Be a Mom’s Efficacy in Enhancing Positive Mental Health among Postpartum Women Presenting Low Risk for Postpartum Depression: Results from a Pilot Randomized Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Recruitment Procedure and Participants
2.3. Randomization
2.4. Interventions
2.5. Measures
2.5.1. Primary Outcome-Positive Mental Health
2.5.2. Secondary Outcomes
2.5.3. Be a Mom’s Web System Data
2.5.4. Be a Mom’s Acceptability and Experience
2.6. Data Analysis
3. Results
3.1. Participant Characteristics
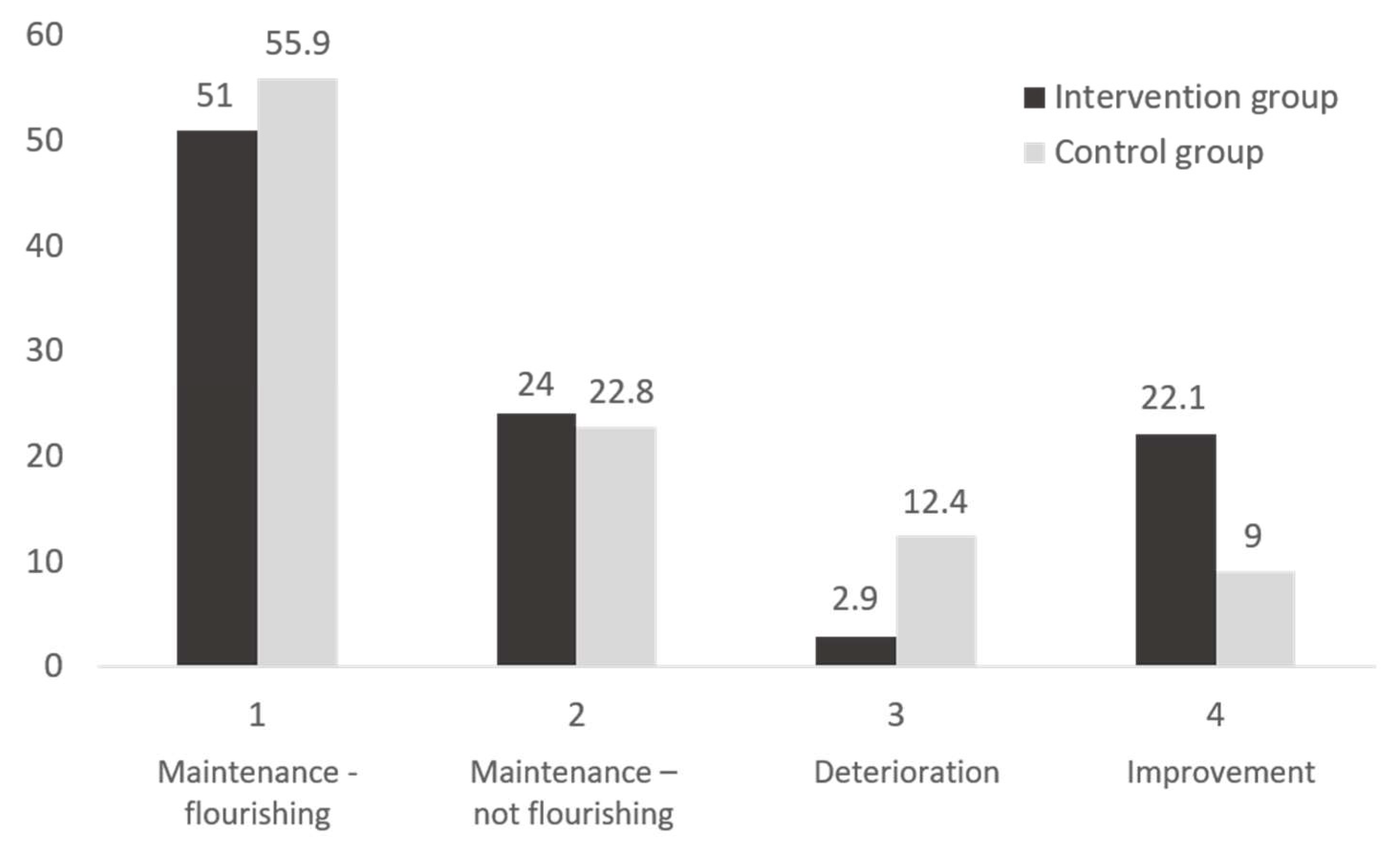
3.2. Be a Mom’s Preliminary Evidence of Efficacy: Comparison with the Control Group
3.3. Adherence to the Intervention, Be a Mom’s Usage and Acceptability
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Winson, N. Transition to motherhood. In The Social Context of Birth, 3rd ed.; Squire, C., Ed.; Routledge: London, UK, 2017. [Google Scholar] [CrossRef]
- Kanotra, S.; D’Angelo, D.; Phares, T.M.; Morrow, B.; Barfield, W.D.; Lansky, A. Challenges faced by new mothers in the early postpartum period: An analysis of comment data from the 2000 Pregnancy Risk Assessment Monitoring System (PRAMS) survey. Matern. Child Health J. 2007, 11, 549–558. [Google Scholar] [CrossRef] [PubMed]
- Woolhouse, H.; Gartland, D.; Perlen, S.; Donath, S.; Brown, S.J. Physical health after childbirth and maternal depression in the first 12 months post partum: Results of an Australian nulliparous pregnancy cohort study. Midwifery 2014, 30, 378–384. [Google Scholar] [CrossRef] [PubMed]
- Woolhouse, H.; McDonald, E.; Brown, S. Women’s experiences of sex and intimacy after childbirth: Making the adjustment to motherhood. J. Psychosom. Obstet. Gynaecol. 2012, 33, 185–190. [Google Scholar] [CrossRef] [PubMed]
- Grice, M.M.; Feda, D.; McGovern, P.; Alexander, B.H.; McCaffrey, D.; Ukestad, L. Giving birth and returning to work: The impact of work-family conflict on women’s health after childbirth. Ann. Epidemiol. 2007, 17, 791–798. [Google Scholar] [CrossRef] [PubMed]
- Nowak, M.J.; Naude, M.; Thomas, G. Returning to work after maternity leave: Childcare and workplace flexibility. J. Ind. Relat. 2013, 55, 118–135. [Google Scholar] [CrossRef]
- Jevitt, C.M.; Groer, M.W.; Crist, N.F.; Gonzalez, L.; Wagner, V.D. Postpartum stressors: A content analysis. Issues Ment. Health Nurs. 2012, 33, 309–318. [Google Scholar] [CrossRef]
- Norhayati, M.N.; Hazlina, N.H.; Asrenee, A.R.; Emilin, W.M. Magnitude and risk factors for postpartum symptoms: A literature review. J. Affect. Disord. 2015, 175, 34–52. [Google Scholar] [CrossRef]
- Murphey, C.; Carter, P.; Price, L.R.; Champion, J.D.; Nichols, F. Psychological distress in healthy low-risk first-time mothers during the postpartum period: An exploratory study. Nurs. Res. Pract. 2017, 2017, 8415083. [Google Scholar] [CrossRef]
