Promoting Evidence-Based Practice for Improved Occupational Safety and Health at Workplaces in Sweden. Report on a Practice-Based Research Network Approach
Abstract
1. Introduction
1.1. Research into Practice—Translation and Dissemination
1.2. The Importance of a Practice-Based Research Network in Occupational Safety and Health
1.3. Occupational Health Services
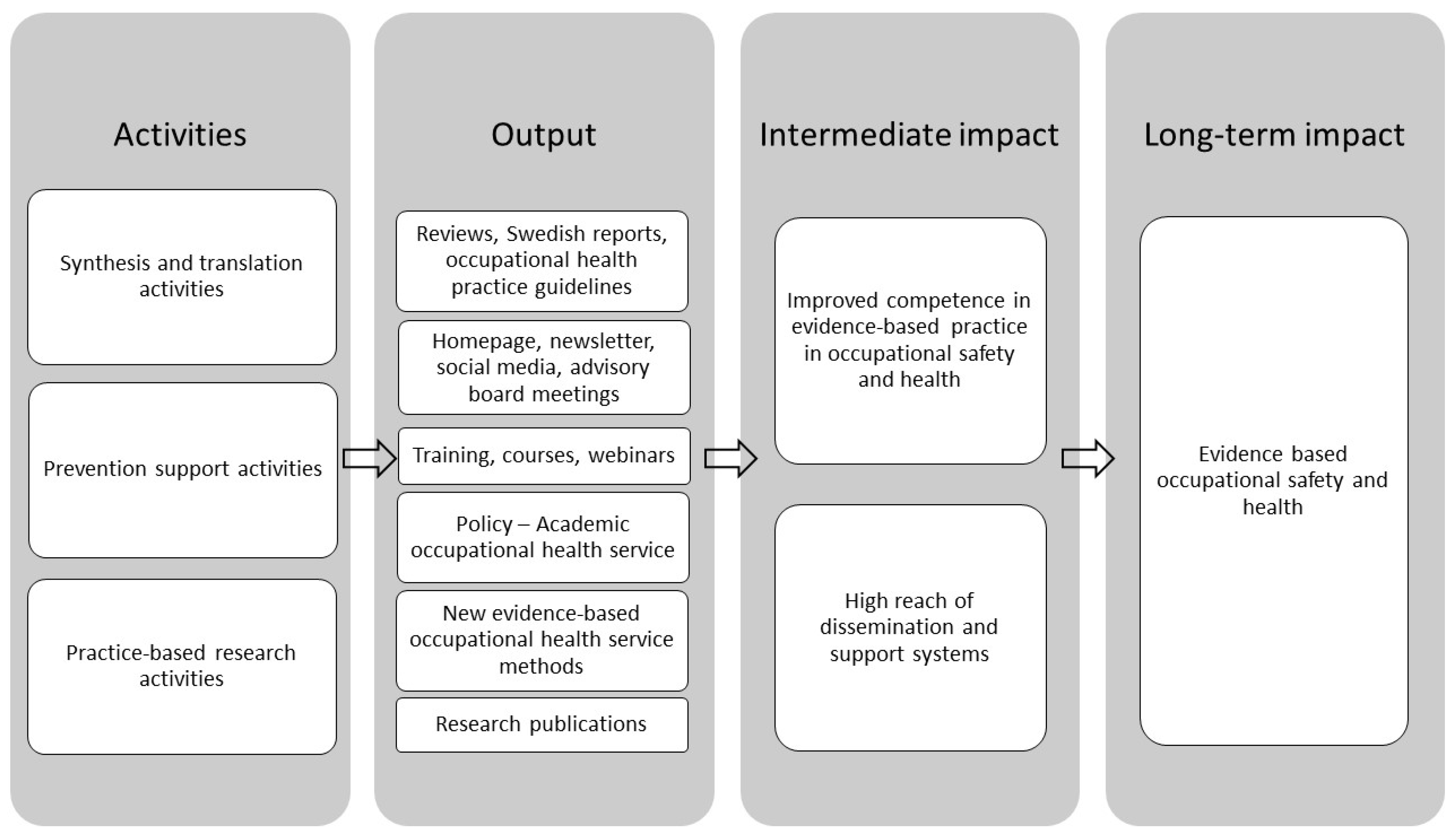
2. The PBRN-OSH Program
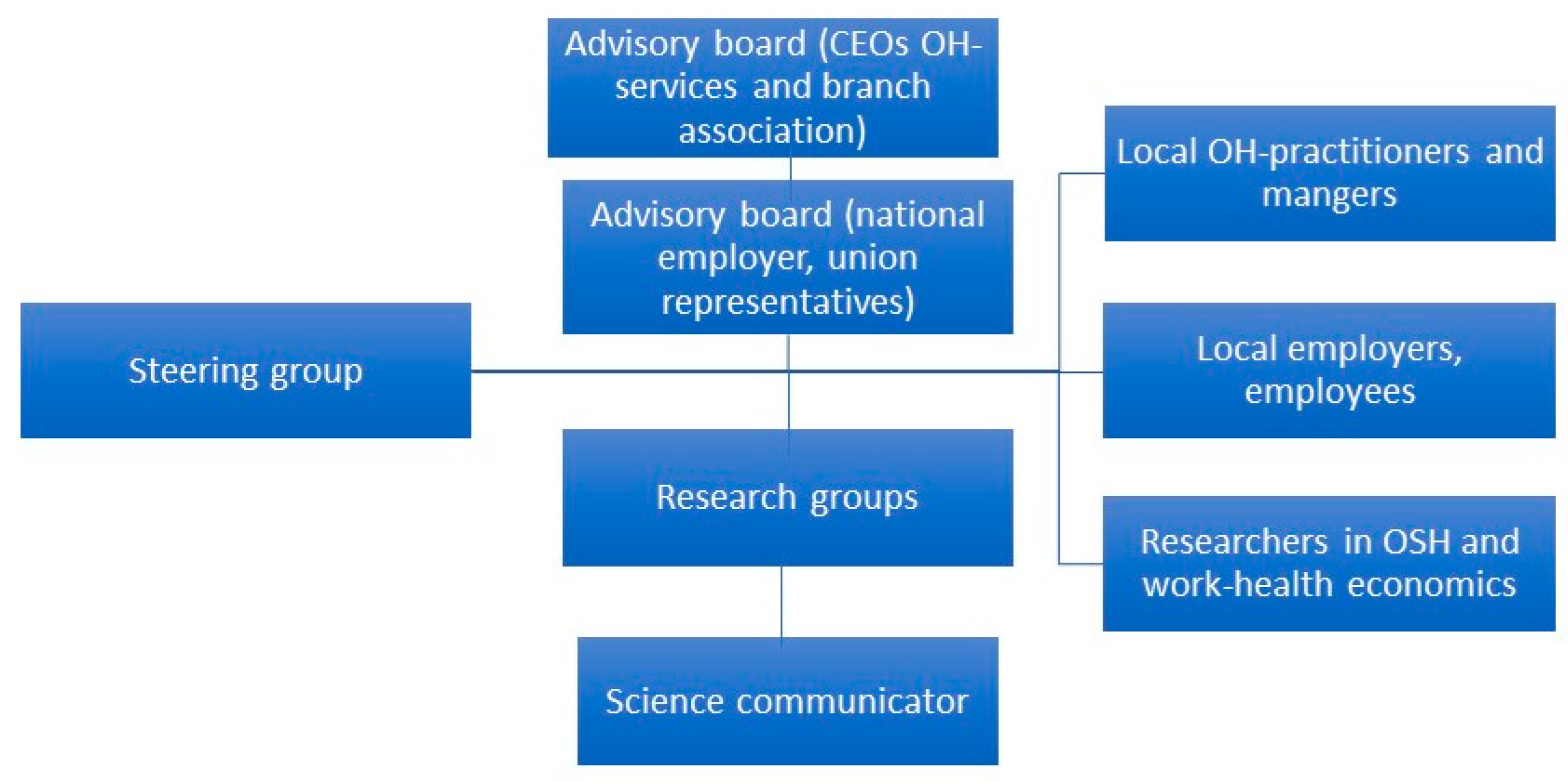
2.1. The Partners in the PBRN-OSH Program
2.2. The Structure of the PBRN-OSH Program
2.2.1. Prevention Synthesis and Translation System
2.2.2. Prevention Support System
2.3. Practice-Based Research Studies
