Manipulative Therapy Plus Ankle Therapeutic Exercises for Adolescent Baseball Players with Chronic Ankle Instability: A Single-Blinded Randomized Controlled Trial
Abstract
1. Introduction
2. Methods
2.1. Design and Ethics
2.2. Participants
2.3. Experimental Procedures and Interventions
2.4. Outcome Measures
2.4.1. Primary Variable
2.4.2. Secondary Variables
2.5. Statistical Analysis
3. Results
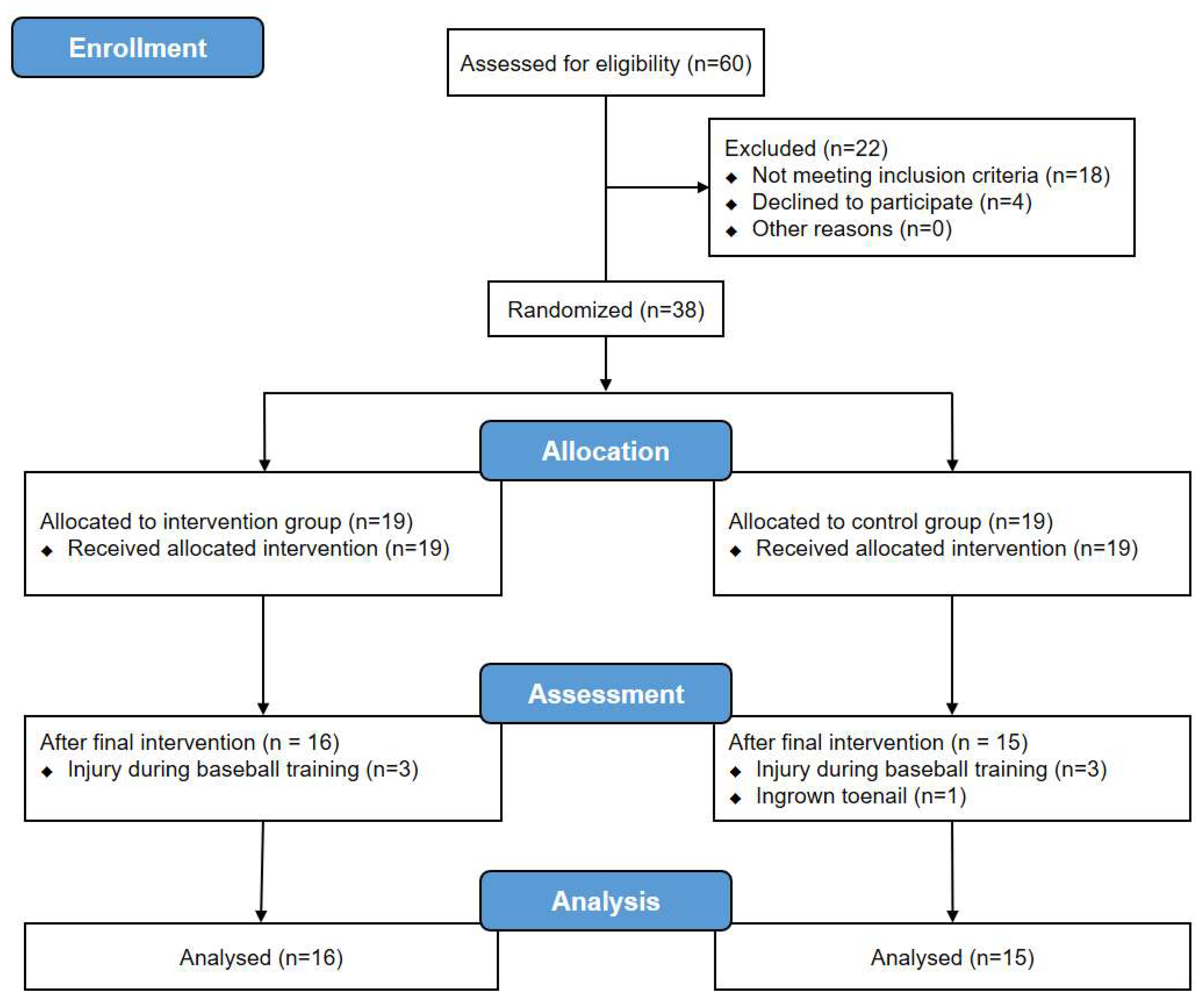
3.1. Participants
3.2. Status of the Ankle
3.3. Pain Intensity and PPT
3.4. Ankle ROM
3.5. Balance Ability
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Habelt, S.; Hasler, C.C.; Steinbrück, K.; Majewski, M. Sport injuries in adolescents. Orthop. Rev. (Pavia) 2011, 3, e18. [Google Scholar] [CrossRef] [PubMed]
- Lucasti, C.J.; Dworkin, M.; Warrender, W.J.; Winters, B.; Cohen, S.; Ciccotti, M.; Pedowitz, D. Ankle and lower leg injuries in professional baseball players. Am. J. Sports Med. 2020, 48, 908–915. [Google Scholar] [CrossRef] [PubMed]
- Drewes, L.K.; McKeon, P.O.; Kerrigan, D.C.; Hertel, J. Dorsiflexion deficit during jogging with chronic ankle instability. J. Sci. Med. Sport 2009, 12, 685–687. [Google Scholar] [CrossRef] [PubMed]
- Valderrabano, V.; Wiewiorski, M.; Frigg, A.; Hintermann, B.; Leumann, A. Chronische instabilität des oberen sprunggelenks. Unfallchirurg 2007, 110, 691–700. [Google Scholar] [CrossRef] [PubMed]
- Denegar, C.R.; Hertel, J.; Fonseca, J. The effect of lateral ankle sprain on dorsiflexion range of motion, posterior talar glide, and joint laxity. J. Orthop. Sports Phys. Ther. 2002, 32, 166–173. [Google Scholar] [CrossRef] [PubMed]
- Koldenhoven, R.M.; Feger, M.A.; Fraser, J.J.; Saliba, S.; Hertel, J. Surface electromyography and plantar pressure during walking in young adults with chronic ankle instability. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 1060–1070. [Google Scholar] [CrossRef]
- Houston, M.N.; Van Lunen, B.L.; Hoch, M.C. Health-related quality of life in individuals with chronic ankle instability. J. Athl. Train. 2014, 49, 758–763. [Google Scholar] [CrossRef]
- Simon, J.E.; Docherty, C.L. Health-related quality of life is decreased in middle-aged adults with chronic ankle instability. J. Sci. Med. Sport. 2018, 21, 1206–1209. [Google Scholar] [CrossRef]
- Pellow, J.E.; Brantingham, J.W. The efficacy of adjusting the ankle in the treatment of subacute and chronic grade I and grade II ankle inversion sprains. J. Manip. Physiol Ther. 2001, 24, 17–24. [Google Scholar] [CrossRef]
- López-Rodríguez, S.; Fernández de-Las-Peñas, C.; Alburquerque-Sendín, F.; Rodríguez-Blanco, C.; Palomeque-del-Cerro, L. Immediate effects of manipulation of the talocrural joint on stabilometry and baropodometry in patients with ankle sprain. J. Manipul. Physiol Ther. 2007, 30, 186–192. [Google Scholar] [CrossRef]