- Weisman, O.; Granat, A.; Gilboa-Schechtman, E.; Singer, M.; Gordon, I.; Azulay, H.; Kuint, J.; Feldman, R. The experience of labor, maternal perception of the infant, and the mother’s postpartum mood in a low-risk community cohort. Arch. Womens Ment. Health 2010, 13, 505–513. [Google Scholar] [CrossRef]
- Slomian, J.; Honvo, G.; Emonts, P.; Reginster, J.Y.; Bruyere, O. Consequences of maternal postpartum depression: A systematic review of maternal and infant outcomes. Womens Health (Lond.) 2019, 15, 1745506519844044. [Google Scholar] [CrossRef]
- Wen, D.J.; Poh, J.S.; Ni, S.N.; Chong, Y.S.; Chen, H.; Kwek, K.; Shek, L.P.; Gluckman, P.D.; Fortier, M.V.; Meaney, M.J.; et al. Influences of prenatal and postnatal maternal depression on amygdala volume and microstructure in young children. Transl. Psychiatry 2017, 7, e1103. [Google Scholar] [CrossRef] [PubMed]
- Bauer, A.; Knapp, M.; Parsonage, M. Lifetime costs of perinatal anxiety and depression. J. Affect. Disord. 2016, 192, 83–90. [Google Scholar] [CrossRef] [PubMed]
- Ladd, C.; Rodriguez McCullough, N.; Carmaciu, C. Perinatal mental illness. InnovAiT 2017, 10, 653–658. [Google Scholar] [CrossRef]
- Weinberg, M.K.; Tronick, E.Z.; Beeghly, M.; Olson, K.L.; Kernan, H.; Riley, J.M. Subsyndromal depressive symptoms and major depression in postpartum women. Am. J. Orthopsychiatry 2001, 71, 87–97. [Google Scholar] [CrossRef]
- Sockol, L.E. A systematic review of the efficacy of cognitive behavioral therapy for treating and preventing perinatal depression. J. Affect. Disord. 2015, 177, 7–21. [Google Scholar] [CrossRef]
- Lin, P.Z.; Xue, J.M.; Yang, B.; Li, M.; Cao, F.L. Effectiveness of self-help psychological interventions for treating and preventing postpartum depression: A meta-analysis. Arch. Womens Ment. Health 2018, 21, 491–503. [Google Scholar] [CrossRef]
- Dennis, C.L.; Creedy, D. Psychosocial and psychological interventions for preventing postpartum depression. Cochrane Database Syst. Rev. 2004. [Google Scholar] [CrossRef]
- Barry, M.M.; Clarke, A.M.; Petersen, I.; Jenkins, R. Implementing Mental Health Promotion; SpringerNature Switzerland: Cham, Switzerland, 2019. [Google Scholar]
- Forsman, A.K.; Wahlbeck, K.; Aaro, L.E.; Alonso, J.; Barry, M.M.; Brunn, M.; Cardoso, G.; Cattan, M.; de Girolamo, G.; Eberhard-Gran, M.; et al. Research priorities for public mental health in Europe: Recommendations of the ROAMER project. Eur. J. Public Health 2015, 25, 249–254. [Google Scholar] [CrossRef]
- Newnham, E.A.; Hooke, G.R.; Page, A.C. Progress monitoring and feedback in psychiatric care reduces depressive symptoms. J. Affect. Disord. 2010, 127, 139–146. [Google Scholar] [CrossRef]
- Trompetter, H.R.; Lamers, S.M.A.; Westerhof, G.J.; Fledderus, M.; Bohlmeijer, E.T. Both positive mental health and psychopathology should be monitored in psychotherapy: Confirmation for the dual-factor model in acceptance and commitment therapy. Behav. Res. Ther. 2017, 91, 58–63. [Google Scholar] [CrossRef]
