Healthcare Workers and Manual Patient Handling: A Pilot Study for Interdisciplinary Training
Abstract
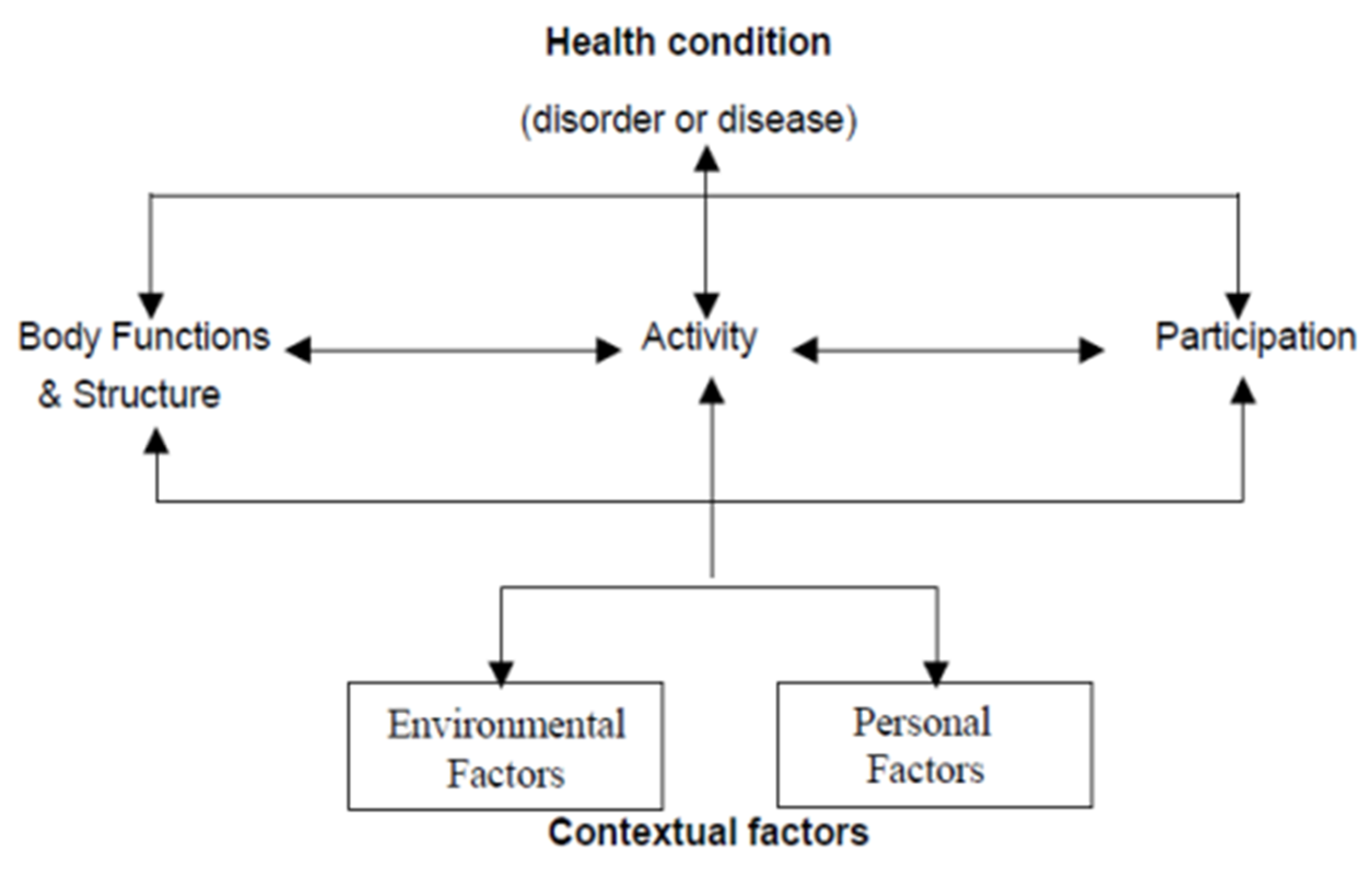
1. Introduction
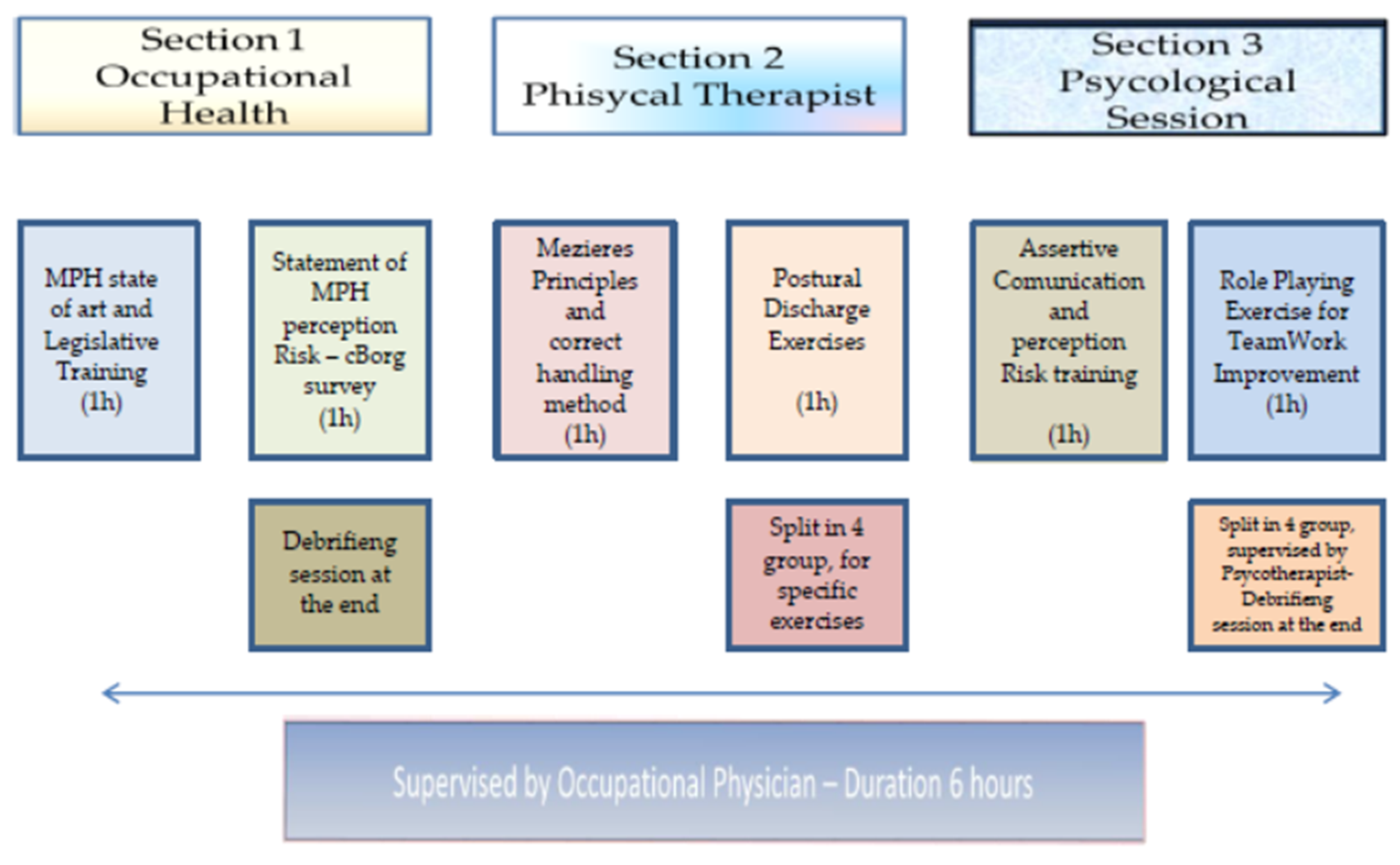
2. Methods
2.1. Setting and Study Design