3. Impact of the PBRN-OSH-Program
3.1. Improved Competence in Evidence-Based Practice in OH-Services
3.2. Accreditation in EBP for OH-Services
3.3. National Guidelines for OH-Services
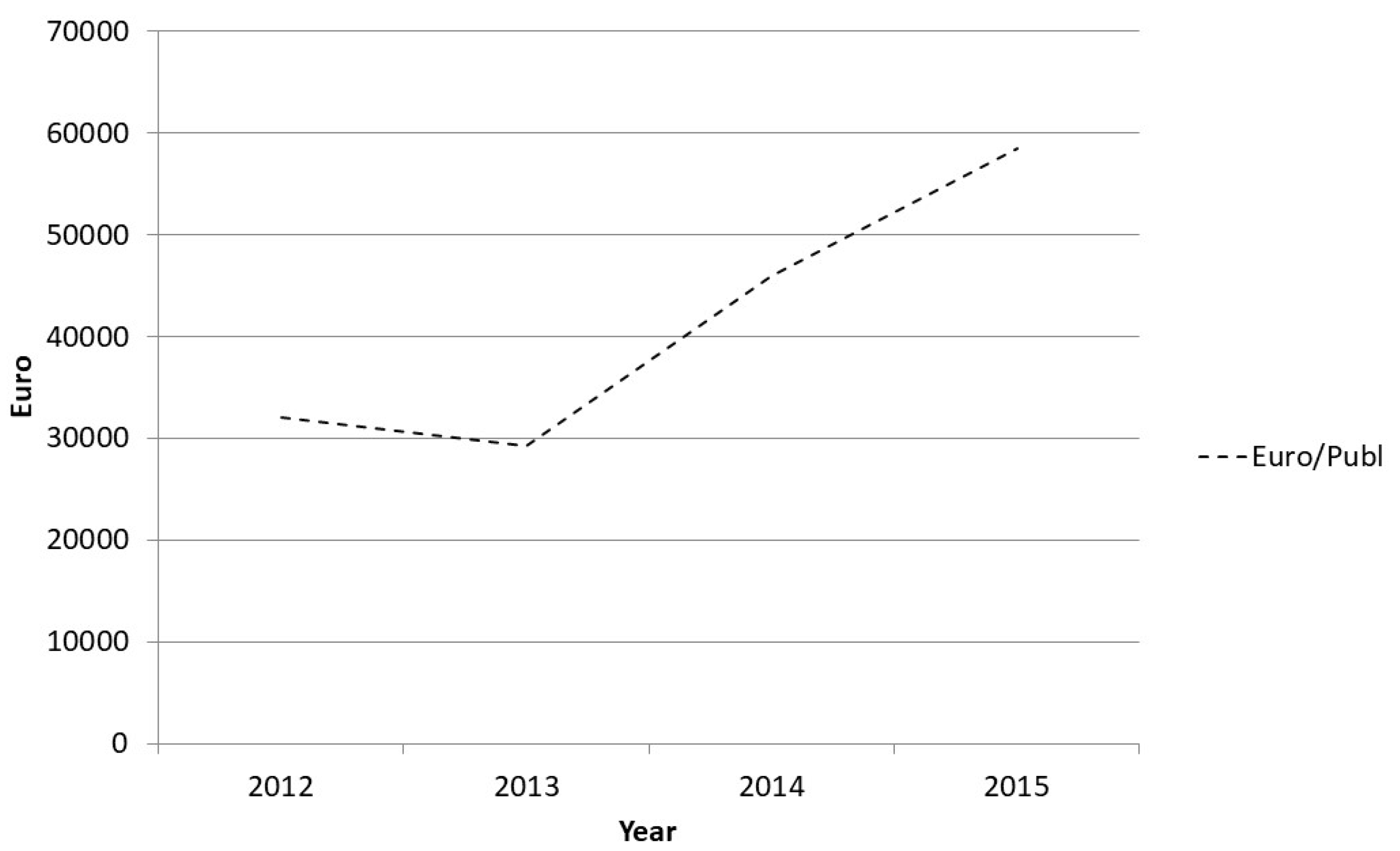
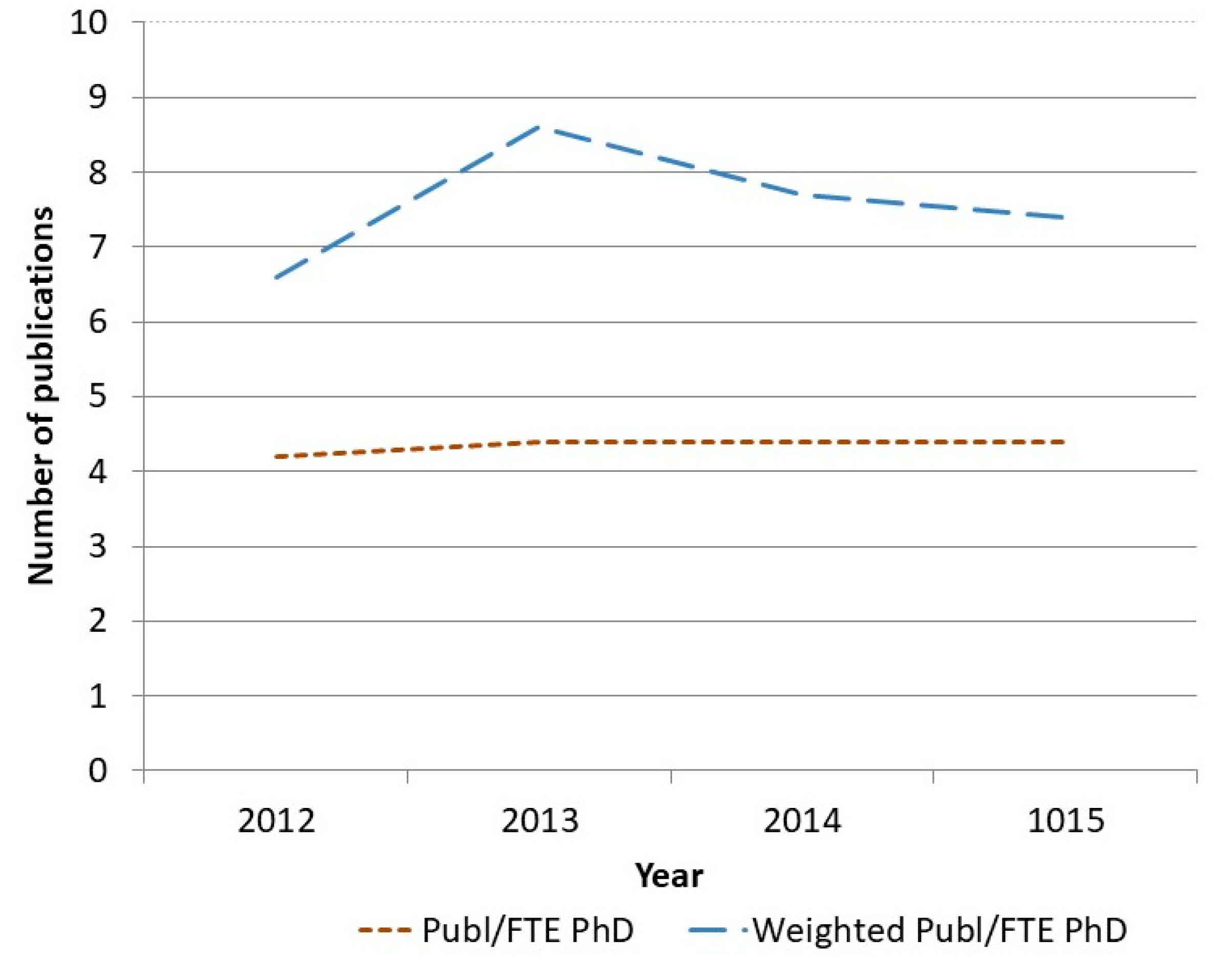
3.4. Increasing Evidence
4. Discussion and Lessons Learned
5. Conclusions
Recommendation for Improving Utilisation of Research into Practice
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Hollander, H.; Es-Sadki, N.; Merkelbach, I. European Innovation Scoreboard 2019. Available online: https://ec.europa.eu/growth/industry/policy/innovation/scoreboards_en (accessed on 14 May 2020).
