Urinary Metal Levels after Repeated Edetate Disodium Infusions: Preliminary Findings
Abstract
1. Introduction
2. Materials and Methods
2.1. Methodology
2.2. Materials
2.3. Statistical Analyses
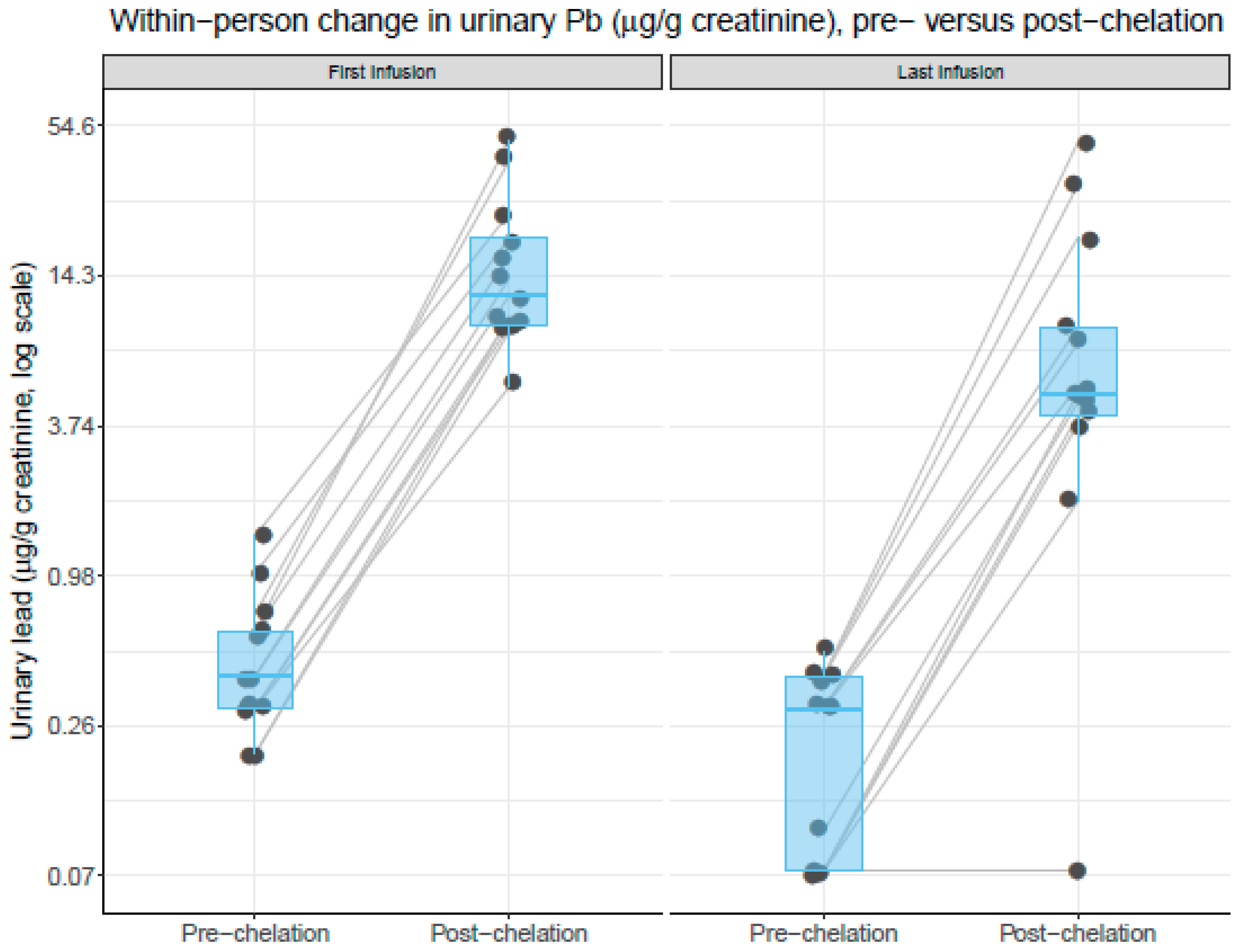
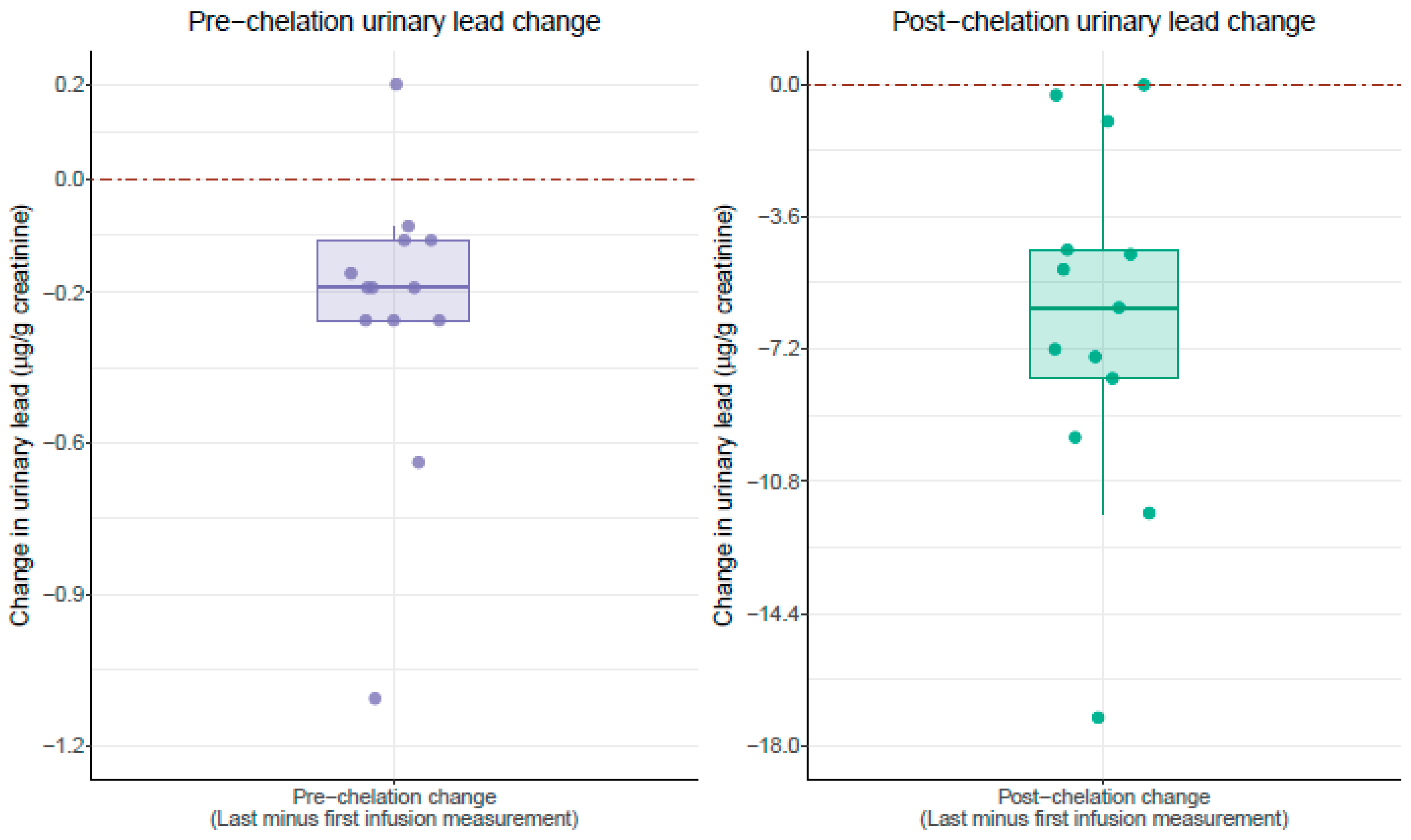
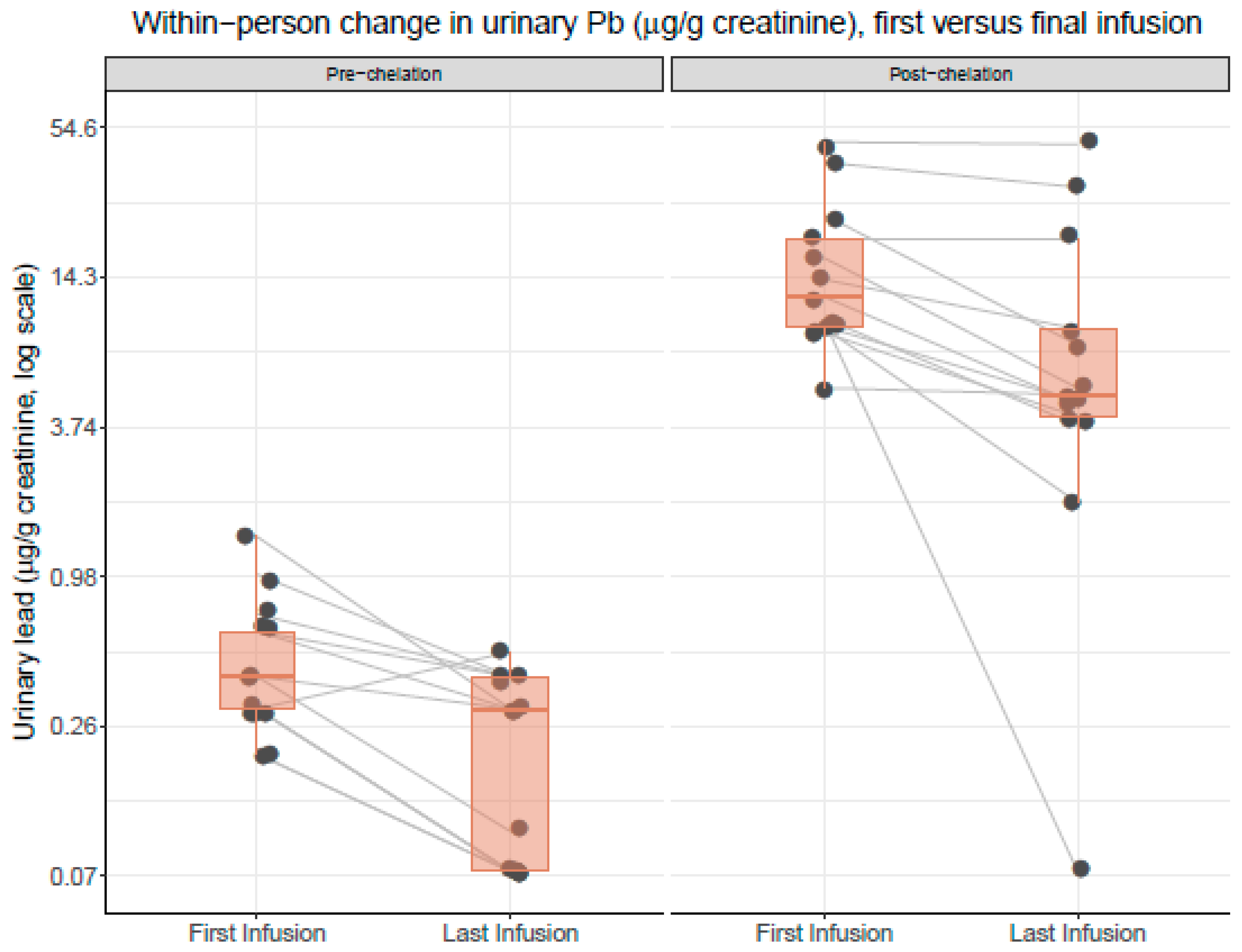
3. Results
4. Discussion
4.1. Edetate Disodium and Patient Safety
4.2. Decrease in Lead Burden
5. Conclusions
Limitations
Author Contributions
Funding
Conflicts of Interest
Data Availability Statement
Abbreviations
| TACT | Trial to Assess Chelation Therapy |
| CDC | Center for Disease Control |
| CAD | coronary artery disease |
| CLI | critical limb ischemia |
| PAD | peripheral artery disease |
| ATSDR | Agency for Toxic Substances and Disease Registry |
| MI | myocardial infarction |
References
- Lanphear, B.P.; Rauch, S.; Auinger, P.; Allen, R.W.; Hornung, R.W. Low-level lead exposure and mortality in US adults: A population-based cohort study. Lancet Public Health 2018, 3, e177–e184. [Google Scholar] [CrossRef]
- Chowdhury, R.; Ramond, A.; O’Keeffe, L.M.; Shahzad, S.; Kunutsor, S.K.; Muka, T.; Gregson, J.; Willeit, P.; Warnakula, S.; Khan, H.; et al. Environmental toxic metal contaminants and risk of cardiovascular outcomes: Systematic review and meta-analysis. BMJ 2018, 362, k3310. [Google Scholar] [CrossRef] [PubMed]
- Lamas, G.A.; Navas-Acien, A.; Mark, D.B.; Lee, K.L. Heavy Metals, Cardiovascular Disease, and the Unexpected Benefits of Chelation Therapy. J. Am. Coll. Cardiol. 2016, 67, 2411–2418. [Google Scholar] [CrossRef] [PubMed]