2.2. Training Model Evaluation
2.3. Ethics
2.4. Statistical Analysis
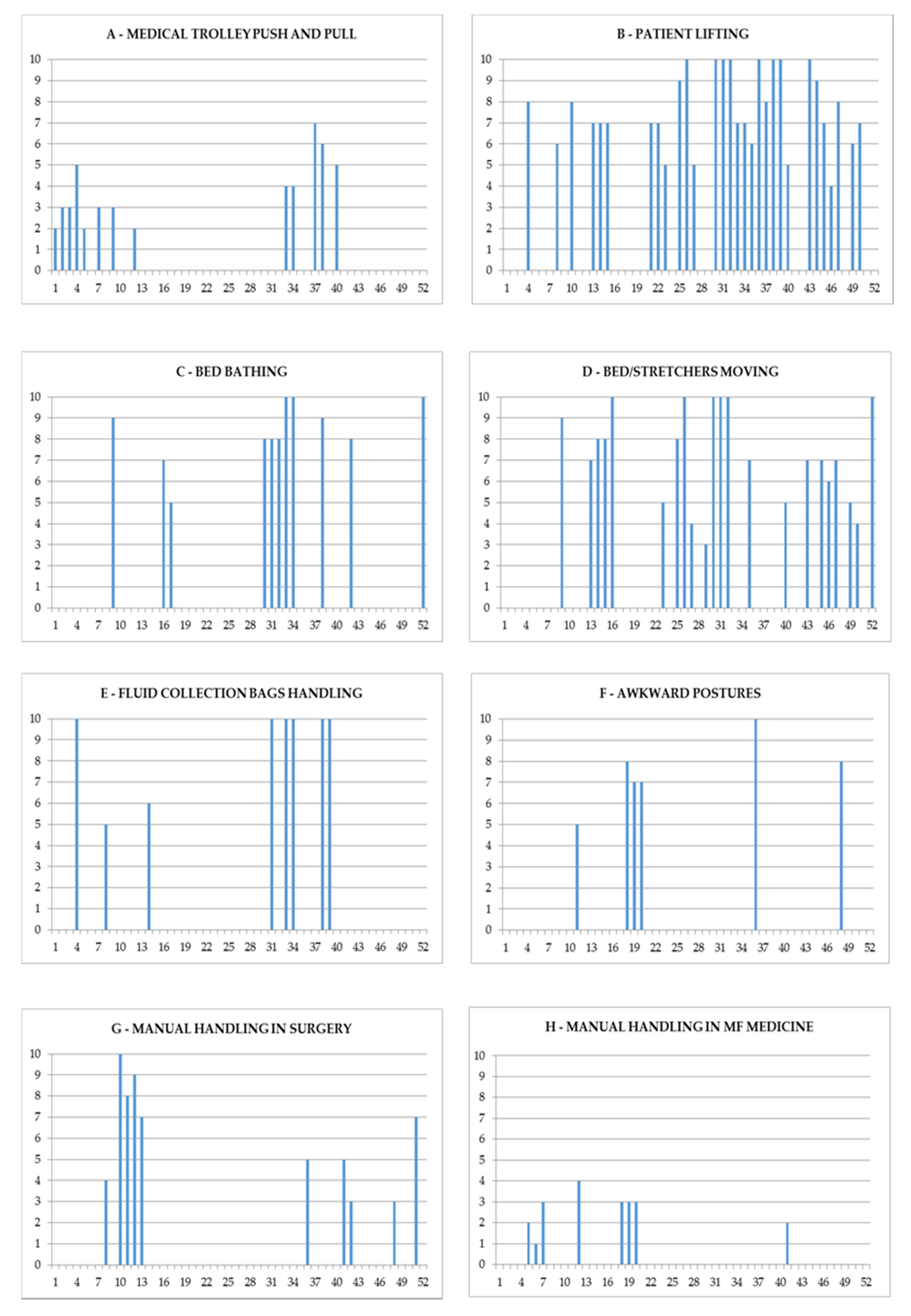
3. Results
3.1. Training Program—Occupational Medicine Section
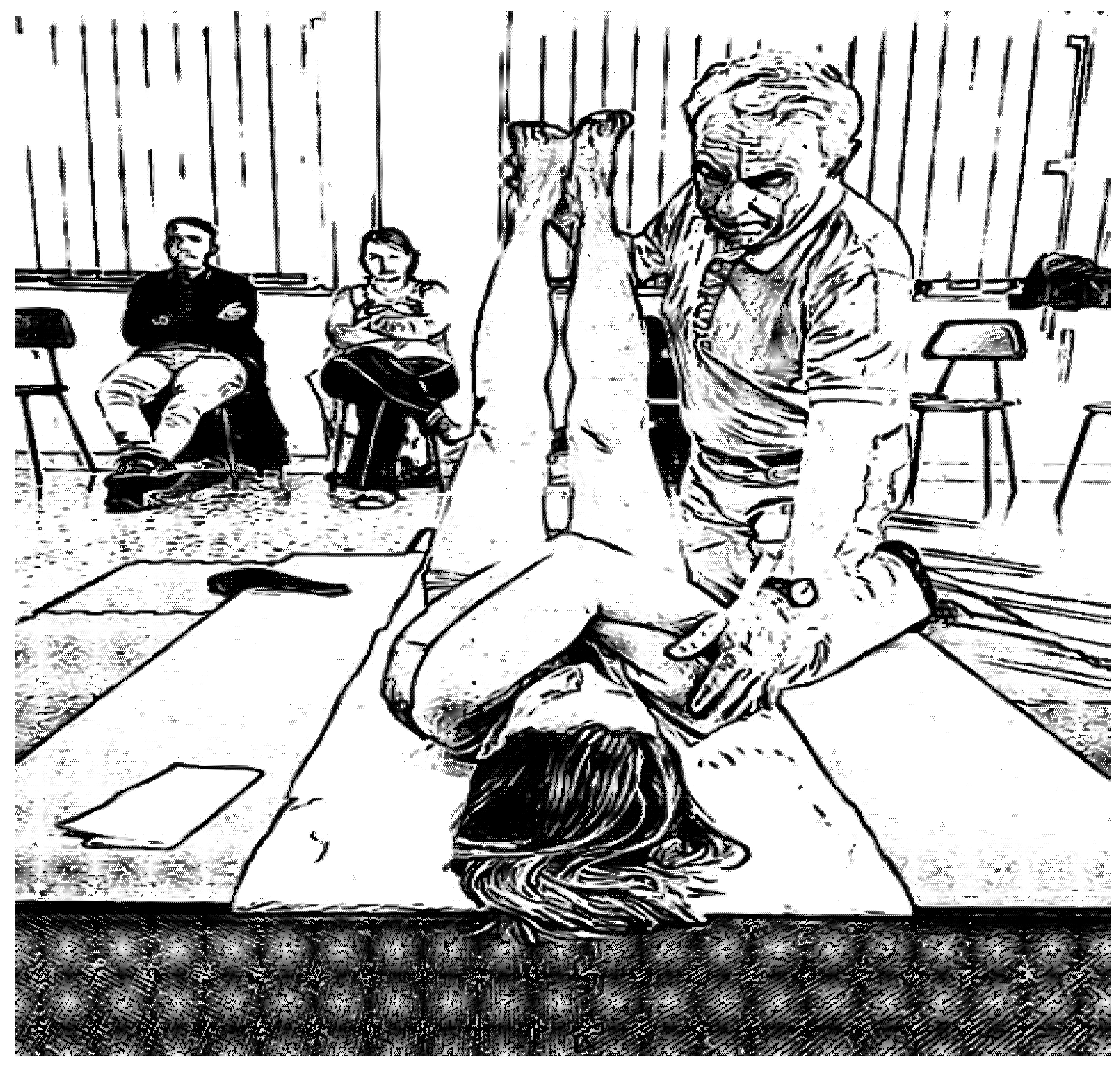
3.2. Training Program—Physiotherapy Section
