Perinatal Mental Illness in the Middle East and North Africa Region—A Systematic Overview
Abstract
1. Introduction
2. Materials and Methods
2.1. Inclusion and Exclusion Criteria
2.2. Population of Interest
2.3. Primary Outcomes
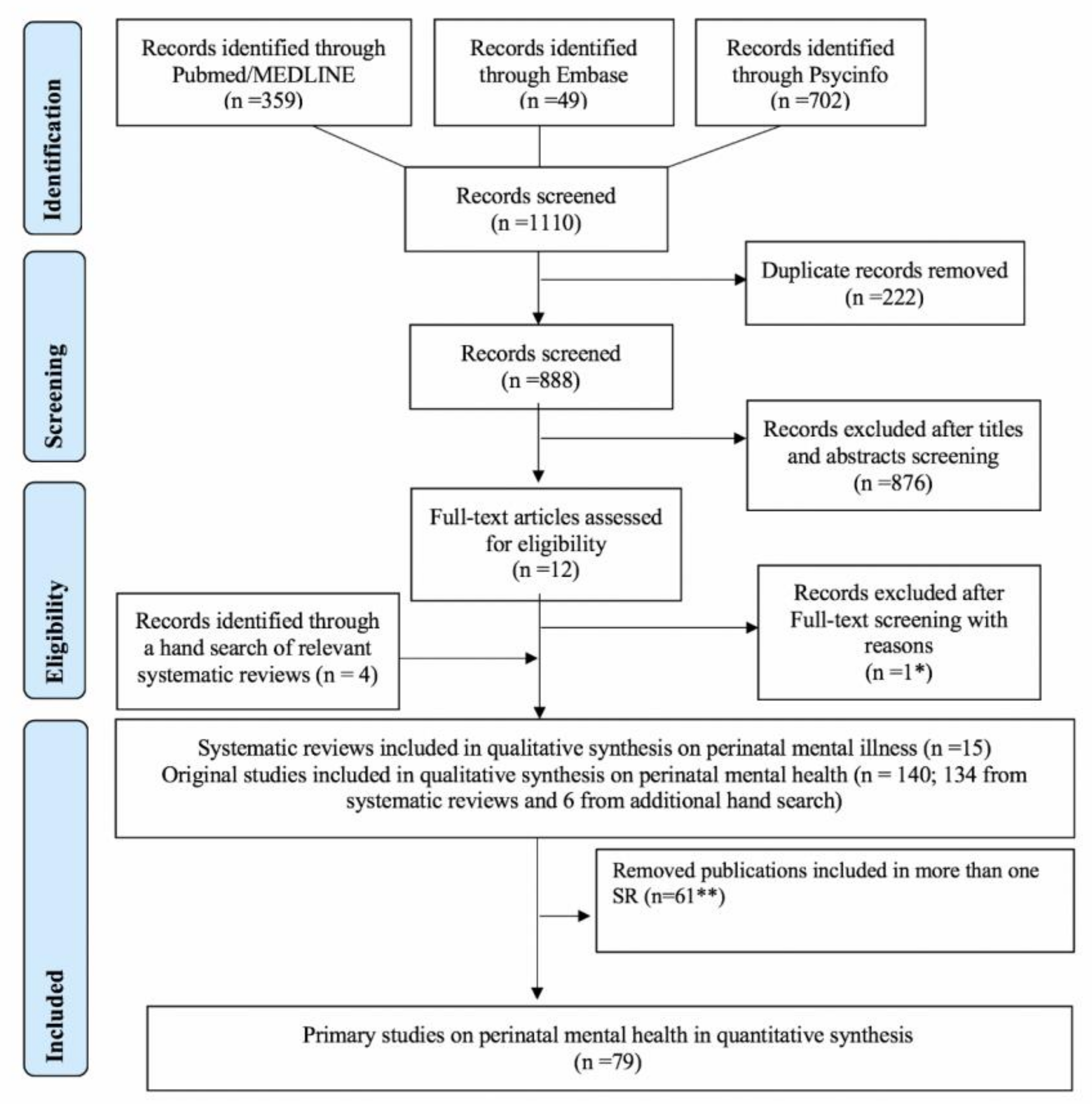
2.4. Literature Search and Data Management
2.5. Quality Assessment
2.6. Synthesis
3. Results
3.1. Characteristics of the Included SRs
3.2. Quality Assessment of the Included SRs
3.3. Overview of SRs with Prevalence Data
3.4. Suicidal Ideation and Suicides
3.5. Overview of SRs with Data on Risk Factors
3.6. Quality Assessment of the Primary Studies
3.7. Overview of Primary Studies with Prevalence Data
3.7.1. Antepartum
3.7.2. Postpartum
3.8. Overview of Primary Studies with Data on Risk Factors
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- O’Hara, M.W.; Wisner, K.L. Perinatal mental illness: Definition, description and aetiology. Best Pract. Res. Clin. Obstet. Gynaecol. 2014, 28, 3–12. [Google Scholar] [CrossRef] [PubMed]
- WHO. Maternal Mental Health and Child Health and Development in Low and Middle Income Countries: Report of the Meeting, Geneva, Switzerland, 30 January–1 February, 2008; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- Miranda, J.J.; Patel, V. Achieving the Millennium Development Goals: Does Mental Health Play a Role? PLoS Med. 2005, 2, e291. [Google Scholar] [CrossRef] [PubMed]
- Oates, M. Perinatal psychiatric disorders: A leading cause of maternal morbidity and mortality. Br. Med. Bull. 2003, 67, 219–229. [Google Scholar] [CrossRef]
- Wachs, T.D.; Black, M.M.; Engle, P.L. Maternal Depression: A Global Threat to Children’s Health, Development, and Behavior and to Human Rights. Child Dev. Perspect. 2009, 3, 51–59. [Google Scholar] [CrossRef]
- Hompes, T.; Izzi, B.; Gellens, E.; Morreels, M.; Fieuws, S.; Pexsters, A.; Schops, G.; Dom, M.; Van Bree, R.; Freson, K.; et al. Investigating the influence of maternal cortisol and emotional state during pregnancy on the DNA methylation status of the glucocorticoid receptor gene (NR3C1) promoter region in cord blood. J. Psychiatr. Res. 2013, 47, 880–891. [Google Scholar] [CrossRef] [PubMed]
- Hendrick, V.; Altshuler, L.; Cohen, L.; Stowe, Z. Evaluation of mental health and depression during pregnancy: Position paper. Psychopharmacol. Bull. 1998, 34, 297–299. [Google Scholar]
- Fisher, J.; De Mello, M.C.; Patel, V.; Rahman, A.; Tran, T.D.; Holton, S.; Holmes, W. Prevalence and determinants of common perinatal mental disorders in women in low- and lower-middle-income countries: A systematic review. Bull. World Heal. Organ. 2011, 90, 139–149. [Google Scholar] [CrossRef]
- Marmot, M.; Friel, S.; Bell, R.; Houweling, T.A.; Taylor, S. Closing the gap in a generation: Health equity through action on the social determinants of health. Lancet 2008, 372, 1661–1669. [Google Scholar] [CrossRef]
- Ali, N.S.; Azam, I.S.; Ali, B.S.; Tabbusum, G.; Moin, S.S. Frequency and Associated Factors for Anxiety and Depression in Pregnant Women: A Hospital-Based Cross-Sectional Study. Sci. World J. 2012, 2012, 653098. [Google Scholar] [CrossRef]
- Eloul, L.; Ambusaidi, A.; Al-Adawi, S. Silent Epidemic of Depression in Women in the Middle East and North Africa Region. Sultan Qaboos Univ. Med. J. 2009, 9, 5–15. [Google Scholar]
- Meltzer-Brody, S. New insights into perinatal depression: Pathogenesis and treatment during pregnancy and postpartum. Dialog-Clin. Neurosci. 2011, 13, 89–100. [Google Scholar]
- Higgins, J.G.S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. Available online: www.training.cochrane.org/handbook (accessed on 28 June 2020).