- Agency for Toxic Substances and Disease Registry (ATSDR). The Priority List of Hazardous Substances. Available online: https://www.atsdr.cdc.gov/ (accessed on 22 May 2019).
- Flora, S.; Mittal, M.; Mehta, A. Heavy metal induced oxidative stress and its possible reversal by chelation therapy. Indian J. Med. Res. 2008, 128, 501–523. [Google Scholar]
- Dimercaptosuccinic Acid (DMSA). A Non-Toxic, Water-Soluble Treatment For Heavy Metal Toxicity. Available online: https://wellnesspharmacy.com/wp-content/uploads/2015/01/dmsa-heavymetaltoxicity.pdf (accessed on 4 June 2019).
- Tellez-Plaza, M.; Jones, M.R.; Dominguez-Lucas, A.; Guallar, E.; Navas-Acien, A. Cadmium exposure and clinical cardiovascular disease: A systematic review. Curr. Atheroscler. Rep. 2013, 15, 356. [Google Scholar] [CrossRef]
- Ujueta, F.; Arenas, I.A.; Diaz, D.; Yates, T.; Beasley, R.; Navas-Acien, A.; Lamas, G.A. Cadmium level and severity of peripheral artery disease in patients with coronary artery disease. Eur. J. Prev. Card. 2018, 26, 1456–1458. [Google Scholar] [CrossRef]
- Arenas, I.; Ujueta, F.; Diaz, D.; Yates, T.; Olivieri, B.; Beasley, R.; Lamas, G.A. Limb Preservation Using Edetate Disodium-based Chelation in Patients with Diabetes and Critical Limb Ischemia: An Open-label Pilot Study. Cureus 2019, 11, e6477. [Google Scholar] [CrossRef]
- Ujueta, F.; Vozzi, C.; Vozzi, L. Edetate Disodium-based Treatment in a Woman with Diabetes and Critical Limb Ischemia Scheduled for Lower Extremity Amputation. Cureus 2019, 11, e6142. [Google Scholar] [CrossRef]
