Interactions between the Physical and Social Environments with Adverse Pregnancy Events Related to Placental Disorders—A Scoping Review
Abstract
:1. Introduction
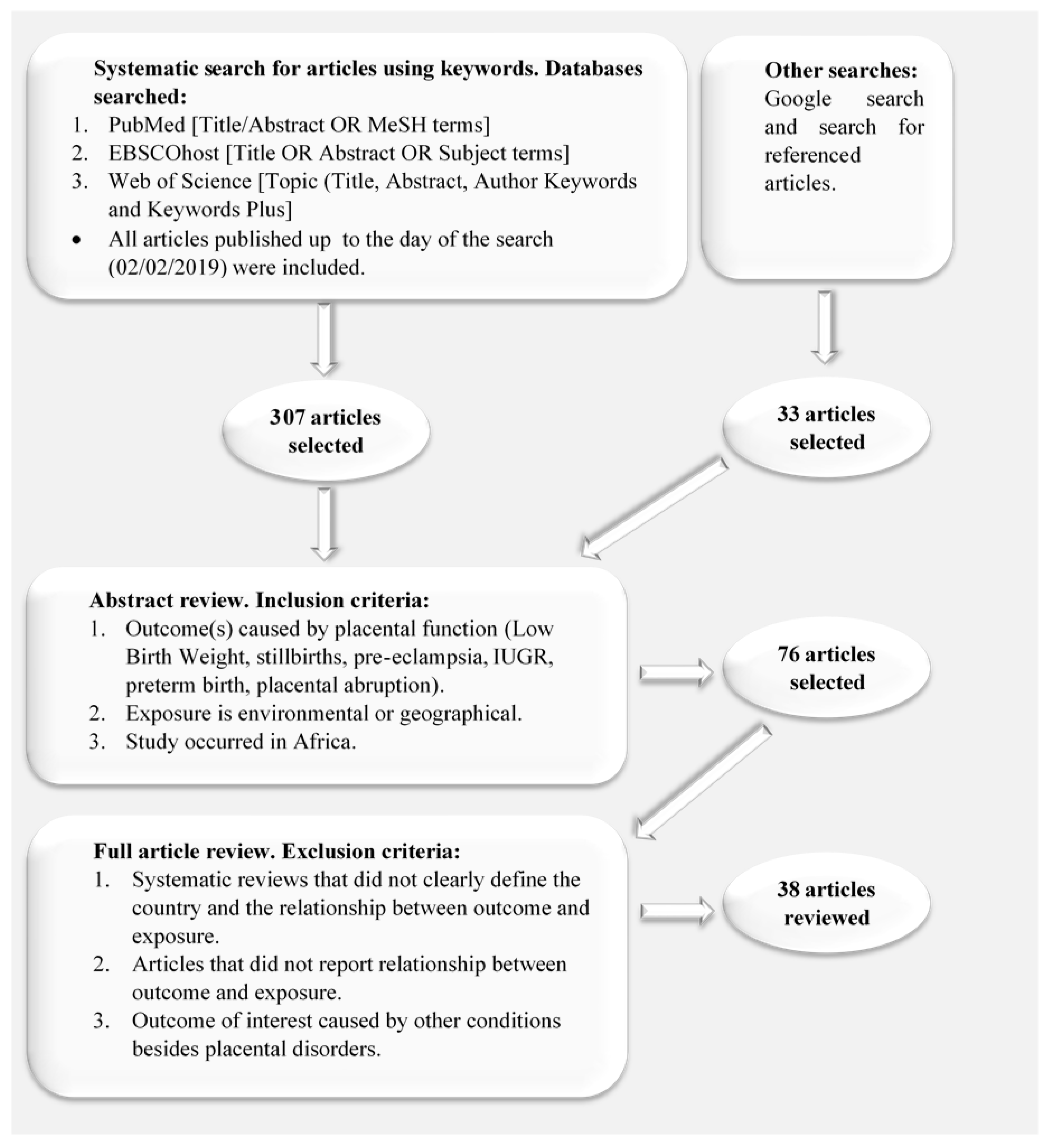
2. Materials and Methods
- Stage 1. Identifying the research question
- Stage 2. Identifying relevant studies
- Stage 3. Study selection
- Stage 4. Charting the data
- Stage 5. Collating, summarising and reporting the results.