- Chaabna, K.; Cheema, S.; Abraham, A.; Alrouh, H.; Lowenfels, A.B.; Maisonneuve, P.; Mamtani, R. Systematic overview of hepatitis C infection in the Middle East and North Africa. World J. Gastroenterol. 2018, 24, 3038–3054. [Google Scholar] [CrossRef] [PubMed]
- Chaabna, K.; Cheema, S.; Abraham, A.; Alrouh, H.; Mamtani, R.; Sheikh, J. Gray literature in systematic reviews on population health in the Middle East and North Africa: Protocol of an overview of systematic reviews and evidence mapping. Syst. Rev. 2018, 7, 94. [Google Scholar] [CrossRef] [PubMed]
- Booth, A.; Clarke, M.; Dooley, G.; Ghersi, D.; Moher, D.; Petticrew, M.; Stewart, L.A. PROSPERO at one year: An evaluation of its utility. Syst. Rev. 2013, 2, 4. [Google Scholar] [CrossRef]
- Hutton, B.; Salanti, G.; Caldwell, D.M.; Chaimani, A.; Schmid, C.H.; Cameron, C.; Ioannidis, J.P.; Straus, S.; Thorlund, K.; Jansen, J.P.; et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: Checklist and explanations. Ann. Intern. Med. 2015, 162, 777–784. [Google Scholar] [CrossRef]
- Zorzela, L.; Loke, Y.K.; Ioannidis, J.P.; Golder, S.; Santaguida, P.; Altman, U.G.; Moher, D.; Vohra, S. PRISMA harms group PRISMA harms checklist: Improving harms reporting in systematic reviews. BMJ 2016, 352, i157. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. J. Clin. Epidemiol. 2009, 62, e1–e34. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. J. Clin. Epidemiol. 2009, 62, 1006–1012. [Google Scholar] [CrossRef]
- Beller, E.M.; Glasziou, P.P.; Altman, D.G.; Hopewell, S.; Bastian, H.; Chalmers, I.; Gøtzsche, P.C.; Lasserson, T.; Tovey, D.; for the PRISMA for Abstracts Group. PRISMA for Abstracts: Reporting Systematic Reviews in Journal and Conference Abstracts. PLoS Med. 2013, 10, e1001419. [Google Scholar] [CrossRef]
- World Population Prospects: The 2015 Revision. Available online: https://population.un.org/wpp/publications/files/key_findings_wpp_2015.pdf. (accessed on 28 June 2020).
- Birth Rate, Crude (per 1,000 people)—Middle East & North Africa | Data. Available online: https://data.worldbank.org/indicator/SP.DYN.CBRT.IN?locations=ZQ (accessed on 19 July 2020).
- National Institutes of Health. PubMed.gov US National Library of Medcine. Available online: http://www.ncbi.nlm.nih.gov/pubmed (accessed on 10 September 2017).
- Elmagarmid, A.; Fedorowicz, Z.; Hammady, H.; Ilyas, I.; Khabsa, M.; Ouzzani, M. Rayyan: A systematic reviews web app for exploring and filtering searches for eligible studies for Cochrane Reviews. In Evidence-Informed Public Health: Opportunities and Challenges. Abstracts of the 22nd Cochrane Colloquium; Cochrane Colloquium: Hyderabad, India, 2014. [Google Scholar]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan-a web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef]
- Shea, B.J.; Grimshaw, J.M.; Wells, G.A.; Boers, M.; Andersson, N.; Hamel, C.; Porter, A.C.; Tugwell, P.; Moher, D.; Bouter, L.M. Development of AMSTAR: A measurement tool to assess the methodological quality of systematic reviews. BMC Med. Res. Methodol. 2007, 7, 10. [Google Scholar] [CrossRef] [PubMed]
- PubMed Health. PICO Framework. Available online: https://www.ncbi.nlm.nih.gov/pubmedhealth/PMHT0029906/ (accessed on 6 February 2018).