- Farooqui, Z.; Bakulski, K.M.; Power, M.C.; Weiddkopf, M.G.; Sparrow, D.; Spiro, A.; Vokonas, P.S.; Nie, L.H.; Hu, H.; Park, S.K. Associations of cumulative Pb exposure and longitudinal changes in Mini-Mental Status Exam scores, global cognition and domains of cognition: The VA Normative Aging Study. Environ. Res. 2017, 152, 102–108. [Google Scholar] [CrossRef]
- Vacchi-Suzzi, C.; Kruse, D.; Harrington, J.; Levine, K.; Meliker, J. Is Urinary Cadmium a Biomarker of Long-term Exposure in Humans? A Review. Curr. Environ. Health Rep. 2016, 3, 450–458. [Google Scholar] [CrossRef]
- Marsden, P. Increased Body Lead Burden—Cause or Consequence of Chronic Renal Insufficiency? N. Engl. J. Med. 2003, 348, 345–347. [Google Scholar] [CrossRef] [PubMed]
- Arenas, I.A.; Navas-Acien, A.; Ergui, I.; Lamas, G.A. Enhanced vasculotoxic metal excretion in post-myocardial infarction patients following a single edetate disodium-based infusion. Environ. Res. 2017, 158, 443–449. [Google Scholar] [CrossRef] [PubMed]
- Ying, Z.; Xu, X.; Chen, M.; Liu, D.; Zhong, M.; Chen, L.; Sun, Q.; Rajagopalan, S. A Synergistic Vascular Effect of Airborne Particulate Matter and Nickel in a Mouse Model. Toxicol. Sci. 2013, 135, 72–80. [Google Scholar] [CrossRef] [PubMed]
- Genchi, G.; Sinicropi, M.S.; Carocci, A.; Lauria, G.; Catalano, A. Mercury Exposure and Heart Diseases. Int. J. Environ. Res. Public Health 2017, 14, 74. [Google Scholar] [CrossRef] [PubMed]
- Lamas, G.A.; Goertz, C.; Boineau, R.; Mark, D.B.; Rozema, T.; Nahin, R.L.; Drisko, J.A.; Lee, K.L. Design of the Trial to Assess Chelation Therapy (TACT). Am. Heart J. 2012, 163, 7–12. [Google Scholar] [CrossRef] [PubMed]