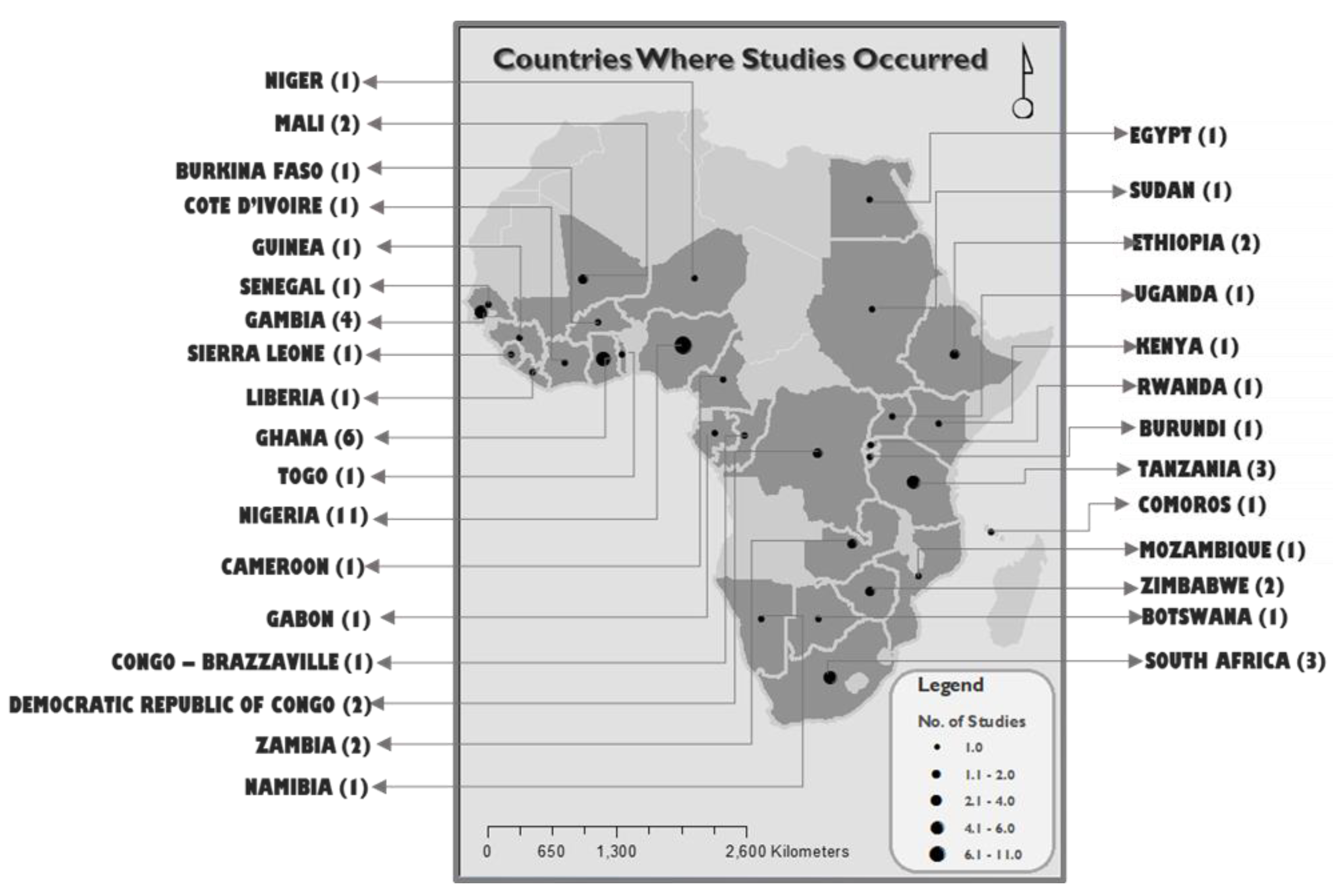
3. Results
3.1. Social and Demographic Factors (Table 2)
3.2. Physical Environmental Factors (Table 2)
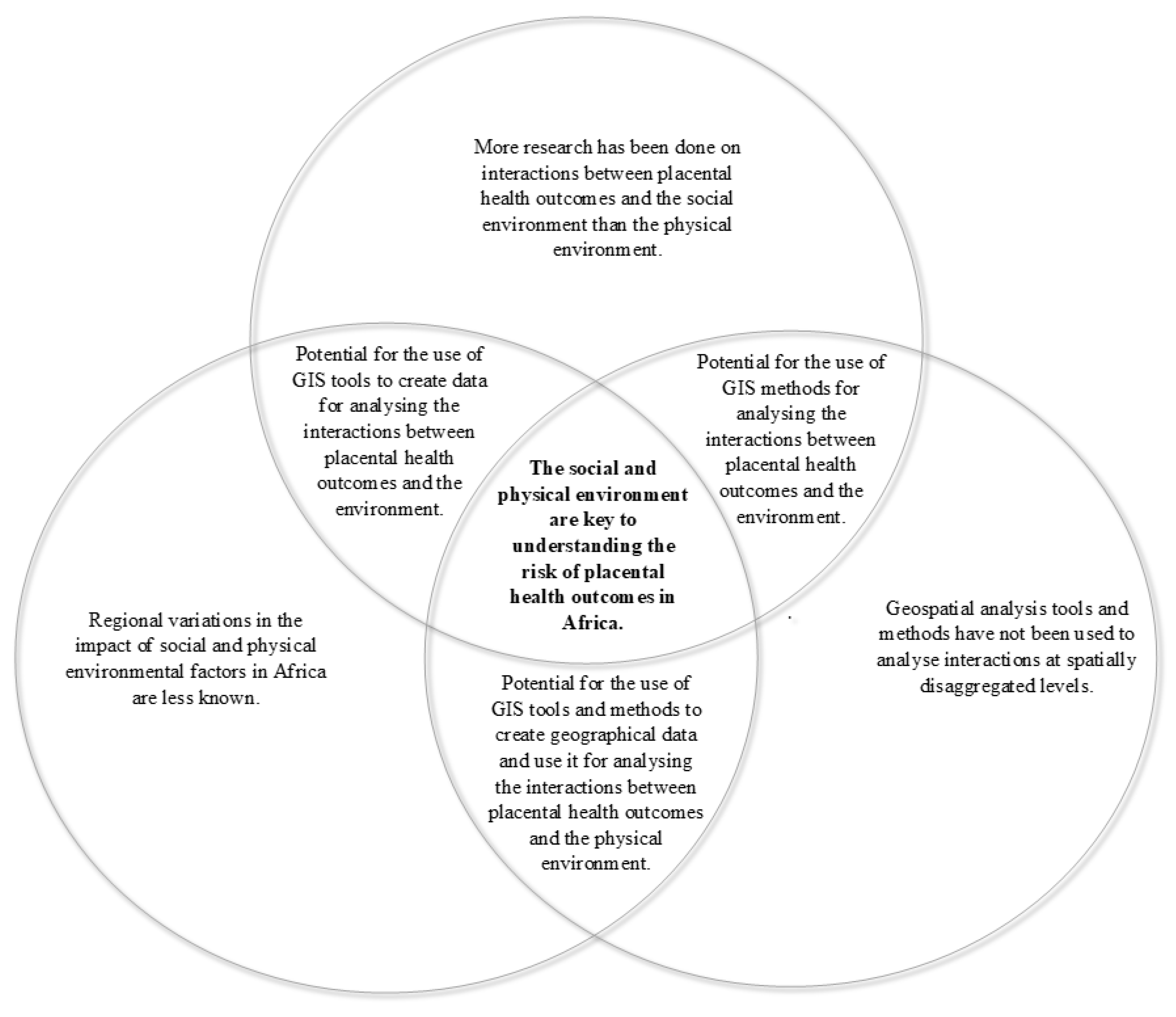
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Parker, S.E.; Werler, M.M. Epidemiology of ischemic placental disease: A focus on preterm gestations. Semin. Perinatol. 2014, 38, 133–138. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- WHO. WHO | Stillbirths. Available online: http://www.who.int/maternal_child_adolescent/epidemiology/stillbirth/en/ (accessed on 21 August 2019).
- WHO | Regional Office for Africa. Social and Economic Determinants of Health. Available online: https://www.afro.who.int/health-topics/social-and-economic-determinants-health (accessed on 21 August 2019).
- Cole, B.L.; Fielding, J.E. Health Impact Assessment: A Tool to Help Policy Makers Understand Health Beyond Health Care. Annu. Rev. Public Health 2007, 28, 393–412. [Google Scholar] [CrossRef]
- WHO. WHO | Social exclusion. Available online: http://www.who.int/social_determinants/themes/socialexclusion/en/ (accessed on 21 August 2019).
- WHO. WHO | Employment conditions. Available online: http://www.who.int/social_determinants/themes/employmentconditions/en/ (accessed on 21 August 2019).
- Omotoso, K.O.; Koch, S.F. Assessing changes in social determinants of health inequalities in South Africa: A decomposition analysis. Int. J. Equity Health 2018, 17, 181. [Google Scholar] [CrossRef] [PubMed]
- Ataguba, J.E.; Day, C.; McIntyre, D. Explaining the role of the social determinants of health on health inequality in South Africa. Glob. Health Action 2015, 8, 28865. [Google Scholar] [CrossRef] [PubMed]
- WHO. WHO | Action: SDH. Available online: https://www.who.int/social_determinants/actionsdh/en/ (accessed on 12 November 2019).
- WHO. WHO | Who We Are? Available online: http://www.who.int/social_determinants/about/en/ (accessed on 12 November 2019).