- Furber, G.; Leach, M.; Guy, S.; Segal, L. Developing a broad categorisation scheme to describe risk factors for mental illness, for use in prevention policy and planning. Aust. N. Z. J. Psychiatry 2017, 51, 230–240. [Google Scholar] [CrossRef] [PubMed]
- Afzal, S.; Khalid, R. Postnatal Affective Disorders: Mapping the research in Pakistan. J. Gender Soc. Issues 2016, 15, 69–92. [Google Scholar]
- Amber Haque, A.N.; Breene, K.-A. Prevalence and Risk Factors of Postpartum Depression in Middle Eastern/Arab Women. J. Muslim Ment. Health 2015, 9. [Google Scholar] [CrossRef]
- Fuhr, D.C.; Calvert, C.; Ronsmans, C.; Chandra, P.S.; Sikander, S.; De Silva, M.J.; Patel, V. Contribution of suicide and injuries to pregnancy-related mortality in low-income and middle-income countries: A systematic review and meta-analysis. Lancet Psychiatry 2014, 1, 213–225. [Google Scholar] [CrossRef]
- James-Hawkins, L.; Shaltout, E.; Nur, A.A.; Nasrallah, C.; Qutteina, Y.; Abdul Rahim, H.F.; Hennink, M.; Yount, K.M. Human and economic resources for empowerment and pregnancy-related mental health in the Arab Middle East: A systematic review. Arch. Womens Ment. Health 2019, 22, 1–14. [Google Scholar] [CrossRef]
- Jones, E.; Coast, E. Social relationships and postpartum depression in South Asia: A systematic review. Int. J. Soc. Psychiatry 2013, 59, 690–700. [Google Scholar] [CrossRef]
- Klainin, P.; Arthur, D.G. Postpartum depression in Asian cultures: A literature review. Int. J. Nurs. Stud. 2009, 46, 1355–1373. [Google Scholar] [CrossRef]
- Mahendran, R.; Puthussery, S.; Amalan, M. Prevalence of antenatal depression in South Asia: A systematic review and meta-analysis. J. Epidemiol. Commun. Health 2019, 73, 768–777. [Google Scholar] [CrossRef]
- Qutteina, Y.; Nasrallah, C.; James-Hawkins, L.; Nur, A.A.; Yount, K.M.; Hennink, M.; Abdul Rahim, H.F. Social resources and Arab women’s perinatal mental health: A systematic review. Women Birth 2018, 31, 386–397. [Google Scholar] [CrossRef]
- Shorey, S.; Chee, C.Y.I.; Ng, E.D.; Chan, Y.H.; Tam, W.W.S.; Chong, Y.S. Prevalence and incidence of postpartum depression among healthy mothers: A systematic review and meta-analysis. J. Psychiatr. Res. 2018, 104, 235–248. [Google Scholar] [CrossRef] [PubMed]
- Zahidie, A.; Jamali, T. An overview of the predictors of depression among adult Pakistani women. J. Coll. Physicians Surg. Pak. 2013, 23, 574–580. [Google Scholar]
- Sawyer, A.; Ayers, S.; Smith, H. Pre- and postnatal psychological wellbeing in Africa: A systematic review. J. Affect. Disord. 2010, 123, 17–29. [Google Scholar] [CrossRef] [PubMed]
- Stewart, R.C. Maternal depression and infant growth: A review of recent evidence. Matern. Child. Nutr. 2007, 3, 94–107. [Google Scholar] [CrossRef] [PubMed]
- Alhasanat, D.; Fry-McComish, J. Postpartum depression among immigrant and Arabic women: Literature review. J. Immigr. Minor. Heal. 2015, 17, 1882–1894. [Google Scholar] [CrossRef]
- Evagorou, O.; Arvaniti, A.; Samakouri, M. Cross-Cultural Approach of Postpartum Depression: Manifestation, Practices Applied, Risk Factors and Therapeutic Interventions. Psychiatr. Q. 2016, 87, 129–154. [Google Scholar] [CrossRef]
- Abdelhai, R.; Mosleh, H. Screening for antepartum anxiety and depression and their association with domestic violence among Egyptian pregnant women. J. Egypt. Public Health Assoc. 2015, 90, 101–108. [Google Scholar] [CrossRef]
- Abou-Saleh, M.T.; Ghubash, R. The prevalence of early postpartum psychiatric morbidity in Dubai: A transcultural perspective. Acta Psychiatr. Scand. 1997, 95, 428–432. [Google Scholar] [CrossRef]
- Abujilban, S.K.; Abuidhail, J.; Al-Modallal, H.; Hamaideh, S.; Mosemli, O. Predictors of antenatal depression among Jordanian pregnant women in their third trimester. Health Care Women Int. 2014, 35, 200–215. [Google Scholar] [CrossRef]
- Agoub, M.; Moussaoui, D.; Battas, O. Prevalence of postpartum depression in a Moroccan sample. Arch. Womens Ment. Health 2005, 8, 37–43. [Google Scholar] [CrossRef]
- Al Dallal, F.H.; Grant, I.N. Postnatal depression among Bahraini women: Prevalence of symptoms and psychosocial risk factors. East Mediterr. Health J. 2012, 18, 439–445. [Google Scholar] [CrossRef] [PubMed]
- Al Hinai, F.I.; Al Hinai, S.S. Prospective study on prevalence and risk factors of postpartum depression in Al-dakhliya governorate in oman. Oman. Med. J. 2014, 29, 198–202. [Google Scholar] [CrossRef] [PubMed]
- Al-Azri, M.; Al-Lawati, I.; Al-Kamyani, R.; Al-Kiyumi, M.; Al-Rawahi, A.; Davidson, R.; Al-Maniri, A. Prevalence and Risk Factors of Antenatal Depression among Omani Women in a Primary Care Setting: Cross-sectional study. Sultan Qaboos. Univ. Med. J. 2016, 16, e35–e41. [Google Scholar] [CrossRef] [PubMed]
- Alami, K.M.; Kadri, N.; Berrada, S. Prevalence and psychosocial correlates of depressed mood during pregnancy and after childbirth in a Moroccan sample. Arch. Womens Ment. Health 2006, 9, 343–346. [Google Scholar] [CrossRef]
- Bener, A.; Burgut, F.T.; Ghuloum, S.; Sheikh, J. A study of postpartum depression in a fast developing country: Prevalence and related factors. Int. J. Psychiatry Med. 2012, 43, 325–337. [Google Scholar] [CrossRef]
- Chaaya, M.; Campbell, O.M.; El Kak, F.; Shaar, D.; Harb, H.; Kaddour, A. Postpartum depression: Prevalence and determinants in Lebanon. Arch. Womens Ment. Health 2002, 5, 65–72. [Google Scholar] [CrossRef]
