Diurnal Profiles of Locomotive and Household Activities Using an Accelerometer in Community-Dwelling Older Adults with Musculoskeletal Disorders: A Cross-Sectional Survey
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
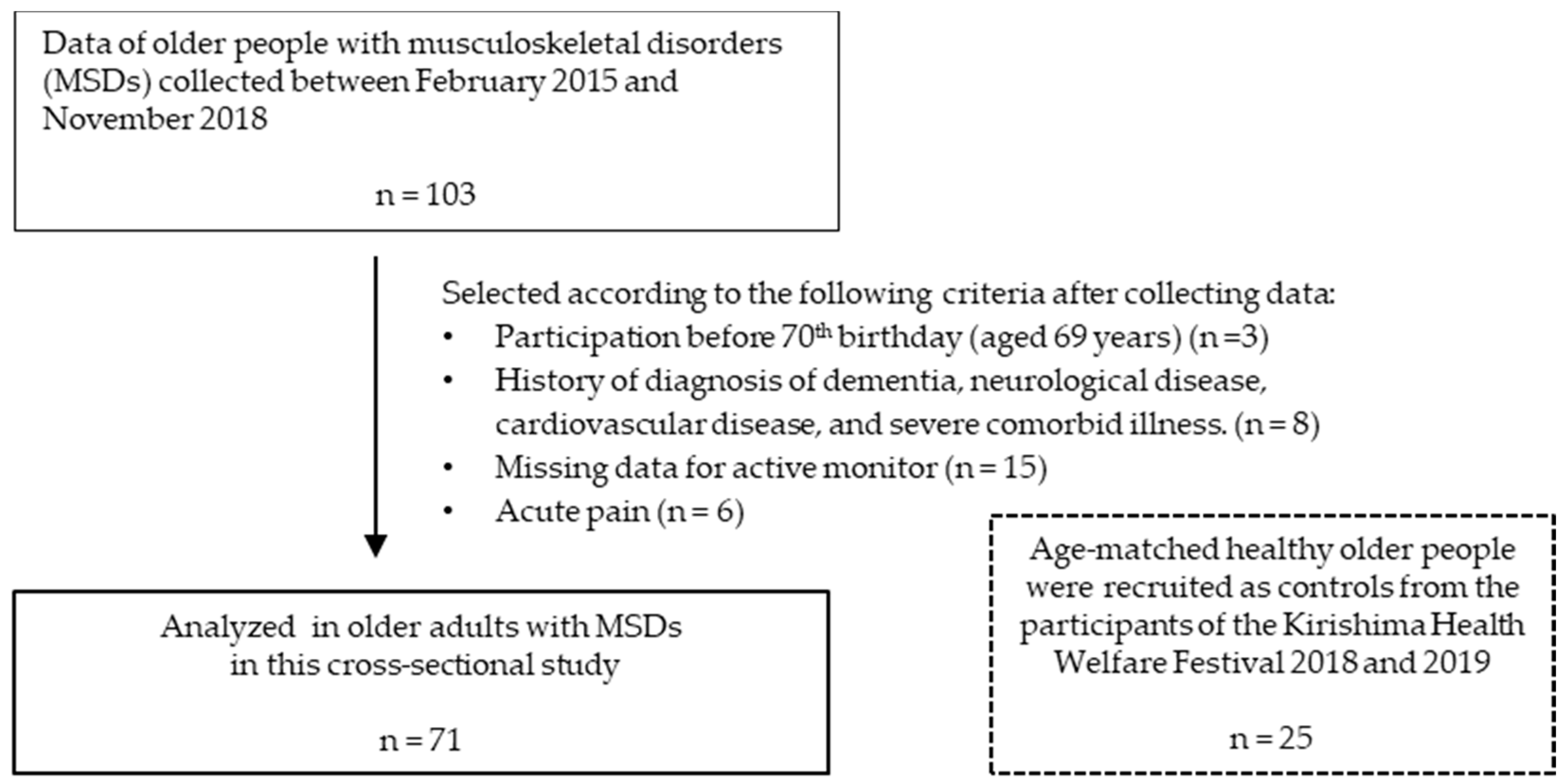
2.2. Participants
2.3. Data Collection and Assessment of Physical Functions
2.4. Assessment of Physical Activity
2.5. Data Analysis
3. Results
3.1. Participant Characteristics
3.2. Physical Activity and Diurnal Profiles Per Day
3.3. Chronic Pain Level and Physical Activity in Older Adults with MSDS
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Walsh, N.E.; Brooks, P.; Hazes, J.M.; Walsh, R.M.; Dreinhöfer, K.; Woolf, A.D.; Akesson, K.; Lidgren, L. Bone and Joint Decade Task Force for Standards of Care for Acute and Chronic Musculoskeletal Pain. Standards of care for acute and chronic musculoskeletal pain: The Bone and Joint Decade (2000–2010). Arch. Phys. Med. Rehabil. 2008, 89, 1830–1845. [Google Scholar] [CrossRef] [PubMed]
- Iijima, H.; Fukutani, N.; Isho, T.; Yamamoto, Y.; Hiraoka, M.; Miyanobu, K.; Jinnouchi, M.; Kaneda, E.; Aoyama, T.; Kuroki, H.; et al. Relationship between pedometer-based physical activity and physical function in patients with osteoarthritis of the knee: A cross-sectional study. Arch. Phys. Med. Rehabil. 2017, 98, 1382–1388. [Google Scholar] [CrossRef] [PubMed]
- Mansi, S.; Milosavljevic, S.; Baxter, G.D.; Tumilty, S.; Hendrick, P. A systematic review of studies using pedometers as an intervention for musculoskeletal diseases. BMC Musculoskelet. Disord. 2014, 15, 231. [Google Scholar] [CrossRef] [PubMed]
- Tudor-Locke, C.; Craig, C.L.; Aoyagi, Y.; Bell, R.C.; Croteau, K.A.; De Bourdeaudhuij, I.; Ewald, B.; Gardner, A.W.; Hatano, Y.; Lutes, L.D.; et al. How many steps/day are enough? For older adults and special populations. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 80. [Google Scholar] [CrossRef]
- Sartini, C.; Wannamethee, S.G.; Iliffe, S.; Morris, R.W.; Ash, S.; Lennon, L.; Whincup, P.H.; Jefferis, B.J. Diurnal patterns of objectively measured physical activity and sedentary behaviour in older men. BMC Public Health 2015, 15, 609. [Google Scholar] [CrossRef]
- Mai, A.; Bloch, A.; Klaaßen-Mielke, R.; Platen, P.; Hinrichs, T. Diurnal profiles of pedometer-determined physical activity in chronically ill and mobility-limited older adults: A cross-sectional study. BMC Public Health 2014, 14, 1268. [Google Scholar] [CrossRef][Green Version]
