Symptoms in Health Care Workers during the COVID-19 Epidemic. A Cross-Sectional Survey
Abstract
1. Introduction
2. Materials and Methods
2.1. Population
2.2. Questionnaire
2.3. Statistics
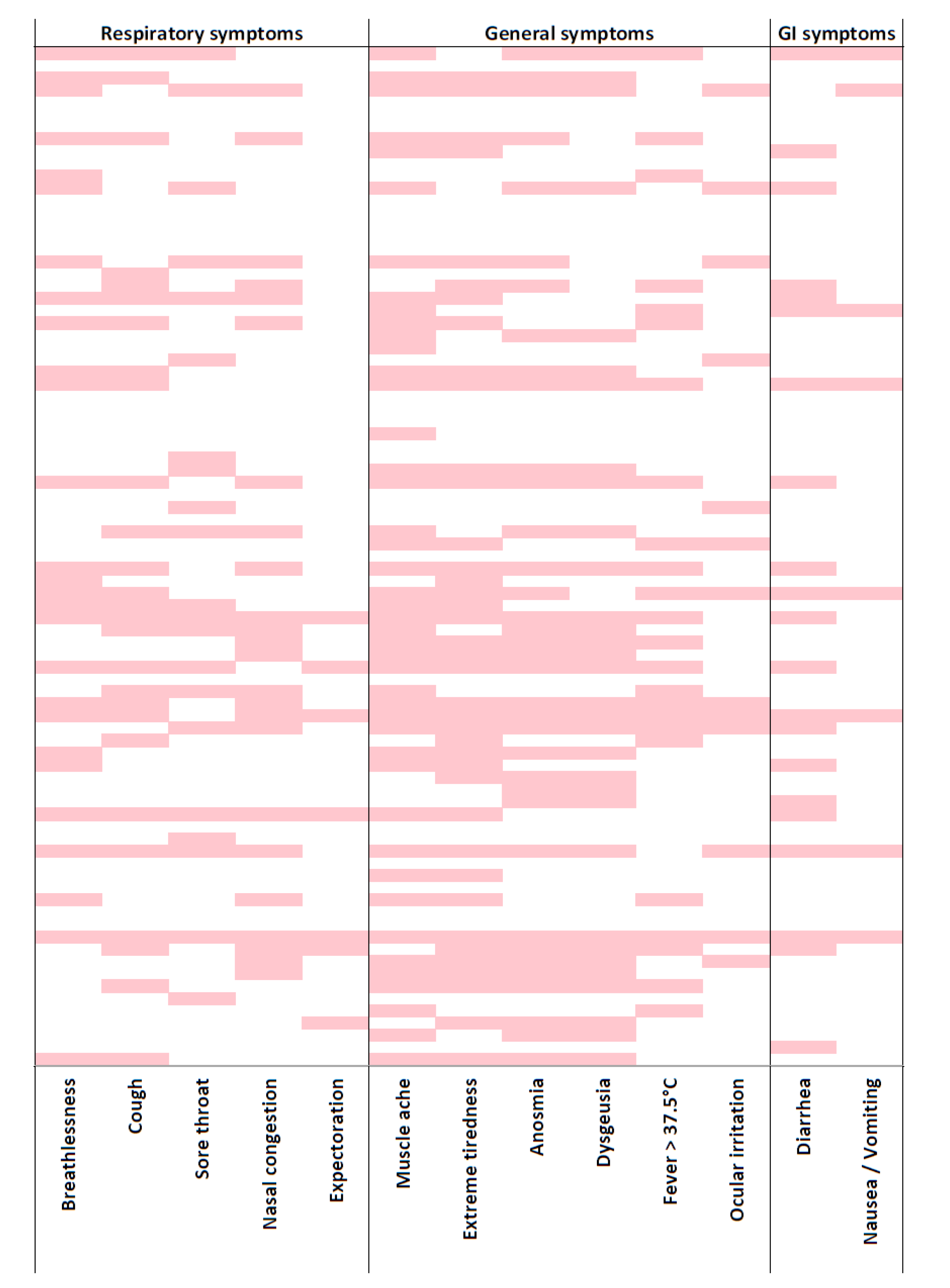
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Bahl, P.; Doolan, C.; de Silva, C.; Chughtai, A.A.; Bourouiba, L.; MacIntyre, C.R. Airborne or droplet precautions for health workers treating COVID-19? J. Infect. Dis. 2020. [Google Scholar] [CrossRef]
- Chirico, F.; Nucera, G.; Magnavita, N. COVID-19: Protecting Healthcare Workers is a priority. Infect. Control Hosp. Epidemiol. 2020, 1. [Google Scholar] [CrossRef]
- Chirico, F.; Nucera, G.; Magnavita, N. Estimating case fatality ratio during COVID-19 epidemics: Pitfalls and alternatives. J. Infect. Dev. Ctries 2020, 14, 438–439. [Google Scholar] [CrossRef] [PubMed]
- Chirico, F.; Nucera, G.; Magnavita, N. Hospital infection and COVID-19: Do not put all your eggs on the “swab” tests. Infect. Control Hosp. Epidemiol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Du, J.; Dong, L.; Wang, T.; Yuan, C.; Fu, R.; Zhang, L.; Liu, B.; Zhang, M.; Yin, Y.; Qin, J.; et al. Psychological symptoms among frontline healthcare workers during COVID-19 outbreak in Wuhan. Gen. Hosp. Psychiatry 2020. [Google Scholar] [CrossRef] [PubMed]
- Hunter, E.; Price, D.A.; Murphy, E.; van der Loeff, I.S.; Baker, K.F.; Lendrem, D.; Lendrem, C.; Schmid, M.L.; Pareja-Cebrian, L. Andrew Welch First experience of COVID-19 screening of health-care workers in England. Lancet 2020, 395, e77–e78. [Google Scholar] [CrossRef]
- Koh, D.; Goh, H.P. Occupational health responses to COVID-19: What lessons can we learn from SARS. J. Occup. Health 2020, 62, e12128. [Google Scholar] [CrossRef]
- Koh, D. Occupational risks for COVID-19 infection. Occup. Med. (Lond.) 2020, 70, 3–5. [Google Scholar] [CrossRef]
- Sim, M.R. The COVID-19 pandemic: Major risks to healthcare and other workers on the front line. Occup. Environ. Med. 2020, 77, 281–282. [Google Scholar] [CrossRef]
- Wee, L.E.; Sim, X.Y.J.; Conceicao, E.P.; Aung, M.K.; Goh, J.Q.; Yeo, D.W.T.; Gan, W.H.; Chua, Y.Y.; Wijaya, L.; Tan, T.T.; et al. Containment of COVID-19 cases among healthcare workers: The role of surveillance, early detection, and outbreak management. Infect. Control Hosp. Epidemiol. 2020. [Google Scholar] [CrossRef]
- Wynants, L.; van Calster, B.; Collins, G.S.; Riley, R.D.; Heinze, G.; Schuit, E.; Bonten, M.M.J.; Damen, J.A.A.; Debray, T.P.A.; de Vos, M.; et al. Prediction models for diagnosis and prognosis of COVID-19 infection: Systematic review and critical appraisal. BMJ 2020, 69, m1328. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; McIntyre, R.S.; Choo, F.N.; Tran, B.; Ho, R.; Sharma, V.K.; et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav. Immun. 2020. [Google Scholar] [CrossRef] [PubMed]
- CDC. Characteristics of Health Care Personnel with COVID-19—United States, February 12–April 9, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 477–481. [Google Scholar] [CrossRef] [PubMed]
- Kisely, S.; Warren, N.; McMahon, L.; Dalais, C.; Henry, I.; Siskind, D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: Rapid review and meta-analysis. BMJ 2020, 369, m1642. [Google Scholar] [CrossRef]
