental Health Intervention. Int. J. Environ. Res. Public Health 2020, 17, 5530. https://doi.org/10.3390/ijerph17155530
O’Brien N, Lawlor M, Chambers F, O’Brien W. State of Mind Ireland-Higher Education: A Mixed-Methods Longitudinal Evaluation of a Positive Mental Health Intervention. International Journal of Environmental Research and Public Health. 2020; 17(15):5530. https://doi.org/10.3390/ijerph17155530
Chicago/Turabian StyleO’Brien, Niamh, Martin Lawlor, Fiona Chambers, and Wesley O’Brien. 2020. "State of Mind Ireland-Higher Education: A Mixed-Methods Longitudinal Evaluation of a Positive Mental Health Intervention" International Journal of Environmental Research and Public Health 17, no. 15: 5530. https://doi.org/10.3390/ijerph17155530
APA StyleO’Brien, N., Lawlor, M., Chambers, F., & O’Brien, W. (2020). State of Mind Ireland-Higher Education: A Mixed-Methods Longitudinal Evaluation of a Positive Mental Health Intervention. International Journal of Environmental Research and Public Health, 17(15), 5530. https://doi.org/10.3390/ijerph17155530