- Smith, V.; Daly, D.; Lundgren, I.; Eri, T.; Benstoem, C.; Devane, D. Salutogenically focused outcomes in systematic reviews of intrapartum interventions: A systematic review of systematic reviews. Midwifery 2014, 30, e151–e156. [Google Scholar] [CrossRef] [PubMed]
- Keyes, C.L. Mental illness and/or mental health? Investigating axioms of the complete state model of health. J. Consult. Clin. Psychol. 2005, 73, 539–548. [Google Scholar] [CrossRef] [PubMed]
- Howell, R.T.; Kern, M.L.; Lyubomirsky, S. Health benefits: Meta-analytically determining the impact of well-being on objective health outcomes. Health Psychol. Rev. 2007, 1, 83–136. [Google Scholar] [CrossRef]
- Keyes, C.L.; Simoes, E.J. To flourish or not: Positive mental health and all-cause mortality. Am. J. Public Health 2012, 102, 2164–2172. [Google Scholar] [CrossRef] [PubMed]
- Schotanus-Dijkstra, M.; Keyes, C.L.M.; de Graaf, R.; Ten Have, M. Recovery from mood and anxiety disorders: The influence of positive mental health. J. Affect. Disord. 2019, 252, 107–113. [Google Scholar] [CrossRef]
- Keyes, C.L.; Dhingra, S.S.; Simoes, E.J. Change in level of positive mental health as a predictor of future risk of mental illness. Am. J. Public Health 2010, 100, 2366–2371. [Google Scholar] [CrossRef]
- Phua, D.Y.; Kee, M.; Koh, D.X.P.; Rifkin-Graboi, A.; Daniels, M.; Chen, H.; Chong, Y.S.; Broekman, B.F.P.; Magiati, I.; Karnani, N.; et al. Positive maternal mental health during pregnancy associated with specific forms of adaptive development in early childhood: Evidence from a longitudinal study. Dev. Psychopathol. 2017, 29, 1573–1587. [Google Scholar] [CrossRef]
- Kazdin, A.E.; Blase, S.L. Rebooting Psychotherapy Research and Practice to Reduce the Burden of Mental Illness. Perspect. Psychol. Sci. 2011, 6, 21–37. [Google Scholar] [CrossRef]
- McGarry, J.; Kim, H.; Sheng, X.; Egger, M.; Baksh, L. Postpartum depression and help-seeking behavior. J. Midwifery Womens Health 2009, 54, 50–56. [Google Scholar] [CrossRef]
- Fonseca, A.; Gorayeb, R.; Canavarro, M.C. Womens help-seeking behaviours for depressive symptoms during the perinatal period: Socio-demographic and clinical correlates and perceived barriers to seeking professional help. Midwifery 2015, 31, 1177–1185. [Google Scholar] [CrossRef]
- Moore, D.; Ayers, S.; Drey, N. A Thematic Analysis of Stigma and Disclosure for Perinatal Depression on an Online Forum. JMIR Ment. Health 2016, 3, e18. [Google Scholar] [CrossRef] [PubMed]
- Dennis, C.L.; Chung-Lee, L. Postpartum depression help-seeking barriers and maternal treatment preferences: A qualitative systematic review. Birth 2006, 33, 323–331. [Google Scholar] [CrossRef] [PubMed]
- Lal, S.; Adair, C.E. E-mental health: A rapid review of the literature. Psychiatr. Serv. 2014, 65, 24–32. [Google Scholar] [CrossRef] [PubMed]
- Andersson, G.; Titov, N. Advantages and limitations of Internet-based interventions for common mental disorders. World Psychiatry 2014, 13, 4–11. [Google Scholar] [CrossRef] [PubMed]