- Balas, E.A.; Boren, S.A. Yearbook of Medical Informatics; Schattauer Verlagsgesellschaft: Stuttgart, Germany, 2000; Managing Clinical Knowledge for Health Care Improvement. [Google Scholar]
- Westfall, J.M.; Mold, J.; Fagnan, L. Practice-based research–“Blue Highways” on the NIH roadmap. JAMA J. Am. Med. Assoc. 2007, 297, 403–406. [Google Scholar] [CrossRef] [PubMed]
- Green, L.A.; Seifert, C.M. Translation of research into practice: Why we can′t “just do it”. J. Am. Board Fam. Pract. 2005, 18, 541–545. [Google Scholar] [CrossRef] [PubMed]
- Minkler, M.; Salvatore, A.L. Participatory Approaches for Study Design and Analysis in Dissemination and Implementation Research; Oxford Scholarship Online: Oxford, UK, 2012. [Google Scholar] [CrossRef]
- Powell, B.J.; Waltz, T.J.; Chinman, M.J.; Damschroder, L.J.; Smith, J.L.; Matthieu, M.M.; Proctor, E.K.; Kirchner, J.E. A refined compilation of implementation strategies: Results from the Expert Recommendations for Implementing Change (ERIC) project. Implement. Sci. 2015, 10, 21. [Google Scholar] [CrossRef] [PubMed]
- EU-OSHA. Priorities for Occupational Safety and Health Research in Europe for the Years 2013–2020; European Agency for Safety and Health at Work: Luxembourg; Publications Office of the European Union: Brussels, Belgium, 2014. [Google Scholar]
- Bumbarger, B.K.; Campbell, E.M. A state agency-university partnership for translational research and the dissemination of evidence-based prevention and intervention. Adm. Policy Ment. Health 2012, 39, 268–277. [Google Scholar] [CrossRef] [PubMed]
- Carpenter, W.R.; Meyer, A.M.; Wu, Y.; Qaqish, B.; Sanoff, H.K.; Goldberg, R.M.; Weiner, B.J. Translating research into practice: The role of provider-based research networks in the diffusion of an evidence-based colon cancer treatment innovation. Med. Care 2012, 50, 737–748. [Google Scholar] [CrossRef] [PubMed]
- FORTE. User Participation. Reserach with and about User Participation; FORTE: Stockholm, Sweden, 2015. [Google Scholar]
- Brett, J.; Staniszewska, S.; Mockford, C.; Herron-Marx, S.; Hughes, J.; Tysall, C.; Suleman, R. Mapping the impact of patient and public involvement on health and social care research: A systematic review. Health Expect. 2014, 17, 637–650. [Google Scholar] [CrossRef] [PubMed]
- Swedish Work Environment Authority. The Work Environment Act. Available online: https://www.government.se/4ac754/contentassets/86e9091526644e90b78d2ff937318530/sfs-19771160-work-environment-act (accessed on 10 May 2020).
- Swedish Association of Occupational Health and Safety. Available online: https://www.foretagshalsor.se/ (accessed on 21 July 2006).
- AFA Insurance. Available online: https://www.afaforsakring.se/andra-sprak/engelska/ (accessed on 4 June 2006).
- FORTE. Available online: www.forte.se/en (accessed on 4 June 2020).
- Wandersman, A.; Duffy, J.; Flaspohler, P.; Noonan, R.; Lubell, K.; Stillman, L.; Blachman, M.; Dunville, R.; Saul, J. Bridging the gap between prevention research and practice: The interactive systems framework for dissemination and implementation. Am. J. Commun. Psychol. 2008, 41, 171–181. [Google Scholar] [CrossRef] [PubMed]
- Kwak, L.; Wahlin, C.; Stigmar, K.; Jensen, I. Developing a practice guideline for the occupational health services by using a community of practice approach: A process evaluation of the development process. BMC Public Health 2017, 17, 89. [Google Scholar] [CrossRef] [PubMed]
- Jensen, I.; Kwak, L. Intervention and Implementation Research within Occupational Health. Development and Evaluation of Cost-Effective Measures for Improved OSH. Report from the PBRN-OSH Programme; Unit of Intervention and Implementation Research on Worker Health, Department of Environmental Medicin, Karolinska Institutet: Stockholm, Sweden, 2018. (In Swedish) [Google Scholar]
- Bik, H.M.; Goldstein, M.C. An Introduction to Social Media for Scientists. PLoS Biol. 2013, 11, e1001535. [Google Scholar] [CrossRef] [PubMed]
- FHVforskning. Available online: http://www.fhvforskning.se/ (accessed on 4 June 2020).
- Professornharordet. In Professornharordet. 2020, p Blog. Available online: http://www.professornharordet.se (accessed on 4 June 2020).