- Dananberg, H.J.; Shearstone, J.; Guillano, M. Manipulation method for the treatment of ankle equinus. J. Am. Podiatr. Med. Assoc. 2000, 90, 385–389. [Google Scholar] [CrossRef] [PubMed]
- Nield, S.; Davis, K.; Latimer, J.; Maher, C.; Adams, R. The effect of manipulation on range of movement at the ankle joint. Scand. J. Rehabil. Med. 1993, 25, 161–166. [Google Scholar] [PubMed]
- Andersen, S.; Fryer, G.A.; McLaughlin, P. The effect of talo-crural joint manipulation on range of motion at the ankle joint in subjects with a history of ankle injury. Australas Chiropr. Osteopat. 2003, 11, 57–62. [Google Scholar]
- LeClaire, J.; Wikstrom, E.A. Massage improves postural control in those with chronic ankle instability. Athl. Train. Sports Health Care 2012, 4, 213–219. [Google Scholar] [CrossRef]
- Hall, E.A.; Docherty, C.L.; Simon, J.; Kingma, J.J.; Klossner, J.C. Strength-training protocols to improve deficits in participants with chronic ankle instability: A randomized controlled trial. J. Athl. Train. 2015, 50, 36–44. [Google Scholar] [CrossRef] [PubMed]
- Gilbreath, J.P.; Gaven, S.L.; Van Lunen, L.; Hoch, M.C. The effects of mobilization with movement on dorsiflexion range of motion, dynamic balance, and self-reported function in individuals with chronic ankle instability. Man. Ther. 2014, 19, 152–157. [Google Scholar] [CrossRef]
- Gillman, S.F. The impact of chiropractic manipulative therapy on chronic recurrent lateral ankle sprain syndrome in two young athletes. J. Chiropr. Med. 2004, 3, 153–159. [Google Scholar] [CrossRef]
- Martínez-Segura, R.; Fernández-de-las-Peñas, C.; Ruiz-Sáez, M.; López-Jiménez, C.; Rodríguez-Blanco, C. Immediate effects on neck pain and active range of motion after a single cervical high-velocity low-amplitude manipulation in subjects presenting with mechanical neck pain: A randomized controlled trial. J. Manipul. Physiol. Ther. 2006, 29, 511–517. [Google Scholar] [CrossRef]
- Beazell, J.R.; Grindstaff, T.L.; Sauer, L.D.; Magrum, E.M.; Ingersoll, C.D.; Hertel, J. Effects of a proximal or distal tibiofibular joint manipulation on ankle range of motion and functional outcomes in individuals with chronic ankle instability. J. Orthop. Sports Phys. Ther. 2012, 42, 125–134. [Google Scholar] [CrossRef]
- Cruz-Diaz, D.; Lomas-Vega, R.; Osuna-Pérez, M.C.; Contreras, F.H.; Martínez-Amat, A. Effects of 6 weeks of balance training on chronic ankle instability in athletes: A randomized controlled trial. Int. J. Sports Med. 2015, 36, 754–760. [Google Scholar] [CrossRef]
- Kim, E.; Choi, H.; Cha, J.H.; Park, J.C.; Kim, T. Effects of neuromuscular training on the rear-foot angle kinematics in elite women field hockey players with chronic ankle instability. J. Sports Sci. Med. 2017, 16, 137–146. [Google Scholar] [PubMed]