- Park, J.; Ishikawa-Takata, K.; Tanaka, S.; Mekata, Y.; Tabata, I. Effects of Walking speed and step frequency on estimation of physical activity using accelerometers. J. Physiol. Anthropol. 2011, 30, 119–127. [Google Scholar] [CrossRef][Green Version]
- Trost, S.G.; McIver, K.L.; Pate, R.R. Conducting accelerometer-based activity assessments in field-based research. Med. Sci. Sports Exerc. 2005, 37, 531–543. [Google Scholar] [CrossRef]
- Ohkawara, K.; Oshima, Y.; Hikihara, Y.; Ishikawa-Takata, K.; Tabata, I.; Tanaka, S. Real-time estimation of daily physical activity intensity by a triaxial accelerometer and a gravity-removal classification algorithm. Br. J. Nutr. 2011, 105, 1681–1691. [Google Scholar] [CrossRef]
- Chen, K.Y.; Bassett, D.R., Jr. The technology of accelerometry-based activity monitors: Current and future. Med. Sci. Sports Exerc. 2005, 37, 490–500. [Google Scholar] [CrossRef]
- Nakanishi, M.; Izumi, S.; Nagayoshi, S.; Kawaguchi, H.; Yoshimoto, M.; Shiga, T.; Ando, T.; Nakae, S.; Usui, C.; Aoyama, T.; et al. Estimating metabolic equivalents for activities in daily life using acceleration and heart rate in wearable devices. Biomed. Eng. Online 2018, 17, 100. [Google Scholar] [CrossRef] [PubMed]
- Oshima, Y.; Kawaguchi, K.; Tanaka, S.; Ohkawara, K.; Hikihara, Y.; Ishikawa-Takata, K.; Tabata, I. Classifying household and locomotive activities using a triaxial accelerometer. Gait Posture 2010, 31, 370–374. [Google Scholar] [CrossRef] [PubMed]
- Park, H.; Park, W.; Lee, M.; Ko, N.; Kim, E.; Ishikawa-Takata, K.; Park, J. The association of locomotive and non-locomotive physical activity measured by an accelerometer with functional fitness in healthy elderly men: A pilot study. J. Exerc. Nutr. Biochem. 2018, 22, 41–48. [Google Scholar] [CrossRef]
- Akihiro, S.; Taira, Y.; Maeda, K.; Natsume, K.; Sakakima, H. Feasibility and effectiveness of home-based exercise programs on physical performance and health-related quality of life of the older people dwelling on an isolated, doctor-less island. Geriatr. Gerontol. Int. 2018, 18, 1313–1317. [Google Scholar] [CrossRef] [PubMed]
- Davis, M.G.; Fox, K.R. Physical activity patterns assessed by accelerometry in older people. Eur. J. Appl. Physiol. 2007, 100, 581–589. [Google Scholar] [CrossRef] [PubMed]