- Green, K.; Broome, H.; Mirabella, J. Postnatal depression among mothers in the United Arab Emirates: Socio-cultural and physical factors. Psychol. Health Med. 2006, 11, 425–431. [Google Scholar] [CrossRef]
- Haider, I. Screening of antenatal depression in Pakistan: Risk factors and effects on obsetric and neonatal outcomes. Asia-Pacific Psy. 2010, 2, 26–32. [Google Scholar]
- Hamdan, A.; Tamim, H. Psychosocial risk and protective factors for postpartum depression in the United Arab Emirates. Arch. Womens Ment. Health 2011, 14, 125–133. [Google Scholar] [CrossRef]
- Husain, N.; Bevc, I.; Husain, M.; Chaudhry, I.B.; Atif, N.; Rahman, A. Prevalence and social correlates of postnatal depression in a low income country. Arch. Womens Ment. Health 2006, 9, 197–202. [Google Scholar] [CrossRef]
- Husain, N.; Parveen, A.; Husain, M.; Saeed, Q.; Jafri, F.; Rahman, R.; Tomenson, B.; Chaudhry, I.B. Prevalence and psychosocial correlates of perinatal depression: A cohort study from urban Pakistan. Arch. Womens Ment. Health 2011, 14, 395–403. [Google Scholar] [CrossRef] [PubMed]
- Kalyani, G.H.S.; Saeed, K.; Rehman, C.I.U.; Mubbashar, M.H. Incidence of depressive illness in Pakistani women during postnatal period. J. Coll. Physicians Surg. Pak. 2001, 11, 246–248. [Google Scholar]
- Karmaliani, R.; Asad, N.; Bann, C.M.; Moss, N.; McClure, E.M.; Pasha, O.; Wright, L.L.; Goldenberg, R.L. Prevalence of anxiety, depression and associated factors among pregnant women of Hyderabad, Pakistan. Int. J. Soc. Psychiatry 2009, 55, 414–424. [Google Scholar] [CrossRef] [PubMed]
- Lteif, Y.; Kesrouani, A.; Richa, S. [Depressive syndromes during pregnancy: Prevalence and risk factors]. J. Gynecol. Obstet. Biol. Reprod. 2005, 34, 262–269. [Google Scholar] [CrossRef]
- Masmoudi, J.; Charfeddine, F.; Trabelsi, S.; Feki, I.; Ben Ayad, B.; Guermazi, M.; Baati, I.; Jaoua, A. Postpartum depression: Prevalence and risk factors. A prospective Study concerning 302 Tunisian parturients. Tunis Med. 2014, 92, 615–621. [Google Scholar] [PubMed]
- Masmoudi, J.; Tabelsi, S.; Charfeddine, F.; Ben Ayed, B.; Guermazzi, M.; Jaoua, A. Study of the prevalence of postpartum depression among 213 Tunisian parturients. Gynecol. Obstet. Fertil. 2008, 36, 782–787. [Google Scholar] [CrossRef]
- Masmoudi, J.; Trabelsi, S.; Charfeddine, F.; Ben Ayed, B.; Guermazi, M.; Jaoua, A.; Karam, E.G.; Hantouche, E.G. Evaluation of affective temperaments in the postpartum depressive symptomatology. Encephale 2010, 36 Suppl 2, D14–D21. [Google Scholar] [CrossRef]
- Mohammad, K.I.; Gamble, J.; Creedy, D.K. Prevalence and factors associated with the development of antenatal and postnatal depression among Jordanian women. Midwifery 2011, 27, e238–e245. [Google Scholar] [CrossRef]
- Rahman, A.; Creed, F. Outcome of prenatal depression and risk factors associated with persistence in the first postnatal year: Prospective study from Rawalpindi, Pakistan. J. Affect. Disord. 2007, 100, 115–121. [Google Scholar] [CrossRef]
- Rahman, A.; Iqbal, Z.; Harrington, R. Life events, social support and depression in childbirth: Perspectives from a rural community in the developing world. Psychol. Med. 2003, 33, 1161–1167. [Google Scholar] [CrossRef]
- Shah, S.M.; Bowen, A.; Afridi, I.; Nowshad, G.; Muhajarine, N. Prevalence of antenatal depression: Comparison between Pakistani and Canadian women. J. Pak. Med. Assoc. 2011, 61, 242–246. [Google Scholar]
- Yehia, D.B.; Callister, L.C.; Hamdan-Mansour, A. Prevalence and predictors of postpartum depression among Arabic Muslim Jordanian women serving in the military. J. Perinat Neonat. Nurs. 2013, 27, 25–33, quiz 34–25. [Google Scholar] [CrossRef] [PubMed]
- Zahidie, A.; Kazi, A.; Fatmi, Z.; Bhatti, M.T.; Dureshahwar, S. Social environment and depression among pregnant women in rural areas of Sind, Pakistan. J. Pak. Med. Assoc. 2011, 61, 1183–1189. [Google Scholar] [PubMed]
- Bener, A.; Gerber, L.M.; Sheikh, J. Prevalence of psychiatric disorders and associated risk factors in women during their postpartum period: A major public health problem and global comparison. Int. J. Womens Health 2012, 4, 191–200. [Google Scholar] [CrossRef] [PubMed]
- Amr, M.A.; Hussein Balaha, M.H. Minor psychiatric morbidity in young saudi mothers using Mini International Neuropsychiatric Interview (MINI). J. Coll. Physicians Surg. Pak. 2010, 20, 680–684. [Google Scholar] [CrossRef]
- Ghubash, R.; Eapen, V. Postpartum mental illness: Perspectives from an Arabian Gulf population. Psychol. Rep. 2009, 105, 127–136. [Google Scholar] [CrossRef]
- Gulamani, S.S.; Premji, S.S.; Kanji, Z.; Azam, S.I. A review of postpartum depression, preterm birth, and culture. J. Perinat. Neonat. Nurs. 2013, 27, 52–59. [Google Scholar] [CrossRef]
- Husain, N.; Munshi, T.; Jafri, F.; Husain, M.; Parveen, A.; Saeed, Q.; Tomenson, B.; Naeem, F.; Chaudhry, N. Antenatal depression is not associated with low-birth weight: A study from urban Pakistan. Front. Psychiatry 2014, 5, 175. [Google Scholar] [CrossRef]
- Kazi, A.; Fatmi, Z.; Hatcher, J.; Kadir, M.M.; Niaz, U.; Wasserman, G.A. Social environment and depression among pregnant women in urban areas of Pakistan: Importance of social relations. Soc. Sci. Med. 2006, 63, 1466–1476. [Google Scholar] [CrossRef]
- Abuidhail, J.; Abujilban, S. Characteristics of Jordanian depressed pregnant women: A comparison study. J. Psychiatr. Ment. Health Nurs. 2014, 21, 573–579. [Google Scholar] [CrossRef]