- Pappa, S.; Ntella, V.; Giannakas, T.; Giannakoulis, V.G.; Papoutsi, E.; Katsaounou, P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav. Immun. 2020. [Google Scholar] [CrossRef]
- Vindegaard, N.; Eriksen Benros, M. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav. Immun. 2020. [Google Scholar] [CrossRef]
- Puro, V.; Magnavita, N.; Ippolito, G. SARS and masks. J. Hosp. Infect. 2004, 56, 73–74. [Google Scholar] [CrossRef]
- Offeddu, V.; Yung, C.F.; Low, M.S.F.; Tam, C.C. Effectiveness of Masks and Respirators against Respiratory Infections in Healthcare Workers: A Systematic Review and Meta-Analysis. Clin. Infect. Dis. 2017, 65, 1934–1942. [Google Scholar] [CrossRef]
- Magnavita, N.; Sestili, C.; Mannocci, A.; Ercoli, E.; Boccia, A.; Bonaga, G.; Sica, S.; Maurici, M.; Alvaro, R.; Sili, A.; et al. Mental and physical wellbeing in Oncology-haematology unit personnel. Arch. Environ. Occup. Health 2017, 73, 375–380. [Google Scholar] [CrossRef]
- Magnavita, N. The exploding spark. Workplace violence in an infectious disease hospital-A longitudinal study. BMRI Biomed. Res. Int. 2013, 2013, 316358. [Google Scholar] [CrossRef]
- Magnavita, N. Workplace violence and occupational stress in health care workers: A chicken and egg situation - Results of a 6-year follow-up study. J. Nurs. Scholarsh. 2014, 46, 366–376. [Google Scholar] [CrossRef]
- Wacholder, S.; McLaughlin, J.K.; Silverman, D.T.; Mandel, J.S. Selection of controls in case-control studies. I. Principles. Am. J. Epidemiol. 1992, 135, 1019–1028. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, D.; Bridges, K.; Duncan-Jones, P.; Grayson, D. Detecting anxiety and depression in general medical settings. BMJ 1988, 297, 897–899. [Google Scholar] [CrossRef] [PubMed]
- Magnavita, N. Anxiety and depression at work. The A/D Goldberg Questionnaire. G. Ital. Med. Lav. Ergon. 2007, 29, 670–671. [Google Scholar] [PubMed]
- Colquitt, J.A. On the dimensionality of organizational justice: A construct validation of a measure. J. Appl. Psychol. 2001, 86, 386–400. [Google Scholar] [CrossRef]
- Magnavita, N.; Bergamaschi, A. Justice at the workplace. Validation of the Italian version of Colquitt’s justice measurement questionnaire (JM20). G. Ital. Med. Lav. Ergon. 2008, 30, 449–450. [Google Scholar]
- Elovainio, M.; Heponiemi, T.; Kuusio, H.; Sinervo, T.; Hintsa, T.; Aalto, A.M. Developing a short measure of organizational justice: A multisample health professionals study. J. Occup. Environ. Med. 2010, 52, 1068–1074. [Google Scholar] [CrossRef]
- Elovainio, M.; Heponiemi, T.; Sinervo, T.; Magnavita, N. Organizational justice and health; review of evidence. G. Ital. Med. Lav. Ergon. 2010, 32, B5–B9. [Google Scholar]
- Magnavita, N.; Garbarino, S. Social psychiatry in the waiting room. What a physician can learn about occupational stress from workers waiting to be examined. Psychiatry J. 2013, 2013, 701872. [Google Scholar] [CrossRef]
- Van, H.N.; Le, M.D.; Van, T.N.; Ngoc, D.N.; Ngoc, A.T.T. A systematic review of effort-reward imbalance among health workers. Int. J. Health Plan. Manag. 2018. [Google Scholar] [CrossRef]
