Productivity Burden of Occupational Noise-Induced Hearing Loss in Australia: A Life Table Modelling Study
Abstract
1. Introduction
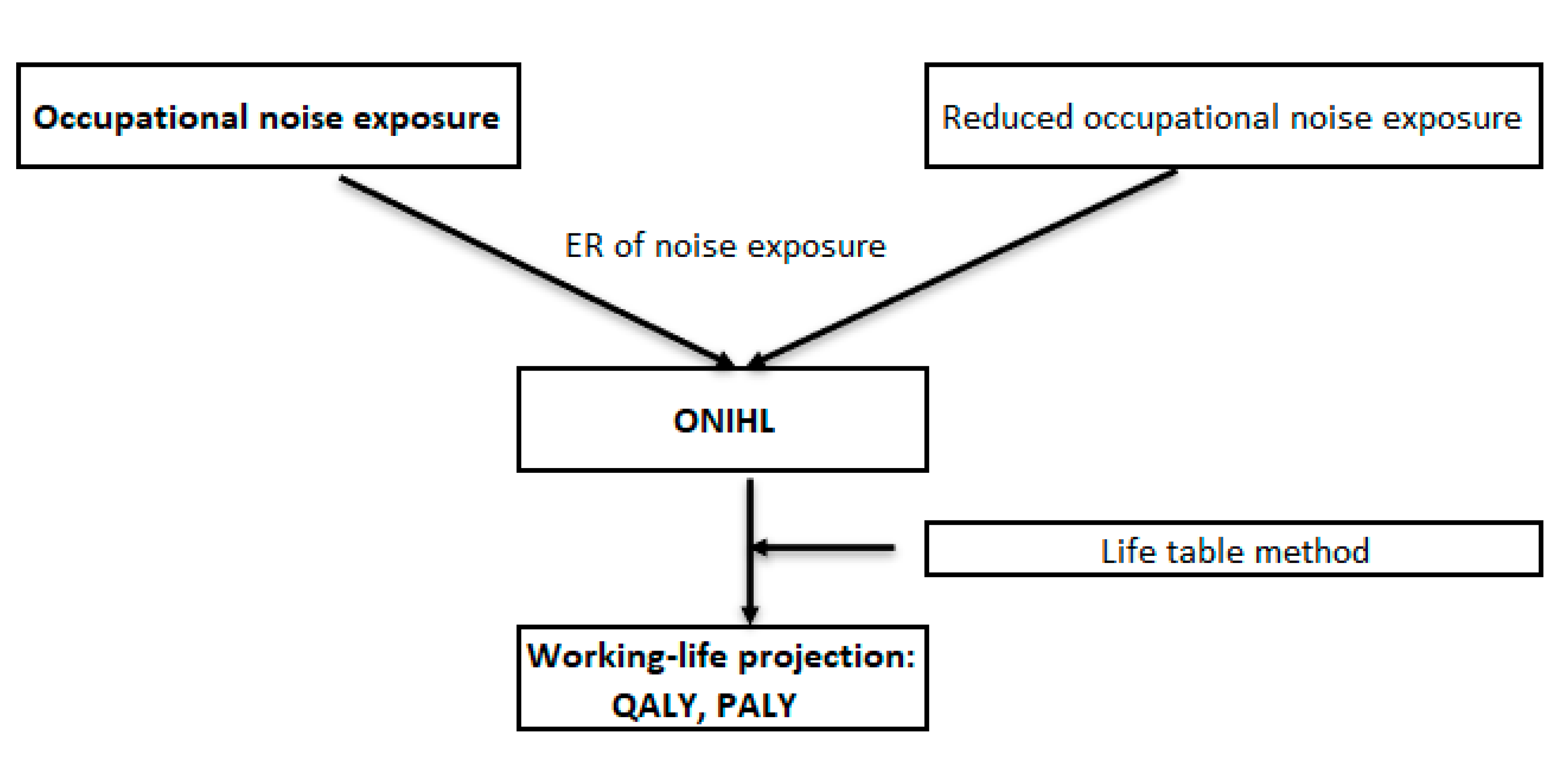
2. Materials and Methods
Data Sources
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Stevens, G.; Flaxman, S.; Brunskill, E.; Mascarenhas, M.; Mathers, C.D.; Finucane, M. Global and regional hearing impairment prevalence: An analysis of 42 studies in 29 countries. Eur. J. Public Health 2011, 23, 146–152. [Google Scholar] [CrossRef] [PubMed]
- Mathers, C.; Smith, A.; Concha, M. Global burden of hearing loss in the year 2000. GBD 2000, 18, 1–30. [Google Scholar]
- International Organization for Standardization. Acoustics: Determination of Occupational Noise Exposure and Estimation of Noise-Induced Hearing Impairmentn. International Organization for Standardizatio, 1990. Available online: https://www.iso.org/standard/6759.html (accessed on 1 June 2020).