- Ahmed, M.k.a.I. Risk factors associated with Postnatal depression in Pakistani women. Pak. J. Soc. Clin. Psych. 2005, 3, 41–50. [Google Scholar]
- Alasoom, L.I.; Koura, M.R. Predictors of postpartum depression in the eastern province capital of saudi arabia. J. Family Med. Prim. Care 2014, 3, 146–150. [Google Scholar] [CrossRef] [PubMed]
- Alharbi, A.A.; Abdulghani, H.M. Risk factors associated with postpartum depression in the Saudi population. Neuropsychiatr. Dis. Treat. 2014, 10, 311–316. [Google Scholar] [CrossRef] [PubMed]
- Ali, F.A.; Israr, S.M.; Ali, B.S.; Janjua, N.Z. Association of various reproductive rights, domestic violence and marital rape with depression among Pakistani women. BMC Psychiatry 2009, 9, 77. [Google Scholar] [CrossRef] [PubMed]
- Asad, N.; Karmaliani, R.; Sullaiman, N.; Bann, C.M.; McClure, E.M.; Pasha, O.; Wright, L.L.; Goldenberg, R.L. Prevalence of suicidal thoughts and attempts among pregnant Pakistani women. Acta Obstet. Gynecol. Scand. 2010, 89, 1545–1551. [Google Scholar] [CrossRef]
- Balaha, M.; Amr, M.; El-Gilany, A.-H.; Sheikh, F. Obstetric and Psychiatric Outcomes in a Sample of Saudi Teen-Aged Mothers. TAF Prev. Med. Bull. 2009, 8, 285. [Google Scholar]
- Bener, A. Psychological distress among postpartum mothers of preterm infants and associated factors: A neglected public health problem. Braz. J. Psychiatry 2013, 35, 231–236. [Google Scholar] [CrossRef]
- Burgut, F.T.; Bener, A.; Ghuloum, S.; Sheikh, J. A study of postpartum depression and maternal risk factors in Qatar. J. Psychosom. Obstet. Gynaecol. 2013, 34, 90–97. [Google Scholar] [CrossRef]
- Din, Z.U.; Ambreen, S.; Iqbal, Z.; Iqbal, M.; Ahmad, S. Determinants of Antenatal Psychological Distress in Pakistani Women. Noro. Psikiyatr. Ars. 2016, 53, 152–157. [Google Scholar] [CrossRef]
- El-Hachem, C.; Rohayem, J.; Bou Khalil, R.; Richa, S.; Kesrouani, A.; Gemayel, R.; Aouad, N.; Hatab, N.; Zaccak, E.; Yaghi, N.; et al. Early identification of women at risk of postpartum depression using the Edinburgh Postnatal Depression Scale (EPDS) in a sample of Lebanese women. BMC Psychiatry 2014, 14, 242. [Google Scholar] [CrossRef]
- El-Khoury, N.; Karam, E.G.; Melhem, N.M. [Depression and pregnancy]. J. Med. Liban 1999, 47, 169–174. [Google Scholar] [PubMed]
- Fareeha Hamid, A.A.; Haider, I.I. Study of anxiety and depression during pregnancy. Pak. J. Med. Sci. 2008, 24, 861–864. [Google Scholar]
- Farhat, E.B.; Chaouch, M.; Chelli, H.; Gara, M.F.; Boukraa, N.; Garbouj, M.; Hamrouni, M.; Fourati, A.; Calvez, T.; Thonneau, P. Reduced maternal mortality in Tunisia and voluntary commitment to gender-related concerns. Int. J. Gynaecol. Obstet. 2012, 116, 165–168. [Google Scholar] [CrossRef] [PubMed]
- Ghazala Sadiq, S.S.; Namrah, A. Evaluation of PostPartum Depression in Rawalpindi/ Islamabad Pakistan. EC Gynaecol. 2015, 1, 19–25. [Google Scholar]
- Ghubash, R.; Abou-Saleh, M.T. Postpartum psychiatric illness in Arab culture: Prevalence and psychosocial correlates. Br. J. Psychiatry 1997, 171, 65–68. [Google Scholar] [CrossRef]
- Gul, M.; Bajwa, S.; Niaz, S.; Haroon, M.; Liaqat, S.; Ahmad, M.; Dawood, S.; Ghazal, F.; Bhatti, A.A.; Nazir, S.; et al. Postnatal depression and its comparison with the gender of newborn in fourth pregnancy. Int. J. Cul. Mental Health 2013, 6, 16–28. [Google Scholar] [CrossRef]
- Habib, S.; Khalid, R. Pregnancy related Psychiatric Problems. 1997. Unpublished manuscript. [Google Scholar]
- Humayun, A.; Haider, I.I.; Imran, N.; Iqbal, H.; Humayun, N. Antenatal depression and its predictors in Lahore, Pakistan. East. Mediterr. Health J. 2013, 19, 327–332. [Google Scholar] [CrossRef]
- Husain, N.; Gater, R.; Tomenson, B.; Creed, F. Social factors associated with chronic depression among a population-based sample of women in rural Pakistan. Soc. Psych. Psychiatr. Epidemiol. 2004, 39, 618–624. [Google Scholar] [CrossRef]
- Jafarey, S.N.; Rizvi, T.; Koblinsky, M.; Kureshy, N. Verbal autopsy of maternal deaths in two districts of Pakistan--filling information gaps. J. Health Popul. Nutr. 2009, 27, 170–183. [Google Scholar] [CrossRef]
- Karmaliani, R.; Bann, C.M.; Mahmood, M.A.; Harris, H.S.; Akhtar, S.; Goldenberg, R.L.; Moss, N. Measuring antenatal depression and anxiety: Findings from a community-based study of women in Hyderabad, Pakistan. Women Health 2006, 44, 79–103. [Google Scholar] [CrossRef] [PubMed]
- Khabour, O.; Amarneh, B.; Bani Hani, E.; Lataifeh, I. Associations Between Variations in TPH1, TPH2 and SLC6A4 Genes and Postpartum Depression: A Study in the Jordanian Population. Balkan J. Med. Genet. 2013, 16, 41–48. [Google Scholar] [CrossRef] [PubMed]
- Khalid, R. Maternity blues and puerperal depression in Pakistani women. Pak. J. Psych. Res. 1989, 4, 3–4. [Google Scholar]
- Khalifa, D.S.; Glavin, K.; Bjertness, E.; Lien, L. Postnatal depression among Sudanese women: Prevalence and validation of the Edinburgh Postnatal Depression Scale at 3 months postpartum. Int. J. Womens Health 2015, 7, 677–684. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, R.; Munaf, S. Nuclear Family system as an Important risk factor for the development of the baby blues. Pak. J. Soc. Clin. Psychol. 2006, 4, 67–74. [Google Scholar]
- Muneer, A.; Minhas, F.A.; Tamiz-ud-Din Nizami, A.; Mujeeb, F.; Usmani, A.T. Frequency and associated factors for postnatal depression. J. Coll. Physicians Surg. Pak. 2009, 19, 236–239. [Google Scholar]