- Bernal, D.; Campos-Serna, J.; Tobias, A.; Vargas-Prada, S.; Benavides, F.G.; Serra, C. Work-related psychosocial risk factors and musculoskeletal disorders in hospital nurses and nursing aides: A systematic review and meta-analysis. Int. J. Nurs. Stud. 2015, 52, 635–648. [Google Scholar] [CrossRef] [PubMed]
- Siegrist, J.; Wege, N.; Puhlhofer, F.; Wahrendorf, M. A short generic measure of work stress in the era of globalization: Effort-reward imbalance. Int. Arch. Occup. Environ. Health 2009, 82, 1005–1013. [Google Scholar] [CrossRef] [PubMed]
- Magnavita, N.; Garbarino, S.; Siegrist, J. The use of parsimonious questionnaires in occupational health surveillance. Psychometric properties of the short Italian version of the Effort/Reward Imbalance questionnaire. TSWJ Sci. World J. 2012, 2012, 372852. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Siegrist, J. Adverse health effects of high-effort/low-reward conditions. J. Occup. Health Psychol. 1996, 1, 27–41. [Google Scholar] [CrossRef]
- Espie, C.A.; Kyle, S.D.; Hames, P.; Gardani, M.; Fleming, L.; Cape, J. The Sleep Condition Indicator: A clinical screening tool to evaluate insomnia disorder. BMJ Open 2014, 4, e004183. [Google Scholar] [CrossRef]
- Palagini, L.; Ragno, G.; Caccavale, L.; Gronchi, A.; Terzaghi, M.; Mauri, M.; Kyle, S.D.; Espie, C.A.; Manni, R. Italian validation of the Sleep Condition Indicator: A clinical screening tool to evaluate Insomnia Disorder according to DSM-5 criteria. Int. J. Psychophysiol. 2015, 98, 435–440. [Google Scholar] [CrossRef]
- Espie, C.A.; Farias Machado, P.; Carl, J.R.; Kyle, S.D.; Cape, J.; Siriwardena, A.N.; Luik, A.I. The Sleep Condition Indicator: Reference values derived from a sample of 200 000 adults. J. Sleep Res. 2018, 27, e12643. [Google Scholar] [CrossRef]
- Maunder, R.G.; Hunter, J.J.; Vincent, L.; Bennett, J.; Peladeau, N.; Leszcz, M.; Sadavoy, J.; Verhaeghe, L.M.; Steinberg, R.; Mazzulli, T. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. Can. Med. Assoc. J. 2003, 168, 1245–1251. [Google Scholar]
- Aronsson, G.; Theorell, T.; Grape, T.; Hammarström, A.; Hogstedt, C.; Marteinsdottir, I.; Skoog, I.; Träskman-Bendz, L.; Hall, C. A systematic review including meta-analysis of work environment and burnout symptoms. BMC Public Health 2017, 17, 264. [Google Scholar] [CrossRef]
- Stewart, N.H.; Arora, V.M. The Impact of Sleep and Circadian Disorders on Physician Burnout. Chest 2019, 156, 1022–1030. [Google Scholar] [CrossRef]
- Magnavita, N.; Heponiemi, T. Violence towards health care workers in a Public Health Care Facility in Italy: A repeated cross-sectional study. BMC Health Serv. Res. 2012, 12, 108. [Google Scholar] [CrossRef]
- Magnavita, N. Work-related symptoms in indoor environments: A puzzling problem for the occupational physician. Int. Arch. Occup. Environ. Health 2015, 88, 185–196. [Google Scholar] [CrossRef] [PubMed]
- European Centre for Disease Prevention and Control (ECDC). Contact tracing: Public Health Management of Persons, Including Healthcare Workers, Having Had Contact with COVID-19 Cases in the European Union–Second Update, 8 April 2020; ECDC: Stockholm, Sweden, 2020; Available online: https://www.ecdc.europa.eu/en/covid-19-contact-tracing-public-health-management (accessed on 16 June 2020).