- Sefton, J.M.; Yarar, C.; Hicks-Little, C.A.; Berry, J.W.; Cordova, M.L. Six weeks of balance training improves sensorimotor function in individuals with chronic ankle instability. J. Orthop. Sports Phys. Ther. 2011, 41, 81–89. [Google Scholar] [CrossRef]
- Hale, S.A.; Hertel, J.; Olmsted-Kramer, L.C. The effect of a 4-week comprehensive rehabilitation program on postural control and lower extremity function in individuals with chronic ankle instability. J. Orthop. Sports Phys. Ther. 2007, 37, 303–311. [Google Scholar] [CrossRef]
- Wright, C.J.; Linens, S.W.; Cain, M.S. A randomized controlled trial comparing rehabilitation efficacy in chronic ankle instability. J. Sport Rehabil. 2017, 26, 238–249. [Google Scholar] [CrossRef]
- Loudon, J.K.; Santos, M.J.; Franks, L.; Liu, W. The effectiveness of active exercise as an intervention for functional ankle instability: A systematic review. Sports Med. 2008, 38, 553–563. [Google Scholar] [CrossRef]
- Sung, Y.B.; Lee, J.H.; Park, Y.H. Effects of thoracic mobilization and manipulation on function and mental state in chronic lower back pain. J. Phys. Ther. Sci. 2014, 26, 1711–1714. [Google Scholar] [CrossRef]
- Walsh, B.M.; Bain, K.A.; Gribble, P.A.; Hoch, M.C. Exercise-based rehabilitation and manual therapy compared with exercise-based rehabilitation alone in the treatment of chronic ankle instability: A critically appraised topic. J. Sport Rehabil. 2020, 1–5. [Google Scholar] [CrossRef]
- Delahunt, E.; Coughlan, G.F.; Caulfield, B.; Nightingale, E.J.; Lin, C.W.; Hiller, C.E. Inclusion criteria when investigating insufficiencies in chronic ankle instability. Med. Sci. Sports Exerc. 2010, 42, 2106–2121. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Academic Press: Cambridge, MA, USA, 2013. [Google Scholar]
- Kim, J.; Shin, W. How to do random allocation (randomization). Clin. Orthop. Surg. 2014, 6, 103–109. [Google Scholar] [CrossRef]
- Marrón-Gómez, D.; Rodríguez-Fernández, Á.L.; Martín-Urrialde, J.A. The effect of two mobilization techniques on dorsiflexion in people with chronic ankle instability. Phys. Ther. Sport 2015, 16, 10–15. [Google Scholar] [CrossRef]
- Kaminski, T.W.; Buckley, B.D.; Powers, M.E.; Hubbard, T.J.; Ortiz, C. Effect of strength and proprioception training on eversion to inversion strength ratios in subjects with unilateral functional ankle instability. Br. J. Sports Med. 2003, 37, 410–415. [Google Scholar] [CrossRef]
- Kitaoka, H.B.; Alexander, I.J.; Adelaar, R.S.; Nunley, J.A.; Myerson, M.S.; Sanders, M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1997, 18, 187–188. [Google Scholar] [CrossRef]
- Boonstra, A.M.; Schiphorst Preuper, H.R.; Reneman, M.F.; Posthumus, J.B.; Stewart, R.E. Reliability and validity of the visual analogue scale for disability in patients with chronic musculoskeletal pain. Int. J. Rehabil. Res. 2008, 31, 165–169. [Google Scholar] [CrossRef] [PubMed]