3.3. Training Program—Psychological Section
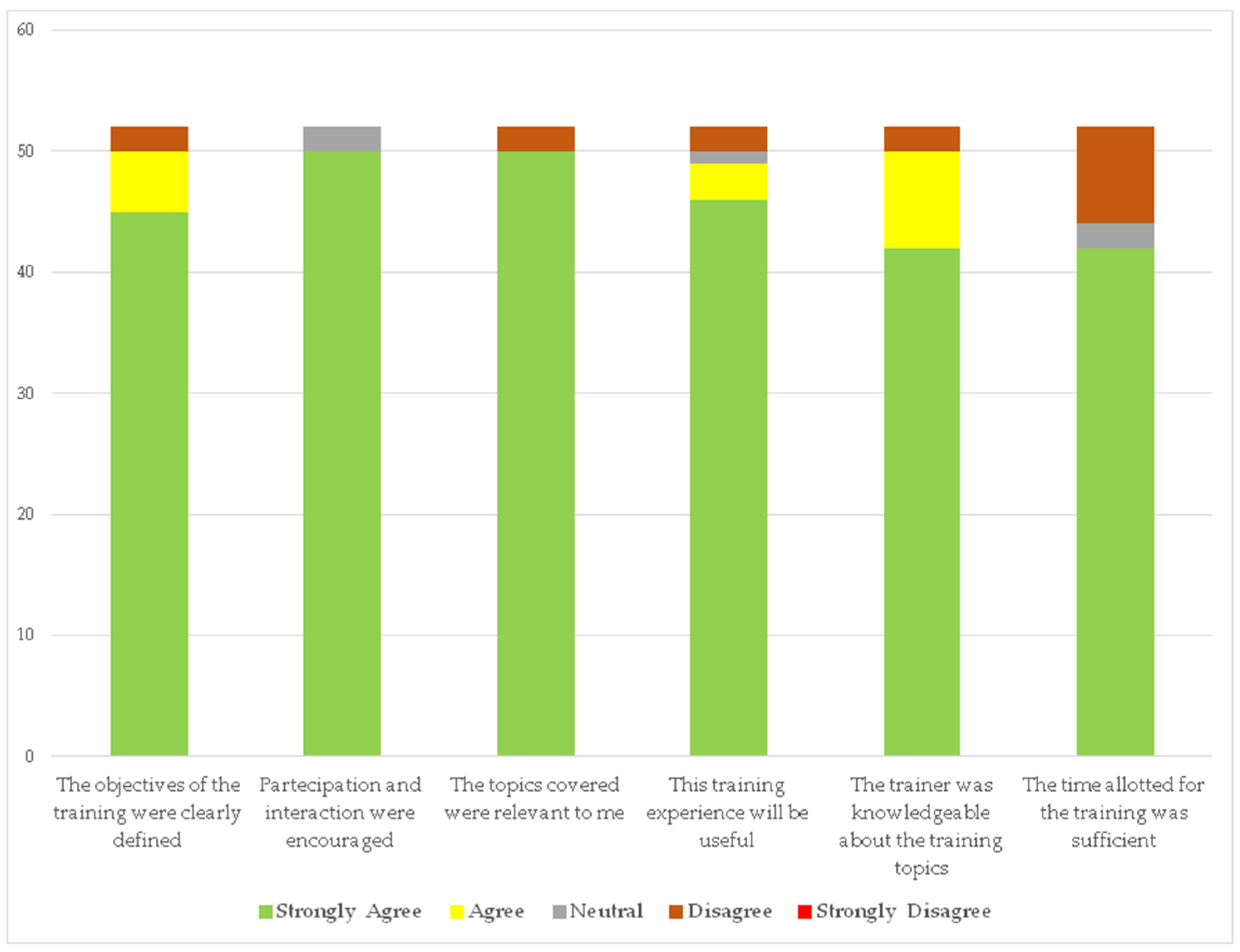
3.4. End of Course Evaluation
4. Discussion
4.1. Training Program—Occupational Medicine Section
4.2. Training Program—Physiotherapy Section
4.3. Training Program—Psychological Section
4.4. Strenght and Weaknesses
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| HCW | health care workers |
| LBP | low back pain |
| MPH | manual patient handling |
| WRMSDs | work-related musculoskeletal diseases |
| SPH | safe patient handling |
| WHO | World Health Organization |
References
- Eurofound. Sixth European Working Conditions Survey—Overview Report; Publications Office of the European Union: Brussels, Belgium; Luxembourg, 2017.