- Lake, M.A. What we know so far: COVID-19 current clinical knowledge and research. Clin. Med. 2020, 20, 124–127. [Google Scholar] [CrossRef]
- Pascarella, G.; Strumia, A.; Piliego, C.; Bruno, F.; Del Buono, R.; Costa, F.; Scarlata, S.; Agrò, F.E. COVID-19 diagnosis and management: A comprehensive review. J. Intern. Med. 2020. [Google Scholar] [CrossRef] [PubMed]
- Zhao, N.; Zhou, Z.L.; Wu, L.; Zhang, X.D.; Han, S.B.; Bao, H.J.; Shu, Y.; Shu, X.G. An update on the status of COVID-19: A comprehensive review. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 4597–4606. [Google Scholar] [CrossRef]
- Jin, Y.H.; Huang, Q.; Wang, Y.Y.; Zeng, X.T.; Luo, L.S.; Pan, Z.Y.; Yuan, Y.F.; Chen, Z.M.; Cheng, Z.S.; Huang, X.; et al. Perceived infection transmission routes, infection control practices, psychosocial changes, and management of COVID-19 infected healthcare workers in a tertiary acute care hospital in Wuhan: A cross-sectional survey. Mil. Med. Res. 2020, 7, 24. [Google Scholar] [CrossRef]
- Wei, W.E.; Li, Z.; Chiew, C.J.; Yong, S.E.; Toh, M.P.; Lee, V.J. Presymptomatic Transmission of SARS-CoV-2 - Singapore, January 23-March 16, 2020. Morb. Mortal. Wkly. Rep. 2020, 69, 411–415. [Google Scholar] [CrossRef] [PubMed]
- Hu, Z.; Song, C.; Xu, C.; Jin, G.; Chen, Y.; Xu, X.; Ma, H.; Chen, W.; Lin, Y.; Zheng, Y.; et al. Clinical Characteristics of 24 Asymptomatic Infections With COVID-19 Screened Among Close Contacts in Nanjing, China. Sci. China Life Sci. 2020, 63, 706–711. [Google Scholar] [CrossRef]
- Chow, E.J.; Schwartz, N.G.; Tobolowsky, F.A.; Zacks, R.L.T.; Huntington-Frazier, M.; Reddy, S.C.; Rao, A.K. Symptom Screening at Illness Onset of Health Care Personnel with SARS-CoV-2 Infection in King County, Washington. JAMA 2020, 323, 2087–2089. [Google Scholar] [CrossRef]
- Tostmann, A.; Bradley, J.; Bousema, T.; Yiek, W.K.; Holwerda, M.; Bleeker-Rovers, C.P.; Oever, J.; Rahamat-Langendoen, J.C.; Hopman, J.; van der Geest-Blankert, N.; et al. Strong associations and moderate predictive value of early symptoms for SARS-CoV-2 test positivity among healthcare workers, the Netherlands, March 2020. Eurosurveillance 2020, 25, 2000508. [Google Scholar] [CrossRef]
- Vaira, L.A.; Salzano, G.; Deiana, G.; De Riu, G. Anosmia and ageusia: Common findings in COVID-19 patients. Laryngoscope 2020, 130, 1787. [Google Scholar] [CrossRef] [PubMed]
- Chilvers, M.A.; McKean, M.; Rutman, A.; Myint, B.S.; Silverman, M.; O’Callaghan, C. The effects of coronavirus on human nasal ciliated respiratory epithelium. Eur. Respir. J. 2001, 18, 965–970. [Google Scholar] [CrossRef] [PubMed]