- Donkin, A.; Goldblatt, P.; Allen, J.; Nathanson, V.; Marmot, M. Global action on the social determinants of health. BMJ Glob. Health 2017, 3, e000603. [Google Scholar] [CrossRef] [Green Version]
- Munn, Z.; Peters, M.; Stern, C.; Tufanaru, C.; McArthur, A.; Aromataris, E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med. Res. Methodol. 2018, 18, 143. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef] [Green Version]
- Ugwa, E.A.; Ashimi, A. An assessment of stillbirths in a tertiary hospital in northern Nigeria. J. Matern. Neonatal Med. 2014, 28, 1585–1588. [Google Scholar] [CrossRef]
- Onyiriuka, A.N. Seasonal variations in birth weights and gender of infants born in a mission hospital in Benin City, Nigeria. Niger. Postgrad. Med. J. 2006, 13, 329–332. [Google Scholar]
- Adam, I.; Haggaz, A.D.; Mirghani, O.A.; Elhassan, E.M. Placenta Previa and Pre-Eclampsia: Analyses of 1645 Cases at Medani Maternity Hospital, Sudan. Front. Physiol. 2013, 4. [Google Scholar] [CrossRef] [Green Version]
- Dinglas, C.; Lardner, D.; Homchaudhari, A.; Kelly, C.; Briggs, C.; Passafaro, M.; Cho, E. Relationship of reported clinical features of pre-eclampsia and postpartum haemorrhage to demographic and other variables. West Afr. J. Med. 2011, 30, 84–88. [Google Scholar]
- Siza, J.E. Risk factors associated with low birth weight of neonates among pregnant women attending a referral hospital in northern Tanzania. Tanzan. J. Health Res. 2008, 10, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feresu, S.A.; Harlow, S.D.; Woelk, G.B. Risk factors for prematurity at Harare Maternity Hospital, Zimbabwe. Int. J. Epidemiol. 2004, 33, 1194–1201. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Owolabi, A.T.; Dare, F.O.; Fasubaa, O.B.; Ogunlola, I.O.; Kuti, O.; Bisiriyu, L.A. Risk factors for retained placenta in southwestern Nigeria. Singap. Med. J. 2008, 49, 532. [Google Scholar]
- Manyeh, A.K.; Amu, A.; Akpakli, D.E.; Williams, J.E.; Gyapong, M.; Gyapong, M. Socioeconomic and demographic factors associated with caesarean section delivery in Southern Ghana: Evidence from INDEPTH Network member site. BMC Pregnancy Childbirth 2018, 18, 405. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mbachu, I.I.; Achigbu, K.I.; Odinaka, K.K.; Eleje, G.U.; Osuagwu, I.K.; Osim, V.O. Tracking stillbirths by referral pattern and causes in a rural tertiary hospital in Southern Nigeria. Niger. Postgrad. Med. J. 2018, 25, 87. [Google Scholar] [CrossRef] [PubMed]
- Ubomba-Jaswa, P.; Ubomba-Jaswa, S.R. Correlates of low birth weight in Botswana. S. Afr. J. Demogr. 1996, 6, 64–73. [Google Scholar]
- Larbi, P.; Dedu, V.K.; Okyere, G.A. Determinants of low birth weight in the Lower Manya Krobo Municipality of the Eastern region of Ghana. Int. J. Reprod. Contracept. Obstet. Gynecol. 2018, 7, 4418–4425. [Google Scholar] [CrossRef]
- Tampah-Naah, A.M.; Anzagra, L.; Yendaw, E. Factors Correlate with Low Birth Weight in Ghana. Br. J. Med. Med. Res. 2016, 16, 1–8. [Google Scholar] [CrossRef]
- Agorinya, I.A.; Kanmiki, E.W.; Nonterah, E.A.; Tediosi, F.; Akazili, J.; Welaga, P.; Azongo, D.; Oduro, A.R. Socio-demographic determinants of low birth weight: Evidence from the Kassena-Nankana districts of the Upper East Region of Ghana. PLoS ONE 2018, 13, e0206207. [Google Scholar] [CrossRef] [Green Version]
- Alhassan, A.; Ayikai, L.A.; Alidu, H.; Yakong, V.N. Stillbirths and associated factors in a peri-urban District in Ghana. J. Med. Biomed. Sci. 2016, 5, 23–31. [Google Scholar] [CrossRef]
- Nayama, M.; Tamakloé-Azamesu, D.; Garba, M.; Idi, N.; Djibril, B.; Kamaye, M.; Marafa, A.; Toure, A.; Diallo, F.; Houfflin-Debarge, V. Hématome rétroplacentaire. Prise en charge dans une maternité de référence du Niger. Étude prospective à propos de 118 cas sur un an. Gynécologie Obs. Fertil. 2007, 35, 975–981. [Google Scholar] [CrossRef]
- Larysa, A.; Yao, T.; Richard, G.; Samuel, O.; John, F.D.J.; Quaye, I.K. Maternal Demographic and Placental Risk Factors in Term Low Birth Weight in Ghana. J. Pregnancy Child Health 2017, 4. [Google Scholar] [CrossRef] [Green Version]
- Shore, H.; Shunu, A.; Musa, A.; Assefa, N. Prevalence and Associated Factors with Low Birth Weight in Kersa District: Based on Data from Health and Demographic Surveillances System in 2014, Eastern Ethiopia. East. Afr. J. Health Biomed. Sci. 2018, 2, 36–44. [Google Scholar]