- Davis, K.G.; Kotowski, S.E. Prevalence of musculoskeletal disorders for nurses in hospitals, long-term care facilities, and home health care: A comprehensive review. Hum. Factors 2015, 57, 754–792. [Google Scholar] [CrossRef] [PubMed]
- Van Hoof, W.; O’Sullivan, K.; O’Keeffe, M.; Verschueren, S.; O’Sullivan, P.; Dankaerts, W. The Efficacy of Interventions for Low Back Pain in Nurses: A Systematic Review. Int. J. Nurs. Stud. 2018, 77, 222–231. [Google Scholar] [CrossRef] [PubMed]
- Alnaami, I.; Awadalla, N.J.; Alkhairy, M.; Alburidy, S.; Alqarni, A.; Algarni, A.; Alshehri, R.; Amrah, B.; Alasmari, M.; Mahfouz, A.A. Prevalence and factors associated with low back pain among health care workers in southwestern Saudi Arabia. BMC Musculoskelet. Disord. 2019, 20, 56. [Google Scholar] [CrossRef]
- Al Dajah, S.; Al Daghdi, A. Prevalence and risk factors of low back pain among nurses in Sudayr region. ESJ 2013, 9, 198–205. [Google Scholar]
- International Organization for Standardization. Ergonomics—Manual Handling of People in the Healthcare Sector. Iso/TR Document 12296; International Organization for Standardization: Geneva, Switzerland, 2012. [Google Scholar]
- Hegewald, J.; Berge, W.; Heinrich, P.; Staudte, R.; Freiberg, A.; Scharfe, J.; Girbig, M.; Nienhaus, A.; Seidler, A. Do Technical Aids for Patient Handling Prevent Musculoskeletal Complaints in Health Care Workers?—A Systematic Review of Intervention Studies. Int. J. Environ. Res. Public Health 2018, 15, 476. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. International Classification of Functioning, Disability and Health, WHO Library Cataloguing-in-Publication Data International Classification of Functioning, Disability and Health: ICF; World Health Organization: Geneva, Switzerland, 2007; ISBN 92 4 154542 9. [Google Scholar]
- Olkowski, B.F.; Stolfi, A.M. Safe Patient Handling Perceptions and Practices: A Survey of Acute Care Physical Therapists. Phys. Ther. 2014, 94, 682–695. [Google Scholar] [CrossRef] [PubMed]
- Genaidy, A.M.; Mital, A.; Bafna, K.M. An endurance training programme for frequent manual carrying tasks. Ergonomics 1989, 32, 149–155. [Google Scholar] [CrossRef]
- De Castro, A.B.; Hagan, P.; Nelson, A. Prioritising safe patient handling: The American Nurses Association’s Handle with Care Campaign. J. Nurs. Adm. 2006, 36, 363–369. [Google Scholar] [CrossRef]
- Clemes, S.A.; Haslam, C.O.; Haslam, R.A. What constitutes effective manual handling training? A systematic review. Occup. Med. 2010, 60, 101–107. [Google Scholar] [CrossRef]
- Vendittelli, D.; Penprase, B.; Pittiglio, L. Musculoskeletal injury prevention for new nurses. Work. Health Saf. 2016, 64, 573–585. [Google Scholar] [CrossRef]
- Lee, S.J.; Faucett., J.; Gillen., M.; Krause, N.; Landry, L. Factors associated with safe patient handling behaviors among critical care nurses. Am. J. Ind. Med. 2010, 53, 886–897. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.J.; Lee, J.H. Safe patient handling behaviors and lift use among hospital nurses: A cross-sectional study. Int. J. Nurs. Stud. 2017, 74, 53–60. [Google Scholar] [CrossRef] [PubMed]
- D’Arcy, L.P.; Sasai, Y.; Stearns, S.C. Do assistive devices, training, and workload affect injury incidence? Prevention efforts by nursing homes and back injuries among nursing assistants. J. Adv. Nurs. 2012, 68, 836–845. [Google Scholar]
- Thomas, D.R.; Thomas, Y.L.N. Interventions to reduce injuries when transferring patients: A critical appraisal of reviews and a realist synthesis. Int. J. Nurs. Stud. 2014, 51, 1381–1394. [Google Scholar] [CrossRef]
- Carta, A.; Parmigiani, F.; Roversi, A.; Rossato, R.; Milini, C.; Parrinello, G.; Apostoli, P.; Alessio, L.; Porru, S. Training in safer and healthier patient handling techniques. Br. J. Nurs. 2010, 19, 576–582. [Google Scholar] [CrossRef]
- Taulaniemi, A.; Kankaanpää, M.; Rinne, M.; Tokola, K.; Parkkari, J.; Suni, J.H. Fear-avoidance beliefs are associated with exercise adherence: Secondary analysis of a randomised controlled trial (RCT) among female healthcare workers with recurrent low back pain. BMC Sports Sci. Med. Rehabil. 2020, 12, 28. [Google Scholar] [CrossRef]
- Resnick, M.; Sanchez, R. Reducing patient handling injuries through contextual training. J. Emerg. Nurs. 2009, 35, 504–508. [Google Scholar] [CrossRef]
- Nastasia, I.; Lortie, M.; Delisle, A.; Gagnon, M. Perception and Biomechanics Data in a Manual Handling Task: A Comparative Study. Ergonomics 2007, 50, 2059–2081. [Google Scholar] [CrossRef]
- Paul, D. Metodo di Movimentazione del Malat; Piccin: Padua, Italy, October 2008; ISBN 978-88-299-1963-5. [Google Scholar]
- Mann, K.; Gordon, J.; MacLeod, A. Reflection and reflective practice in health professions education: A systematic review. Adv. Health Sci. Educ. 2009, 14, 595–621. [Google Scholar] [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Ann. Intern. Med. 2007, 147, 573–577. [Google Scholar] [CrossRef]
- Italian Legislative Decree n.81, April 2008, Coordinated Text with Legislative Decree 3 August 2009, n. 106. Available online: https://www.ispettorato.gov.it/it-it/strumenti-e-servizi/Documents/Testo-unico-salute-sicurezza-sul-lavoro-81-08-edizione-gennaio-2020.pdf (accessed on 9 July 2020).