- Lan, F.Y.; Filler, R.; Mathew, S.; Buley, J.; Iliaki, E.; Bruno-Murtha, L.A.; Osgood, R.; Christophi, C.A.; Fernandez-Montero, A.; Kales, S.N. COVID-19 Symptoms Predictive of Healthcare Workers’ SARS-CoV-2 PCR Results. PLoS ONE 2020, 15, e0235460. [Google Scholar] [CrossRef]
- To, K.K.; Tsang, O.T.; Leung, W.S.; Tam, A.R.; Wu, T.C.; Lung, D.C.; Yip, C.C.Y.; Cai, J.P.; Chan, J.M.C.; Chik, T.S.H.; et al. Temporal profiles of viral load in posterior oropharyngeal saliva samples and serum antibody responses during infection by SARS-CoV-2: An observational cohort study. Lancet Infect. Dis. 2020, 20, 565–574. [Google Scholar] [CrossRef]
- Van den Bergh, M.F.Q.; Buiting, A.G.M.; Pas, S.D.; Bentvelsen, R.G.; van den Bijllaardt, W.; van Oudheusden, A.J.G.; van Rijen, M.M.L.; Verweij, J.J.; Koopmans, M.P.G.; Kluytmans, J.J.W. Prevalence and Clinical Presentation of Health Care Workers with Symptoms of Coronavirus Disease 2019 in 2 Dutch Hospitals During an Early Phase of the Pandemic. JAMA Netw. Open 2020, 3, e209673. [Google Scholar] [CrossRef] [PubMed]
- Rivett, L.; Sridhar, S.; Sparkes, D.; Routledge, M.; Jones, N.K.; Forrest, S.; Young, J.; Pereira-Dias, J.; Hamilton, W.L.; Ferris, M.; et al. Screening of healthcare workers for SARS-CoV-2 highlights the role of asymptomatic carriage in COVID-19 transmission. Elife 2020, 9, e58728. [Google Scholar] [CrossRef] [PubMed]
- Maben, J.; Bridges, J. Covid-19: Supporting Nurses’ Psychological and Mental Health. J. Clin. Nurs. 2020. [Google Scholar] [CrossRef]
- Fang, Y.; Zhang, H.; Xie, J.; Lin, M.; Ying, L.; Pang, P.; Ji, W. Sensitivity of chest CT for COVID-19: Comparison to RT-PCR. Radiology 2020. [Google Scholar] [CrossRef]
- Sun, D.; Yang, D.; Li, Y.; Zhou, J.; Wang, W.; Wang, Q.; Lin, N.; Cao, A.; Wang, H.; Zhang, Q. Psychological impact of 2019 novel coronavirus (2019-nCoV) outbreak in health workers in China. Epidemiol. Infect. 2020, 148, e96. [Google Scholar] [CrossRef]
- Cai, W.; Lian, B.; Song, X.; Hou, T.; Deng, G.; Li, H. A cross-sectional study on mental health among health care workers during the outbreak of Corona Virus Disease 2019. Asian J. Psychiatr. 2020, 51, 102111. [Google Scholar] [CrossRef]
- Zhu, J.; Sun, L.; Zhang, L.; Wang, H.; Fan, A.; Yang, B.; Li, W.; Xiao, S. Prevalence and Influencing Factors of Anxiety and Depression Symptoms in the First-Line Medical Staff Fighting Against COVID-19 in Gansu. Front. Psychiatry 2020, 11, 386. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.Y.; Yang, Y.Z.; Zhang, X.M.; Xu, X.; Dou, Q.L.; Zhang, W.W.; Cheng, A.S.K. The prevalence and influencing factors in anxiety in medical workers fighting COVID-19 in China: A cross-sectional survey. Epidemiol. Infect. 2020, 148, e98. [Google Scholar] [CrossRef] [PubMed]