- Crisp, D.; Griffiths, K.; Mackinnon, A.; Bennett, K.; Christensen, H. An online intervention for reducing depressive symptoms: Secondary benefits for self-esteem, empowerment and quality of life. Psychiatry Res. 2014, 216, 60–66. [Google Scholar] [CrossRef] [PubMed]
- van den Heuvel, J.F.; Groenhof, T.K.; Veerbeek, J.H.; van Solinge, W.W.; Lely, A.T.; Franx, A.; Bekker, M.N. eHealth as the Next-Generation Perinatal Care: An Overview of the Literature. J. Med. Internet Res. 2018, 20, e202. [Google Scholar] [CrossRef]
- Fonseca, A.; Alves, S.; Monteiro, F.; Gorayeb, R.; Canavarro, M.C. Be a Mom, a Web-Based Intervention to Prevent Postpartum Depression: Results From a Pilot Randomized Controlled Trial. Behav. Ther. 2019. [Google Scholar] [CrossRef]
- Fonseca, A.; Monteiro, F.; Alves, S.; Gorayeb, R.; Canavarro, M.C. Be a Mom, a web-based intervention to prevent postpartum depression: The enhancement of self-regulatory skills and its association with postpartum depressive symptoms. Front. Psychol. 2019, 10, 265. [Google Scholar] [CrossRef]
- Ciarrochi, J.; Kashdan, T.B. (Eds.) The foundations of flourishing. In Mindfulness, Acceptance and Positive Psychology; New Harbinger Press: Oakland, CA, USA, 2013; pp. 1–29. [Google Scholar]
- Powell, J.; Hamborg, T.; Stallard, N.; Burls, A.; McSorley, J.; Bennett, K.; Griffiths, K.M.; Christensen, H. Effectiveness of a web-based cognitive-behavioral tool to improve mental well-being in the general population: Randomized controlled trial. J. Med. Internet Res. 2012, 15, e2. [Google Scholar] [CrossRef]
- Rasanen, P.; Lappalainen, P.; Muotka, J.; Tolvanen, A.; Lappalainen, R. An online guided ACT intervention for enhancing the psychological wellbeing of university students: A randomized controlled clinical trial. Behav. Res. Ther. 2016, 78, 30–42. [Google Scholar] [CrossRef]
- Gammer, I.; Hartley-Jones, C.; Jones, F.W. A Randomized Controlled Trial of an Online, Compassion-Based Intervention for Maternal Psychological Well-Being in the First Year Postpartum. Mindfulness 2020, 11, 928–939. [Google Scholar] [CrossRef]
- Haga, S.M.; Kinser, P.; Wentzel-Larsen, T.; Lisøy, C.; Garthus-Niegel, S.; Slinning, K.; Drozd, F. Mamma Mia—A randomized controlled trial of an internet intervention to enhance subjective well-being in perinatal women. J. Posit. Psychol. 2020. [Google Scholar] [CrossRef]
- Lee, E.W.; Denison, F.C.; Hor, K.; Reynolds, R.M. Web-based interventions for prevention and treatment of perinatal mood disorders: A systematic review. BMC Pregnancy Childbirth 2016, 16, 38. [Google Scholar] [CrossRef] [PubMed]
- Eldridge, S.M.; Chan, C.L.; Campbell, M.J.; Bond, C.M.; Hopewell, S.; Thabane, L.; Lancaster, G.A. PAFS consensus group (2016) CONSORT 2010 statement: Extension to randomised pilot and feasibility trials. BMJ 2016, 355, i5239. [Google Scholar] [CrossRef] [PubMed]