- Jäger, M.; Jordan, C.; Theilmeier, A.; Wortmann, N.; Kuhn, S.; Nienhaus, A.; Luttmann, A. Lumbar-Load Analysis of Manual Patient-Handling Activities for Biomechanical Overload Prevention Among Healthcare Workers. Ann. Occup. Hyg. 2013, 57, 528–544. [Google Scholar] [PubMed]
- Yoshinaga, N.; Nakamura, Y.; Tanoue, H.; MacLiam, F.; Aoishi, K.; Shiraishi, Y. Is modified brief assertiveness training for nurses effective? A single-group study with long-term follow-up. J. Nurs. Manag. 2018, 26, 59–65. [Google Scholar] [CrossRef] [PubMed]
- Ziam, S.; Laroche, E.; Lakhal, S.; Alderson, M.; Gagne, C. Application of MSD prevention practices by nursing staff working in healthcare settings. Int. J. Ind. Ergon. 2020, 77, 102959. [Google Scholar] [CrossRef]
- Skotte, J.H.; Essendrop, M.; Hansen, A.F.; Schibye, B. A dynamic 3D biomechanical evaluation of the load on the low back during different patient-handling tasks. J. Biomech. 2002, 35, 1357–1366. [Google Scholar] [CrossRef]
- Salmani Nodooshan, H.; Choobineh, A.; Razeghi, M.; Shahnazar Nezhad Khales, T. Designing, prototype making and evaluating a mechanical aid device for patient transfer between bed and stretcher. Int. J. Occup. Saf. Ergon. 2017, 23, 491–500. [Google Scholar] [CrossRef] [PubMed]
- Kang, M.H.; Choi, S.H.; Oh, J.S. Postural taping applied to the low back influences kinematics and EMG activity during patient transfer in physical therapists with chronic low back pain. J. Electromyogr. Kinesio. 2013, 23, 787–793. [Google Scholar] [CrossRef]
- Jordan, C.; Luttmann, A.; Theilmeier, A.; Kuhn, S.; Wortmann, N.; Jäger, M. Characteristic values of the lumbar load of manual patient handling for the application in workers’ compensation procedures. J. Occup. Med. Toxicol. 2011, 6, 17. [Google Scholar] [CrossRef]
- Smedley, J.; Trevelyan, F.; Inskip, H.; Buckle, P.; Cooper, C.; Coggon, D. Impact of ergonomic intervention on back pain among nurses. Scand. J. Work Environ. Health 2003, 29, 117–123. [Google Scholar] [CrossRef]
- Garg, A.; Kapellusch, J.M. Long-term efficacy of an ergonomics program that includes patient-handling devices on reducing musculoskeletal injuries to nursing personnel. Hum. Factors: J. Hum. Factors Ergon. Soc. 2012, 54, 608–625. [Google Scholar] [CrossRef]
- Kuijer, P.P.; Verbeek, J.H.; Visser, B.; Elders, L.A.; Van Roden, N.; Van den Wittenboer, M.E.; Lebbink, M.; Burdorf, A.; Hulshof, C.T. An evidence-based multidisciplinary practice guideline to reduce the workload due to lifting for preventing work-related low back pain. Ann. Occup. Environ. Med. 2014, 26, 16. [Google Scholar] [CrossRef]
- Nelson, A.; Baptiste, A.S. Evidence-based practices for safe patient handling and movement. Online J. Issues Nurs. 2004, 9, 4. [Google Scholar]
- Krill, C.; Raven, C.; Staffileno, B.A. Moving from a clinical question to research: The implementation of a safe patient handling program. Medsurg Nurs. 2012, 21, 104–116. [Google Scholar] [PubMed]