- Naglaa, A.; Mohamed, G.A.M.; Nadia, A.; Said, K.; Hamida, A.; Maklof, A. Postpartum Depression: Prevalence and Predictors among Women at El Eman’s Specialized Hospital. J. Am. Sci. 2011, 7, 122–128. [Google Scholar]
- Nayak, M.B.; Al-Yattama, M. Assault victim history as a factor in depression during pregnancy. Obstet. Gynecol. 1999, 94, 204–208. [Google Scholar] [CrossRef]
- Osman, H.; Saliba, M.; Chaaya, M.; Naasan, G. Interventions to reduce postpartum stress in first-time mothers: A randomized-controlled trial. BMC Womens Health 2014, 14, 125. [Google Scholar] [CrossRef]
- Ministry of Health and Population Egypt. The National Maternal Mortality Study: Egypt 2000; Ministry of Health and Population: Cairo, Egypt, 2000. [Google Scholar]
- Rahman, A.; Iqbal, Z.; Bunn, J.; Lovel, H.; Harrington, R. Impact of maternal depression on infant nutritional status and illness: A cohort study. Arch. Gen. Psychiatry 2004, 61, 946–952. [Google Scholar] [CrossRef]
- Rahman, A.; Lovel, H.; Bunn, J.; Iqbal, Z.; Harrington, R. Mothers’ mental health and infant growth: A case-control study from Rawalpindi, Pakistan. Child. Care Health Dev. 2004, 30, 21–27. [Google Scholar] [CrossRef] [PubMed]
- Rasheed, H.; Khalid, R. Maternity blues and Symptoms of Puerperal Depression four weeks after child birth: A comparitive study. 1988. Unpublished thesis. [Google Scholar]
- Sadaf, M. Antenatal Screening for Postpartum Depression. J. Rawalpindi Med. Coll. 2011, 15, 47–49. [Google Scholar]
- Saeed, A.; Raana, T.; Saeed, A.M.; Humayun, A. Effect of antenatal depression on maternal dietary intake and neonatal outcome: A prospective cohort. Nutr. J. 2016, 15, 64. [Google Scholar] [CrossRef]
- Saleh el, S.; El-Bahei, W.; Del El-Hadidy, M.A.; Zayed, A. Predictors of postpartum depression in a sample of Egyptian women. Neuropsychiatr. Dis. Treat. 2013, 9, 15–24. [Google Scholar] [CrossRef]
- Sarwar, A.; Khalid, R. To stuady Postnatal depression among pakistani women. 1990. Unpublished thesis. [Google Scholar]
- Sharifa Mir, R.K.; Hatcher, J.; Asad, N.; Sikander, S. Prevalence and risk factors contributing to depression among pregnant women in district Chitral, Pakistan. J. Pak. Psych. Soc. 2012, 9, 28–36. [Google Scholar]
- Stuchbery, M.; Matthey, S.; Barnett, B. Postnatal depression and social supports in Vietnamese, Arabic and Anglo-Celtic mothers. Soc. Psych. Epid. 1998, 33, 483–490. [Google Scholar] [CrossRef] [PubMed]
- Syeda Rabia, U.N.; Qazi, S.; Afreen, H. Frequency and Risk Profiles Associated with Antenatal Anxiety and Depression in Middle Socioeconomic Women. Ann. Abbasi Shaheed Hosp. Karachi & K.M.D.C. 2017, 22, 88–96. [Google Scholar]
- Waqas, A.; Raza, N.; Lodhi, H.W.; Muhammad, Z.; Jamal, M.; Rehman, A. Psychosocial factors of antenatal anxiety and depression in Pakistan: Is social support a mediator? PLoS ONE 2015, 10, e0116510. [Google Scholar] [CrossRef]
- Yasmeen, K.; Tayyaba, M.; Chatan, D.; Naeem, M.; Numan, M.; Adnan Maqsood, C. Associated Risk Factors for Postpartum Depression Presenting at a Teaching Hospital. Ann. King Edward Med. Uni. 2010, 16. [Google Scholar] [CrossRef]
- Al-Modayfer, O.; Alatiq, Y.; Khair, O.; Abdelkawi, S. Postpartum depression and related risk factors among Saudi females. Int. J. Cul. Mental Health 2015, 8, 316–324. [Google Scholar] [CrossRef]
- Amarin, Z.; Khader, Y.; Okour, A.; Jaddou, H.; Al-Qutob, R. National maternal mortality ratio for Jordan, 2007-2008. Int. J. Gynaecol. Obstet. 2010, 111, 152–156. [Google Scholar] [CrossRef] [PubMed]
- Melrose, S. Seasonal Affective Disorder: An Overview of Assessment and Treatment Approaches. Depress. Res. Treat. 2015, 2015, 178564. [Google Scholar] [CrossRef] [PubMed]
- Azam, I.S. Post partum anxiety and depression in peri-urban communities of Karachi, Pakistan: A quasi-experimental study. BMC Public Health 2009, 9, 384. [Google Scholar] [CrossRef]
- Tsai, A.C.; Scott, J.A.; Hung, K.J.; Zhu, J.Q.; Matthews, L.T.; Psaros, C.; Tomlinson, M. Reliability and validity of instruments for assessing perinatal depression in African settings: Systematic review and meta-analysis. PLoS ONE 2013, 8, e82521. [Google Scholar] [CrossRef] [PubMed]
- Patel, V. Explanatory models of mental illness in sub-Saharan Africa. Soc. Sci. Med. 1995, 40, 1291–1298. [Google Scholar] [CrossRef]
- Cox, J.L.; Holden, J.M.; Sagovsky, R. Detection of Postnatal Depression. Br. J. Psychiatry 1987, 150, 782–786. [Google Scholar] [CrossRef]
- Afzal, S.; Khalid, R. Social Support and Postnatal Depression in Pakistani Context. Pak. J. Soc. Clin. Psychol. 2014, 12, 34–38. [Google Scholar]
- Levis, B.; Yan, X.W.; He, C.; Sun, Y.; Benedetti, A.; Thombs, B.D. Comparison of depression prevalence estimates in meta-analyses based on screening tools and rating scales versus diagnostic interviews: A meta-research review. BMC Med. 2019, 17, 65. [Google Scholar] [CrossRef]
- Thombs, B.D.; Kwakkenbos, L.; Levis, A.W.; Benedetti, A. Addressing overestimation of the prevalence of depression based on self-report screening questionnaires. CMAJ 2018, 190, E44–E49. [Google Scholar] [CrossRef]
| Systematic Review | A Priori Design Included? | Duplicate Study Selection/Data Extraction? | Comprehensive Literature Search Performed? | Status of Publication as Inclusion Criteria? | List of Included Studies Provided? | Characteristics of Included Studies Provided? * | Quality of Studies Assessed and Documented? | Quality Assessment Used Appropriately? | Methods Used to Combine Results Appropriate? | Likelihood of Publication Bias Assessed? | Conflict of Interest Stated? ** | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (Afzal and Khalid, 2016) [30] | − | − | + | + | + | + | + | − | - | − | − | |