- Wylde, V.; Palmer, S.; Learmonth, I.D.; Dieppe, P. Test-retest reliability of Quantitative Sensory Testing in knee osteoarthritis and healthy participants. Osteoarthr. Cartil. 2011, 19, 655–658. [Google Scholar] [CrossRef] [PubMed]
- Yeo, H.K.; Wright, A. Hypoalgesic effect of a passive accessory mobilisation technique in patients with lateral ankle pain. Man. Ther. 2011, 16, 373–377. [Google Scholar] [CrossRef]
- Konor, M.M.; Morton, S.; Eckerson, J.M.; Grindstaff, T.L. Reliability of three measures of ankle dorsiflexion range of motion. Int. J. Sports Phys. Ther. 2012, 7, 279–287. [Google Scholar]
- Swanenburg, J.; de Bruin, E.D.; Favero, K.; Uebelhart, D.; Mulder, T. The reliability of postural balance measures in single and dual tasking in elderly fallers and non-fallers. BMC Musculoskelet. Disord. 2008, 9, 162. [Google Scholar] [CrossRef]
- Palazzo, F.; Caronti, A.; Lebone, P.; Proietti, A.; Panzarino, M.; Annino, G. Effects of stimulating surface during static upright posture in the elderly. Somatosens. Mot. Res. 2015, 32, 61–66. [Google Scholar] [CrossRef]
- Kearney, R.S.; McGuinness, K.R.; Achten, J.; Costa, M.L. A systematic review of early rehabilitation methods following a rupture of the Achilles tendon. Physiotherapy 2012, 98, 24–32. [Google Scholar] [CrossRef]
- Brown, A.J.; Shimozono, Y.; Hurley, E.T.; Kennedy, J.G. Arthroscopic repair of lateral ankle ligament for chronic lateral ankle instability: A systematic review. Arthroscopy 2018, 34, 2497–2503. [Google Scholar] [CrossRef]
- Lubbe, D.; Lakhani, E.; Brantingham, J.W.; Parkin-Smith, G.F.; Cassa, T.K.; Globe, G.A.; Korporaal, C. Manipulative therapy and rehabilitation for recurrent ankle sprain with functional instability: A short-term, assessor-blind, parallel-group randomized trial. J. Manipul. Physiol. Ther. 2015, 38, 22–34. [Google Scholar] [CrossRef]
- Flynn, T.W.; Fritz, J.M.; Wainner, R.S.; Whitman, J.M. The audible pop is not necessary for successful spinal high-velocity thrust manipulation in individuals with low back pain. Arch. Phys. Med. Rehabil. 2003, 84, 1057–1060. [Google Scholar] [CrossRef]
- Willems, T.; Witvrouw, E.; Verstuyft, J.; Vaes, P.; De Clercq, D. Proprioception and muscle strength in subjects with a history of ankle sprains and chronic instability. J. Athl. Train. 2002, 37, 487–493. [Google Scholar]
- McCann, R.S.; Crossett, I.D.; Terada, M.; Kosik, K.B.; Bolding, B.A.; Gribble, P.A. Hip strength and star excursion balance test deficits of patients with chronic ankle instability. J. Sci. Med. Sport 2017, 20, 992–996. [Google Scholar] [CrossRef]
