Facial Skin Temperature and Discomfort When Wearing Protective Face Masks: Thermal Infrared Imaging Evaluation and Hands Moving the Mask
Abstract
1. Introduction
2. Materials and Methods
2.1. Temperature Measurements
2.2. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Chen, J. Pathogenicity and transmissibility of 2019-nCoV-A quick overview and comparison with other emerging viruses. Microbes Infect. 2020, 22, 69–71. [Google Scholar] [CrossRef] [PubMed]
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef] [PubMed]
- Lee, V.J.; Aguilera, X.; Heymann, D.; Wilder-Smith, A. Lancet Infectious Diseases Commission Preparedness for emerging epidemic threats: A Lancet Infectious Diseases Commission. Lancet Infect. Dis. 2020, 20, 17–19. [Google Scholar] [CrossRef]
- Peng, X.; Xu, X.; Li, Y.; Cheng, L.; Zhou, X.; Ren, B. Transmission routes of 2019-nCoV and controls in dental practice. Int. J. Oral Sci. 2020, 12, 9. [Google Scholar] [CrossRef]
- To, K.K.-W.; Tsang, O.T.-Y.; Chik-Yan Yip, C.; Chan, K.-H.; Wu, T.-C.; Chan, J.M.C.; Leung, W.-S.; Chik, T.S.-H.; Choi, C.Y.-C.; Kandamby, D.H.; et al. Consistent detection of 2019 novel coronavirus in saliva. Clin. Infect. Dis. 2020. [Google Scholar] [CrossRef]
- MacIntyre, C.R.; Wang, Q.; Cauchemez, S.; Seale, H.; Dwyer, D.E.; Yang, P.; Shi, W.; Gao, Z.; Pang, X.; Zhang, Y.; et al. A cluster randomized clinical trial comparing fit-tested and non-fit-tested N95 respirators to medical masks to prevent respiratory virus infection in health care workers. Influenza Other Respir. Viruses 2011, 5, 170–179. [Google Scholar] [CrossRef]
- MacIntyre, C.R.; Wang, Q.; Seale, H.; Yang, P.; Shi, W.; Gao, Z.; Rahman, B.; Zhang, Y.; Wang, X.; Newall, A.T.; et al. A randomized clinical trial of three options for N95 respirators and medical masks in health workers. Am. J. Respir. Crit. Care Med. 2013, 187, 960–966. [Google Scholar] [CrossRef]