| (Alhasanat and Fry-McComish, 2015) [42] | − | + | + | − | + | + | − | − | - | − | − | |
| (Amber Haque, 2015) [31] | − | N/A | + | − | + | + | − | − | - | − | − | |
| (Evagorou et al., 2016) [43] | − | − | + | − | − | − | − | − | - | − | − | |
| (Fisher et al., 2012) [8] | − | − | + | − | + | + | + | + | + | + | + | |
| (Fuhr et al., 2014) [32] | + | + | + | + | + | + | + | + | + | + | + | |
| (James-Hawkins et al., 2019) [33] | + | + | + | + | + | + | + | + | - | N/A | + | |
| (Jones and Coast, 2013) [34] | − | − | + | - | + | + | − | − | - | − | + | |
| (Klainin and Arthur, 2009) [35] | + | − | + | − | + | + | − | − | - | − | + | |
| (Mahendran et al., 2019) [36] | N/A | + | + | + | + | + | + | + | + | + | + | |
| (Qutteina et al., 2018) [37] | − | + | + | - | + | + | + | + | - | N/A | + | |
| (Sawyer et al., 2010) [40] | − | N/A | + | − | + | + | − | − | - | − | + | |
| (Shorey et al., 2018) [38] | + | + | + | + | + | + | + | + | + | + | + | |
| (Stewart, 2007) [41] | − | − | − | − | + | + | − | − | - | − | − | |
| (Zahidie and Jamali, 2013) [39] | − | − | − | − | + | + | − | − | - | − | − | |
| Country | Study | Illness | Study Setting | Sample Size | Study Instrument | Instrument Cut off Score | Antepartum | Postpartum | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1st Trimester | 2nd Trimester | 3rd Trimester | All Three | <6 Weeks | 6 Weeks to 3 Months | >3 Months up to 1 Year | |||||||
| Bahrain | (Al Dallal and Grant, 2012) [48] | Depression | Hospital | 237 | EPDS | ≥12 | - | - | - | - | - | 37.1% | - |
| Egypt | (Naglaa A. Mohamed and Maklof, 2011) [104] | Depression | Hospital | 110 | EPDS | Unclear | - | - | - | - | - | - | 51.8% |
| Egypt | (Saleh el et al., 2013) [113] | Depression | Unclear | 120 | EPDS | ≥13 | - | - | - | - | - | - | 17.9% |
| Jordan | (Mohammad et al., 2011) [65] | Depression | Hospital | 353 | EPDS | Unclear | - | - | 19.0% | - | - | 22.1% | 21.2% |
| Jordan | (Yehia et al., 2013) [69] | Depression | Hospital | 300 | EPDS | Unclear | - | - | - | - | - | - | 83.0% |
| Lebanon | (Chaaya et al., 2002) [53] | Depression | Hospital | 396 | EPDS | >12 | - | - | - | - | - | - | 21.0% |
| Morocco | (Agoub et al., 2005) [47] | Depression | Hospital | 144 | MINI | N/A | - | - | - | - | 6.9–18.7% | - | 5.6–11.8% |
| 144 | EPDS | >12 | - | - | - | - | 20.1% | - | - | ||||
| Morocco | (Alami et al., 2006) [51] | Depression | Hospital | 100 | EPDS | Unclear | - | - | - | - | 21% | - | - |
| 100 | MINI | N/A | 17.4% | 16.0% | 15.7%% | 19.2% | 16.8% | 14.0% | 6–12% | ||||
| Oman | (Al Hinai and Al Hinai, 2014) [49] | Depression | Hospital | 282 | EPDS | >13 | - | - | - | - | 13.5% | 10.6% | - |
| Pakistan | (Ahmed, 2005) [78] | Depression | Hospital | 90 | EPDS | Unclear | - | - | - | - | - | - | 27.0% |
| Pakistan | (Ali et al., 2009) [80] | Depression& Anxiety | Community | Unclear | AKUADS/ Unclear diagnostic tool | Unclear | - | - | - | - | - | - | 28.8% * |
| Pakistan | (Ali et al., 2012) [81] | Depression | Hospital | 167 | HADS | ≥8 | - | - | - | 16.8% | - | - | - |
| Pakistan | (Din et al., 2016) [86] | Depression | Hospital | 230 | DASS-42 | ≥9 | - | - | 29.1% | - | - | - | - |
| Pakistan | (Gulamani et al., 2013) [74] | Depression | Hospital | 214 | EPDS | Unclear | - | - | - | - | 15.3–35.3% | - | |
| Pakistan | (Habib, 1997) [94] | Postnatal blues & PPD | Unclear | 30 | Gordon’s (1984); Pitt’s (1968) | Unclear | - | - | - | - | 50.0% | - | 20–37% |
| Pakistan | (Fareeha Hamid, 2008) [89] | Depression | Hospital | 100 | HADS | Unclear | - | - | - | 18.0% | - | - | - |
| Pakistan | (Humayun et al., 2013) [95] | Depression | Hospital | 506 | EPDS | ≥ 10 | - | - | 75.0% | - | - | - | - |
| Pakistan | (Husain et al., 2006) [57] | Depression | Community | 149 | EPDS | ≥12 | - | - | - | - | - | 36.0% | - |
| Pakistan | (Husain et al., 2011) [58] | Depression | Hospital | 149 | EPDS | >12 | - | - | 25.8% | - | - | - | 38.3% |
| Pakistan | (Husain et al., 2014) [75] | Depression | Hospital | 1357 | EPDS | ≥12 | - | - | 13.4% | - | - | - | - |
| Pakistan | (Haider, 2010)[55] | Depression | Hospital | 213 | EPDS | >12 | - | - | 42.7% | - | - | - | - |
| Pakistan | (Kalyani et al., 2001) [59] | Depression | Community | 120 | EPDS | >10 | - | - | - | - | 63.3% | - | - |
| Pakistan | (Karmaliani et al., 2006) [98] | Perinatal mental disorders | Community | 1000 | AKUADS | Unclear | - | 11.5% | - | - | - | - | - |
| Pakistan | (Karmaliani et al., 2009) [60] | Depression | Community | 1368 | AKUADS | ≥13 | - | 18.0% | - | - | - | - | - |
| Pakistan | (Kazi et al., 2006) [76] | Depression | Hospital | 292 | CES-D | ≥16 | - | - | - | 39.4% | - | - | - |
| Pakistan | (Sharifa Mir, 2012) [115] | Depression | Hospital | 328 | AKUADS | >13 | - | - | - | 33.8% | - | - | - |
| Pakistan | (Muneer et al., 2009) [103] | Depression | Unclear | 154 | EPDS | Unclear | - | - | - | - | - | - | 33.0% |
| Pakistan | (Asad et al., 2010) [83] | Depression/ Anxiety | Hospital | 1368 | AKUADS | Unclear | - | 18.0% | - | - | - | - | - |
| Pakistan | (Syeda Rabia, 2017) [117] | Depression | Hospital | 520 | HADS | >8 | - | - | - | 23.1% | - | - | - |
| Pakistan | (Rahman et al., 2003)[67] | Perinatal mental disorders | Community | T0 = 701 T1 = 632 T2 = 541 | SCAN | N/A | - | - | 25.0% (T1) | - | - | 28.0% (T2) | - |