- Lai, J.; Ma, S.; Wang, Y.; Cai, Z.; Hu, J.; Wei, N.; Wu, J.; Du, H.; Chen, T.; Li, R.; et al. Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw. Open 2020, 3, e203976. [Google Scholar] [CrossRef] [PubMed]
- Chew, N.W.S.; Lee, G.K.H.; Tan, B.Y.Q.; Jing, M.; Goh, Y.; Ngiam, N.; Yeo, L.L.L.; Ahmad, A.; Khan, F.A.; Shanmugam, G.N.; et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav. Immun. 2020. [Google Scholar] [CrossRef]
- Xiang, Y.T.; Yang, Y.; Li, W.; Zhang, L.; Zhang, Q.; Cheung, T.; Ng, C.H. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry 2020, 7, 228–229. [Google Scholar] [CrossRef]
- Walton, M.; Murray, E.; Christian, M.D. Mental health care for medical staff and affiliated healthcare workers during the COVID-19 pandemic. Eur. Heart J. Acute Cardiovasc. Care 2020. [Google Scholar] [CrossRef]
- Bohlken, J.; Schömig, F.; Lemke, M.R.; Pumberger, M.; Riedel-Heller, S.G. COVID-19 Pandemic: Stress Experience of Healthcare Workers—A Short Current Review. Psychiatr. Prax. 2020, 47, 190–197. [Google Scholar] [CrossRef]
- Garbarino, S.; Magnavita, N. Sleep problems are a strong predictor of stress-related metabolic changes in police officers. A prospective study. PLoS ONE 2019, 14, e0224259. [Google Scholar] [CrossRef]
| Variable | Positive n (%) | Exposed n (%) | Control n (%) | Chi Square Test for Groups p |
|---|---|---|---|---|
| Groups | 82 (13.8) | 152 (25.5) | 361 (60.7) | |
| Gender, female | 56 (68.3) | 104 (68.4) | 257 (71.2) | n.s. |
| Family, single | 64 (78.0) | 116 (76.3) | 273 (75.6) | n.s. |
| With Children | 40 (48.8) | 71 (46.7) | 199 (55.1) | n.s. |
| With Parents/Relatives | 62 (75.6) | 131 (86.2) | 294 (81.4) | n.s. |
| With Help | 69 (84.1) | 117 (77.0) | 281 (77.8) | n.s. |
| Variable | Positive n (%) | Exposed n (%) | Control n (%) | Chi Square Test for Groups p |
|---|---|---|---|---|
| Job category | <0.001 | |||
| Physician | 11 (13.4) | 39 (25.7) | 86 (23.8) | |
| Nurse | 58 (70.7) | 84 (55.3) | 155 (42.9) | |
| Technician | 7 (8.5) | 14 (9.2) | 43 (11.9) | |
| Clerk | 2 (2.4) | 7 (4.6) | 47 (13.0) | |
| Other | 4 (4.9) | 8 (5.3) | 30 (8.3) | |
| Age class (years) | 0.012 | |||
| <35 | 12 (14.6) | 16 (10.5) | 36 (10.0) | |
| 36–45 | 17 (20.7) | 40 (26.3) | 61 (16.9) | |
| 46–55 | 38 (46.3) | 60 (39.5) | 137 (38.0) | |
| >55 | 15 (18.3) | 36 (23.7) | 127 (35.2) |
| Symptom | Positive n (%) | Exposed n (%) | Control n (%) | Chi Square Test for Groups p |
|---|---|---|---|---|
| Fever | 23 (28.0) | 7 (4.6) | 6 (1.7) | <0.001 |
| Breathlessness | 26 (31.7) | 9 (5.9) | 10 (2.8) | <0.001 |
| Cough | 26 (31.7) | 16 (10.5) | 15 (4.2) | <0.001 |