- Mgaya, A.; Massawe, S.N.; Kidanto, H.; Mgaya, H.N. Grand multiparity: Is it still a risk in pregnancy? BMC Pregnancy Childbirth 2013, 13, 241. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Igwegbe, A.O.; Eleje, G.U.; Okpala, B.C. Management outcomes of abruptio placentae at Nnamdi Azikiwe University Teaching Hospital, Nnewi, Nigeria. Niger. J. Med. 2013, 22, 234–238. [Google Scholar]
- Dohbit, J.S.; Foumane, P.; Tochie, J.N.; Mamoudou, F.; Temgoua, M.N.; Tankeu, R.; Aletum, V.; Mboudou, E. Maternal and neonatal outcomes of vaginal breech delivery for singleton term pregnancies in a carefully selected Cameroonian population: A cohort study. BMJ Open 2017, 7, e017198. [Google Scholar] [CrossRef]
- Nkwabong, E.; Nounemi, N.K.; Sando, Z.; Mbu, R.; Mbede, J. Risk factors and placental histopathological findings of term born low birth weight neonates. Placenta 2015, 36, 138–141. [Google Scholar] [CrossRef]
- Tégueté, I.; Maiga, A.W.; Leppert, P. Maternal and neonatal outcomes of grand multiparas over two decades in Mali. Acta Obstet. et Gynecol. Scand. 2012, 91, 580–586. [Google Scholar] [CrossRef]
- Ozumba, B.; Igwegbe, A. The challenge of grandmultiparity in Nigerian obstetric practice. Int. J. Gynecol. Obstet. 1992, 37, 259–264. [Google Scholar] [CrossRef]
- Luke, B. Nutrition and Multiple Gestation. Semin. Perinatol. 2005, 29, 349–354. [Google Scholar] [CrossRef]
- Eriksen, K.G.; Radford, E.J.; Silver, M.; Fulford, A.J.C.; Wegmüller, R.; Prentice, A.M. Influence of intergenerational in utero parental energy and nutrient restriction on offspring growth in rural Gambia. FASEB J. 2017, 31, 4928–4934. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Röllin, H.B.; Kootbodien, T.; Channa, K.; Odland, J. Øyvind Prenatal Exposure to Cadmium, Placental Permeability and Birth Outcomes in Coastal Populations of South Africa. PLoS ONE 2015, 10, e0142455. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oladeinde, H.B.; Oladeinde, O.B.; Omoregie, R.; Onifade, A.A. Prevalence and determinants of low birth weight: The situation in a traditional birth home in Benin City, Nigeria. Afr. Health Sci. 2016, 15, 1123–1129. [Google Scholar] [CrossRef]
- Omokanye, L.O.; Olatinwo, A.W.O.; Salaudeen, A.G.; Ajiboye, A.D.; Durowade, K.A. A 5-year review of pattern of placenta previa in Ilorin, Nigeria. Int. J. Health Sci. 2017, 11, 35–40. [Google Scholar]
- Mahe, A.; Perret, J.L.; Ly, F.; Fall, F.; Rault, J.; Dumont, A. The cosmetic use of skin-lightening products during pregnancy in Dakar, Senegal: A common and potentially hazardous practice. Trans. R. Soc. Trop. Med. Hyg. 2007, 101, 183–187. [Google Scholar] [CrossRef]
- Kahn, L.G.; Trasande, L. Environmental Toxicant Exposure and Hypertensive Disorders of Pregnancy: Recent Findings. Curr. Hypertens. Rep. 2018, 20, 87. [Google Scholar] [CrossRef]
- Dutta, A.; Khramtsova, G.; Brito, K.; Alexander, D.; Mueller, A.; Chinthala, S.; Adu, D.; Ibigbami, T.; Olamijulo, J.; Odetunde, A.; et al. Household air pollution and chronic hypoxia in the placenta of pregnant Nigerian women: A randomized controlled ethanol Cookstove intervention. Sci. Total Environ. 2018, 619, 212–220. [Google Scholar] [CrossRef]
- Dutta, A.; Brito, K.; Khramtsova, G.; Mueller, A.; Chinthala, S.; Alexander, D.; Adu, D.; Ibigbami, T.; Olamijulo, J.; Odetunde, A.; et al. Household air pollution and angiogenic factors in pregnant Nigerian women: A randomized controlled ethanol cookstove intervention. Sci. Total Environ. 2017, 599, 2175–2181. [Google Scholar] [CrossRef]
- Abubakari, A.; Jahn, A. Maternal Dietary Patterns and Practices and Birth Weight in Northern Ghana. PLoS ONE 2016, 11, e0162285. [Google Scholar] [CrossRef]
- Feresu, S.A.; Harlow, S.D.; Woelk, G.B. Risk Factors for Low Birthweight in Zimbabwean Women: A Secondary Data Analysis. PLoS ONE 2015, 10, e0129705. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Owili, P.; Muga, M.A.; Kuo, H.-W. Gender Difference in the Association between Environmental Tobacco Smoke and Birth Weight in Africa. Int. J. Environ. Res. Public Health 2018, 15, 1409. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Girma, S.; Fikadu, T.; Getahun, E.A.; Haftu, D.; Gedamu, G.; Dewana, Z.; Getachew, B. Factors associated with low birthweight among newborns delivered at public health facilities of Nekemte town, West Ethiopia: A case control study. BMC Pregnancy Childbirth 2019, 19, 220. [Google Scholar] [CrossRef] [Green Version]