| Pakistan | (Rahman et al., 2004a) [108] | Depression | Community | 265 | SCAN | N/A | - | - | - | - | - | - | 25.0% |
| Pakistan | (Rahman et al., 2004b) [109] | Depression | Hospital | 172 | SRQ-20 | Unclear | - | - | - | - | - | - | 41.0% |
| Pakistan | (Rahman and Creed, 2007) [66] | Depression | Community | T1: 701 (antepartum) T2: 632 T3: 160 T4: 129 | SCAN | N/A | - | - | - | - | 94.0% (T2) | 76.0% (T3) | 62% (T4) |
| Pakistan | (Rasheed, 1988) [110] | Postnatal blues & PPD | Unclear | 103 | Unclear | Unclear | - | - | - | - | - | - | 54.4% |
| Pakistan | (Sadaf, 2011) [111] | Depression | Hospital | 150 | HAM-D | Unclear | - | - | - | 10.0% | - | - | - |
| Pakistan | (Saeed et al., 2016) [112] | Depression | Hospital | 82 | EPDS | ≥9 | - | - | - | 42.7% | - | - | - |
| Pakistan | (Shah et al., 2011) [68] | Depression | Community | 128 | EPDS | ≥13 | - | - | - | 46.9% | - | - | - |
| Pakistan | (Yasmeen et al., 2010) [119] | Depression | Hospital | 100 | EPDS | Unclear | - | - | - | - | - | 41.0% | |
| Pakistan | (Waqas et al., 2015) [118] | Depression | Hospital | 500 | HADS | ≥11 | - | - | - | 31.8% | - | - | - |
| Pakistan | (Zahidie et al., 2011) [70] | Depression | Mixed | 375 | CES-D | ≥16 | - | - | - | 61.1% | - | - | - |
| Qatar | (Bener et al., 2012a)[52] | Depression | Hospital | 1379 | EPDS | >12 | - | - | - | - | - | 17.6% | - |
| Saudi Arabia | (Al-Modayfer et al., 2015) [121] | Depression | Hospital | 571 | EPDS | Unclear | - | - | - | - | 14.0% | - | - |
| Saudi Arabia | (Amr and Hussein Balaha, 2010) [72] | Depression | Hospital | 367 | MINI | N/A | - | - | - | - | - | - | 6.0% |
| Saudi Arabia | (Balaha et al., 2009) [83] | Depression | Hospital | 800 | MINI | N/A | - | - | - | - | - | - | 10.2% |
| Sudan | (Khalifa et al., 2015) [101] | Depression | Hospital | 238 | EPDS | ≥12 | - | - | - | - | - | 9.2% | - |
| 40 | MINI | N/A | - | - | - | - | - | 45%* | - | ||||
| Tunisia | (Masmoudi et al., 2008) [63] | Depression | Hospital | 213 | EPDS | >10 | - | - | - | - | 19.2% | 13.2% | - |
| UAE | (Abou-Saleh and Ghubash, 1997) [45] | Depression | Hospital | 95 | EPDS | >11 | - | - | - | - | 18.0% | - | - |
| 95 | SRQ | Unclear | - | - | - | - | 24.0% | - | - | ||||
| UAE | (Green et al., 2006) [54] | Depression | Hospital | T0 = 125 T1 = 86 T2 = 56 | EPDS | ≥13 | - | - | - | - | - | 22.0% (T1) | 12.5% (T2) |
| UAE | (Hamdan and Tamim, 2011) [56] | Depression | Hospital | 137 | MINI | N/A | - | - | - | - | - | 10.0% | - |
| EPDS | >10 | - | - | - | - | - | 85.6% | - | |||||
| Attribute Defined | Population N (%) | Outcome N (%) | Data Collection Time N (%) | Study Setting N (%) |
|---|---|---|---|---|
| Yes | 73 (100%) | 73 (100%) | 4 (5.5%) | 50 (68.4%) |
| No | - | - | 34 (46.6%) | 15 (20.5%) |
| Unclear | - | - | 35 (47.9%) | 8 (9.6%) |
| Risk Categories * | Number of Studies | Odds Ratio/Relative Risk ** | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Bahrain | Egypt | Jordan | Kuwait | Lebanon | Morocco | Oman | Pakistan | Qatar | Saudi Arabia | Tunisia | UAE | Low (95% CI) | Median | High (95% CI) | |
| Relational | 41 | 1 | 1 | 3 | 1 | 4 | 2 | 2 | 16 | 3 | 2 | 2 | 4 | 0.3 (0.1–0.7) | 7.06 | 13.83 (NA) |
| Psychological | 27 | 1 | 0 | 4 | 0 | 2 | 2 | 1 | 7 | 3 | 1 | 3 | 3 | 0.78 (NA) | 1.38 | 1.98 (NA) |
| Physiological and health | 15 | 0 | 1 | 1 | 0 | 1 | 2 | 0 | 6 | 0 | 1 | 0 | 3 | 2.68 (NA) | ||
| Occupational | 2 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 2.27 (NA) | 29.03 | 55.8 (NA) |
| Sociodemographic | 27 | 1 | 3 | 3 | 0 | 1 | 2 | 2 | 8 | 3 | 2 | 0 | 2 | 0.13 (NA) | 1.25 | 2.37 (NA) |
| Predictors of response to trauma | 16 | 0 | 2 | 0 | 0 | 1 | 2 | 0 | 7 | 0 | 2 | 0 | 2 | - | - | - |
| Lifestyle | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | - | - | - |
| Negative environmental exposures | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | - | - | - |
| Genetic | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | - | - | - |
| Neuroanatomical | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | - | - | - |
| Total | 128 | 3 | 7 | 11 | 1 | 10 | 10 | 6 | 44 | 9 | 8 | 5 | 14 | |||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Doraiswamy, S.; Jithesh, A.; Chaabane, S.; Abraham, A.; Chaabna, K.; Cheema, S. Perinatal Mental Illness in the Middle East and North Africa Region—A Systematic Overview. Int. J. Environ. Res. Public Health 2020, 17, 5487. https://doi.org/10.3390/ijerph17155487
Doraiswamy S, Jithesh A, Chaabane S, Abraham A, Chaabna K, Cheema S. Perinatal Mental Illness in the Middle East and North Africa Region—A Systematic Overview. International Journal of Environmental Research and Public Health. 2020; 17(15):5487. https://doi.org/10.3390/ijerph17155487
Chicago/Turabian StyleDoraiswamy, Sathyanarayanan, Anupama Jithesh, Sonia Chaabane, Amit Abraham, Karima Chaabna, and Sohaila Cheema. 2020. "Perinatal Mental Illness in the Middle East and North Africa Region—A Systematic Overview" International Journal of Environmental Research and Public Health 17, no. 15: 5487. https://doi.org/10.3390/ijerph17155487
APA StyleDoraiswamy, S., Jithesh, A., Chaabane, S., Abraham, A., Chaabna, K., & Cheema, S. (2020). Perinatal Mental Illness in the Middle East and North Africa Region—A Systematic Overview. International Journal of Environmental Research and Public Health, 17(15), 5487. https://doi.org/10.3390/ijerph17155487