- Eysenbach, G.; Group, C.-E. CONSORT-EHEALTH: Improving and standardizing evaluation reports of Web-based and mobile health interventions. J. Med. Internet Res. 2011, 13, e126. [Google Scholar] [CrossRef]
- Alves, S.; Fonseca, A.; Canavarro, M.C.; Pereira, M. Predictive validity of the Postpartum Depression Predictors Inventory-Revised (PDPI-R): A longitudinal study with Portuguese women. Midwifery 2019, 69, 113–120. [Google Scholar] [CrossRef]
- Fonseca, A.; Pereira, M.; Araújo-Pedrosa, A.; Gorayeb, R.; Ramos, M.M.; Canavarro, M.C. Be a Mom: Formative evaluation of a web-based psychological intervention to prevent postpartum depression. Cogn. Behav. Pract. 2018, 25, 473–495. [Google Scholar] [CrossRef]
- Alves, S.; Fonseca, A.; Canavarro, M.C.; Pereira, M. Preliminary Psychometric Testing of the Postpartum Depression Predictors Inventory-Revised (PDPI-R) in Portuguese Women. Matern. Child Health J. 2018, 22, 571–578. [Google Scholar] [CrossRef]
- Keyes, C.L.; Wissing, M.; Potgieter, J.P.; Temane, M.; Kruger, A.; van Rooy, S. Evaluation of the Mental Health Continuum-Short Form (MHC-SF) in Setswana-speaking South Africans. Clin. Psychol. Psychother. 2008, 15, 181–192. [Google Scholar] [CrossRef]
- Monteiro, F.; Fonseca, A.; Pereira, M.; Canavarro, M.C. Measuring positive mental health in the postpartum period: The bifactor structure of the Mental Health Continuum-Short Form in Portuguese women. Assessment 2020. [Google Scholar] [CrossRef]
- Areias, M.E.; Kumar, R.; Barros, H.; Figueiredo, E. Comparative incidence of depression in women and men, during pregnancy and after childbirth. Validation of the Edinburgh Postnatal Depression Scale in Portuguese mothers. Br. J. Psychiatry 1996, 169, 30–35. [Google Scholar] [CrossRef] [PubMed]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [PubMed]
- Pais-Ribeiro, J.; Silva, I.; Ferreira, T.; Martins, A.; Meneses, R.; Baltar, M. Validation study of a Portuguese version of the Hospital Anxiety and Depression Scale. Psychol. Health Med. 2007, 12, 225–235. [Google Scholar] [CrossRef] [PubMed]
- Rogers, E.S.; Chamberlin, J.; Ellison, M.L.; Crean, T. A consumer-constructed scale to measure empowerment among users of mental health services. Psychiatr. Serv. 1997, 48, 1042–1047. [Google Scholar] [CrossRef] [PubMed]
- Jorge-Monteiro, M.F.; Ornelas, J.H. Properties of the Portuguese version of the empowerment scale with mental health organization users. Int. J. Ment. Health Syst. 2014, 8, 48. [Google Scholar] [CrossRef]
- Barnes, C.R.; Adamson-Macedo, E.N. Perceived Maternal Parenting Self-Efficacy (PMP S-E) tool: Development and validation with mothers of hospitalized preterm neonates. J. Adv. Nurs 2007, 60, 550–560. [Google Scholar] [CrossRef]
- Rusbult, C.E.; Martz, J.M.; Agnew, C.R. The Investment Model Scale: Measuring commitment level, satisfaction level, quality of alternatives, and investment size. Pers. Relatsh. 1998, 5, 357–387. [Google Scholar] [CrossRef]