- Gates, G.A.; Mills, J.H. Presbycusis. Lancet 2005, 366, 1111–1120. [Google Scholar] [CrossRef]
- Hearing Care Industry Association (HCIA). The Social and Economic Cost of Hearing Loss in Australia. Australia: HCIA. 2017. Available online: http://www.hcia.com.au/hcia-wp/wp-content/uploads/2015/05/Social-and-Economic-Cost-of-Hearing-Health-in-Australia_June-2017.pdf (accessed on 1 June 2020).
- Stucky, S.R.; Wolf, K.E.; Kuo, T. The economic effect of age--related hearing loss: National, state, and local estimates, 2002 and 2030. J. Am. Geriatr. Soc. 2010, 58, 618–619. [Google Scholar] [CrossRef] [PubMed]
- Access Economics. Listen Hear! The Economic Impact and Cost of Hearing Loss in Australia. Report for The Cooperative Research Centre for Cochlear Implant and Hearing Aid Innovation and Victorian Deaf Society. 2006. Available online: https://apo.org.au/sites/default/files/resource-files/2006-02/apo-nid2755.pdf (accessed on 1 June 2020).
- Lie, A.; Skogstad, M.; Johannessen, H.A.; Tynes, T.; Mehlum, I.S.; Nordby, K.-C.; Engdahl, B.; Tambs, K. Occupational noise exposure and hearing: A systematic review. Int. Arch. Occup. Environ. Health 2016, 89, 351–372. [Google Scholar] [CrossRef] [PubMed]
- Safe work Australia. Occupational Noise-Induced Hearing Loss in Australia. ACT; 2010. Available online: https://www.safeworkaustralia.gov.au/doc/occupational-noise-induced-hearing-loss-australia (accessed on 1 June 2020).
- Lewkowski, K.H.J.; Li, I.W.; Williams, W.; McCausland, K.; Gray, C.; Ytterstad, E.; Glass, D.; Fuente, A.; Si, S.; Florath, I.; et al. Exposure to noise and ototoxic chemicals in the Australian workforce. J. Occup. Med. 2019, 76, 341–348. [Google Scholar]
- Li, X.; Song, Z.; Wang, T.; Zheng, Y.; Ning, X. Health impacts of construction noise on workers: A quantitative assessment model based on exposure measurement. J. Clean Prod. 2016, 135, 721–731. [Google Scholar] [CrossRef]
- Nelson, D.I.; Nelson, R.Y.; Concha-Barrientos, M.; Fingerhut, M. The global burden of occupational noise-Induced hearing loss. Am. J. Ind. Med. 2005, 48, 446–458. [Google Scholar] [CrossRef] [PubMed]
- Dobie, R.A. The burdens of age-related and occupational noise-induced hearing loss in the United States. Ear Hear. 2008, 29, 565–577. [Google Scholar] [CrossRef] [PubMed]
- Magliano, D.J.; Martin, V.J.; Owen, A.J.; Zomer, E.; Liew, D. The Productivity Burden of Diabetes at a Population Level. Diabetes Care 2018, 41, 979–984. [Google Scholar] [CrossRef] [PubMed]
- Owen, A.J.; Maulida, S.B.; Zomer, E.; Liew, D. Productivity burden of smoking in Australia: A life table modelling study. Tob. Control 2018, 05, 42–63. [Google Scholar] [CrossRef] [PubMed]
- Concha-Barrientos, M. Occupational Noise: Assessing the Burden of Disease from Work-Related Hearing Impairment at National and Local Levels. WHO: Geneva, Switzerland, 2004. Available online: https://www.who.int/quantifying_ehimpacts/publications/9241591927/en/ (accessed on 1 June 2020).