- Hoque, M.; Hoque, E.; Kader, S.B. Pregnancy complications of grandmultiparity at a rural setting of South Africa. Iran. J. Reprod. Med. 2008, 6, 25–31. [Google Scholar]
- Hailu, L.D.; Kebede, D.L. Determinants of Low Birth Weight among Deliveries at a Referral Hospital in Northern Ethiopia. Bio. Med Res. Int. 2018, 2018. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stringer, E.M.; Vwalika, B.; Killam, W.P.; Giganti, M.J.; Mbewe, R.; Chi, B.H.; Chintu, N.; Rouse, D.; Goldenberg, R.L.; Stringer, J.S.A. Determinants of Stillbirth in Zambia. Obstet. Gynecol. 2011, 117, 1151–1159. [Google Scholar] [CrossRef] [PubMed]
- Ozumba, B.C. Abruptio Placentae at The University of Nigeria Teaching Hospital, Enugu: A 3-Year Study. Aust. N. Z. J. Obstet. Gynaecol. 1989, 29, 117–120. [Google Scholar] [CrossRef] [PubMed]
- Jammeh, A.; Sundby, J.; Vangen, S. Maternal and obstetric risk factors for low birth weight and preterm birth in rural Gambia: A hospital-based study of 1579 deliveries. Open J. Obstet. Gynecol. 2011, 1, 94–103. [Google Scholar] [CrossRef] [Green Version]
- Uji, A.B.; Abeshi, S.; Njoku, C.; Agan, T.U.; Ekabua, J. Obstetric outcomes of booked teenage pregnancies at University of Calabar Teaching Hospital, Nigeria. Adolesc. Health Med. Ther. 2012, 3, 105–109. [Google Scholar] [CrossRef] [Green Version]
- El-Baz, M.A.; El-Deeb, T.S.; El-Noweihi, A.M.; Mohany, K.M.; Shaaban, O.; Abbas, A.M. Environmental factors and apoptotic indices in patients with intrauterine growth retardation: A nested case-control study. Environ. Toxicol. Pharmacol. 2015, 39, 589–596. [Google Scholar] [CrossRef]
- Ceesay, S.M.; Prentice, A.M.; Cole, T.J.; Foord, F.; Poskitt, E.M.; Weaver, L.T.; Whitehead, R.G. Effects on birth weight and perinatal mortality of maternal dietary supplements in rural gambia: 5 year randomised controlled trial. BMJ 1997, 315, 786–790. [Google Scholar] [CrossRef] [PubMed]
- Tiruneh, F.N.; Chuang, K.-Y.; Chuang, Y.-C. Women’s autonomy and maternal healthcare service utilization in Ethiopia. BMC Health Serv. Res. 2017, 17, 718. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Makanga, P.T.; Schuurman, N.; Sacoor, C.; Boene, H.; Vilanculo, F.; Vidler, M.; Magee, L.A.; Von Dadelszen, P.; Sevene, E.; Munguambe, K.; et al. Seasonal variation in geographical access to maternal health services in regions of southern Mozambique. Int. J. Health Geogr. 2017, 16, 1–16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Makanga, P.T.; Sacoor, C.; Schuurman, N.; Lee, T.; Vilanculo, F.C.; Munguambe, K.; Boene, H.; Ukah, U.V.; Vidler, M.; Magee, L.A.; et al. Place-specific factors associated with adverse maternal and perinatal outcomes in Southern Mozambique: A retrospective cohort study. BMJ Open 2019, 9, e024042. [Google Scholar] [CrossRef] [Green Version]
- Seabrook, J.; Woods, N.; Clark, A.F.; De Vrijer, B.; Penava, D.; Gilliland, J.A. The association between alcohol outlet accessibility and adverse birth outcomes: A retrospective cohort study. J. Neonatal Perinat. Med. 2018, 11, 71–77. [Google Scholar] [CrossRef] [Green Version]
- Seabrook, J.A.; Smith, A.; Clark, A.F.; Gilliland, J. Geospatial analyses of adverse birth outcomes in Southwestern Ontario: Examining the impact of environmental factors. Environ. Res. 2019, 172, 18–26. [Google Scholar] [CrossRef]
| Theme | Keywords |
|---|---|
| Socio-economic or demographic exposures | Social factors, socio-cultural, socio-economic, education, maternal age, parity, antenatal care visits, location, wealth index, nutrition, diet, educational level, sex of baby, geographical location, ethnic background, cultural beliefs. |
| Physical/environmental exposures | Environmental risk factors, environment influences, environmental hazards, neighbourhood conditions, environmental characteristics, air pollution, pollution, environmental exposure, environmental disparities, contaminants, outdoor air pollution, household air pollution, |
| Outcomes | Low birth weight, pre-eclampsia, stillbirth, foetal growth restriction, placental abnormalities |
| Settings | All African countries were listed including Africa and Sub-Saharan Africa keywords |
| Stillbirth | IUGR | Pre-Eclampsia | Low Birth Weight | Placental Abruption | Preterm Birth | Notes | |