- Rodrigues, D.; Lopes, D. The Investment Model Scale (IMS): Further studies on construct validation and development of a shorter version (IMS-S). J. Gen. Psychol. 2013, 140, 16–28. [Google Scholar] [CrossRef]
- Schulz, K.F.; Altman, D.G.; Moher, D.; Group, C. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. BMJ 2010, 340, c332. [Google Scholar] [CrossRef]
- Siddiqui, O.; Hung, H.M.; O’Neill, R. MMRM vs. LOCF: A comprehensive comparison based on simulation study and 25 NDA datasets. J. Biopharm. Stat. 2009, 19, 227–246. [Google Scholar] [CrossRef]
- Dyrbye, L.N.; Harper, W.; Moutier, C.; Durning, S.J.; Power, D.V.; Massie, F.S.; Eacker, A.; Thomas, M.R.; Satele, D.; Sloan, J.A.; et al. A multi-institutional study exploring the impact of positive mental health on medical students’ professionalism in an era of high burnout. Acad. Med. 2012, 87, 1024–1031. [Google Scholar] [CrossRef] [PubMed]
- Zheng, X.; Morrell, J.; Watts, K. Changes in maternal self-efficacy, postnatal depression symptoms and social support among Chinese primiparous women during the initial postpartum period: A longitudinal study. Midwifery 2018, 62, 151–160. [Google Scholar] [CrossRef]
- Law, K.H.; Dimmock, J.; Guelfi, K.J.; Nguyen, T.; Gucciardi, D.; Jackson, B. Stress, Depressive Symptoms, and Maternal Self-Efficacy in First-Time Mothers: Modelling and Predicting Change across the First Six Months of Motherhood. Appl. Psychol. Health Well Being 2019, 11, 126–147. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. Regulation of cognitive processes through perceived self-efficacy. Dev. Psychol. 1989, 25, 729–735. [Google Scholar] [CrossRef]
- Bornstein, M.H.; Hendricks, C.; Hahn, C.-S.; Haynes, O.M.; Painter, K.M.; Tamis-LeMonda, C.S. Contributors to Self-Perceived Competence, Satisfaction, Investment, and Role Balance in Maternal Parenting: A Multivariate Ecological Analysis. Parent. Sci. Pract. 2003, 3, 285–326. [Google Scholar] [CrossRef]
- Dyrdal, G.M.; Roysamb, E.; Nes, R.B.; Vitterso, J. Can a Happy Relationship Predict a Happy Life? A Population-Based Study of Maternal Well-Being During the Life Transition of Pregnancy, Infancy, and Toddlerhood. J. Happiness Stud. 2011, 12, 947–962. [Google Scholar] [CrossRef] [PubMed]
- Huppert, F.A. A New Approach to Reducing Disorder and Improving Well-Being. Perspect. Psychol. Sci. 2009, 4, 108–111. [Google Scholar] [CrossRef]
- Herrman, H.; Saxena, S.; Moodie, R. Promoting Mental Health: Concepts, Emerging Evidence, Practice. A WHO Report in Collaboration with the Victoria Health Promotion Foundation and the University of Melbourne; World Health Organization: Geneva, Switzerland, 2005. [Google Scholar]
- National Institute for Health and Excellence. Antenatal and Postnatal Mental Health: Clinical Management and Service Guidance. Updated February 2020. 2014. Available online: https://www.nice.org.uk/guidance/cg192/resources/antenatal-and-postnatal-mental-health-clinical-management-and-service-guidance-pdf-35109869806789 (accessed on 8 May 2020).