- Australian Institute of Health and Welfare. General Record of Incidence of Mortality Books. Canberra, Australia; 2015. Available online: https://data.gov.au/data/dataset/488ef6d4-c763-4b24-b8fb-9c15b67ece19 (accessed on 1 June 2020).
- Shield, B. Evaluation of the Social and Economic Costs of Hearing Impairment. A Report for Hear-It London South Bank University. 2006. Available online: https://www.hear-it.org/sites/default/files/multimedia/documents/Hear_It_Report_October_2006.pdf (accessed on 1 June 2020).
- Hawthorne, G.; Korn, S.; Richardson, J. Population norms for the AQoL derived from the 2007 Australian National Survey of Mental Health and Wellbeing. Aust. N. Z. Int. J. Public Health 2013, 37, 7–16. [Google Scholar] [CrossRef] [PubMed]
- Health and Safety Executive. Real World Use and Performance of Hearing Protection. 2009. Available online: https://www.hse.gov.uk/research/rrpdf/rr720.pdf (accessed on 1 June 2020).
- Australian Bureau of Statistics. National Health Survey 2014–2015. 2015. Available online: https://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/4364.0.55.0012014-15?OpenDocument (accessed on 1 June 2020).
- International Organization for Standardization. Acoustics—Estimation of Noise-Induced Hearing Loss (ISO 1999:2013). 2013. Available online: https://www.iso.org/obp/ui/fr/#iso:std:iso:1999:ed-3:v1:en (accessed on 1 June 2020).
- Huang, L.; Frijters, P.; Dalziel, K.; Clarke, P. Life satisfaction, QALYs, and the monetary value of health. Soc. Sci. Med. 2018, 211, 131–136. [Google Scholar] [CrossRef] [PubMed]
- Nachtegaal, J.; Festen, J.M.; Kramer, S.E. Hearing Ability in Working Life and Its Relationship With Sick Leave and Self-Reported Work Productivity. Ear Hear. 2012, 33, 94–103. [Google Scholar] [CrossRef] [PubMed]
- Deloitte Access Economics. Social and Economic Costs of Hearing Loss in New Zealand. The National Foundation for the Deaf. 2016. Available online: https://www2.deloitte.com/content/dam/Deloitte/au/Documents/Economics/deloitte-au-economics-social-economic-cost-hearing-loss-new-zealand-021216.pdf (accessed on 1 June 2020).
- Australian Bureau of Statistics. Disability, Ageing and Carers, Australia: Summary of Findings. Australian Bureau of Statistics: Canberra, Australia, 2015. Available online: https://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/4430.02018?OpenDocument (accessed on 1 June 2020).
- The World Bank. Current Gross Domestic Product-Data 2016. Available online: https://data.worldbank.org (accessed on 1 June 2020).
- Australian Bureau of Statistics. Characteristics of Employment. Australian Bureau of Statistics: Canberra, Australia, 2016. Available online: https://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/6333.0August%202016 (accessed on 1 June 2020).
- DG Employment Social Affairs and Inclusion. Evaluation of the Practical Implementation of the EU Occupational Safety and Health (OSH) Directives in EU Member States. DG Employment, Social Affairs and Inclusion. 2015. Available online: http://ec.europa.eu/social/BlobServlet?docId=16938&langId=en (accessed on 1 June 2020).