- Bramberg, E.B.; Nyman, T.; Kwak, L.; Alipour, A.; Bergstrom, G.; Elinder, L.S.; Hermansson, U.; Jensen, I. Development of evidence-based practice in occupational health services in Sweden: A 3-year follow-up of attitudes, barriers and facilitators. Int. Arch. Occup. Environ. Health 2017, 90, 335–348. [Google Scholar] [CrossRef] [PubMed]
- Björk Brämberg, E.; Nyman, T.L.K.; Alipour, A.; Bergström, G.; Schäfer Elinder, L.; Hermansson, U.; Jensen, I. Development of Evidence Based Practice in Occupational Health Services. A Three-Year Follow-Up of Attitudes, Barriers and Facilitators; IMM, Unit of Intervention and Implementation Research; Karolinska Institute: Stockholm, Sweden, 2015. [Google Scholar]
- SAWEE. Myndigheten för Arbetsmiljökunskap. Available online: https://www.mynak.se/ (accessed on 10 May 2006).
- Brownson, R.C.; Baker, E.A.; Deshpande, A.D.; Gillespie, K.N. Evidence-Based Public Health; Oxford University Press: New York, NY, USA, 2018. [Google Scholar]
- Barreto, J.E.; Whitehair, C.L. Social Media and Web Presence for Patients and Professionals: Evolving Trends and Implications for Practice. PM&R 2017, 9, S98–S105. [Google Scholar] [CrossRef]
- Brown, C.H.; Curran, G.; Palinkas, L.A.; Aarons, G.A.; Wells, K.B.; Jones, L.; Collins, L.M.; Duan, N.; Mittman, B.S.; Wallace, A.; et al. An Overview of Research and Evaluation Designs for Dissemination and Implementation. Annu. Rev. Public Health 2017, 38, 1–22. [Google Scholar] [CrossRef] [PubMed]
- Gordan, V.V.; Makhija, S.K.; Rindal, D.B.; Meyerowitz, C.; Fellows, J.L.; Ziegenfuss, J.Y.; Cochran, D.L.; Hudak, S.; Gilbert, G.H.; National Dental PBRN Collaborative Group. Leadership in practice-based research: The National Dental PBRN. J. Dent. 2019, 87, 24–27. [Google Scholar] [CrossRef] [PubMed]
- Fisher, M.; Brewer, S.E.; Westfall, J.M.; Simpson, M.; Zittleman, L.; O’Leary, S.T.; Fernald, D.H.; Nederveld, A.; Nease, D.E. Strategies for Developing and Sustaining Patient and Community Advisory Groups: Lessons from the State Networks of Colorado Ambulatory Practices and Partners (SNOCAP) Consortium of Practice-Based Research Networks. J. Am. Board Fam. Med. 2019, 32, 663–673. [Google Scholar] [CrossRef] [PubMed]
- Durlak, J.A.; DuPre, E.P. Implementation matters: A review of research on the influence of implementation on program outcomes and the factors affecting implementation. Am. J. Commun. Psychol. 2008, 41, 327–350. [Google Scholar] [CrossRef] [PubMed]
- Westfall, J.M.; Roper, R.; Gaglioti, A.; Nease, D.E. Practice-Based Research Networks: Strategic Opportunities to Advance Implementation Research for Health Equity. Ethn. Dis. 2019, 29, 113–118. [Google Scholar] [CrossRef] [PubMed]
- Bohlin, G.; Bergman, M. Researchers’ Views on Communication and Open Science in Sweden; Public and Science (VA): Stockholm, Sweden, 2019. [Google Scholar]

| Occupational Health Practice Guidelines |
|---|
| Guideline for non-specific low back-pain (launched 2014, updated 2018) Guideline for the treatment and prevention of common mental disorders at work (launched 2015, updated 2018) Guideline for health screening at work (launched 2015, updated 2018) Guideline for alcohol problems at work (launched 2016) Guideline for measuring noise-exposure at work (launched 2016) |
| Work Health Economic Analysis Tools |
| Analysis tool for the treatment and prevention of common mental disorders at work (launched 2016) Analysis tool for non-specific low back-pain (launched 2018) Analysis tool for health screening at work (launched 2018) |
| Question/Statement | n | Yes, % (n) | No, % (n) | |
|---|---|---|---|---|
| Aware of the guideline | 339 | 45.1 (153) | 54.9 (186) | |
| Questions put to those who answered yes to the question above, % (n) | ||||
| Yes partly | Yes fully | No | ||
| Adhere to the guideline | 142 # | 47.9 (68) | 30.3 (43) | 21.8 (31) |
| Agree | Partly agree | Disagree | ||
| The guideline is clear and understandable | 109 | 59.6 (65) | 33.9 (37) | 6.4 (7) |
| fits with our way of working | 108 | 37 (40) | 50 (54) | 13.0 (14) |