| Expectorate | 7 (8.5) | 5 (3.3) | 5 (1.4) | <0.002 |
| Sore throat | 20 (24.4) | 20 (13.2) | 14 (3.9) | <0.001 |
| Anosmia | 35 (42.7) | 1 (0.7) | 3 (0.8) | <0.001 |
| Dysgeusia | 31 (37.8) | 5 (3.3) | 4 (1.1) | <0.001 |
| Nasal congestion | 24 (29.3) | 12 (7.9) | 16 (4.4) | <0.001 |
| Eye irritation | 13 (15.9) | 14 (9.2) | 22 (6.1) | <0.013 |
| Exhaustion | 39 (47,6) | 31 (20.4) | 21 (5.8) | <0.001 |
| Muscle pain | 43 (52.4) | 22 (14.5) | 23 (6.4) | <0.001 |
| Diarrhoea | 20 (24.4) | 13 (8.6) | 15 (4.2) | <0.001 |
| Nausea | 7 (8.5) | 3 (2.0) | 5 (1.4) | <0.001 |
| No symptom | 24 (29.3) | 100 (65.8) | 299 (82.8) | <0.001 |
| Distressed | 24 (29.3) | 47 (30.9) | 109 (30.2) | n.s. |
| Anxious | 29 (35.4) | 29 (19.1) | 41 (11.4) | <0.001 |
| Depressed | 30 (36.9) | 40 (26.3) | 51 (14.1) | <0.001 |
| Symptom | Positive OR (95%CI) | Exposed OR (95%CI) | Control OR (95%CI) |
|---|---|---|---|
| Fever | 23.065 (9.012–59.033) *** | 2.856 (0.944- 8.645) | 1 |
| Breathlessness | 16.296 (7.456–35.619) *** | 2.209 (0.879–5.550) | 1 |
| Cough | 10.710 (5.343–21.467) *** | 2.714 (1.305–5.641) ** | 1 |
| Expectorate | 6.645 (2.054–21.504) ** | 2.422 (0.691–8.490) | 1 |
| Sore throat | 7.995 (3.836–16.666) *** | 3.755 (1.843–7.652) *** | 1 |
| Anosmia | 88.865 (26.297–300.301) *** | 0.790 (0.082–7.658) | 1 |
| Dysgeusia | 54.250 (18.389–160.042) *** | 3.036 (0.804–11.464) | 1 |
| Nasal congestion | 8.922 (4.471–17.807) *** | 1.848 (0.852–4.007) | 1 |
| Eye irritation | 2.903 (1.395–6.042) ** | 1.563 (0.777–3.144) | 1 |
| Exhaustion | 14.684 (7.914–27.246) *** | 4.148 (2.296–7.494) *** | 1 |
| Muscle pain | 16.203 (8.847–29.676) *** | 2.487 (1.340–4.616) ** | 1 |
| Diarrhoea | 7.441 (3.615–15.317) *** | 2.157 (1.001–4.652) * | 1 |
| Nausea | 6.645 (2.054–21.504) ** | 1.434 (0.338–6.075) | 1 |
| No symptom | 0.086 (0.050–0.149) *** | 0.399 (0.259–0.615) *** | 1 |
| Distressed | 0.957 (0.565–1.619) | 1.035 (0.686–1.561) | 1 |
| Anxious | 4.271 (2.446–7.457) *** | 1.840 (1.095–3.092) * | 1 |
| Depressed | 3.507 (2.047–6.007) *** | 2.171 (1.361–3.463) ** | 1 |
| Symptom | Model I OR (95%CI) | Model II OR (95%CI) | Model III OR (95%CI) |
|---|---|---|---|
| Fever | 24.265 (9.296–63.338) *** | 21.599 (8.215–56.793) *** | 20.270 (7.688–53.442) *** |
| Breathlessness | 17.503 (7.846–39.047) *** | 15.746 (7.005–35.393) *** | 14.931 (6.621–33.668) *** |
| Cough | 10.974 (5.379–22. 386) *** | 9.839 (4.767–20.307) *** | 9.046 (4.359–18.773) *** |
| Expectorate | 7.614 (2.178–26.615) *** | 6.653 (1.881–23.526) ** | 6.364 (1.795–22.565) ** |
| Sore throat | 8.684 (4.064–18.557) *** | 8.007 (3.717–17.248) *** | 7.536 (3.485–16.296) *** |