- Hiller, C.E.; Kilbreath, S.L.; Refshauge, K.M. Chronic ankle instability: Evolution of the model. J. Athl. Train. 2011, 46, 133–141. [Google Scholar] [CrossRef]
- Donovan, L.; Hertel, J. A new paradigm for rehabilitation of patients with chronic ankle instability. Phys. Sportsmed. 2012, 40, 41–51. [Google Scholar] [CrossRef]
- Cruz-Díaz, D.; Lomas Vega, R.; Osuna-Pérez, M.C.; Hita-Contreras, F.; Martínez-Amat, A. Effects of joint mobilization on chronic ankle instability: A randomized controlled trial. Disabil. Rehabil. 2015, 37, 601–610. [Google Scholar] [CrossRef]
- Hoch, M.C.; McKeon, P.O. Joint mobilization improves spatiotemporal postural control and range of motion in those with chronic ankle instability. J. Orthop. Res. 2011, 29, 326–332. [Google Scholar] [CrossRef]
- Hall, E.A.; Chomistek, A.K.; Kingma, J.J.; Docherty, C.L. Balance- and strength-training protocols to improve chronic ankle instability deficits, part I: Assessing clinical outcome measures. J. Athl. Train. 2018, 53, 568–577. [Google Scholar] [CrossRef]
- Holt, K.R.; Haavik, H.; Lee, A.C.; Murphy, B.; Elley, C.R. Effectiveness of chiropractic care to improve sensorimotor function associated with falls risk in older people: A randomized controlled trial. J. Manipul. Physiol. Ther. 2016, 39, 267–278. [Google Scholar] [CrossRef]
| Intervention Group (n = 16) | Control Group (n = 15) | p-Value | |
|---|---|---|---|
| Age (y) | 13.88 ± 1.54 | 14.27 ± 1.49 | 0.478 |
| Affected Side (%) | |||
| Rt | 32.3 | 29.0 | 0.886 |
| Lt | 19.4 | 19.4 | |
| Height (cm) | 166.54 ± 9.60 | 169.49 ± 7.82 | 0.359 |
| Weight (kg) | 67.68 ± 13.80 | 71.18 ± 16.69 | 0.529 |
| Body Mass Index (kg/m2) | 24.18 ± 3.25 | 24.50 ± 4.04 | 0.807 |
| Career (y) | 3.75 ± 2.27 | 4.17 ± 2.31 | 0.616 |
| Pre a | Post a | Within Group b | Between Groups b | p-Value (T*G) | ||
|---|---|---|---|---|---|---|
| Effect Size | Mean (CI) | |||||
| AOFAS Score-total | ||||||
| Intervention Group | 65.06 ± 8.42 | 83.88 ± 12.20 | 1.74 | −18.82 ††† (−25.59, −12.03) | −13.49 ‡‡ (−21.52, −5.44) | 0.002 ** |
| Control Group | 62.60 ± 8.76 | 67.93 ± 7.80 | 0.64 | −5.33 † (−10.11, −0.55) | ||
| AOFAS Score-pain | ||||||
| Intervention Group | 27.50 ± 4.47 | 34.38 ± 6.29 | 1.23 | −6.88 ††† (−9.43, −4.32) | −8.21 ‡‡ (−11.86, −4.55) | <0.001 *** |
| Control Group | 28.00 ± 4.14 | 26.67 ± 4.88 | 0.29 | 1.33 (−1.53, 4.19) | ||
| AOFAS Score-function | ||||||
| Intervention Group | 37.56 ± 6.21 | 45.50 ± 3.86 | 1.46 | −7.94 †† (−12.00, −3.88) | −1.27 (−6.48, 3.93) | 0.621 |
| Control Group | 34.60 ± 5.84 | 41.27 ± 4.86 | 1.23 | −6.67 †† (−10.24, −3.09) | ||
| AOFAS Score-alignment | ||||||
| Intervention Group | 0.00 ± 0.00 | 4.00 ± 4.13 | 0.97 | −4.00 † (−6.20, −1.80) | −4.00 ‡‡ (−6.18, −1.82) | 0.001 ** |
| Control Group | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.00 | 0.00 (0.00, 0.00) | ||