| Age Groups | # of ONIHL | QALY Loss | PALY Loss | WTP for QALYs (AUD Million) | Long-term Condition Premium (AUD Million) | Value of PALYs (AUD Million) |
|---|---|---|---|---|---|---|
| Males | ||||||
| 20–24 * | 2126 | 1495 | 3011 | $152.5 | $80.3 | $472.8 |
| 25–29 * | 4316 | 2820 | 4807 | $287.8 | $152.9 | $754.7 |
| 30–34 | 4073 | 4142 | 7890 | $422.7 | $223.2 | $1238.7 |
| 35–39 | 8432 | 7912 | 15,385 | $807.3 | $430.8 | $2415.5 |
| 40–44 | 5200 | 4391 | 10,238 | $448.0 | $241.5 | $1607.4 |
| 45–49 | 10,374 | 7622 | 17,312 | $777.7 | $421.5 | $2718.0 |
| 50–54 | 8156 | 4892 | 11,403 | $499.1 | $271.7 | $1790.3 |
| 55–59 | 18,649 | 8097 | 17,748 | $826.2 | $448.2 | $2786.4 |
| 60–64 | 18,893 | 4157 | 9077 | $424.1 | $229.0 | $1425.0 |
| Total | 80,219 | 45,526 | 96,871 | $4645.4 | $2499.2 | $15,208.8 |
| Females | ||||||
| 20–24 * | 911 | 574 | 970 | $29.7 | $14.0 | $152.3 |
| 25–29 * | 886 | 588 | 989 | $30.5 | $14.5 | $155.3 |
| 30–34 | 44 | 45 | 77 | $2.3 | $1.1 | $12.0 |
| 35–39 | 505 | 480 | 905 | $24.9 | $11.9 | $142.1 |
| 40–44 | 4362 | 3740 | 9239 | $193.8 | $93.3 | $1450.5 |
| 45–49 | 7178 | 5364 | 14,660 | $277.9 | $134.3 | $2301.6 |
| 50–54 | 4356 | 2655 | 5927 | $137.5 | $66.8 | $930.6 |
| 55–59 | 1576 | 689 | 1213 | $35.7 | $17.4 | $190.5 |
| 60–64 | 11,699 | 2556 | 4710 | $132.4 | $64.8 | $739.4 |
| Total | 31,517 | 16,692 | 38,690 | $864.7 | $418.2 | $6074.3 |
| Reducing High Level Noise Exposure | # of HL Averted | QALY Gained | PALY Gained | WTP for QALYs Gained (AUD Million) | Long-term Condition Premium Gained (AUD Million) | Value of PALYs Gained (AUD Million) |
|---|---|---|---|---|---|---|
| Males | ||||||
| 10% reduction | 6159 | 3364 | 7156 | $343.2 | $184.7 | $1123.4 |
| 25% reduction | 15,396 | 8407 | 17,884 | $857.8 | $461.6 | $2807.8 |
| 50% reduction | 30,799 | 16,819 | 35,777 | $1716.2 | $923.5 | $5617.0 |
| 75% reduction | 46,198 | 25,228 | 53,665 | $2574.2 | $1385.2 | $8425.4 |
| 90% reduction | 55,434 | 30,271 | 64,394 | $3088.8 | $1662.2 | $10,109.8 |
| Females | ||||||
| 10% reduction | 2225 | 1160 | 2657 | $60.1 | $29.0 | $417.1 |
| 25% reduction | 5559 | 2895 | 6636 | $150.0 | $72.5 | $1041.8 |
| 50% reduction | 11,122 | 5793 | 13,278 | $300.1 | $145.1 | $2084.6 |
| 75% reduction | 16,687 | 8692 | 19,922 | $450.3 | $217.8 | $3127.8 |
| 90% reduction | 20,021 | 10,428 | 23,902 | $540.2 | $261.2 | $3752.6 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Si, S.; Lewkowski, K.; Fritschi, L.; Heyworth, J.; Liew, D.; Li, I. Productivity Burden of Occupational Noise-Induced Hearing Loss in Australia: A Life Table Modelling Study. Int. J. Environ. Res. Public Health 2020, 17, 4667. https://doi.org/10.3390/ijerph17134667
Si S, Lewkowski K, Fritschi L, Heyworth J, Liew D, Li I. Productivity Burden of Occupational Noise-Induced Hearing Loss in Australia: A Life Table Modelling Study. International Journal of Environmental Research and Public Health. 2020; 17(13):4667. https://doi.org/10.3390/ijerph17134667
Chicago/Turabian StyleSi, Si, Kate Lewkowski, Lin Fritschi, Jane Heyworth, Danny Liew, and Ian Li. 2020. "Productivity Burden of Occupational Noise-Induced Hearing Loss in Australia: A Life Table Modelling Study" International Journal of Environmental Research and Public Health 17, no. 13: 4667. https://doi.org/10.3390/ijerph17134667
APA StyleSi, S., Lewkowski, K., Fritschi, L., Heyworth, J., Liew, D., & Li, I. (2020). Productivity Burden of Occupational Noise-Induced Hearing Loss in Australia: A Life Table Modelling Study. International Journal of Environmental Research and Public Health, 17(13), 4667. https://doi.org/10.3390/ijerph17134667