- de Melo, L.L.; Menec, V.H.; Ready, A.E. Relationship of functional fitness with daily steps in community-dwelling older adults. J. Geriatr. Phys. Ther. 2014, 37, 116–120. [Google Scholar] [CrossRef]
- Yamamoto, N.; Miyazaki, H.; Shimada, M.; Nakagawa, N.; Sawada, S.S.; Nishimuta, M.; Kimura, Y.; Kawakami, R.; Nagayama, H.; Asai, H.; et al. Daily step count and all-cause mortality in a sample of Japanese elderly people: A cohort study. BMC Public Health 2018, 18, 540. [Google Scholar] [CrossRef]
- Tudor-Locke, C.; Craig, C.L.; Thyfault, J.P.; Spence, J.C. A step-defined sedentary lifestyle index: <5000 steps/day. Appl. Physiol. Nutr. Metab. 2013, 38, 100–114. [Google Scholar]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in older adults: Evidence for a phenotype. J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, 146–156. [Google Scholar] [CrossRef]
- Nakai, Y.; Makizako, H.; Kiyama, R.; Tomioka, K.; Taniguchi, Y.; Kubozono, T.; Takenaka, T.; Ohishi, M. Association between chronic pain and physical frailty in community-dwelling older adults. Int. J. Environ. Res. Public Health 2019, 16, 1330. [Google Scholar] [CrossRef]
- Liberman, O.; Freud, T.; Peleg, R.; Keren, A.; Press, Y. Chronic pPain and geriatric syndromes in community-dwelling patients aged ≥65 years. J. Pain Res. 2018, 11, 1171–1180. [Google Scholar] [CrossRef] [PubMed]
- Dobson, F.; Hinman, R.S.; Roos, E.M.; Abbott, J.H.; Stratford, P.; Davis, A.M.; Buchbinder, R.; Snyder-Mackler, L.; Henrotin, Y.; Thumboo, J.; et al. OARSI recommended performance-based tests to assess physical function in people diagnosed with hip or knee osteoarthritis. Osteoarthr. Cartil. 2013, 21, 1042–1052. [Google Scholar] [CrossRef] [PubMed]
- Mizumoto, A.; Ihira, H.; Makino, K.; Saitoh, S.; Ohnishi, H.; Furuna, T. Physical activity changes in the winter in older persons living in northern Japan: A prospective study. BMC Geriatr. 2015, 15, 43. [Google Scholar] [CrossRef] [PubMed]
- Rapp, K.; Klenk, J.; Benzinger, P.; Franke, S.; Denkinger, M.D.; Peter, R.; ActiFE Ulm Study Group. Physical performance and daily walking duration: Associations in 1271 women and men aged 65–90 years. Aging Clin. Exp. Res. 2012, 24, 455–460. [Google Scholar] [PubMed]
- Johansson, J.; Nordström, A.; Nordström, P. Objectively measured physical activity is associated with parameters of bone in 70-year-old men and women. Bone 2015, 81, 72–79. [Google Scholar] [CrossRef]