| Pre a | Post a | Within Group b | Between Groups b | p-Value (T*G) | ||
|---|---|---|---|---|---|---|
| Effect Size | Mean (CI) | |||||
| VAS-Resting Pain | ||||||
| Intervention Group | 11.44 ± 10.39 | 1.25 ± 3.42 | −1.11 | 10.19 †† (4.59, 15.78) | 10.99 ‡‡ (3.08, 18.89) | 0.008 ** |
| Control Group | 7.00 ± 11.08 | 7.80 ± 10.75 | 0.073 | −0.8 (−6.91, 5.31) | ||
| VAS-Movement Pain | ||||||
| Intervention Group | 40.63 ± 10.13 | 7.94 ± 12.21 | −2.89 | 32.69 ††† (25.91, 39.46) | 26.56 ‡‡‡ (16.84, 36.40) | <0.001 *** |
| Control Group | 37.53 ± 19.06 | 31.46 ± 19.07 | −0.32 | 6.13 (−1.64, 13.77) | ||
| PPT | ||||||
| Intervention Group | 5.20 ± 2.50 | 6.14 ± 2.05 | 0.41 | −0.94 (−2.02, 0.14) | −0.13 (−1.84, 1.59) | 0.883 |
| Control Group | 5.90 ± 1.89 | 6.71 ± 2.26 | 0.39 | −0.81 (−2.27, 0.64) | ||
| Pre a | Post a | Within Group b | BetweenGroups b | p-Value(T*G) | ||
|---|---|---|---|---|---|---|
| Effect Size | Mean (CI) | |||||
| Dorsiflexion | ||||||
| Intervention Group | 34.26 ± 8.28 | 41.02 ± 4.97 | 0.94 | −6.76 †† (−11.30, −2.21) | −7.15 ‡‡‡ (−12.05, −2.23) | 0.006 ** |
| Control Group | 32.59 ± 4.04 | 32.20 ± 5.31 | −0.08 | 0.39 (−1.73, 2.51) | ||
| Plantar Flexion | ||||||
| Intervention Group | 30.89 ± 11.36 | 29.85 ± 7.55 | −0.10 | 1.04 (−3.09, 5.18) | −0.52 (−7.36, 6.33) | 0.879 |
| Control Group | 28.82 ± 8.51 | 27.26 ± 6.29 | −0.20 | 1.56 (−4.39, 7.50) | ||
| Inversion | ||||||
| Intervention Group | 43.98 ± 8.82 | 47.67 ± 6.49 | 0.47 | −3.69 (−7.64, 0.26) | −4.63 (−10.07, 0.81) | 0.092 |
| Control Group | 40.01 ± 8.67 | 39.07 ± 7.19 | −0.12 | 0.94 (−3.15, 5.02) | ||
| Eversion | ||||||
| Intervention Group | 23.85 ± 6.38 | 28.12 ± 8.38 | 0.56 | −4.27 †† (−6.96, −1.58) | −4.27 ‡‡ (−7.79, −0.53) | 0.026 * |
| Control Group | 22.15 ± 6.29 | 22.26 ± 5.60 | 0.02 | 0.00 (−2.78, 2.56) | ||
| Pre a | Post a | Within Group b | Between Groups b | p-Value (T*G) | ||
|---|---|---|---|---|---|---|
| Effect Size | Mean (CI) | |||||
| Bipedal Stance | ||||||
| Area (cm2) | ||||||
| Intervention Group | 1.83 ± 1.88 | 1.67 ± 1.44 | −0.09 | 0.16 (−1.15, 1.47) | 0.61 (−0.79, 2.01) | 0.381 |
| Control Group | 1.25 ± 0.87 | 1.70 ± 1.22 | 0.41 | −0.45 (−1.02, 0.12) | ||
| Path Length (cm) | ||||||
| Intervention Group | 12.41 ± 3.39 | 11.77 ± 1.77 | −0.22 | 0.70 (−0.90, 2.19) | 1.80 (−0.22, 3.66) | 0.080 |
| Control Group | 10.69 ± 2.75 | 11.77 ± 2.60 | 0.40 | −1.10 (−2.36, 0.21) | ||
| Velocity (cm/s) | ||||||
| Intervention Group | 1.24 ± 0.34 | 1.18 ± 0.18 | −0.20 | 0.06 (−0.09, 0.22) | 0.17 (−0.02, 0.37) | 0.079 |
| Control Group | 1.07 ± 0.28 | 1.18 ± 0.26 | 0.40 | −0.11 (−0.24, 0.02) | ||
| APSD | ||||||
| Intervention Group | 0.16 ± 0.09 | 0.18 ± 0.10 | 0.21 | −0.02 (−0.10, 0.05) | 0.03 (−0.06, 0.12) | 0.542 |
| Control Group | 0.15 ± 0.09 | 0.20 ± 0.08 | 0.59 | −0.05 (−0.10, 0.01) | ||