- Li, Y.; Tokura, H.; Guo, Y.P.; Wong, A.S.W.; Wong, T.; Chung, J.; Newton, E. Effects of wearing N95 and surgical facemasks on heart rate, thermal stress and subjective sensations. Int. Arch. Occup. Environ. Health 2005, 78, 501–509. [Google Scholar] [CrossRef]
- Fitzpatrick, T.B. The validity and practicality of sun-reactive skin types I through VI. Arch. Dermatol. 1988, 124, 869–871. [Google Scholar] [CrossRef]
- MacIntyre, C.R.; Chughtai, A.A.; Rahman, B.; Peng, Y.; Zhang, Y.; Seale, H.; Wang, X.; Wang, Q. The efficacy of medical masks and respirators against respiratory infection in healthcare workers. Influenza Other Respir. Viruses 2017, 11, 511–517. [Google Scholar] [CrossRef]
- Radonovich, L.J.; Simberkoff, M.S.; Bessesen, M.T.; Brown, A.C.; Cummings, D.A.T.; Gaydos, C.A.; Los, J.G.; Krosche, A.E.; Gibert, C.L.; Gorse, G.J.; et al. N95 Respirators vs Medical Masks for Preventing Influenza Among Health Care Personnel: A Randomized Clinical Trial. JAMA 2019, 322, 824–833. [Google Scholar] [CrossRef] [PubMed]
- Scarano, A.; Petrini, M.; Mastrangelo, F.; Noumbissi, S.; Lorusso, F. The Effects of Liquid Disinfection and Heat Sterilization Processes on Implant Drill Roughness: Energy Dispersion X-ray Microanalysis and Infrared Thermography. J. Clin. Med. 2020, 9, 19. [Google Scholar] [CrossRef] [PubMed]
- Scarano, A.; Lorusso, F.; Arcangelo, M.; D’Arcangelo, C.; Celletti, R.; de Oliveira, P.S. Lateral Sinus Floor Elevation Performed with Trapezoidal and Modified Triangular Flap Designs: A Randomized Pilot Study of Post-Operative Pain Using Thermal Infrared Imaging. Int. J. Environ. Res. Public Health 2018, 15, 1277. [Google Scholar] [CrossRef]
- Scarano, A.; Lorusso, F.; Di Cerbo, A.; Lucchina, A.G.; Carinci, F. Eradication of hairy mouth after oncological resection of the tongue and floor mouth using a diode laser 808 nm. Postoperative pain assessment using thermal infrared imaging. Lasers Surg. Med. 2019, 51, 516–521. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Yin, H.; Di, Y.; Liu, Y.; Liu, J. Human local and total heat losses in different temperature. Physiol. Behav. 2016, 157, 270–276. [Google Scholar] [CrossRef]