|---|---|---|---|---|---|---|---|
| Social Exposures | |||||||
| Education Level | 0 [23] 0 [26] 0 [21] 0 [46] | The preterm births were associated with complications caused by placental disorders, which are eclampsia, hypertension, placenta praevia, malaria during pregnancy. | |||||
| 1 [14] 2 [22] | 1 [16] | 1 [24] 2 [25] 1 [18] | 2 [47] | |||
| 2 [17] | 2 [48] 2 [49] | |||||
| Parity | 0 [31] | 0 [50] | 0 [25] 0 [31] 0 [39] 0 [51] | 0 [31] | The effect of parity changes with different types of stillbirths, which is macerated and recent stillbirths [52]. Compared to pauciparous women, more grand multiparas are of low socioeconomic status and less of them practice prenatal care utilisation [35]. | ||
| 1 [14] 1 [52] 1 [27] 1 [22] | 1 [16] 1 [53] | 1 [21] 1 [24] | 1 [28] 1 [32] 1 [35] 1 [24] | |||
| 1 [52] 1 [22] | 1 [16] | 1 [54] 1 [34] | 1 [54] | |||
| Booking Status | |||||||
| 1 [14] | ||||||
| Maternal Age | 0 [22] | 0 [25] 0 [46] 0 [51] | Authors speculate that higher education weakens the negative effect higher maternal age has on birth weight [26]. Young and advanced age had a negative effect compared to middle age | ||||
| 1 [14] 1 [52] | 1 [16] | 2 [26] 2 [48] 1 [39] 1 [40] 1 [49] | ||||
| 1 [14] 1 [27] | 1 [24] 1 [23] 1 [54] 1 [21] 1 [55] | 1 [54] 1 [47] | ||||
| Residence | In the Gambia, primary health care (PHC) villages have village health workers and resident traditional birth attendants because they have a population of more than 400 inhabitants [54]. | ||||||
| 1 [54] | 1 [54] | |||||
| |||||||
| Rural/Urban Residency | 0 [25] 0 [49] | ||||||
| 1 [30] 1 [46] 2 [48] | 1 [47] | |||||
| Wealth Index | 0 [25] 0 [49] | ||||||
| 2 [48] | ||||||
| 1 [30] | ||||||
| Maternal employment | The protective or risk effect of the woman being employed on placental health outcomes depends on the type of work the woman does, that is, whether it is labour-intensive employment or not. | ||||||
| 1 [56] | 1 [21] 2 [48] | 1 [47] | ||||
| 2 [27] | 1 [28] | |||||
| Maternal Season of Birth | Adjusting for offspring season of birth does not alter the magnitude of change in birth weight of offspring of women born in different birth seasons [38]. This could mean that the effects of a woman’s bad nutrition during their season of birth may affect her baby’s birthweight, despite the baby receiving good nutrition. | ||||||
| 1 [38] | ||||||
| Paternal Season of Birth | 0 [38] | ||||||
| Prenatal Care | 0 [25] 0 [51] | Physical access is not a problem in Botswana; hence, the rate of antenatal care seeking is good [23]. | |||||
| 2 [56] | 2 [24] 2 [23] 2 [46] | |||||
| 1 [46] | 1 [34] 1 [18] | 1 [47] | ||||
| Nutrition | 2 [47] | Cultural beliefs in Northern Ghana affect women’s weight gain as some beliefs state that if you gain weight, the baby will gain weight causing a difficult delivery or leading to a caesarean section birth [46]. Therefore, pregnant women may deprive themselves of food fearing a difficult delivery. There is a claim that a nutritious drink called “mahewu” (a traditional drink in Zimbabwe) has protective qualities if drunk during pregnancy [47]. Authors suggest that studies are needed to investigate whether nutrition affects the development of the placenta or the nutrition of the foetus [47]. | |||||
| |||||||
| 1 [49] | ||||||
| Marital Status | 0 [21] 0 [49] | Being a married teenager is protective against having a low birth weight (LBW) baby compared to being an unmarried teenager [23]. This effect is not as strong with older women. Married women get family support even from the extend family members [26]. Different socio-cultural practices relating to marriages could be contributing to different nature of relationship between birth weight and marital status in different regions of Ghana [26]. | |||||
| 2 [40] | 1 [28] | |||||
| 1 [23] 1 [29] 1 [26] 1 [18] | 1 [47] | |||||
| Type of Union | |||||||
| |||||||
| 2 [40] | ||||||
| Drinking and Smoking | 1 [24] | 0 [28] | 1 [47] | Authors found no association between smoking and placental abruption, which they explained as being the result of Nigerien women not having tendencies of smoking [28]. | |||
| Socioeconomic Status | 0 [46] | ||||||
| 2 [26] 2 [21] | ||||||
| Use of Skin Lightening Cream | 1 [42] | Placental weight of users of skin lightening cream is significantly lower [42]. | |||||