- Diaz, D.; Fonseca, V.; Aude, Y.W.; Lamas, G.A. Chelation therapy to prevent diabetes-associated cardiovascular events. Curr. Opin. Endocrinol. Diabetes Obes. 2018, 25, 258–266. [Google Scholar] [CrossRef]
- Escolar, E.; Lamas, G.A.; Mark, D.B.; Boineau, R.; Goertz, C.; Rosenberg, Y.; Nahin, R.L.; Ouyang, P.; Rozema, T.; Magaziner, A.; et al. The effect of an EDTA-based chelation regimen on patients with diabetes mellitus and prior myocardial infarction in the Trial to Assess Chelation Therapy (TACT). Circ. Cardiovasc. Qual. Outcomes 2013, 7, 15–24. [Google Scholar] [CrossRef]
- Lamas, G.A.; Goertz, C.; Boineau, R.; Mark, D.B.; Rozema, T.; Nahin, R.L.; Lindblad, L.; Lewis, E.F.; Drisko, J.; Lee, K.L. Effect of disodium EDTA chelation regimen on cardiovascular events in patients with previous myocardial infarction: The TACT randomized trial. JAMA 2013, 309, 1241–1250. [Google Scholar] [CrossRef] [PubMed]
- Fihn, S.D.; Blankenship, J.C.; Alexander, K.P.; Bittl, J.A.; Byrne, J.G.; Fletcher, B.J.; Fonarow, G.C.; Lange, R.A.; Levine, G.N.; Maddox, T.M.; et al. 2014 ACC/AHA/AATS/PCNA/SCAI/STS Focused Update of the Guideline for the Diagnosis and Management of Patients with Stable Ischemic Heart Disease. J. Am. Coll. Cardiol. 2014, 64, 1929–1949. [Google Scholar] [CrossRef]
- Levey, A.S.; Coresh, J.; Greene, T.; Stevens, L.A.; Zhang, Y.L.; Hendriksen, S.; Kusek, J.W.; Van Lente, F. Chronic Kidney Disease Epidemiology Collaboration. Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann. Intern. Med. 2006, 145, 247–254. [Google Scholar] [CrossRef]