- Yip, W.L.; Leung, L.P.; Lau, P.F.; Tong, H.K. The effect of wearing a face mask on body temperature. Hong Kong J. Emerg. Med. 2005, 12, 23–27. [Google Scholar] [CrossRef]
- Nadel, E.R.; Mitchell, J.W.; Stolwijk, J.A.J. Differential thermal sensitivity in the human skin. Pflügers Archiv 1973, 340, 71–76. [Google Scholar] [CrossRef]
- Stevens, J.C.; Choo, K.K. Temperature sensitivity of the body surface over the life span. Somatosens Mot. Res. 1998, 15, 13–28. [Google Scholar] [CrossRef]
- Nakamura, M.; Yoda, T.; Crawshaw, L.I.; Kasuga, M.; Uchida, Y.; Tokizawa, K.; Nagashima, K.; Kanosue, K. Relative importance of different surface regions for thermal comfort in humans. Eur. J. Appl. Physiol. 2013, 113, 63–76. [Google Scholar] [CrossRef]
- Crawshaw, L.I.; Nadel, E.R.; Stolwijk, J.A.; Stamford, B.A. Effect of local cooling on sweating rate and cold sensation. Pflügers Arch. 1975, 354, 19–27. [Google Scholar] [CrossRef]
- Stevens, J.C.; Marks, L.E.; Simonson, D.C. Regional sensitivity and spatial summation in the warmth sense. Physiol. Behav. 1974, 13, 825–836. [Google Scholar] [CrossRef]
- Lenhardt, R.; Sessler, D.I. Estimation of mean body temperature from mean skin and core temperature. Anesthesiology 2006, 105, 1117–1121. [Google Scholar] [CrossRef] [PubMed]
- Marrakchi, S.; Maibach, H.I. Biophysical parameters of skin: Map of human face, regional, and age-related differences. Contact Derm. 2007, 57, 28–34. [Google Scholar] [CrossRef] [PubMed]
- Hanson, M.A. Development of a draft British standard: The assessment of heat strain for workers wearing personal protective equipment. Ann. Occup. Hyg. 1999, 43, 309–319. [Google Scholar] [CrossRef]
- Laird, I.S.; Goldsmith, R.; Pack, R.J.; Vitalis, A. The effect on heart rate and facial skin temperature of wearing respiratory protection at work. Ann. Occup. Hyg. 2002, 46, 143–148. [Google Scholar] [CrossRef]