| Variables | Intervention Group (n = 191) | Control Group (n = 176) | t/χ2 |
|---|---|---|---|
| M (SD)/n (%) | M (SD)/n (%) | ||
| Age | 33 (4.04) | 33 (4.43) | −0.14 |
| Marital status | 0.53 | ||
| Married/co-habiting | 183 (95.8) | 170 (96.6) | |
| Single | 4 (2.1) | 2 (1.1) | |
| In a relationship (without living together) | 4 (2.1) | 4 (2.3) | |
| Primiparous | 140 (73.3) | 122 (69.3) | 0.71 |
| Employment status | 3.35 | ||
| Employed | 176 (92.1) | 170 (96.6) | |
| Not currently working | 15 (7.9) | 6 (3.4) | |
| Educational level | 5.66 | ||
| Up to the 9th grade | 2 (1.0) | 4 (2.3) | |
| 10th to 12th grade | 30 (15.7) | 26 (14.8) | |
| Bachelor’s degree | 83 (43.5) | 58 (33) | |
| Master’s or Doctorate | 76 (39.8) | 88 (50) | |
| Household monthly income | 4.92 | ||
| Less than 580€ | 8 (4.2) | 9 (5.1) | |
| 580–1000€ | 88 (46.1) | 80 (45.5) | |
| 1000–2000€ | 87 (45.5) | 70 (39.8) | |
| More than 2000€ | 8 (4.2) | 17 (9.7) | |
| Residence | 1.06 | ||
| Urban | 141 (73.8) | 138 (78.4) | |
| Rural | 50 (26.2) | 38 (21.6) | |
| Psychopathology history | 6.86 * | ||
| Yes | 48 (25.1) | 25 (14.2) | |
| No | 143 (74.9) | 151 (85.8) | |
| Positive mental health | 3.86 * | ||
| Flourishing | 109 (57.1) | 118 (67) | |
| Not flourishing | 82 (42.9) | 58 (33) | |
| Infant’s age (in months) | 1.89 (0.94) | 1.87 (1.32) | 0.16 |
| Infant’s sex | 0.43 | ||
| Male | 98 (51.3) | 93 (53.1) | |
| Infant’s gestational weeks (at birth) | 38.89 (1.64) | 38.95 (1.77) | −0.33 |
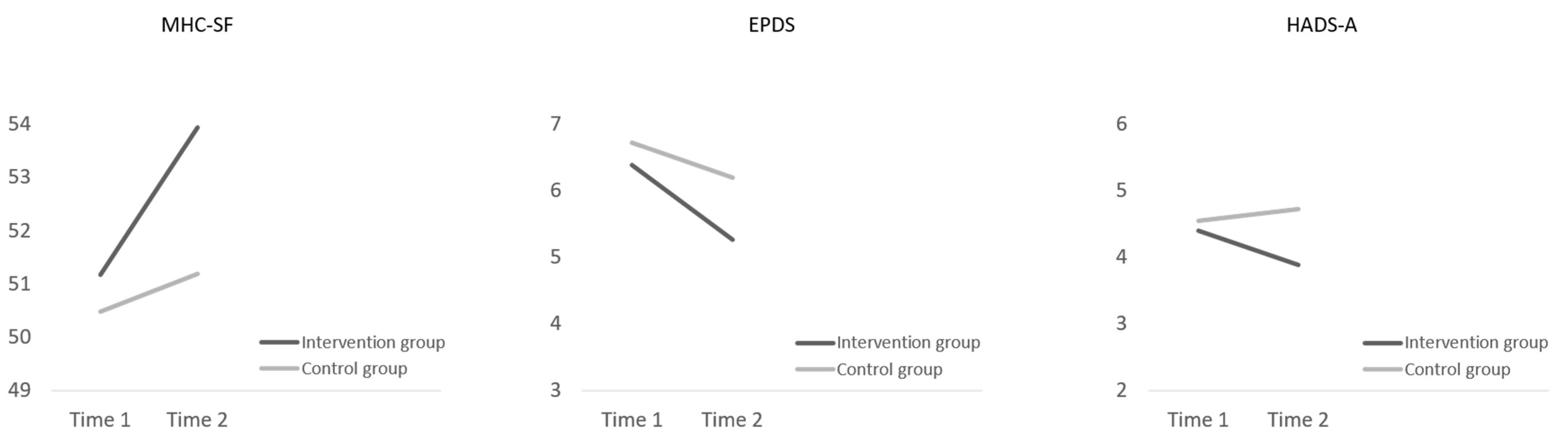
| Variables | Group | Time 1 M (SE) | Time 2 M (SE) | Effect | B (SE) | 95% CI | p |
|---|---|---|---|---|---|---|---|
| MHC-SF | Intervention | 51.17 (0.54) | 53.94 (0.69) | Time | −2.77 (0.69) | [−4.13, −1.40] | <0.001 |
| Control | 50.47 (0.57) | 51.19 (0.61) | Group | −2.74 (0.93) | [−4.56, −0.92] | 0.003 | |
| Time × Group | 2.05 (0.93) | [0.22, 3.87] | 0.028 | ||||
| Psychopathology history | 0.43 (0.88) | [−1.31, 2.16] | 0.630 | ||||
| MHC-SF baseline category | 13.75 (0.73) | [12.31, 15.18] | <0.001 | ||||
| Infant’s age | −0.10 (0.31) | [−0.70, 0.50] | 0.748 | ||||
| EPDS | Intervention | 6.38 (0.26) | 5.26 (0.33) | Time | 1.12 (0.34) | [0.45, 1.80] | 0.001 |
| Control | 6.72 (0.27) | 6.19 (0.29) | Group | 0.93 (0.45) | [−0.06, 1.81] | 0.036 | |
| Time × Group | −0.60 (0.46) | [−1.50, 0.31] | 0.194 | ||||
| Psychopathology history | −1.43 (0.42) | [−2.25, −0.61] | 0.001 | ||||
| MHC-SF baseline category | −2.75 (0.34) | [−3.42, −2.08] | <0.001 | ||||
| Infant’s age | −0.05 (0.14) | [−0.33, 0.23] | 0.739 | ||||
| HADS-A | Intervention | 4.40 (0.22) | 3.88 (0.28) | Time | 0.53 (0.29) | [−0.04, 1.09] | 0.069 |
| Control | 4.54 (0.23) | 4.72 (0.25) | Group | 0.84 (0.38) | [0.09, 1.59] | 0.028 | |
| Time × Group | −0.71 (0.38) | [−1.46, 0.05] | 0.067 | ||||
| Psychopathology history | −2.02 (0.36) | [−2.73, −1.31] | <0.001 | ||||