- Wang, X.; Mukherjee, B.; Sung, P. Does information on blood heavy metals improve cardiovascular mortality prediction? JAHA 2019, 8, e013571. [Google Scholar] [CrossRef] [PubMed]
- Colicino, E.; Just, A.; Kioumourtzoglou, M.; Vokonas, P.; Cardenas, A.; Sparrow, D.; Weissopf, M.; Nie, L.H.; Hu, H.; Schwartz, J.; et al. Blood DNA methylation biomarkers of cumulative lead exposure in adults. J. Expo. Sci. Environ. Epidemiol. 2019. [Google Scholar] [CrossRef] [PubMed]
| Pre-Chelation | Post-Chelation | |||||
|---|---|---|---|---|---|---|
| Metals | First | Final Infusion | Percent Change | p-Value | First | Final Infusion | Percent Change | p-Value |
| (µg/g of Creatinine) | (µg/g of Creatinine) | |||||
| Pb | 0.5 ± 0.4 | 0.2 ± 0.2 | −54.5% | 0.006 | 17. ± 13.0 | 11.2 ± 13.8 | −36.3% | 0.0004 |
| Cd | 0.4 ± 0.2 | 0.4 ± 0.5 | −7.7% | 0.86 | 3.1 ± 1.5 | 2.9 ± 1.7 | −6.7% | 0.65 |
| Ni | 3.6 ± 2.3 | 3.8 ± 2.9 | 4.5% | 0.85 | 7.4 ± 3.2 | 6.2 ± 2.7 | −15.9% | 0.24 |
| As | 23.2 ± 13.7 | 47.1 ± 6.6 | 102% | 0.21 | 19.8 ± 13.3 | 50.2 ± 64.6 | 153% | 0.12 |
| Hg | 0.8 ± 0.69 | 0.85 ± 0.8 | 11% | 0.79 | 0.40 ± 0.5 | 0.42 ± 0.4 | 3.8% | 0.91 |
| Baseline Characteristics | ||||||
|---|---|---|---|---|---|---|
| Age | Sex | Race | CAD | PAD | Diabetes | Smoking |
| 86 | M | Hispanic | Y | Y | N | N |
| 69 | M | Hispanic | Y | Y | Y | N |
| 68 | M | Caucasian | Y | Y | Y | Y |
| 55 | M | Caucasian | Y | Y | Y | Y |
| 56 | M | Caucasian | Y | N | Y | Y |
| 76 | F | Caucasian | Y | Y | N | Y |