| Anosmia | 117.362 (31.583–436.122) *** | 102.991 (27.676–383.267) *** | 100.727 (26.520–382.578) *** |
| Dysgeusia | 62.763 (20.247–194.557) *** | 58.098 (18.580–181.665) *** | 51.813 (16.573–161.980) *** |
| Nasal congestion | 9.246 (4.549–18.792) *** | 7.997 (3.879–16.485) *** | 7.565 (3.651–15.675) *** |
| Eye irritation | 3.884 (1.780–8.475) ** | 3.293 (1.488–7.289) ** | 3.087 (1.383–6.891) ** |
| Exhaustion | 18.121 (9.403–34.920) *** | 16.414 (8.461–31.845) *** | 16.111 (8.128–31.937) *** |
| Muscle pain | 20.100 (10.498–38.486) *** | 18.321 (9.487–35.383) *** | 18.310 (9.221–36.360) *** |
| Diarrhoea | 7.616 (3.641–15.933) *** | 6.517 (3.080–13.788) *** | 5.799 (2.718–12.374) *** |
| Nausea | 6.267 (1.881–20.880) ** | 5.457 (1.611–18.491) ** | 5.129 (1.507–17.464) ** |
| Anxious | 4.395 (2.479–7.792) *** | 3.715 (2.021–6.827) *** | 3.704 (1.854–7.401) *** |
| Depressed | 3.849 (2.208–6.707) *** | 3.284 (1.811–5.957) *** | 3.175 (1.596–6.315) *** |
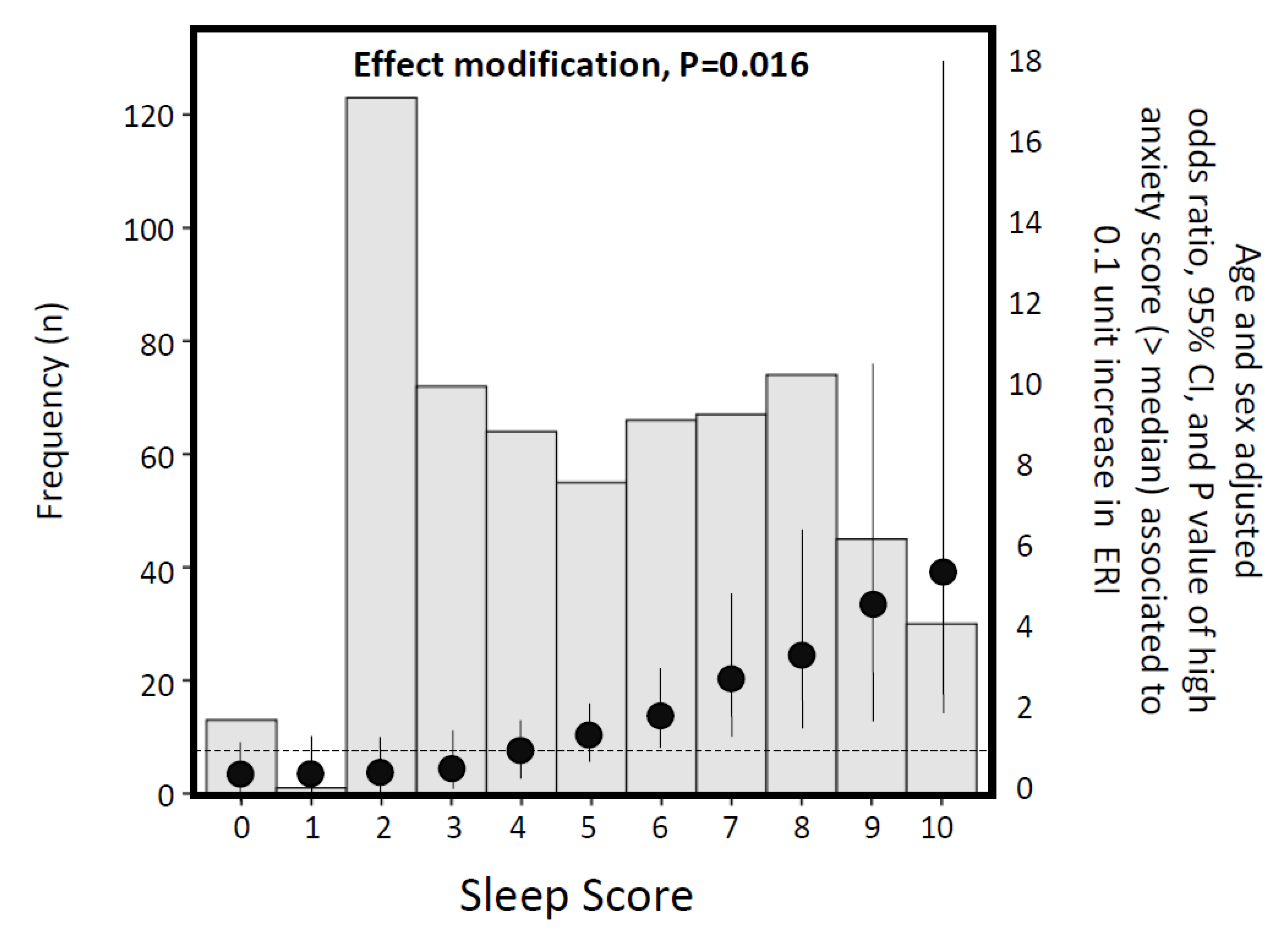
| Variable | Anxiety Standardized Beta | p | Depression Standardized Beta | p |
|---|---|---|---|---|
| Group * | −0.130 | 0.000 | −0.138 | 0.000 |
| Gender (female) | 0.123 | 0.000 | 0.074 | 0.019 |
| Age | - | - | - | - |
| Family | - | - | - | - |
| Children | - | - | - | - |
| Parents | - | - | - | - |
| Helping people | - | - | - | - |
| Effort | 0.154 | 0.000 | 0.155 | 0.000 |
| Reward | - | - | −0.111 | 0.002 |
| Justice | −0.129 | 0.000 | −0.070 | 0.047 |
| Sleep quality | −0.531 | 0.000 | −0.496 | 0.000 |
| Coefficient of determination R2 | 0.458 | 0.430 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Magnavita, N.; Tripepi, G.; Di Prinzio, R.R. Symptoms in Health Care Workers during the COVID-19 Epidemic. A Cross-Sectional Survey. Int. J. Environ. Res. Public Health 2020, 17, 5218. https://doi.org/10.3390/ijerph17145218
Magnavita N, Tripepi G, Di Prinzio RR. Symptoms in Health Care Workers during the COVID-19 Epidemic. A Cross-Sectional Survey. International Journal of Environmental Research and Public Health. 2020; 17(14):5218. https://doi.org/10.3390/ijerph17145218
Chicago/Turabian StyleMagnavita, Nicola, Giovanni Tripepi, and Reparata Rosa Di Prinzio. 2020. "Symptoms in Health Care Workers during the COVID-19 Epidemic. A Cross-Sectional Survey" International Journal of Environmental Research and Public Health 17, no. 14: 5218. https://doi.org/10.3390/ijerph17145218
APA StyleMagnavita, N., Tripepi, G., & Di Prinzio, R. R. (2020). Symptoms in Health Care Workers during the COVID-19 Epidemic. A Cross-Sectional Survey. International Journal of Environmental Research and Public Health, 17(14), 5218. https://doi.org/10.3390/ijerph17145218