- Dawson, A.P.; McLennan, S.N.; Schiller, S.D.; Jull, G.A.; Hodges, P.W.; Stewart, S. Interventions to prevent back pain and back injury in nurses: A systematic review. Occup. Environ. Med. 2007, 64, 642–650. [Google Scholar] [CrossRef] [PubMed]
- Seo, D.C. An explicative model of unsafe work behavior. Saf. Sci. 2005, 43, 187–211. [Google Scholar] [CrossRef]
- Felknor, S.A.; Aday, L.A.; Burau, K.D.; Delclos, G.L.; Kapadia, A.S. Safety climate and its association with injuries and safety practices in public hospitals in Costa Rica. Int. J. Occup. Environ. Health 2000, 6, 18–25. [Google Scholar] [CrossRef] [PubMed]
- Rønning, S.B.; Bjørkly, S. The use of clinical role-play and reflection in learning therapeutic communication skills in mental health education: An integrative review. Adv. Med. Educ. Pract. 2019, 10, 415–425. [Google Scholar] [CrossRef] [PubMed]
- Daniels, K.; Auguste, T. Moving Forward in Patient Safety: Multidisciplinary Team Training. Semin. Perinatol. 2013, 37, 146–150. [Google Scholar] [CrossRef]
- De Oliveira Sato, T.; Ferreira Faisting, A.L. Effectiveness of ergonomic training to reduce physical demands and musculoskeletal symptoms—An overview of systematic reviews. Int. J. Ind. Ergon. 2019, 74, 102845. [Google Scholar]
- Novack, D.H.; Suchman, A.L.; Clark, W.; Epstein, R.M.; Najberg, E.; Kaplan, C. Calibrating the physician. Personal awareness and effective patient care. Working Group on Promoting Physician Personal Awareness, American Academy on Physician and Patient. JAMA 1997, 278, 502–509. [Google Scholar] [CrossRef]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Garzillo, E.M.; Monaco, M.G.L.; Corvino, A.R.; D’Ancicco, F.; Feola, D.; Della Ventura, D.; Miraglia, N.; Lamberti, M. Healthcare Workers and Manual Patient Handling: A Pilot Study for Interdisciplinary Training. Int. J. Environ. Res. Public Health 2020, 17, 4971. https://doi.org/10.3390/ijerph17144971
Garzillo EM, Monaco MGL, Corvino AR, D’Ancicco F, Feola D, Della Ventura D, Miraglia N, Lamberti M. Healthcare Workers and Manual Patient Handling: A Pilot Study for Interdisciplinary Training. International Journal of Environmental Research and Public Health. 2020; 17(14):4971. https://doi.org/10.3390/ijerph17144971
Chicago/Turabian StyleGarzillo, Elpidio Maria, Maria Grazia Lourdes Monaco, Anna Rita Corvino, Francesco D’Ancicco, Daniela Feola, Dino Della Ventura, Nadia Miraglia, and Monica Lamberti. 2020. "Healthcare Workers and Manual Patient Handling: A Pilot Study for Interdisciplinary Training" International Journal of Environmental Research and Public Health 17, no. 14: 4971. https://doi.org/10.3390/ijerph17144971
APA StyleGarzillo, E. M., Monaco, M. G. L., Corvino, A. R., D’Ancicco, F., Feola, D., Della Ventura, D., Miraglia, N., & Lamberti, M. (2020). Healthcare Workers and Manual Patient Handling: A Pilot Study for Interdisciplinary Training. International Journal of Environmental Research and Public Health, 17(14), 4971. https://doi.org/10.3390/ijerph17144971