| 84 | M | Caucasian | Y | Y | Y | N |
| 90 | F | Hispanic | Y | Y | Y | Y |
| 80 | M | Caucasian | Y | Y | Y | N |
| 83 | F | Hispanic | Y | Y | Y | Y |
| 69 | F | Hispanic | Y | Y | Y | N |
| 82 | M | Hispanic | Y | Y | Y | N |
| 64 | M | Caucasian | Y | N | Y | N |
| 75 | M | Hispanic | Y | Y | Y | N |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alam, Z.H.; Ujueta, F.; Arenas, I.A.; Nigra, A.E.; Navas-Acien, A.; Lamas, G.A. Urinary Metal Levels after Repeated Edetate Disodium Infusions: Preliminary Findings. Int. J. Environ. Res. Public Health 2020, 17, 4684. https://doi.org/10.3390/ijerph17134684
Alam ZH, Ujueta F, Arenas IA, Nigra AE, Navas-Acien A, Lamas GA. Urinary Metal Levels after Repeated Edetate Disodium Infusions: Preliminary Findings. International Journal of Environmental Research and Public Health. 2020; 17(13):4684. https://doi.org/10.3390/ijerph17134684
Chicago/Turabian StyleAlam, Zenith H., Francisco Ujueta, Ivan A. Arenas, Anne E. Nigra, Ana Navas-Acien, and Gervasio A. Lamas. 2020. "Urinary Metal Levels after Repeated Edetate Disodium Infusions: Preliminary Findings" International Journal of Environmental Research and Public Health 17, no. 13: 4684. https://doi.org/10.3390/ijerph17134684
APA StyleAlam, Z. H., Ujueta, F., Arenas, I. A., Nigra, A. E., Navas-Acien, A., & Lamas, G. A. (2020). Urinary Metal Levels after Repeated Edetate Disodium Infusions: Preliminary Findings. International Journal of Environmental Research and Public Health, 17(13), 4684. https://doi.org/10.3390/ijerph17134684