| LRSD | ||||||
| Intervention Group | 0.17 ± 0.11 | 0.14 ± 0.07 | −0.31 | 0.03 (−0.02, 0.09) | 0.03 (−0.05, 0.13) | 0.338 |
| Control Group | 0.11 ± 0.05 | 0.11 ± 0.12 | 0.00 | 0.00 (−0.08, 0.06) | ||
| Unipedal Stance | ||||||
| Area (cm2) | ||||||
| Intervention Group | 8.93 ± 3.74 | 7.67 ± 2.69 | −0.38 | 1.26 (−0.65, 3.15) | 0.12 (−2.56, 2.80) | 0.928 |
| Control Group | 7.46 ± 4.20 | 6.32 ± 2.72 | −0.30 | 1.14 (−0.93, 3.21) | ||
| Path Length (cm) | ||||||
| Intervention Group | 51.79 ± 11.83 | 40.49 ± 11.51 | −0.97 | 11.30 †† (4.73, 17.88) | 9.90 ‡‡ (3.11, 16.83) | 0.006 ** |
| Control Group | 47.90 ± 12.49 | 46.56 ± 12.56 | −0.11 | 1.40 (−0.96, 3.63) | ||
| Velocity (cm/s) | ||||||
| Intervention Group | 5.18 ± 1.18 | 4.05 ± 1.15 | −0.97 | 1.13 †† (0.47, 1.79) | 1.00 ‡‡ (0.31, 1.68) | 0.006 ** |
| Control Group | 4.79 ± 1.25 | 4.66 ± 1.26 | −0.11 | 0.13 (−0.10, 0.37) | ||
| APSD | ||||||
| Intervention Group | 0.46 ± 0.17 | 0.32 ± 0.10 | −0.95 | 0.14 † (0.03, 0.24) | 0.10 (−0.04, 0.24) | 0.140 |
| Control Group | 0.41 ± 0.19 | 0.37 ± 0.11 | −0.24 | 0.04 (−0.06, 0.14) | ||
| LRSD | ||||||
| Intervention Group | 0.45 ± 0.19 | 0.36 ± 0.11 | −0.55 | 0.09 (−0.01, 0.20) | 0.08 (−0.11, 0.27) | 0.392 |
| Control Group | 0.43 ± 0.19 | 0.42 ± 0.20 | −0.05 | 0.01 (−0.16, 0.19) | ||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shin, H.-J.; Kim, S.-H.; Jung, H.J.; Cho, H.-y.; Hahm, S.-C. Manipulative Therapy Plus Ankle Therapeutic Exercises for Adolescent Baseball Players with Chronic Ankle Instability: A Single-Blinded Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2020, 17, 4997. https://doi.org/10.3390/ijerph17144997
Shin H-J, Kim S-H, Jung HJ, Cho H-y, Hahm S-C. Manipulative Therapy Plus Ankle Therapeutic Exercises for Adolescent Baseball Players with Chronic Ankle Instability: A Single-Blinded Randomized Controlled Trial. International Journal of Environmental Research and Public Health. 2020; 17(14):4997. https://doi.org/10.3390/ijerph17144997
Chicago/Turabian StyleShin, Ho-Jin, Sung-Hyeon Kim, Han Jo Jung, Hwi-young Cho, and Suk-Chan Hahm. 2020. "Manipulative Therapy Plus Ankle Therapeutic Exercises for Adolescent Baseball Players with Chronic Ankle Instability: A Single-Blinded Randomized Controlled Trial" International Journal of Environmental Research and Public Health 17, no. 14: 4997. https://doi.org/10.3390/ijerph17144997
APA StyleShin, H.-J., Kim, S.-H., Jung, H. J., Cho, H.-y., & Hahm, S.-C. (2020). Manipulative Therapy Plus Ankle Therapeutic Exercises for Adolescent Baseball Players with Chronic Ankle Instability: A Single-Blinded Randomized Controlled Trial. International Journal of Environmental Research and Public Health, 17(14), 4997. https://doi.org/10.3390/ijerph17144997