- Cotter, J.D.; Taylor, N.A.S. The distribution of cutaneous sudomotor and alliesthesial thermosensitivity in mildly heat-stressed humans: An open-loop approach. J. Physiol. 2005, 565, 335–345. [Google Scholar] [CrossRef]
- Smith, J.D.; MacDougall, C.C.; Johnstone, J.; Copes, R.A.; Schwartz, B.; Garber, G.E. Effectiveness of N95 respirators versus surgical masks in protecting health care workers from acute respiratory infection: A systematic review and meta-analysis. CMAJ 2016, 188, 567–574. [Google Scholar] [CrossRef]
- Offeddu, V.; Yung, C.F.; Low, M.S.F.; Tam, C.C. Effectiveness of Masks and Respirators against Respiratory Infections in Healthcare Workers: A Systematic Review and Meta-Analysis. Clin. Infect. Dis. 2017, 65, 1934–1942. [Google Scholar] [CrossRef]
- Luximon, Y.; Anne Sheen, K.; Luximon, A. Time dependent infrared thermographic evaluation of facemasks. Work 2016, 54, 825–835. [Google Scholar] [CrossRef]
- Gu, J.; Zhong, Y.; Hao, Y.; Zhou, D.; Tsui, H.; Hao, C.; Gao, Q.; Ling, W.; Lau, J.T.F. Preventive behaviors and mental distress in response to H1N1 among university students in Guangzhou, China. Asia Pac. J. Public Health 2015, 27, NP1867–NP1879. [Google Scholar] [CrossRef]
- Christensen, J.; Vaeth, M.; Wenzel, A. Thermographic imaging of facial skin—Gender differences and temperature changes over time in healthy subjects. Dentomaxillofac. Radiol. 2012, 41, 662–667. [Google Scholar] [CrossRef] [PubMed]
| Humidity | Heat | Breathing Difficulty | Discomfort | Mask Touching | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Groups | N95 | Surgical Mask | N95 | Surgical Mask | N95 | Surgical Mask | N95 | Surgical Mask | N95 | Surgical Mask |
| Average (SD) | 50 ± 8.4 | 45.01 ± 3.4 | 60.5 ± 4.22 | 40.4 ± 6.77 | 60.5 ± 5.7 | 30.2 ± 6.33 | 60.3 ± 3.4 | 41.5 ± 1.5 | 12 ± 9.6 | 5.8 ± 9.6 |
| p-value | p < 0.05 | p < 0.01 | p < 0.01 | p < 0.01 | p < 0.05 | |||||
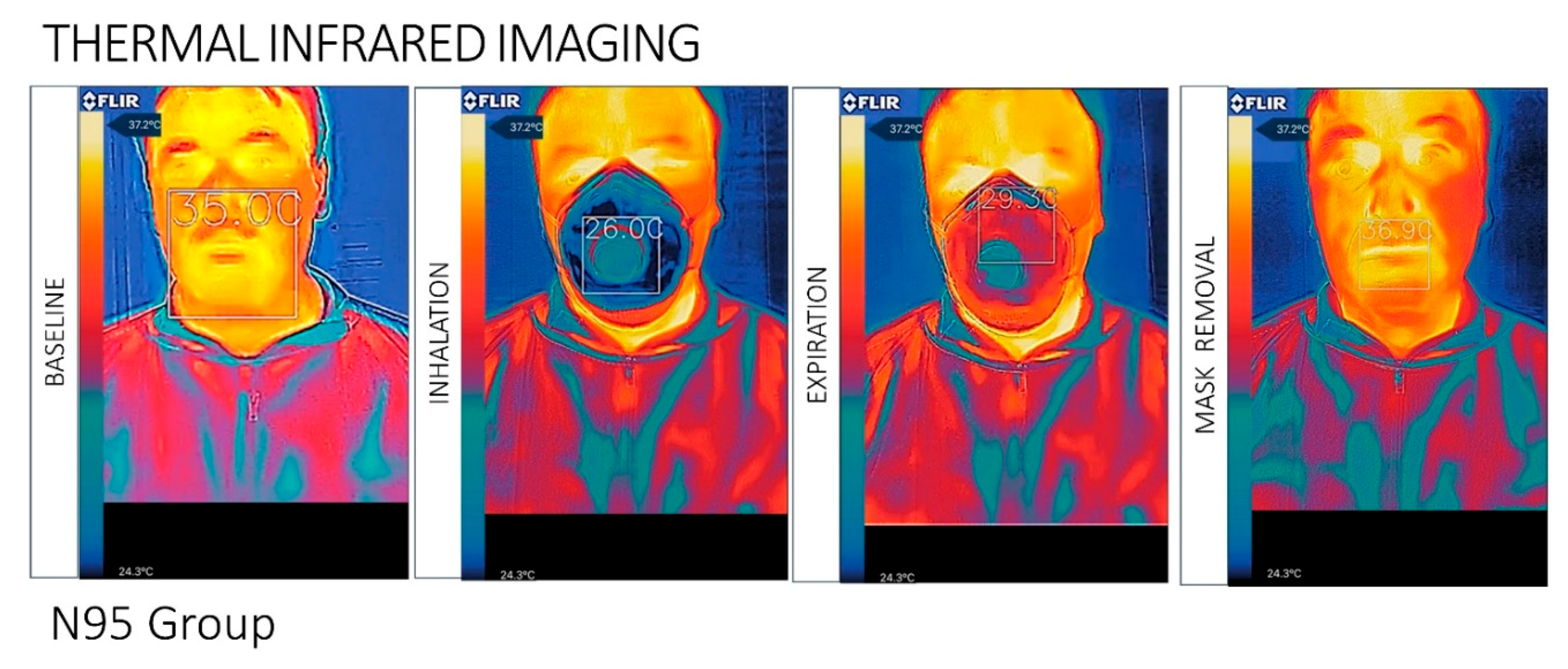
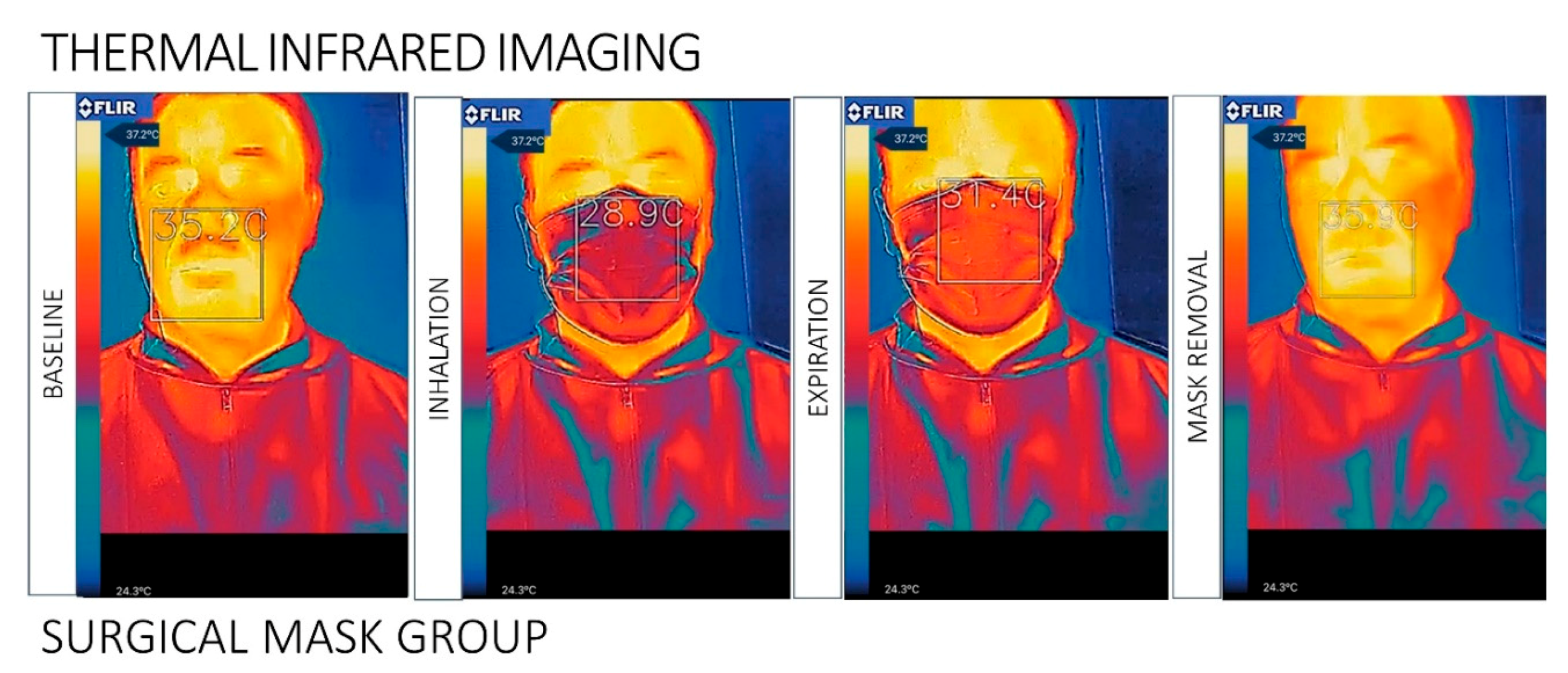
| Temperature Baseline | Temperature Inhalation | Temperature Exhalation | Temperature Mask Removal | |||||