- Tawashy, A.E.; Eng, J.J.; Krassioukov, A.V.; Warburton, D.E.; Ashe, M.C.; Hung, C. Physical activity is related to lower levels of pain, fatigue and depression in individuals with spinal-cord injury: A correlational study. Spinal Cord. 2009, 47, 301–306. [Google Scholar] [CrossRef]
- Høidrup, S.; Sørensen, T.I.; Strøger, U.; Lauritzen, J.B.; Schroll, M.; Grønbaek, M. Leisure-time physical activity levels and changes in relation to risk of hip fracture in men and women. Am. J. Epidemiol. 2001, 154, 60–68. [Google Scholar] [CrossRef]
- Sumizono, M.; Sakakima, H.; Otsuka, S.; Terashi, T.; Nakanishi, K.; Ueda, K.; Takada, S.; Kikuchi, K. The effect of exercise frequency on neuropathic pain and pain-related cellular reactions in the spinal cord and midbrain in a rat sciatic nerve injury model. J. Pain Res. 2018, 11, 281–291. [Google Scholar] [CrossRef]
- Cyarto, E.V.; Myers, A.; Tudor-Locke, C. Pedometer accuracy in nursing home and community-dwelling older adults. Med. Sci. Sports Exerc. 2004, 36, 205–209. [Google Scholar] [CrossRef]
- Dworkin, R.H.; O’Connor, A.B.; Backonja, M.; Farrar, J.T.; Finnerup, N.B.; Jensen, T.S.; Kalso, E.A.; Loeser, J.D.; Miaskowski, C.; Nurmikko, T.J.; et al. Pharmacologic Management of Neuropathic Pain: Evidence-Based Recommendations. Pain 2007, 132, 237–251. [Google Scholar] [CrossRef]
- Hamilton, S.L.; Clemes, S.A.; Griffiths, P.L. UK adults exhibit higher step counts in summer compared to winter months. Ann. Hum. Biol. 2008, 35, 154–169. [Google Scholar] [CrossRef] [PubMed]


| Older Adults with MSDs (n = 71) | Control Older Adults (n = 25) | p-Value | |
|---|---|---|---|
| Age (years) | 81.1 ± 5.0 | 79.5 ± 3.5 | 0.072 |
| Men/women (n) | 15/56 | 10/15 | 0.064 |
| Body mass index (kg/m2) | 23.7 ± 3.3 | 22.5 ± 2.6 | 0.097 |
| Diagnosis of orthopedic disease for rehabilitation * (n) | |||
| Osteoarthritis of the knee | 31 | ― | |
| Chronic low back pain | 17 | ― | |
| Lumbar spondylosis | 17 | ― | |
| Lumbar spinal stenosis | 10 | ― | |
| Conservative therapy after fracture (e.g., lumbar vertebrae, patella) | 2 | ― | |
| After surgery of the lower limbs (e.g., TKA, THA, osteosynthesis) | 9 | ― | |
| After surgery of lumbar or cervical spine (e.g., PLF, depression, lumber disc herniation) | 6 | ― | |
| Chronic pain (NRS) (n) | <0.001 | ||
| None (0) | 0 | 25 | |
| Mild (1–3) | 20 | 0 | |
| Moderate (4–6) | 38 | 0 | |
| Severe (7–10) | 13 | 0 |
| Older Adults with MSDs (n = 71) | Control Older Adults (n = 25) | p-Value | |
|---|---|---|---|