| MHC-SF baseline category | −1.62 (0.30) | [−2.20, −1.04] | <0.001 | ||||
| Infant’s age | 0.05 (0.12) | [−0.20, 0.29] | 0.710 | ||||
| PMPS-E | Intervention | 69.06 (0.48) | 73.09 (0.59) | Time | −4.11 (0.58) | [−5.14, −2.92] | <0.001 |
| Control | 67.87 (0.50) | 72.57 (0.53) | Group | −0.56 (0.81) | [−2.09, 1.05] | 0.517 | |
| Time × Group | −0.63 (0.77) | [−2.15, 0.81] | 0.375 | ||||
| Psychopathology history | −0.80 (0.79) | [−2.41, 0.72] | 0.285 | ||||
| MHC-SF baseline category | 3.84 (0.65) | [2.54, 5.10] | <0.001 | ||||
| Infant’s age | 0.94 (0.27) | [0.40, 1.47] | 0.001 | ||||
| ES | Intervention | 61.05 (0.38) | 61.52 (0.46) | Time | −0.47 (0.40) | [−1.27, 0.32] | 0.244 |
| Control | 61.32 (0.40) | 61.05 (0.42) | Group | −0.47 (0.63) | [−1.70, 0.76] | 0.454 | |
| Time × Group | 0.74 (0.54) | [−0.32, 1.79] | 0.170 | ||||
| Psychopathology history | 0.73 (0.65) | [−0.55, 2.01] | 0.264 | ||||
| MHC-SF baseline category | 4.29 (0.53) | [3.24, 5.34] | <0.001 | ||||
| Infant’s age | −0.22 (0.22) | [−0.66, 0.22] | 0.331 | ||||
| IMS-S | Intervention | 6.54 (0.09) | 6.36 (0.11) | Time | 0.19 (0.09) | [0.00, 0.37] | 0.046 |
| Control | 6.48 (0.09) | 6.30 (0.10) | Group | −0.05 (0.14) | [−0.33, 0.23] | 0.718 | |
| Time × Group | −0.02 (0.12) | [−0.26, 0.23] | 0.901 | ||||
| Psychopathology history | 0.20 (0.15) | [−0.08, 0.49] | 0.166 | ||||
| MHC-SF baseline category | 0.57 (0.12) | [0.33, 0.81] | <0.001 | ||||
| Infant’s age | −0.11 (0.05) | [−0.21, −0.02] | 0.024 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Monteiro, F.; Pereira, M.; Canavarro, M.C.; Fonseca, A. Be a Mom’s Efficacy in Enhancing Positive Mental Health among Postpartum Women Presenting Low Risk for Postpartum Depression: Results from a Pilot Randomized Trial. Int. J. Environ. Res. Public Health 2020, 17, 4679. https://doi.org/10.3390/ijerph17134679
Monteiro F, Pereira M, Canavarro MC, Fonseca A. Be a Mom’s Efficacy in Enhancing Positive Mental Health among Postpartum Women Presenting Low Risk for Postpartum Depression: Results from a Pilot Randomized Trial. International Journal of Environmental Research and Public Health. 2020; 17(13):4679. https://doi.org/10.3390/ijerph17134679
Chicago/Turabian StyleMonteiro, Fabiana, Marco Pereira, Maria Cristina Canavarro, and Ana Fonseca. 2020. "Be a Mom’s Efficacy in Enhancing Positive Mental Health among Postpartum Women Presenting Low Risk for Postpartum Depression: Results from a Pilot Randomized Trial" International Journal of Environmental Research and Public Health 17, no. 13: 4679. https://doi.org/10.3390/ijerph17134679
APA StyleMonteiro, F., Pereira, M., Canavarro, M. C., & Fonseca, A. (2020). Be a Mom’s Efficacy in Enhancing Positive Mental Health among Postpartum Women Presenting Low Risk for Postpartum Depression: Results from a Pilot Randomized Trial. International Journal of Environmental Research and Public Health, 17(13), 4679. https://doi.org/10.3390/ijerph17134679