|---|---|---|---|---|---|---|---|---|
| Groups | N95 | Surgical Mask | N95 | Surgical Mask | N95 | Surgical Mask | N95 | Surgical Mask |
| Average (SD) | 35.0 ± 2.8 °C | 35.2 ± 3.1 °C | 26.0 ± 3.6 °C | 28.9 ± 3.1 °C | 29.3° C ± 3.8 | 31.4° C ± 3.6 | 36.9 ± 4.2 °C | 35.9 ± 3.4 °C |
| p-value | p > 0.05 | p < 0.01 | p < 0.01 | p < 0.01 | ||||
| Temperature Difference ΔT[b-in] | Temperature Difference ΔT[in-ex] | Temperature Difference ΔT[b-rem] | ||||
|---|---|---|---|---|---|---|
| Groups | N95 | Surgical Mask | N95 | Surgical Mask | N95 | Surgical Mask |
| Average (SD) | 1.2 ± 0.5 °C | 0.7 ± 0.5 °C | 3.3 ± 3.6 °C | 2.5 ± 3.3 °C | 1.9 ± 3.5 °C | 0.7 ± 3.3 °C |
| p-value | p > 0.05 | p < 0.01 | p < 0.01 | |||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Scarano, A.; Inchingolo, F.; Lorusso, F. Facial Skin Temperature and Discomfort When Wearing Protective Face Masks: Thermal Infrared Imaging Evaluation and Hands Moving the Mask. Int. J. Environ. Res. Public Health 2020, 17, 4624. https://doi.org/10.3390/ijerph17134624
Scarano A, Inchingolo F, Lorusso F. Facial Skin Temperature and Discomfort When Wearing Protective Face Masks: Thermal Infrared Imaging Evaluation and Hands Moving the Mask. International Journal of Environmental Research and Public Health. 2020; 17(13):4624. https://doi.org/10.3390/ijerph17134624
Chicago/Turabian StyleScarano, Antonio, Francesco Inchingolo, and Felice Lorusso. 2020. "Facial Skin Temperature and Discomfort When Wearing Protective Face Masks: Thermal Infrared Imaging Evaluation and Hands Moving the Mask" International Journal of Environmental Research and Public Health 17, no. 13: 4624. https://doi.org/10.3390/ijerph17134624
APA StyleScarano, A., Inchingolo, F., & Lorusso, F. (2020). Facial Skin Temperature and Discomfort When Wearing Protective Face Masks: Thermal Infrared Imaging Evaluation and Hands Moving the Mask. International Journal of Environmental Research and Public Health, 17(13), 4624. https://doi.org/10.3390/ijerph17134624