| lay-out makes it easy to work with | 105 | 43.8 (46) | 46.7 (49) | 9.5 (10) |
| is adaptable to our organization | 108 | 38.0 (41) | 48.1 (52) | 13.9 (159) |
| Takes our customers preferences into consideration | 106 | 34.0 (36) | 56.6 (60) | 34.0 (36) |
| Barriers to implementation | ||||
| I don’t know enough to work according to the guideline | 114 | 12.3 (14) | 27.2 (31) | 60.5 (69) |
| Lack of managerial support | 112 | 12.5 (14) | 17.9 (20) | 69.6 (78) |
| Guideline is difficult and complex | 112 | 10.7 (12) | 33.0 (37) | 56.3 (63) |
| Working according to the guideline is time-consuming | 110 | 11.8 (13) | 41.8 (46) | 46.4 (51) |
| Difficult to change routines | 111 | 2.7 (3) | 36.0 (40) | 61.3 (68) |
| Courses |
|---|
| Course in evidence-based practice Training in evidence-based brief alcohol rehabilitation Workshop implementation of brief alcohol rehabilitation Course in alcohol and drug problems, possible interventions in practice. Course in problem-solving based dialogue method |
| Seminars in Occupational Health Practice Guidelines |
| Guideline for non-specific low back-pain Guideline for the treatment and prevention of common mental disorders at work Guideline for health screening at work Guideline for alcohol problems at work Guideline for measuring noise exposure at work Economic analysis tool for common mental disorders |
| Task | Researchers | Partners |
|---|---|---|
| Resources (who is paying for what, intangible resources allocated, etc.) | Yes | Yes |
| Research design incl. intervention, method, etc. | Yes, but respect and listen to partners experiences and knowledge | Yes, but the final decisions must always be based on research quality and expertise |
| Data collection | Yes, responsible for designing how and when data collection should occur, material for information, etc. | Yes, if no conflict of interest, sensitive data, or other |
| Analysing data | Yes | No |
| Interpreting results | Yes, and if partners have no conflict of interest make use of the partners specific expertise of the setting/context (their workplace/work situation, etc.) | Yes, if no conflict of interest |
| Presenting and disseminating results | Yes | Yes |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
B. Jensen, I.; Björk Brämberg, E.; Wåhlin, C.; Björklund, C.; Hermansson, U.; Lohela Karlson, M.; Schäfer Elinder, L.; Munck af Rosenschöld, P.; Nevala, T.; Carter, N.; et al. Promoting Evidence-Based Practice for Improved Occupational Safety and Health at Workplaces in Sweden. Report on a Practice-Based Research Network Approach. Int. J. Environ. Res. Public Health 2020, 17, 5283. https://doi.org/10.3390/ijerph17155283
B. Jensen I, Björk Brämberg E, Wåhlin C, Björklund C, Hermansson U, Lohela Karlson M, Schäfer Elinder L, Munck af Rosenschöld P, Nevala T, Carter N, et al. Promoting Evidence-Based Practice for Improved Occupational Safety and Health at Workplaces in Sweden. Report on a Practice-Based Research Network Approach. International Journal of Environmental Research and Public Health. 2020; 17(15):5283. https://doi.org/10.3390/ijerph17155283
Chicago/Turabian StyleB. Jensen, Irene, Elisabeth Björk Brämberg, Charlotte Wåhlin, Christina Björklund, Ulric Hermansson, Malin Lohela Karlson, Liselotte Schäfer Elinder, Peter Munck af Rosenschöld, Tarja Nevala, Ned Carter, and et al. 2020. "Promoting Evidence-Based Practice for Improved Occupational Safety and Health at Workplaces in Sweden. Report on a Practice-Based Research Network Approach" International Journal of Environmental Research and Public Health 17, no. 15: 5283. https://doi.org/10.3390/ijerph17155283
APA StyleB. Jensen, I., Björk Brämberg, E., Wåhlin, C., Björklund, C., Hermansson, U., Lohela Karlson, M., Schäfer Elinder, L., Munck af Rosenschöld, P., Nevala, T., Carter, N., Mellblom, B., & Kwak, L. (2020). Promoting Evidence-Based Practice for Improved Occupational Safety and Health at Workplaces in Sweden. Report on a Practice-Based Research Network Approach. International Journal of Environmental Research and Public Health, 17(15), 5283. https://doi.org/10.3390/ijerph17155283