| Exposure to Heat or Sun | 1 [24] | Long exposure to the sun and fire during work increases risk of LBW [24]. | |||||
| Sex of Baby | 0 [54] 0 [51] 0 [49] | The geographical and ethnical differences between the northern [46] and southern [21] regions of Ghana may explain the observed differences in the relationships with LBW. | |||||
| |||||||
| 1 [23] 1 [26] 2 [21] 1 [46] 1 [48] | ||||||
| Season | Supplementation has a greater effect on improving the pregnant woman’s outcomes during the hunger season [57], reducing the odds of having a low birth weight child. | ||||||
| 1 [57] | ||||||
| Labour Work | 1 [30] | ||||||
| Unstable Income | 1 [29] | ||||||
| Unplanned Pregnancy | 1 [29] | ||||||
| Place of Delivery | The prevalence of LBW for deliveries attended by traditional birth attendants was lower than that in institutions [40]. | ||||||
| Season | |||||||
| 1 [28] | Increased incidence of placental abruption during the rainy season could be due to the intense field work the women are subjected to [28]. | |||||
| Ethnicity | 0 [26] 0 [49] | 0 [28] | The socio-cultural practices of the major ethnic groups in the study area of the upper eastern region of Ghana are not that different [26], which may have influenced the findings of no association between ethnicity and LBW. Authors recommend a further investigation of the variations of sex of the baby as risk factor of LBW in the northern and southern regions of Ghana [26]. | ||||
| Religion | 0 [26] 0 [49] | The assumption made by the authors, to explain the nonexistence of an association, is that it is considered taboo in Ghana for women to smoke, therefore the possibility of religion playing a role in reducing the habit of smoking by women is reduced, thus exhibiting no relationship with LBW incidence [26]. | |||||
| Environmental Exposures | |||||||
| Environment Tobacco Smoke | 1 [48] | The risk effect of exposure to environmental tobacco smoke (ETS) increases in male children [48]. | |||||
| Environmental toxicants | In the Democratic Republic of Congo (DRC) and South Africa, studies showed that increased exposure to heavy metals (lead, cadmium and chromium) increased the risk of having preeclampsia [43]. | ||||||
| 1 [56] | 1 [43] | |||||
| Kitchen location | |||||||
| 1 [48] | ||||||
| Household Air Pollution | |||||||
| Pollutant Cooking Fuel | 1 [48] | ||||||
| Diet (Vine and Root Vegetables) | 2 [39] | Authors asked the question, “Is it the low cadmium in soil or the inability of the vegetables to absorb it that give home grown vine and root vegetables a protective effect against adverse birth outcomes?” | |||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dube, Y.P.; Nyapwere, N.; Magee, L.A.; Vidler, M.; Moore, S.E.; Barratt, B.; Craik, R.; Dadelszen, P.v.; Makanga, P.T.; The PRECISE Network. Interactions between the Physical and Social Environments with Adverse Pregnancy Events Related to Placental Disorders—A Scoping Review. Int. J. Environ. Res. Public Health 2020, 17, 5421. https://doi.org/10.3390/ijerph17155421
Dube YP, Nyapwere N, Magee LA, Vidler M, Moore SE, Barratt B, Craik R, Dadelszen Pv, Makanga PT, The PRECISE Network. Interactions between the Physical and Social Environments with Adverse Pregnancy Events Related to Placental Disorders—A Scoping Review. International Journal of Environmental Research and Public Health. 2020; 17(15):5421. https://doi.org/10.3390/ijerph17155421
Chicago/Turabian StyleDube, Yolisa Prudence, Newton Nyapwere, Laura A. Magee, Marianne Vidler, Sophie E. Moore, Benjamin Barratt, Rachel Craik, Peter von Dadelszen, Prestige Tatenda Makanga, and The PRECISE Network. 2020. "Interactions between the Physical and Social Environments with Adverse Pregnancy Events Related to Placental Disorders—A Scoping Review" International Journal of Environmental Research and Public Health 17, no. 15: 5421. https://doi.org/10.3390/ijerph17155421
APA StyleDube, Y. P., Nyapwere, N., Magee, L. A., Vidler, M., Moore, S. E., Barratt, B., Craik, R., Dadelszen, P. v., Makanga, P. T., & The PRECISE Network. (2020). Interactions between the Physical and Social Environments with Adverse Pregnancy Events Related to Placental Disorders—A Scoping Review. International Journal of Environmental Research and Public Health, 17(15), 5421. https://doi.org/10.3390/ijerph17155421