| Physical functions | |||
| Timed Up and Go test (second) | 12.7 ± 4.5 | 6.6 ± 1.0 | <0.001 |
| CS-30 test (repetitions) | 11.8 ± 3.9 | 17.5 ± 5.2 | <0.001 |
| Steps parameters (steps) | |||
| Steps per day | 2563.8 ±2063.7 | 5137.6 ± 2844.2 | <0.001 |
| Steps per hour | 150.9 ± 121.3 | 302.2 ± 167.3 | <0.001 |
| Physical activities (MET-h/week) * | |||
| Locomotive activity | 2.3 ± 3.1 | 11.5 ± 10.9 | <0.001 |
| Household activity | 15.8 ± 8.9 | 15.1 ± 5.5 | 0.667 |
| Steps Per Day (Steps) | Locomotive Activity (MET-h/Week) | Household Activity (MET-h/Week) | |
|---|---|---|---|
| Chronic pain (n = 71) | |||
| Mild (n = 20) | 2987.2 ± 2152.6 | 3.7 ± 4.7 | 17.9 ± 9.0 |
| Moderate (n = 38) | 2717.5 ± 2150.4 | 2.1 ± 2.3 | 16.5 ± 9.2 |
| Severe (n = 13) | 1490.1 ± 1268.7 | 0.8 ± 0.8 | 12.5 ± 7.5 |
| p-value (Mild vs. Severe) | 0.032 | 0.065 | 0.147 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sakakima, H.; Takada, S.; Norimatsu, K.; Otsuka, S.; Nakanishi, K.; Tani, A. Diurnal Profiles of Locomotive and Household Activities Using an Accelerometer in Community-Dwelling Older Adults with Musculoskeletal Disorders: A Cross-Sectional Survey. Int. J. Environ. Res. Public Health 2020, 17, 5337. https://doi.org/10.3390/ijerph17155337
Sakakima H, Takada S, Norimatsu K, Otsuka S, Nakanishi K, Tani A. Diurnal Profiles of Locomotive and Household Activities Using an Accelerometer in Community-Dwelling Older Adults with Musculoskeletal Disorders: A Cross-Sectional Survey. International Journal of Environmental Research and Public Health. 2020; 17(15):5337. https://doi.org/10.3390/ijerph17155337
Chicago/Turabian StyleSakakima, Harutoshi, Seiya Takada, Kosuke Norimatsu, Shotaro Otsuka, Kazuki Nakanishi, and Akira Tani. 2020. "Diurnal Profiles of Locomotive and Household Activities Using an Accelerometer in Community-Dwelling Older Adults with Musculoskeletal Disorders: A Cross-Sectional Survey" International Journal of Environmental Research and Public Health 17, no. 15: 5337. https://doi.org/10.3390/ijerph17155337
APA StyleSakakima, H., Takada, S., Norimatsu, K., Otsuka, S., Nakanishi, K., & Tani, A. (2020). Diurnal Profiles of Locomotive and Household Activities Using an Accelerometer in Community-Dwelling Older Adults with Musculoskeletal Disorders: A Cross-Sectional Survey. International Journal of Environmental Research and Public Health, 17(15), 5337. https://doi.org/10.3390/ijerph17155337





